1. Introduction
Today, the healthcare landscape faces two major sources of disruption: hyper-dynamic competition and changing customer demands. On the one hand, digitalization has the power to disrupt the industry’s current competitive dynamics, causing disorder and leading to volatile, uncertain, complex, and ambiguous (VUCA) conditions [
1]. On the other hand, digitalization makes processes, business models, and services smart and convenient for the client, following a user-driven design. Although VUCA worlds are caused by digitalization, digital capabilities are also a prerequisite to successfully cope with VUCA. Closing the digitalization gap is paramount to healthcare providers being challenged to evolve into VUCA service organizations [
2]. Here, digitalization serves as the glue and linking pin to overcome obstacles and constraints stemming from hierarchies, specializations, and the preponderance of evidence-based and science-driven healthcare. Thus, the digitalization imperative exceeds narrow MINT interpretations, standing for math, information, natural sciences, and technology. For this reason, this acronym deserves an adjustment to suit the emerging MMM–MINT framework, which also addresses the fields of medicine, marketing, and management.
In addition, we also witness a paradigm shift towards value-based healthcare, moving from treating sickness to sustaining health. Already today, patients act as co-value creators of their own health by complying with therapy standards and medical interventions. This move shifts the patients’ role and understanding as they increasingly demand to be treated as healthcare customers.
Today, hospitals still struggle with both sources of disruption—hyper-dynamic competition and changing customer demands. Many healthcare providers are burdened by the legacies of age, inertia, administrative malpractices, and anachronistic governance regimes of command and order. They often show classic signs of autocratic expert organizations lacking cross-functional coordination and networked value processes to meet cost, quality, service and agility targets. Isolated high-tech centers can only unfold their usefulness if they are part of integrated healthcare and workflow landscapes. In this respect, global supply chain management and intertwined value networks are evidence that communication, coordination, and collaboration are crucial to success. To turn full circle, creativity and capital complement the aforementioned C-ingredients of corporate success [
3].
In contrast to other industries and potential new entrants, hospitals are anything but service-, client-, and/or process-driven [
4]. This explains their vulnerability to the aggressive MedTech and HealthTech visions of digital tycoons such as SAP, Google, Salesforce, Amazon, and Apple, which challenge entrenched wisdom. These digital tycoons consequently apply digital acumen and professionalism to a currently legacy-driven healthcare system not yet braced for artificial intelligence, machine learning, and internet of medical things in big data applications. They also embrace a customer and service understanding better fitting the value-based healthcare—where proactivity beats reactivity:
Why pay for chronic diseases, avoidable therapies, and high-tech diagnostics if people are fully committed to preserve and improve their health status by means of sustainable lifestyles? Quantified self-technologies and wearables may greatly contribute to better personal health decisions, as demonstrated by digital assistants. In brief, digitalization is a multi-faceted phenomenon underlying, coining, and foreshadowing the future of healthcare. Here, ICT competences are key to success in times of disorder, dismantling, and destruction. For sure, IT competences and alignment can only be preconditions for competences, technologies, workflows, and systems of standard alignment. Beyond this, the alignment of hardware, software, brainware, and peopleware may foster strategic and operational responsiveness, robustness, and resilience with respect to VUCA conditions.
Contribution
To stay competitive and successfully deal with today’s VUCA dynamics, established healthcare organizations need to continuously adapt. However, today no standardized strategy or approach supporting continuous adaptation exists. Thus, healthcare organizations are left alone when navigating the VUCA world. I.e., when designing and implementing the continual analysis of their context and competition to identify relevant changes to be met by customized adaptation strategies fitting their unique strengths and weaknesses. While hiring consultants is possible, it is not a solution enabling hospitals to deal with constant change independently in the future.
To address this gap and enable organizations to handle the complex gestalt of holistic analyses, this article proposes, introduces, and adopts a holistic method and corresponding tool support. It aligns the MMM and MINT perspectives to excel in value-based healthcare and digitalization. To achieve this 360-degree healthcare imperative, we resort to established methods, e.g., strategic management, stakeholder value, and value-based healthcare, to address the hospitals’ domain-specific challenges and potential.
This has several advantages. First, normally, suitable theories, methods, frameworks, roadmaps, canvases, and balanced scorecards are used in an isolated and solitary fashion. In contrast, this article aims to achieve a holistic understanding. We propose and introduce the GOLD Framework, aiming at a domain-specific selection, integration, and interlinkage of these approaches [
5]. Second, the GOLD Tool integration brings the GOLD Framework to life. It enables the co-analysis and co-alignment by assimilating the selected methods into a holistic, coherent, and consistent multi-perspective and multi-step analysis process [
6]. Third, the GOLD Tool enables a structured and standardized yet customizable analysis approach, guiding its users step by step and from perspective to perspective [
7]. Fourth, this holistic approach supports the identification of relevant sources of change, their analyses, and their evaluation, and derives customized mitigation strategies. Fifth, it aims to achieve a new level of transparency, tangibility, and stakeholder alignment, easing and supporting strategic decision-making towards ambidextrous healthcare.
The contribution of the article is to demonstrate how to derive an IT-tool-supported multi-perspective approach for the healthcare domain, e.g., hospitals. It enables and integrates the top-down refinement from external to internal influences, covering macro-, meso-, and micro-level analyses (see details in
Section 4): The macro-challenges of the healthcare and hospital system get, e.g., identified and analyzed by adopting the PESTEL framework resulting in a portfolio of potential risks and opportunities. On the meso level, an adapted version of Porter’s 5 forces delineates the competitive dynamics in healthcare. The micro level gets addressed with the ambidextrous healthcare framework. It resembles a multi-perspective approach of strategic and operative coherence since many decision vectors cause a multi-constraint system (see
Figure 1).
This article’s structure:
Section 1 introduces the article. In
Section 2, we summarize relevant theories and suitable materials for the healthcare domain, its changing trends, and approaches for dealing with it.
Section 3 introduces the GOLD Framework, the GOLD Tool, and the generic process towards a domain-specific GOLD Tool integration.
Section 4 depicts the exemplary domain-specific GOLD Tool integration.
Section 5 discusses the results and their benefits/limitations before the article concludes in
Section 6 with the contributions and outlook.
3. The GOLD Approach: Materials and Methods
This section introduces the article’s methods and materials. They are the foundation of achieving a holistic understanding, stakeholder alignment, and decision support.
