Phytochemical Profiling of the Ethanolic Extract of Zaleya pentandra L. Jaffery and Its Biological Activities by In-Vitro Assays and In-Silico Molecular Docking
Abstract
1. Introduction
2. Materials and Methods
2.1. Collection and Preparation of Plant Extract
2.2. Phytochemical Analysis
2.2.1. Phytochemical Screening
2.2.2. Determination of Total Flavonoid and Total Phenolic Content
2.2.3. Gas Chromatography–Mass Spectrometry (GC–MS) Analysis
2.3. Biological Assay
2.3.1. Antioxidant Activity
2.3.2. Antibacterial Activity
2.3.3. Antiviral Activity
2.3.4. Enzyme Inhibition Assay
2.4. Computational Method
2.4.1. Molecular Docking Studies
2.4.2. ADMET Studies
2.5. Statistical Analysis
3. Results
3.1. Phytochemical Analysis
3.1.1. Primarily Phytochemical Screening
3.1.2. Total Phenolic and Flavonoid Content
3.1.3. Gas Chromatography–Mass Spectrometry (GC–MS) Analysis
3.2. Biological Activities
3.2.1. Antioxidant Activity
3.2.2. Antibacterial Activity
3.2.3. Antiviral Activity
3.2.4. Enzyme Inhibition Assays
3.3. Molecular Docking Studies
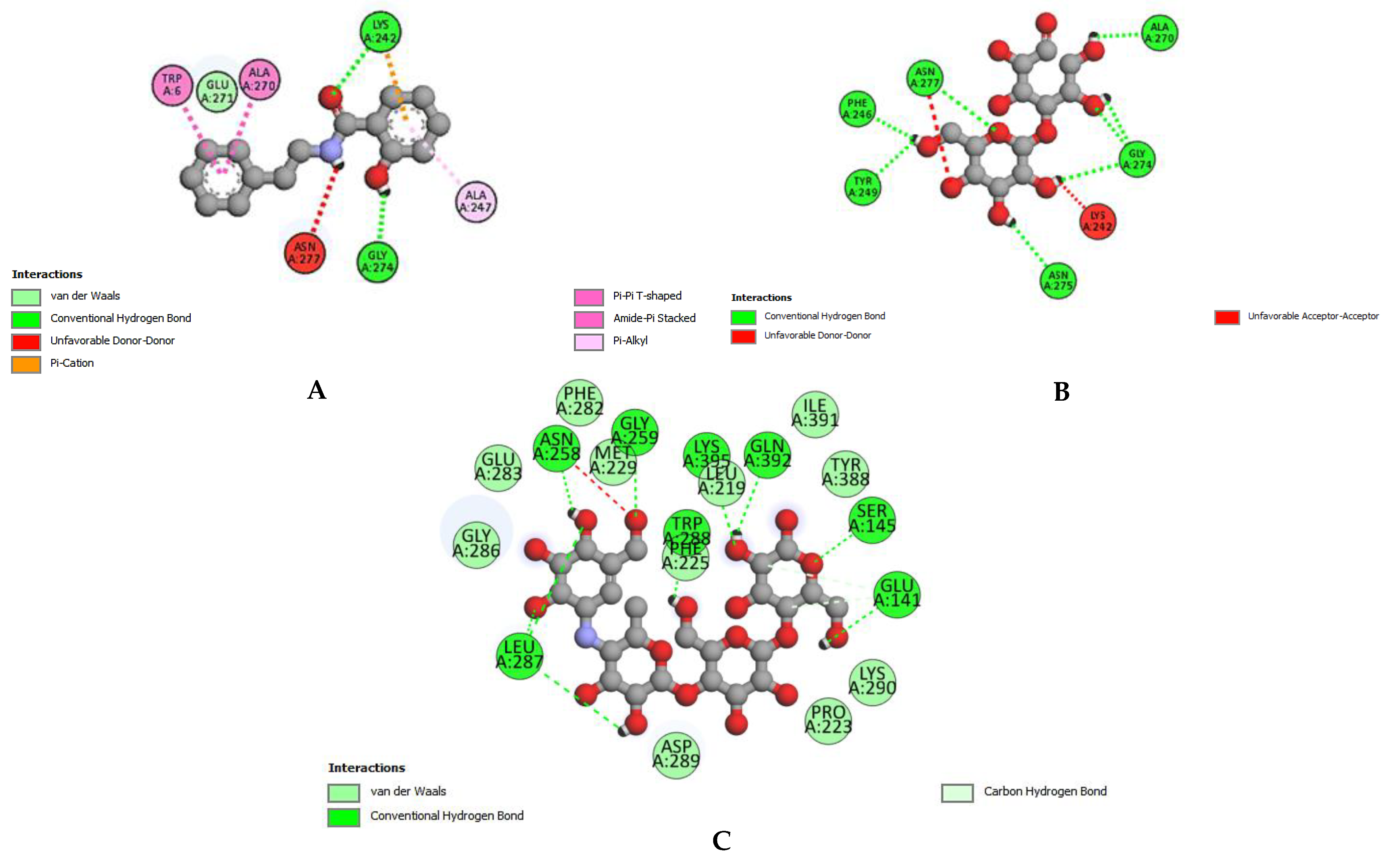
3.3.1. Molecular Docking for the Enzyme α-Glucosidase
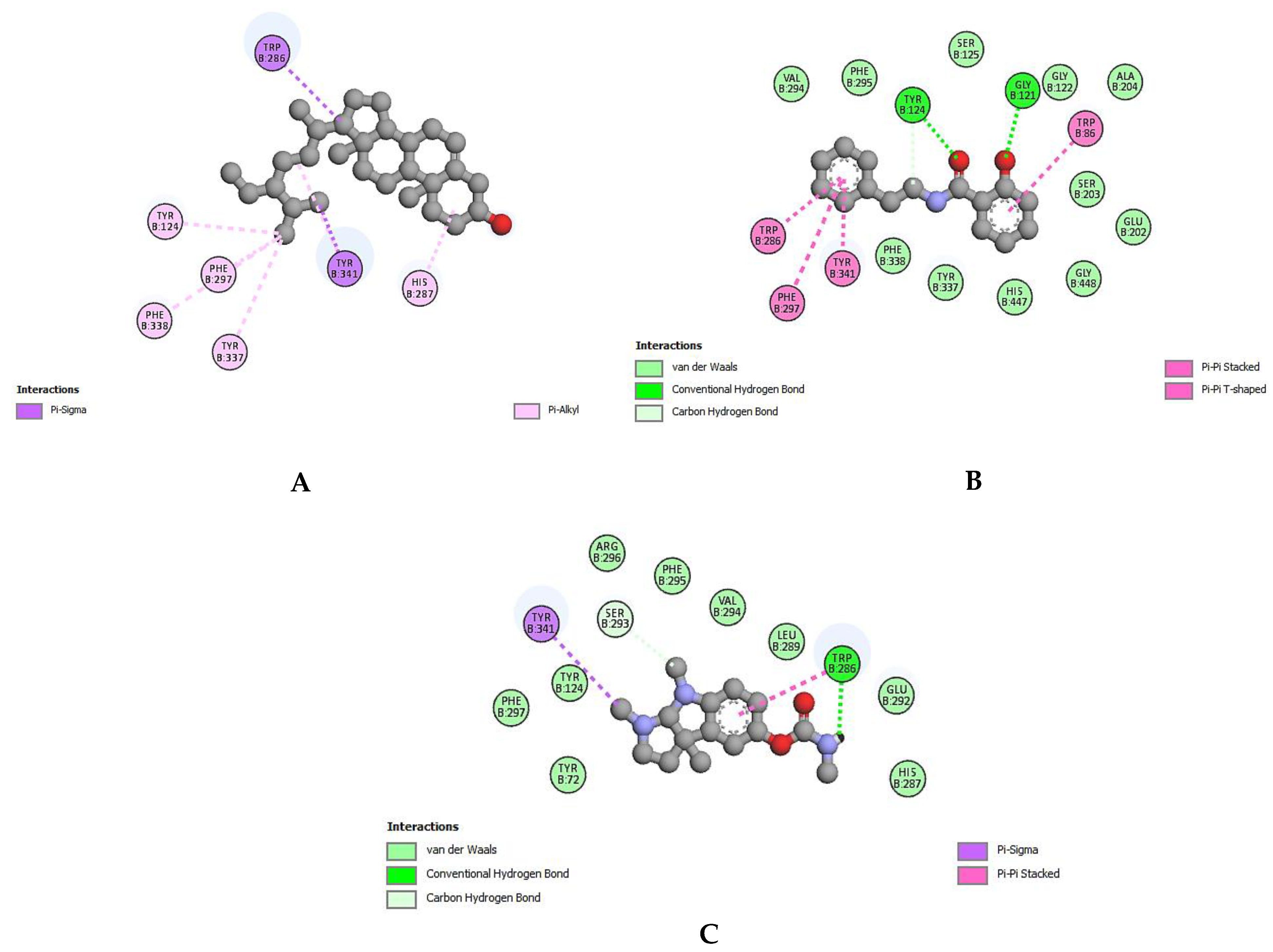
3.3.2. Molecular Docking for the Enzyme Acetylcholinesterase
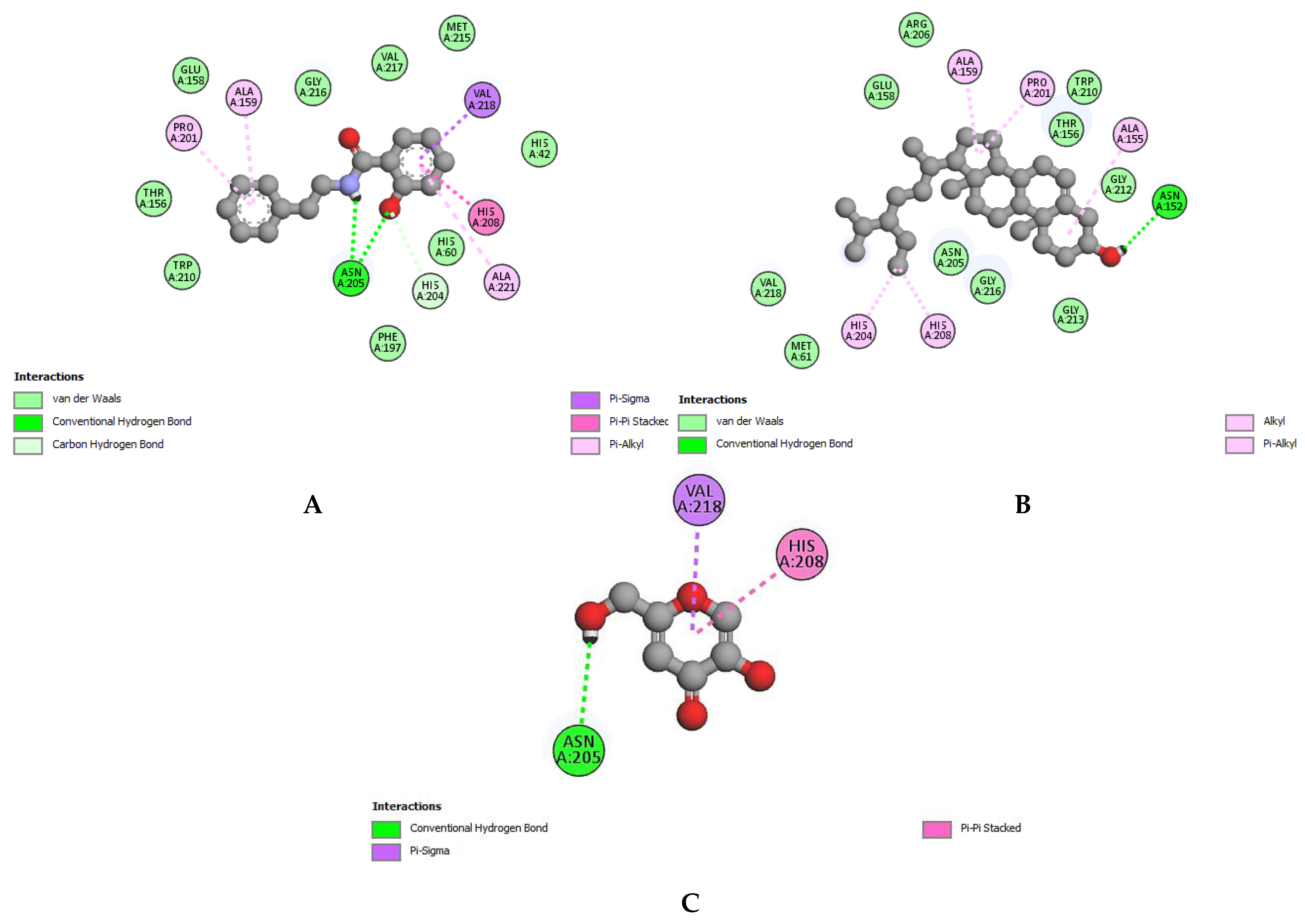
3.3.3. Molecular Docking for the Enzyme Tyrosinase
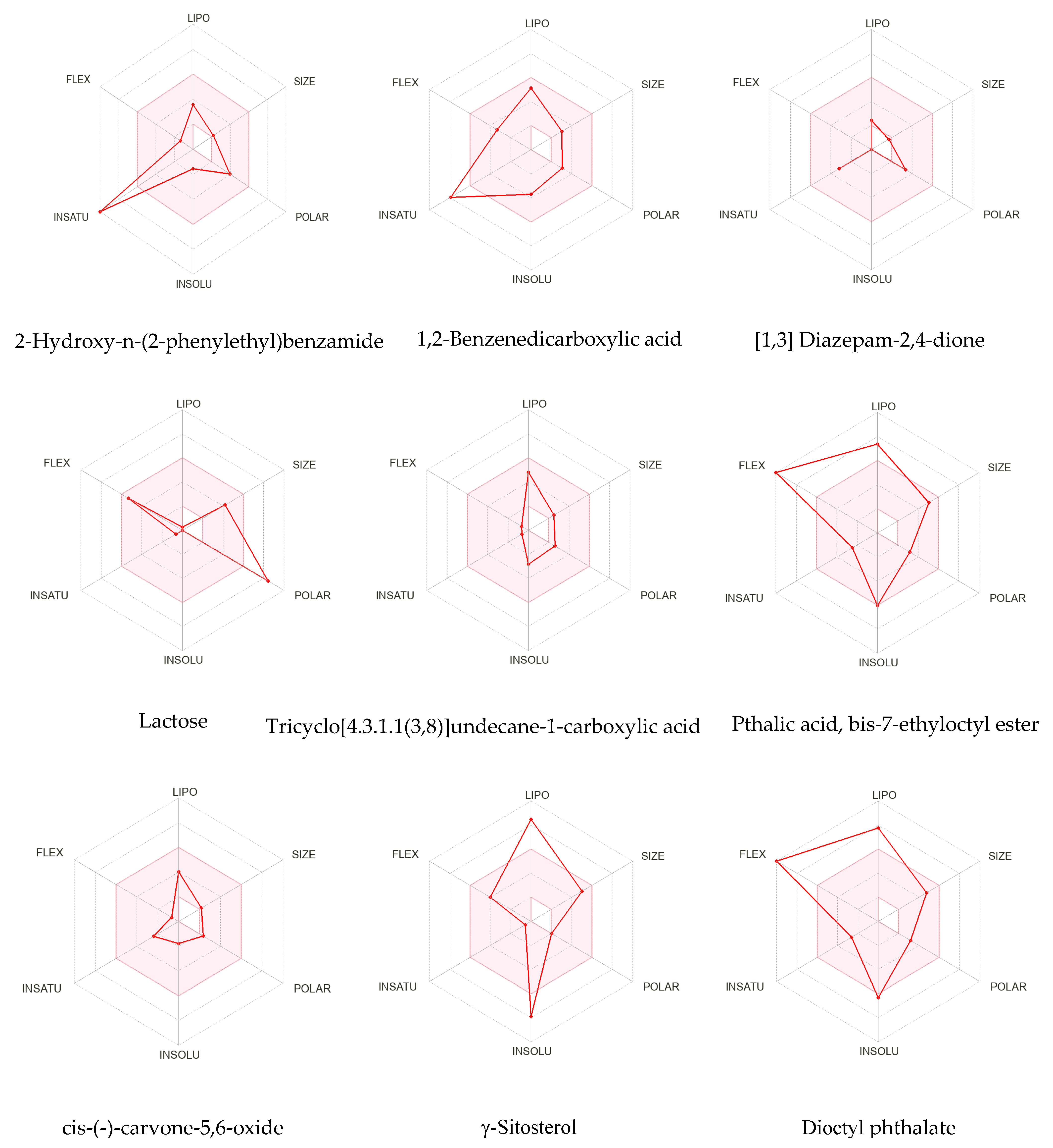
3.4. ADMET Studies