Our goal is to develop a multi-perspective and interactive framework—the global organization alignment and decision (GOLD) Framework—guiding the analysis of an organization’s context from top to bottom. Its main contribution: First, it guides all involved stakeholders towards an organization-wide and aligned business strategy. Second, it enables the involved users to focus on their core competences while complementing the missing (strategic) expertise with a holistic and domain-specific process guiding them step by step [
7]. The domain-specific process defined as framework and enacted as IT-tool support complements the users’ expertise with relevant theories, rules, information, etc. in a holistic and aligned fashion enabling (more) educated decisions. Third, it makes information, decisions and results transparent, monitors them, and even enables to derive at educated corrective measures.
Especially in times of VUCA, organizations benefit from this holistic, multi-step, and multi-perspective approach to increase transparency and tangibility while enabling educated and agile reactions. We propose the GOLD Framework and GOLD Tool to support consultants or organizations in systematically designing and integrating the customized process: In
Section 3.1, we introduce the need and benefits of the GOLD Framework and GOLD Tool.
Section 3.2 describes the generic process of designing a domain-specific GOLD Tool integration for a chosen target group.
Section 3.3 adopts the introduced process of
Section 3.3 for the article’s chosen target group—the hospitals’ management—to derive at the healthcare-domain-specific GOLD Tool.
3.1. Introduction of the Global Organization Alignment and Decision (GOLD) Tool
Digitalization and VUCA influences lead to continual and potentially disruptive industry changes. Thus, organizations need to continuously analyze their external contexts. The identified external changes are evaluated in the context of the organization’s internal (core) competences, strengths, and weaknesses to categorize the changes as potential new threats, opportunities, or ignorable. Based on this understanding, organizations should prioritize their next adaption/adoption projects to overcome the innovator’s dilemma: “when new technologies cause great firms to fail” [
29]. This reactive mitigation strategy only works if organizations do not overlook threatening changes and embrace dynamic capabilities that allow for agile and fast adaptation [
30].
Thus, the relevant question is how to support organizations in identifying and mitigating new opportunities and risks on time? Generally, external changes and trends are rather intangible and complex. Therefore, organizations need a holistic approach, ideally driven by a standardized process that integrates the relevant perspectives and methods for analysis. This enables organizations to continually analyze their external context, identify changes, and make these changes transparent and tangible (see
Figure 2). After identifying the changes and their impact on the industry and the organization, they need to be analyzed, evaluated, and prioritized to then design and implement suitable mitigation strategies. Throughout the process, complementary perspectives and expertise must be integrated, aligned, and supported to derive educated decisions for the organization.
Today, organizations are often supported by consultants who select fitting perspectives and methods for analysis and guide them in their usage. However, organizations miss a standardized, guided, and tool-supported approach that allows them to independently customize, analyze, and derive educated decisions. This article proposes and introduces the GOLD Framework building on the dynamic capability logic, commanding a sensing, seizing, and transforming process of change management [
30,
31]. It enables the design of dynamic and customizable strategies depicted as canvas-based interfaces, easing usability due to their familiarity in practice.
To guide this holistic, complex, and continuous process of analysis, we propose that it gets IT-tool supported. Here, we suggest the adoption of the GOLD Tool. The GOLD Tool builds on prior work such as the Business Model Developer [
32,
33] and has already been adopted in other projects targeting the Industry 4.0 context and the complexity of multi-stakeholder collaborations [
6,
7]. It has several features that support organizations in continuously analyzing their risks and potentials in a transparent, aligned, and aggregated fashion [
6,
7,
28]:
It integrates any theory and method of analysis (e.g., as a canvanized version).
It supports the integration of as many processes, steps, and perspectives as desired.
It supports the customization of the methods and/or steps to suit the target groups.
It enables users to connect the different steps, perspectives, and methods of analysis via hierarchization, interconnections, and/or overlaps. This step ensures that all entries and elements are up to date as e.g., changes in connected parts get highlighted and require checking and modifications from the users.
It guides users through the multi-step analysis process in a pre-defined and/or customizable order.
These features are the backbone of supporting a holistic, multi-perspective analysis process. Here, the GOLD Tool enables users to enforce and pre-define as many rules as desired but simultaneously offers endless customization potentials, preventing any undesired restrictions. It is unique in making analyses, results, decisions, and consequences transparent and tangible via guidance, precision, and connections despite their complexity. This allows for a new level of shared mental models and alignment among diverse stakeholder groups and experts. To build on it, it even sets the basis for decision-outcome analyses and learning (e.g., trial and error and feedback loops) to enable forecasts and scenario planning.
The GOLD Tool itself is generic, but it can be easily customized for any target group and its domain. Organizations benefit most from it if they receive and adopt it as a domain-specific instantiation [
33]. We describe the generic process of designing a domain-specific GOLD Tool in
Section 3.2 and then apply this approach to the healthcare domain in
Section 3.3. The results are introduced in
Section 4, which shows snippets of the domain-specific GOLD Tool integration for the hospitals’ management, our target group.
3.2. Proposed and Newly Designed Method: The Generic Process of Designing a Domain-Specific GOLD Tool Integration
In this sub-section, we introduce the generic process for the domain-specific GOLD Tool integration customized for a specific target group (see
Figure 3). It consists of seven steps. Each of these steps consists of two to four sub-steps (see
Figure 4). The seventh step introduces the continuous improvement and iteration of the domain-specific GOLD Tool. As the tool is meant to support organizations in adapting to changes, the GOLD Tool instantiation must be challenged and iterated over time to enable and guide its users sustainably. When describing the process steps, we assume a scenario in which a consultant customizes the GOLD Tool for the client.
Next, we introduce all seven steps of the method for domain-specific GOLD Tool support:
Define the Context of Interest: Here, the consultant defines and selects the industry, the domain, and specific target group. Also, additional dimensions such as an organization’s size, its core competencies, and its role in the corresponding supply chain can be relevant and should be addressed. This target group refinement is crucial to derive customized process steps, setting the basis for the customized domain-specific GOLD Tool.
Select Perspectives for Analysis: To derive suitable perspectives for analysis, the consultant first needs to understand the target group’s specific challenges. Identifying and understanding the challenges guides the selection of suitable domain experts. Based on their expertise, they explore and preselect the relevant perspectives and suitable theories, concepts, and frameworks for each perspective to ensure that they are addressed correctly and in the required detail. The perspectives and their support methods guide the target group to understand why, what, and how to analyze its context, and challenges/opportunities and to derive educated strategic decisions.
Canvanize Perspectives of Analysis: Since many theories, concepts, and frameworks are not defined and self-explanatory enough to guide practitioners independently, it is important to transform them into a more tangible, guidance- and result-driven form. This step is crucial to make them applicable, usable, and capable of integrating into GOLD. We suggest to canvanize them. Canvases, also referred to as visual inquiry tools, decompose complex artifacts into multiple modules. These get transformed into visual building blocks, which are structured in a logical order [
34]. The canvas and its building blocks are tangible at one glance, allowing for the canvas-wide alignment of the ideas/answers. This helps to establish a shared understanding among their interdisciplinary user groups [
35,
36]. Canvases have been already introduced in multiple fields and thus benefit from a broad familiarity. The business model canvas supporting the design of new business models is the most widely adopted [
37,
38]. To canvanize the perspectives and corresponding theories, concepts, and methods, the consultant needs to identify all relevant aspects of each to derive categories and sub-categories. These categories set the building blocks. To create a useful canvas, the categories’ and thus building blocks’ logic and interrelations must be understood to hierarchize and group them into a well-organized canvas. Ideally, the canvases’ building blocks have guiding headlines, icons, and questions to ensure that users understand their meaning. In addition, users benefit from a visual formation of the building blocks proposing a logical order of analysis. Once this step is completed, all perspectives are supported by one or more canvases. These guide the target group in defining and refining their analyses in a visual and guided manner, ensuring that nothing important gets forgotten.
Identify Dependencies of Canvases: After defining all canvases, which act as individual modules in GOLD, the process architecture and canvases’ interdependencies need to be defined. Thus, the domain experts and consultants need to define and describe the hierarchies/refinements, unilateral and multi-lateral dependencies, interleaving/overlaps of the canvases, and their building blocks and/or individual entries. In addition, they can also pre-formalize specific (business) rules, e.g., “you cannot proceed without filling in this particular building block,” “whenever you enter information in building block A, you must also define your corresponding decisions in building blocks D and E,” or “if you entered X, you cannot enter Z”. This step enables the transparency, aggregation, and up to date (horizontal and vertical) alignment of information. Whenever analyses, decisions, knowledge, information, and/or data change, it will be forwarded and thus pushed and shown on all other levels for which this change is relevant and might potentially trigger further changes and modifications. In the long run, this allows users to benefit from learned input–output dependencies.
Integrate Canvases and Dependencies: Once the canvases and their (inter-)dependencies are defined they get integrated into the GOLD Tool, following the pre-defined process architecture of step four. When this step is finished, the domain-knowledge and its holistic interrelationships become visible for the first time.
Adopt the Approach and Implement: Now, the GOLD Tool is ready to be adopted by the target group. The target group/users can now implement and analyze their macro, meso, and micro levels to obtain a holistic understanding of their status quo. Based on this understanding, they can make educated strategic decisions that drive their customized mitigation strategies.
Continuous Improvement: The domain-specific GOLD Tool instantiation is never finished. Ideally, it gets continually adopted, tested, evaluated, and iterated with suitable (and changing) use cases to validate the holistic processes’ usefulness, correctness, and theory-to-practice fit. Given the VUCA influences and technological advancements, new and/or changing perspectives, canvases, and dependencies become useful.
In addition, the users should regularly check and adapt their analyses and derive necessary changes to their decisions and strategies to ensure continuous industry fit.
3.3. The Domain-Specific GOLD Tool Integration for the Healthcare Domain
This section introduces all required materials and inputs needed to address and refine all seven steps of the process outlined in
Section 3.2 to design the healthcare-domain-specific GOLD Tool. The derived domain-specific GOLD Tool is shown in
Section 4.
3.3.1. Define Context
This article focuses on the healthcare industry and, particularly, on established healthcare organizations such as hospitals. Today, they face the challenge of digitalization and the industry’s VUCA conditions, as well as changing customer demands pushing towards value-based healthcare and initiating new competitive dynamics in the healthcare industry. The chosen target group for the holistic multi-perspective support in GOLD is the hospital’s management, which benefits from new mitigation strategies.
3.3.2. Select Perspectives for Analysis
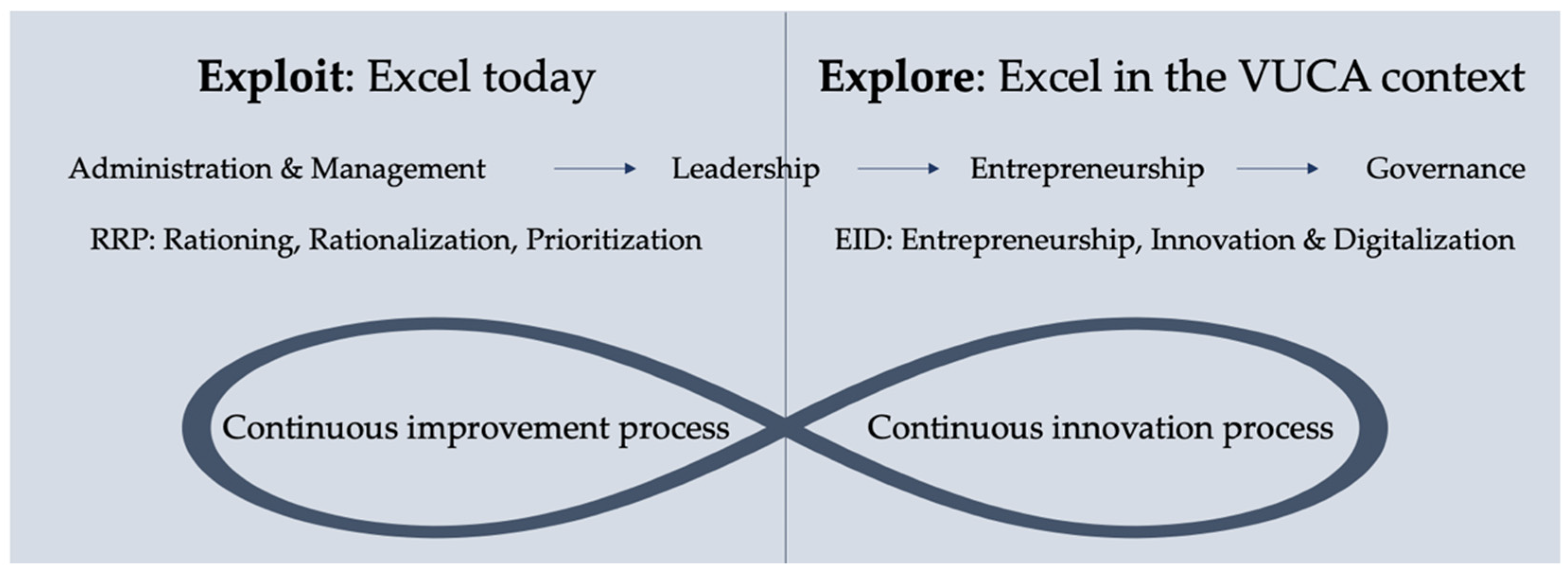
To enable the hospital’s management to make the most of its situation and competencies, it needs to be guided and supported in analyzing its external context (e.g., digitalization trends, VUCA, value-based healthcare, and MMM–MINT) and the hospital’s vision (e.g., survival, profitability, and return on health) to identify relevant external changes. Here, it needs to evaluate the derived challenges and opportunities to then design a suitable mitigation strategy and goal (e.g., ambidextrous healthcare, AMLEG) and implement it (e.g., RRP–EID, P2P framework, and TTTPPP).