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Aziz, M.; Ahmad, S.; Iqbal, M.N.; Khurshid, U.; Saleem, H.; Alamri, A.; Anwar, S.; Alamri, A.S.; Chohan, T.A. Phytochemical, pharmacological, and In-silico molecular docking studies of Strobilanthes glutinosus Nees: An unexplored source of bioactive compounds. S. Afr. J. Bot. 2022, 147, 618–627. [Google Scholar] [CrossRef]
- Aumeeruddy, M.Z.; Mahomoodally, M.F. Combating breast cancer using combination therapy with 3 phytochemicals: Piperine, sulforaphane, and thymoquinone. Cancer 2019, 125, 1600–1611. [Google Scholar] [CrossRef] [PubMed]
- Djordjevic, S.M. From medicinal plant raw material to herbal remedies. In Aromatic and Medicinal Plants: Back to Nature; BoD—Books on Demand: Norderstedt, Germany, 2017; pp. 269–288. [Google Scholar]
- Savithramma, N.; Rao, M.L.; Suhrulatha, D. Screening of medicinal plants for secondary metabolites. Middle-East J. Sci. Res. 2011, 8, 579–584. [Google Scholar]
- Kumar, D.; Bajaj, S.; Mehrotra, R. Knowledge, attitude and practice of complementary and alternative medicines for diabetes. Public Health 2006, 120, 705–711. [Google Scholar] [CrossRef] [PubMed]
- Ahn, K. The worldwide trend of using botanical drugs and strategies for developing global drugs. BMB Rep. 2017, 50, 111. [Google Scholar] [CrossRef]
- Singh, B.; Bhat, T.K.; Singh, B. Potential therapeutic applications of some antinutritional plant secondary metabolites. J. Agric. Food Chem. 2003, 51, 5579–5597. [Google Scholar] [CrossRef]
- Seca, A.M.; Pinto, D.C. Biological potential and medical use of secondary metabolites. Medicines 2019, 6, 66. [Google Scholar] [CrossRef]