To best support hospitals in this challenge, we identified and consulted healthcare management experts. In this case, two of the three authors are experts and consultants in the healthcare domain. They selected the relevant perspectives to be integrated into the domain-specific GOLD Tool. In addition to the healthcare- and digitalization-specific frameworks (see the frameworks and theories introduced in
Section 2.1), we also propose generic theories/frameworks such as PESTEL, Porter’s 5 Forces, and SWOT, which are widely adopted and already perceived as standard. These are briefly introduced here.
PESTEL: Aims at analyzing external political, economic, social, technological, environmental, and legal influences to identify relevant changes for the organization, e.g., new laws, such as the Hospitals’ Future Act nudging hospitals to digitally transform [
39]. Thus, it is essential for hospitals to be aware of these changes to prepare on time.
Porter’s 5 Forces [
40] states that any industry faces (at least) the following five competitive forces: direct competition, buyers, suppliers, substitutes, and new entrants. Porter found that the latter two are often overlooked.
SWOT [
41,
42] stands for strengths, weaknesses, opportunities, and threats. Given an organization’s internal strengths and weaknesses, they shall interpret external changes or trends to identify opportunity and/or threat potentials. All three methods of analysis aim to support organizations in analyzing their external contexts, interpreting them based on their unique situations, and deriving suitable adaptations and/or new paths.
3.3.3. Canvanize Perspectives of Analysis
While the logic of many frameworks, theories, and methods becomes clear after reading the descriptions, they are often not tangible enough for practitioners to transfer them to their practical contexts. Thus, although they are useful and helpful, they are often not adapted or not correctly adapted in practice. To ease the transfer from theory into practice, we suggest the canvanization step. In this sub-section, we introduce the canvanized VUCA framework to demonstrate and explain canvanization and its benefits (see
Figure 5).
After reading the VUCA framework description in
Section 2.1.1, users understand why VUCA conditions need to be considered. However, it remains unclear how to approach and analyze the VUCA dynamics given the organization’s context and how to derive suitable mitigation/adaptation strategies. To support the VUCA analysis, we designed a VUCA canvas analyzing and reflecting on all four VUCA dimensions. Based on these (potential) influences, users shall then reflect on related opportunities and threats given their unique context, competition, and competencies. Based on this analysis, potential strategies for mitigating the risks or enabling the opportunities can be defined. After having done it for all four dimensions in isolation, the canvas asks to derive an overarching VUCA conclusion. Based on this conclusion the most important changes/risks need to be identified to prioritize their mitigation. This is in line with the VUCA capabilities (vision, understanding, clarity, and agility) setting the groundwork to adopt dynamic capabilities or introduce new capabilities, strategies, or partnerships [
2,
3].
3.3.4. Identify Canvases’ Dependencies—Framework Alignment
Already, the multi-step analysis process in
Figure 2 showed a stepwise refinement and implied the hierarchization of the steps’ order. In the GOLD Tool,
Figure 6 shows an integrated and refined version addressing several exemplary perspectives and frameworks for analysis. In this sub-section, we aim to align the aforementioned frameworks, culminating in a manifesto for healthcare navigation in a 360-degree fashion. Healthcare navigation transcends the operational therapy and treatment levels, challenging the entrenched wisdom of conventional value creation.
First, the VUCA framework reminds us to incorporate states of discontinuity, disorder, and disruption into our mindsets, business models, and value strategies. Hospitals and healthcare institutions are challenged to accumulate corresponding VUCA capabilities to survive and thrive under conditions of hyper-competition.
Second, the RRP–EID framework is a plea for balanced healthcare navigation. Numerator and denominator navigation should aim for a strategic fit to avoid oversteering. Operational and strategic excellence are not mutually exclusive as Amazon demonstrates.
Third, ambidextrous healthcare navigation embodies the professional application of AMLEG skills in specific and sophisticated decision arenas in healthcare. Administration, management, leadership, entrepreneurship, and governance are supposed to compete with or substitute for each other. They can contribute to a self-enhancing navigation system that takes advantage of all AMLEG dimensions. The governance issue of the AMLEG framework incorporates all aspects of ownership and control prerogatives, which are essential in decision-making processes. However, visionary leadership, entrepreneurship, and governance cannot compensate for deficient administration or management, and vice versa. The AMLEG framework is a self-enhancing system calling for balanced navigation.
Fourth, the P2P framework reflects entrepreneurial blue ocean logic to step outside or complement the core business by means of start-ups and new ventures. The latter serve as strategic vehicles for exploring new arenas of sustainable value creation. The knowing-doing gap describes substantial implementation gaps that can be closed or alleviated through the P2P framework. Profit platforms represent the culmination point of value creation because of landslide digitalization, globalization, and scalability options.
Fifth, the TTTPPP framework epitomizes the new normal of digitalized healthcare, hinging on value creation by means of decision support. The latter is increasingly advanced due to big data applications, algorithms, or artificial intelligence in healthcare [
13]. The crypto-economy ushers in an era of invisible asset exploration and exploitation, which has a strong bearing on knowledge-intensive healthcare, as reflected by precision medicine. Not only can customers and criminals be predicted, but also patients!
Sixth, the MMM–MINT framework is a response to technology-driven products, services, and outcomes that often do not meet the entire advocacy of the demand side. The all-pervasive MINT disciplines in advanced healthcare deserve alignment with management, marketing, and medicine to enable a patient journey without pain points.
3.3.5. Integrate, Adopt, and Continuously Improve the Process
Once the perspectives, canvases, and their dependencies are defined, they are designed and integrated into the GOLD Tool.
Figure 6,
Figure 7 and the figures in
Section 4—Results—are all screenshots of (connected) perspectives and canvases designed, integrated, and usable in the healthcare-domain-specific GOLD Tool.
To adopt and implement the domain-specific GOLD Tool, the target group/users should follow the structure and logic of the multi-step analysis process (see
Figure 8). Initially, each canvas is empty (see
Figure 5). However, if desired, it can have some exemplary empty fields (see
Figure 7) or fields with pre-proposed inputs (see
Figure 9).
While (and after) the users analyze their current context and derive a suitable mitigation strategy, they also shall question and reflect on whether they would benefit from the adaptations and/or additions of the steps/perspectives/canvases. This way, they can further customize the process to their liking and needs.
In addition, they should ensure to regularly re-do and re-check whether their findings are still up to date or whether new changes impact their industry and/or organization in a way that requires action. One major advantage of the holistic process integration into the GOLD Tool is that the tool allows and enforces the connection of canvases, building blocks, and entries and makes the users aware of changes at other levels. This then triggers the users to check whether their analyses, findings, and/or decisions must be updated as well or whether they are still valid as they are.
4. Results
This section demonstrates how the domain-specific GOLD Tool for healthcare organizations, consisting of canvanized and interconnected frameworks/perspectives, can be adopted and applied. To keep the exemplary adoption tangible, we refined the multi-step analysis process (see
Figure 2) and pre-selected four canvanized perspectives covering all four steps, as highlighted in green in
Figure 8.
Here, one canvanized perspective addresses the macro level, one the meso level, and two address the micro level analysis. The macro-level gets analyzed via the PESTEL framework (see
Figure 9), and the meso-level via an adapted Porter’s 5 Forces analysis (see
Figure 10). Then the findings of both analyses are adopted and interpreted on the micro level (see
Figure 11), interpreting the findings based on the return on health logic (addressing RRP–EID) and the ambidextrous healthcare strategy (refined via AMLEG).
Figure 8 shows the result after step 5, where canvases and their dependencies are integrated into the domain-specific GOLD Tool (following the method depicted in
Figure 4) by considering and depicting the hierarchy across the three meta levels (macro, meso, and micro). In addition, the blue building blocks are clickable and refer to and open the canvanized framework versions. If the user clicks on PESTEL, an initially empty version of
Figure 9 opens, and if the user clicks on Porter’s 5 Forces, then
Figure 10 opens. This cross-referencing ensures that whenever the user wants to refer to the same framework/canvas/information, it can link it and thus achieve a single source of truth.
In this results section, the chosen healthcare experts pre-filled all shown canvases in a generic fashion. This is meant to support the final users (e.g., a hospital’s management) to be guided and nudged to better understand the structure of the canvases, reflect at least on the pre-filled-out perspectives/aspects, and modify, exchange, add, and/or delete the inputs given their knowledge and needs. When the healthcare experts pre-filled out the canvases, they adopted and applied the canvases from the perspective of a hospital (e.g., the Charité University Hospital in Berlin).
In the following, we briefly describe the interdependencies and findings of the pre-selected canvases. The analysis starts with the PESTEL framework (see
Figure 9). First, a generic analysis identifies the universal influences (e.g., political influences such as the Hospitals’ Future Act (in Germany)), the demographic change of population, the privatization of hospitals, the need to ensure healthcare service supply, and the equity of supply (see zoom-in highlighted in green in
Figure 9). Some entries are addressed in several of the six PESTEL dimensions: laws are political and legal influences, and the demographic change is a social influence that gets addressed in the political and legal dimensions.
Figure 8.
Holistic framework of strategic healthcare management: Translating theories into action.
Figure 8.
Holistic framework of strategic healthcare management: Translating theories into action.
Figure 9.
Adopted and applied PESTEL Analysis (showcase).
Figure 9.
Adopted and applied PESTEL Analysis (showcase).
These generic trends and influences are interpreted from the perspective of the hospital’s unique strengths and weaknesses to determine whether they are potential opportunities or threats. Once these opportunities and threats are prioritized, the hospital can focus on the most important and urgent ones to derive useful mitigation strategies step by step. In this article, we define risks to be mitigated as both overlooked opportunities and neglected threats. The Hospitals’ Future Act, for example, nudges towards the digitalization of Germany’s hospitals [
20,
43]. Given a hospital’s current digitalization level and infrastructure, the Hospitals’ Future Act can be either perceived as an opportunity (e.g., “we are already digitalized and thus will not face penalties” or “great that we receive the long-awaited initial funding to make digitalization a reality”) or as a threat (e.g., “we cannot digitalize in the pre-set timeframe and will face penalties” or “we lack the needed skills to make it possible”). Given its capabilities and perception, the hospital can design a context-fitting digitalization strategy that potentially includes support from external consultants to internally compensate for missing expertise.
Once the hospital management addressed, analyzed, and interpreted all six dimensions, it can derive an overall conclusion: the grand strategy for the coming years, e.g., Charité 2030. Given this long-term goal (e.g., the next 10 years), it can derive short-term, mid-term, and long-term steps. To derive these next steps it should first jump to the meso level, analyzing the status quo of the healthcare industry via the Porter’s 5 Forces analysis. This analysis of the industry’s unique competitive forces adds relevant aspects that should be considered when prioritizing the mitigation strategy by the hospital on the micro level.