- Sadaf, H.M.; Bibi, Y.; Ishaque, M.; Nisa, S.; Qayyum, A.; Safdar, N.; Shah, Z.H.; Alsamadany, H.; Chung, G. Determination of ROS Scavenging, Antibacterial and Antifungal Potential of Methanolic Extract of Otostegia limbata (Benth.) Boiss. Plants 2021, 10, 2360. [Google Scholar] [CrossRef]
- Bingol, Z.; Kızıltaş, H.; Gören, A.C.; Kose, L.P.; Topal, M.; Durmaz, L.; Alwasel, S.H.; Gulcin, İ. Antidiabetic, anticholinergic and antioxidant activities of aerial parts of shaggy bindweed (Convulvulus betonicifolia Miller subsp.)–profiling of phenolic compounds by LC-HRMS. Heliyon 2021, 7, e06986. [Google Scholar] [CrossRef]
- Saleem, H.; Khurshid, U.; Sarfraz, M.; Tousif, M.I.; Alamri, A.; Anwar, S.; Alamri, A.; Ahmad, I.; Abdallah, H.H.; Mahomoodally, F.M. A comprehensive phytochemical, biological, toxicological and molecular docking evaluation of Suaeda fruticosa (L.) Forssk.: An edible halophyte medicinal plant. Food Chem. Toxicol. 2021, 154, 112348. [Google Scholar] [CrossRef] [PubMed]
- Mukherjee, P.K.; Biswas, R.; Sharma, A.; Banerjee, S.; Biswas, S.; Katiyar, C. Validation of medicinal herbs for anti-tyrosinase potential. J. Herb. Med. 2018, 14, 1–16. [Google Scholar] [CrossRef]
- Sajid-Ur-Rehman, M.; Ishtiaq, S.; Khan, M.A.; Alshamrani, M.; Younus, M.; Shaheen, G.; Abdullah, M.; Sarwar, G.; Khan, M.S.; Javed, F. Phytochemical profiling, in vitro and in vivo anti-inflammatory, analgesic and antipyretic potential of Sesuvium sesuvioides (Fenzl) Verdc.(Aizoaceae). Inflammopharmacology 2021, 29, 789–800. [Google Scholar] [CrossRef] [PubMed]
- Afzal, S.; Chaudhary, B.; Uzair, M.; Afzal, K.; Bokhari, T. Isolation of pentandraone from methanolic extract of aerial part of Zaleya pentandra. Int. Res. J. Pharm. 2013, 4, 2–23. [Google Scholar]
- Saleem, H.; Zengin, G.; Locatelli, M.; Ahmad, I.; Khaliq, S.; Mahomoodally, M.F.; Hussain, R.; Rengasamy, K.R.; Mollica, A.; Abidin, S.A.Z. Pharmacological, phytochemical and in-vivo toxicological perspectives of a xero-halophyte medicinal plant: Zaleya pentandra (L.) Jeffrey. Food Chem. Toxicol. 2019, 131, 110535. [Google Scholar] [CrossRef] [PubMed]
- Afzal, S.; Chaudhry, B.A.; Saeed, J.; Afzal, K.; Ahmed, B.; Qadir, M.I. Antibacterial and antioxidant activity of methanolic extract of Zaleya pentandra. Acta Pol. Pharm. 2016, 73, 147–151. [Google Scholar]
- Mughal, T.A.; Aslam, F.; Yousaf, Z.; Nisar, N.; Leung, P.C. In vitro cytotoxic activity of Zaleya pentandra L. Extracts against the breast cancer adenocarcinoma cell line MCF-7. JPMA 2020, 2019. [Google Scholar] [CrossRef]
- Kareti, S.R.; Subash, P. In silico exploration of anti-Alzheimer’s compounds present in methanolic extract of Neolamarckia cadamba bark using GC–MS/MS. Arab. J. Chem. 2020, 13, 6246–6255. [Google Scholar] [CrossRef]
- Harborne, A. Phytochemical Methods a Guide to Modern Techniques of Plant Analysis; Springer Science & Business Media: Berlin/Heidelberg, Germany, 1998. [Google Scholar]
- Sembiring, E.N.; Elya, B.; Sauriasari, R. Phytochemical screening, total flavonoid and total phenolic content and antioxidant activity of different parts of Caesalpinia bonduc (L.) Roxb. Pharmacogn. J. 2018, 10, 123–127. [Google Scholar] [CrossRef]