The Porter’s 5 Forces analysis shows the current trends, power, and pressures of the (German) healthcare industry from a hospital’s perspective (see
Figure 10). First, looking at the direct competition, the hospitals can be categorized from narrow- to broad-range offers and from low-end to high-end quality. Based on these two dimensions, hospitals can position themselves in comparison to their direct competitors—other hospitals. Here, e.g., the Charité has a broad range of high-end offers. Second, the hospitals serve their customers, ranging from patients, their families, and the patients’ insurances. Third, the suppliers of a hospital are diverse, covering outpatient care (e.g., supplying patients and diagnostics), equipment (e.g., for treatments and operations), pharmacies (e.g., for medicine), construction/property, and IT services (e.g., offering safety and security). Fourth, identifying and analyzing the substitute offers, such as outpatient treatment, homeware, pharmacies, and telemedicine. Fifth, identifying potential new entrants, such as existing organizations currently serving other industries but able to enter this industry or new start-ups. New entrants have the greatest potential to disrupt the current industry dynamics with new technologies and approaches. Here, e.g., organizations from the HealthTech and MedTech sectors could introduce path-breaking innovations. Thus, it is important to consider this often-forgotten competitive force. In addition to these five forces, we added a sixth force—the complementors (e.g., analytics providers)—which enable hospitals to innovate, expand, and improve their offers. It is a relevant resource to strengthen their competitiveness. Here, competition between hospitals becomes possible.
Figure 10.
Partly adapted and applied Porter 5 Forces Analysis.
Figure 10.
Partly adapted and applied Porter 5 Forces Analysis.
Based on this analysis, the hospital’s management can derive additional opportunities and threats, which, combined with the findings of the PESTEL analysis, are the basis to derive actions for their hospitals on the micro level.
At this stage, the identified opportunities and threats need to be further refined and interpreted to plan corresponding adaptations. Thus, the hospital’s management has the task of designing, planning, and implementing their “reaction” strategy on the micro-level. Here, two frameworks are particularly relevant in the healthcare context. First, the return on health, describing the concrete goals to achieve via RRP and/or EID measures. Second, the structure and implementation from the ambidextrous healthcare perspective, which are refined with the AMLEG framework. In
Figure 11, the AMLEG framework integrates the design of the RRP and EID potentials as well as the ambidexterity encompassing operational excellence focusing on exploiting what is already there (see the left), and strategic excellence aimed at exploring novel innovations (see the right).
Figure 11.
Explaining return on health by means of the AMLEG framework.
Figure 11.
Explaining return on health by means of the AMLEG framework.
The AMLEG framework shows that, given the identified findings based on the outside-in analysis approach, the hospital has three possible reactions: freeze, adapt, or proactively drive the change. First, freeze means to keep doing what the hospital currently does. Here, some improvements and optimization are possible; however, when facing more radical external changes, this strategy is not successful in the long run. Second, the strategy to continually adapt to better fit the external changes allows the hospital to sustain its current competitiveness. This strategy works as long as the hospital’s dynamic capabilities are sufficient to address the changes qualitatively and on time [
30]. Third, it can proactively drive new changes. This approach is in line with the blue ocean strategy of rather identifying and inventing new markets and potentials than getting better in the fierce competition of existing markets [
9]. To lead this strategy to success, the hospital needs to be open to complementors and to continuously invent new approaches, technologies, and/or solutions to sustain its head start.
Given this portfolio of options, which is further refined by the additional frameworks covered in
Section 2.1, the hospital’s management needs to derive short-, mid-, and long-term strategies. In the short term, it can build upon the resource-based view, meaning that it must identify what it currently excels at and how to exploit it even more. In the mid-term, it can search for new capabilities and skills in the form of new hires, external collaboration partners, and complementors. This expands their exploration and increases their chances of staying competitive. In the long term, the hospital can also take more radical, invasive, and path-breaking steps to change the organization’s structure, culture, (IT) infrastructure, etc. towards fully embracing ambidextrous healthcare. Here, the hospital’s governance and AMLEG-style also play an important role, as they show how progressively the hospital is already organized.
Thus, this pre-filled-out, multi-step, and multi-perspective outside-in analysis guides a hospital’s management through the current trends of their external environment and industry. This makes the approach and support more tangible and enables the users to build upon them and/or modify them to better fit their needs. In addition, it also makes different coping strategies visible, which inspires the hospital’s management to find new and customized ways to fit their strengths, weaknesses, opportunities, and threats.
5. Comparison and Discussion: Towards the Lever of the GOLD Approach
This section discusses the status quo of healthcare organizations and the available support and demonstrates the lever of the GOLD approach and its IT-tool support.
5.1. Enabling the Lever of the GOLD Tool to Improve the Status Quo
When evaluating the status quo of the healthcare and hospital systems with respect to managing today’s IT challenges and the ensuing digital gap, it becomes evident that irrespective of the hospitals’ employment of high-tech equipment, they are anything but process-driven, patient-centered, or interface-oriented. Instead, today’s digital reality shows that hospitals consist of specialist silos, strict hierarchies, and inside-out expert focus, which create an ecosystem of non-cooperation, non-communication, and non-compliance with overall values. Thus, in Germany, digitalization is not a matter of technological constraints; it is a matter of people, power, and politics.
Therefore, hospitals still embody the crucial elements of craftsman organizations, which do not live up to the advanced industrial flow principles as first implemented by the famous Japanese carmaker Toyota [
44]. Here, digital tools and technologies significantly increase the pressure to act by speeding up processes, ensuring systemic connectivity, and making activities leaner, smarter, and more efficient [
45].
To move the healthcare system to the next level, it must think, collaborate, and act in a more holistic fashion. To achieve this, it must address the following five aspects:
Hospitals must rigorously detect IT and digitalization gaps through audits.
Hospitals should employ holistic navigation systems such as the GOLD Tool to delineate interfaces, interdependencies, and interdisciplinary fields of cooperation.
Digitalization is not only a matter of hardware and software but also of brainware and peopleware. All too often, people and cultures resist digital progress due to change-blocking path dependencies and legacies of age.
Hospitals must give digitalization a seat at the strategic table by creating a C-level position in the shape of a chief digital office [
46].
The GOLD Tool is no mantra or silver bullet, but a platform-based integration tool for creating a connected ecosystem of concerted and consigned action. Thus, the more it gets integrated into the existing (interconnected) IT infrastructure, the greater its lever and its possibilities for support.