- Hayat, M.M.; Uzair, M. Biological potential and GC-MS analysis of phytochemicals of Farsetia hamiltonii (Royle). Biomed. Res. 2019, 30, 609–616. [Google Scholar] [CrossRef]
- Aati, H.Y.; Anwar, M.; Al-Qahtani, J.; Al-Taweel, A.; Khan, K.-u.-R.; Aati, S.; Usman, F.; Ghalloo, B.A.; Asif, H.M.; Shirazi, J.H. Phytochemical profiling, in vitro biological activities, and in-silico studies of Ficus vasta Forssk.: An unexplored plant. Antibiotics 2022, 11, 1155. [Google Scholar] [CrossRef] [PubMed]
- Ellman, G.L.; Courtney, K.D.; Andres Jr, V.; Featherstone, R.M. A new and rapid colorimetric determination of acetylcholinesterase activity. Biochem. Pharmacol. 1961, 7, 88–95. [Google Scholar] [CrossRef] [PubMed]
- Palanisamy, U.D.; Ling, L.T.; Manaharan, T.; Appleton, D. Rapid isolation of geraniin from Nephelium lappaceum rind waste and its anti-hyperglycemic activity. Food Chem. 2011, 127, 21–27. [Google Scholar] [CrossRef]
- Orhan, I.E.; Senol, F.S.; Gulpinar, A.R.; Sekeroglu, N.; Kartal, M.; Sener, B. Neuroprotective potential of some terebinth coffee brands and the unprocessed fruits of Pistacia terebinthus L. and their fatty and essential oil analyses. Food Chem. 2012, 130, 882–888. [Google Scholar] [CrossRef]
- Daina, A.; Michielin, O.; Zoete, V. SwissADME: A free web tool to evaluate pharmacokinetics, drug-likeness and medicinal chemistry friendliness of small molecules. Sci. Rep. 2017, 7, 42717. [Google Scholar] [CrossRef] [PubMed]
- Banerjee, P.; Eckert, A.O.; Schrey, A.K.; Preissner, R. ProTox-II: A webserver for the prediction of toxicity of chemicals. Nucleic Acids Res. 2018, 46, W257–W263. [Google Scholar] [CrossRef] [PubMed]
- Aykul, S.; Martinez-Hackert, E. Determination of half-maximal inhibitory concentration using biosensor-based protein interaction analysis. Anal. Biochem. 2016, 508, 97–103. [Google Scholar] [CrossRef] [PubMed]
- Murugesu, S.; Ibrahim, Z.; Ahmed, Q.U.; Uzir, B.F.; Yusoff, N.I.N.; Perumal, V.; Abas, F.; Shaari, K.; Khatib, A. Identification of α-glucosidase inhibitors from Clinacanthus nutans leaf extract using liquid chromatography-mass spectrometry-based metabolomics and protein-ligand interaction with molecular docking. J. Pharm. Anal. 2019, 9, 91–99. [Google Scholar] [CrossRef]
- Moreau, R.A.; Powell, M.J.; Singh, V. Pressurized liquid extraction of polar and nonpolar lipids in corn and oats with hexane, methylene chloride, isopropanol, and ethanol. J. Am. Oil Chem. Soc. 2003, 80, 1063–1067. [Google Scholar] [CrossRef]
- Sari, R.; Wahyuningrum, M.; Rafi, M.; Wientarsih, I. Effect of ethanol polarity on extraction yield, antioxidant, and sunscreen activities of phytochemicals from Gyrinops versteegii leaves. IOP Conf. Ser. Mater. Sci. Eng. 2020, 925, 012038. [Google Scholar]
- Zhou, K.; Yu, L. Effects of extraction solvent on wheat bran antioxidant activity estimation. LWT-Food Sci. Technol. 2004, 37, 717–721. [Google Scholar] [CrossRef]
- Phrompittayarat, W.; Putalun, W.; Tanaka, H.; Jetiyanon, K.; Wittaya-Areekul, S.; Ingkaninan, K. Comparison of various extraction methods of Bacopa monnieri. Naresuan Univ. J. Sci. Technol. (NUJST) 2013, 15, 29–34. [Google Scholar]