Generally, the GOLD Tool serves as a holistic platform to create a holistic IT landscape by connecting and aligning people, systems, and hardware solutions by means of a one-thing approach. The GOLD Tool propels intra- and interdisciplinary cooperation and coordination of value-generating activities among involved agents. It could serve as the initial starting point to overcome parochialism in hospitals because formerly protected fiefdoms have become digitally connected. The GOLD Tool goes beyond technological gimmicks to bridge interests and disciplinary buffer zones. The one-health approach stands for service alignment since a single interface with a patient is anything but a lived reality. The GOLD Tool application in hospitals depends on five critical success factors:
Technical support: The GOLD Tool must be implemented from the service engineering point of view. Technological obstacles should be overcome with respect to systems’ integration and embeddedness.
Leadership support: Management innovations such as the GOLD Tool should be promoted by C-level agents. The chief digital officer or chief information officer could have a strong bearing on tool implementation.
Financial support: Digital change is not a free lunch but depends on financial aid and budgeting. Digitalization resembles a strategic investment, not a burden. The financial return on investment in the GOLD Tool could be very substantial due to better, smarter, leaner, and faster asset utilization in healthcare.
Platform acceptance by ease of use: The GOLD Tool reaches the tipping point of success if it is convenient, smart, and accessible. In hospitals, medical consultants are important change agents and thus should adopt the role of positive storytellers. Platform obstacles should be minimized, as user friendliness, convenience, and ease are crucial aspects of service engineering.
Social and cultural acceptance: Professionals in German clinics often perceive dashboard management systems as tight straightjackets. In contrast, the GOLD Tool is a holistic decision support system fostering customized and adapted communication, coordination, and collaboration, which must be communicated and proven to opponents.
5.2. Discussion
The GOLD Framework resembles a holistic navigation master plan that co-aligns strategy, consulting, IT, and business transformation from the viewpoint of healthcare under VUCA conditions.
Digitalization has a strong bearing on healthcare and consulting. First, the healthcare and IT industries converge when it comes to big data applications, artificial intelligence, or algorithm-based precision medicine. Second, the consulting industry witnesses disruptive digitalization imperatives as digital tools are employed to solve data-centered problems within knowledge-based and decision-induced contexts.
Compared against the status quo, the GOLD Framework contributes substantially to progress in strategic planning from the viewpoint of theoretical and practical evidence. In contrast to dashboard management systems such as canvas models or balanced scorecards, it is far more holistic and encompassing. It bridges the disciplines of management and strategy with information systems and service engineering. The GOLD Tool resembles a gold standard for proceeding with consulting and strategy-making in healthcare to arrive at fast, professional, and smart decision-making. It can be easily advanced from a paper-and-pencil version to a digital navigation masterpiece when transformed and integrated as a domain-specific GOLD Tool.
We propose to address VUCA navigation in a framework-based way that foreshadows the optional avenues of corporate development in a holistic manner. The generic framework is anything but a silver bullet for ultimate success. Rather, it is a multi-perspective approach in a canvanized format that translates theories into action. Here, the GOLD Tool fosters the idea of connected tool planning by means of data and information alignment in a systems-of-systems way. The latter condenses the complexities of consulting and healthcare into a canvas of canvas logic that incorporates theories, tools, and techniques of strategic management and could progress towards a smartphone-based navigation application following an onion logic.
On the one hand, the GOLD Tool is somehow a digitalized decision platform reflecting the crucial aspects of smart VUCA navigation. On the other hand, it is the bedrock for an integrated AMLEG pentagon model of strategic planning and execution, taking full advantage of administration, management, leadership, entrepreneurship, and governance in a truly smart way. This 360-degree AMLEG corporate navigation system goes beyond the known plan, do, check, and act steering because it is also a dialogue platform with respect to a creative design and thinking process commencing with proposals, premises, and perceptions (ideation, inspiration, and imagination) that are transformed into canvas-based strategies and value models on behalf of the client, customer, or case.
Our contribution is a platform-based solution that could start as an analogous canvas process that can be easily digitalized. It can be adopted as a generic tool but gains significant value the more domain-specific knowledge gets pre-defined and integrated by domain experts. In addition, user-generated content is also valuable to overcome the generic framework step and progress towards domain-specific insights. However, tools, techniques, and gadgets do not compensate for a lack of creativity and charisma since the most valuable business models do not incorporate AI but are inspired by visionary leaders, bright people, and smart characters. Thus, the GOLD Framework cannot compensate for a lack of the I-actors (ideation, inspiration, imagination, intelligence, or insinuation) that are a precondition for great business innovations. However, it may instigate a productive I-process in a systematic, tool-based, and digitalized way.
The GOLD Tool as a service follows the train of thought of software as a service (SaaS) since it transforms the paper and pencil world of methods into action by means of software and service engineering. Decision support, connected tool application, and real-time KPI control are alleviated, which contributes to smart corporate navigation in a holistic way. The GOLD Tool is a one-thing approach condensing relevant information at one glance. The idea of objective key results is also leveled up due to connected decision services when being challenged to pay attention to KPIs on the strategic and operative levels. In addition, the GOLD Tool also meets the standards of advanced consulting tools with respect to the digitalization imperative in contemporary consulting:
Consulting firms may use the GOLD Tool to optimize their own business models.
They arrive at better, faster, and smarter problem solutions on behalf of their clients.
The GOLD Framework fits comfortably with the challenge of solving digitally induced management problems.
The GOLD Tool shares common ground with the mindset of digital unicorns and tycoons that refrain from old-school consulting.
We propose to launch the GOLD approach carefully, incrementally, and gradually in the healthcare industry, as it often resists institutional managerial and cultural changes; this is especially true in hospitals that are “over-administrated,” “under-led,” and/or “miss-navigated.” Expert organizations such as hospitals are anything but smart service organizations due to a lack of alignment, interface coordination, seamless processes, and empathetic patient-centeredness. The GOLD Tool deserves a clear-cut testing, evaluation, and piloting procedure to meet the entire advocacy of the academic and practical communities. It should be applied to different hospital and healthcare contexts and could be transferred to other contexts and industries. Finally, the domain-specific GOLD Tool will be a must-have for healthcare management if it is available in a smart digital format that satisfies the needs of the born-digitals.
6. Contributions
This article introduced the healthcare system’s and, in particular, the hospitals’ challenges when confronted with the accelerated pace of continual changes due to digitalization and VUCA. Hospitals have two strategic options. They can drive the change and lead the innovation front, or they need to be fast adapters by excelling at dynamic capabilities. This means analyzing their context and adapting to and/or adopting new technologies, products, processes, and business models to sustain competitiveness. Ideally, they do both, embracing ambidextrous healthcare where they continuously improve what they already excel at while exploring new ways of delivering value to their customers/patients.
Today’s approaches do not provide sufficient guidance as they are specialized and adopted in isolation. Here, hospitals struggle to analyze and understand their (changing) environment and to derive suitable mitigation and adaptation strategies that fit their unique strengths and weaknesses. This has several reasons: First, it requires the adoption of suitable analysis methods and frameworks. Second, they need to be correctly understood and applied. Third, they must be considered as parts of a whole to derive a holistic understanding of their context, options, and consequences. Fourth, IT tool support for making the analysis, findings, and connections visible does not exist. This explains why PowerPoint, Microsoft Teams, and Miro are popular in strategic workshops. While consultants offer support, this becomes very costly, outsources strategic decision-making, and does not offer long-term solutions or the enablement of the hospital’s management.
To address today’s shortcomings and ensure that the hospital’s management does not overlook any relevant industry, competition, or customer changes, hospitals need to develop and integrate a process supporting the regular macro, meso, and micro analyses of their environment. The underlying logic and framework represent the semantic layer of knowledge mapping integrated into one holistic GOLD Framework, which comes alive in the GOLD Tool. This living version allows us to actively guide, nudge, and align the involved stakeholders. The more expert knowledge of domain experts gets formalized and integrated, the greater its lever of support. The support ranges from selecting (a mix of) suitable frameworks and methods to customizing and adapting them to improve usability and user-friendliness (e.g., canvanization) and integrating them into a holistic framework/process guiding the involved stakeholders step by step.
This onion approach, covering the analysis, interpretation, and reaction design processes from the generic to the specific, has the potential to enable holistic decision- and control-support. Here, the adoption of the healthcare domain-specific GOLD Tool is ideal as it guides healthcare organizations through what to analyze, how to analyze it, and how to react to it. The GOLD Tool is unique in that it excels at multi-perspective analyses, guides and supports the user through the analysis process, and remains customizable to better fit the hospital’s specific context and internal processes and/or tools [
6]. In addition, it will be possible to integrate additional features in the future.
6.1. Limitations
This article’s contribution is the design of a ready-to-implement, domain-specific instantiation of the GOLD Tool, supporting the management of hospitals in deriving customized navigation support in the context of today’s VUCA world. This domain-specific language customized for non-IT experts such as a hospital’s management addresses the sweet spot of enabling healthcare professionals to benefit from customized and guiding tool support along the complete strategic decision-making process.
While the design and its approach were designed, evaluated, and approved by two experts in the healthcare industry engaged in regular consulting projects, the proposed design and solution were not yet adopted and tested by use cases. Given the holistic nature of the approach its adoption and testing in hospitals is quite complex and will take up to one to two years to achieve. We are already in contact with interested hospitals, but at this stage, we cannot provide data, facts, or feedback from specific use cases. Here, we pose and set out to test the following hypothesis in future studies:
“The healthcare domain-specific instantiation of the GOLD Tool increases the shared understanding and alignment of the management, allowing them to make educated strategic decisions leading to improved outcomes and confidence in the management.”
6.2. Future Research
Future research directions include, but are not limited to, further evaluating, and iterating the healthcare-domain-specific integration of the GOLD Tool with use cases and examples. In addition, we also aim to explore the usability of this approach in other domains and contexts to further validate its applicability. Finally, we conclude with ten tenets ensuring that the GOLD Tool adoption adds value:
Embeddedness: The GOLD Tool should be deemed an embedded business solution that is congruent with the corporate culture and governance system of an organization. It is more than a technological gadget. It is a holistic approach embarking on strategic planning and corporate navigation.
Agility and Resilience: In contrast to waterfall planning, the GOLD Tool resembles an agile, robust, and resilient navigation logic when placing special emphasis on key strategic as well as operative success factors in a holistic, systemic, and connected manner.
Connected Navigation: Modern AMLEG navigation is also a matter of smart data and information transformation in a world of connected decision support. The GOLD Tool may serve as the platform for the desired alignment of MINT and management.
Mutually Inclusive: We invite other planning systems, strategy frameworks, and business models to become connected with the GOLD Tool. The latter can be handled as a closed, hybrid, or open system, depending on the situation at hand.
Contribution to Value Propositions and Competitive Advantages: The GOLD Tool goes beyond the balanced scorecard, objective key results, and business model canvas as it helps translate independent planning parameters into a corporate strategy.
Smart AMLEG Navigation: Administration, management, leadership, entrepreneurship, and governance are the cornerstones of a navigation pentagon. The latter takes full advantage of the GOLD Tool by means of smart data and information transformation.
Advanced Consulting: The GOLD Tool transcends and obliterates the old-school consulting, as reflected by pen and paper planning. The latter does not outlive its usefulness but deserves “digital updates” for the purpose of leaner, aggregated, aligned, and smarter problem–solution fits. The prevalence of digital challenges, IT-tools, and digital clients calls for a paradigm shift in consulting propelled by the GOLD Tool.
Overcoming the Knowing–Doing Gap: The GOLD Tool cannot replace strategy execution under real-life conditions of politics and power play, but it triggers business transformation by means of digital companionship. Being always informed about the key performance indicators and red flags is of great value when forced to get things done quickly in a robust 80:20 fashion.
No Mantra—No Silver Bullet—No Miracles: All too often, business and strategy tools become hyped, leading to narrowed and myopic views because they evoke the impression of “no alternatives.” The GOLD Tool invites everyone to take part in an open discussion on tools, techniques, and theories.
Navigation Ecosystem: Finally, the GOLD Tool is more than a tool from the viewpoint of management philosophy. For sure, it is a plea for connected tool integration, bearing in mind a one-thing approach. However, the latter also stands for the idea of ecosystem navigation when aligning and condensing different parameters through ambidextrous capabilities. Today, multi-bottleneck navigation is the new normal under conditions of disorder, disruption, and discontinuity.