- Basit, A.; Ahmad, S.; Sherif, A.E.; Aati, H.Y.; Ovatlarnporn, C.; Khan, M.A.; Rao, H.; Ahmad, I.; Shahzad, M.N.; Ghalloo, B.A. New mechanistic insights on Justicia vahlii Roth: UPLC-Q-TOF-MS and GC–MS based metabolomics, in-vivo, in-silico toxicological, antioxidant based anti-inflammatory and enzyme inhibition evaluation. Arab. J. Chem. 2022, 15, 104135. [Google Scholar] [CrossRef]
- Rodrigues, M.J.; Custódio, L.; Mecha, D.; Zengin, G.; Cziáky, Z.; Sotkó, G.; Pereira, C.G. Nutritional and Phyto-Therapeutic Value of the Halophyte Cladium mariscus L.(Pohl.): A Special Focus on Seeds. Plants 2022, 11, 2910. [Google Scholar] [CrossRef]
- Balamurugan, R.; Duraipandiyan, V.; Ignacimuthu, S. Antidiabetic activity of γ-sitosterol isolated from Lippia nodiflora L. in streptozotocin induced diabetic rats. Eur. J. Pharmacol. 2011, 667, 410–418. [Google Scholar] [CrossRef]
- Jung Choi, S.; Kim, M.J.; Jin Heo, H.; Kim, J.K.; Jin Jun, W.; Kim, H.K.; Kim, E.-K.; Ok Kim, M.; Yon Cho, H.; Hwang, H.-J. Ameliorative effect of 1, 2-benzenedicarboxylic acid dinonyl ester against amyloid beta peptide-induced neurotoxicity. Amyloid 2009, 16, 15–24. [Google Scholar] [CrossRef]
- Ghalloo, B.A.; Khan, K.-u.-R.; Ahmad, S.; Aati, H.Y.; Al-Qahtani, J.H.; Ali, B.; Mukhtar, I.; Hussain, M.; Shahzad, M.N.; Ahmed, I. Phytochemical Profiling, In Vitro Biological Activities, and In Silico Molecular Docking Studies of Dracaena reflexa. Molecules 2022, 27, 913. [Google Scholar] [CrossRef]
- Saravanakumar, K.; Park, S.; Sathiyaseelan, A.; Kim, K.-N.; Cho, S.-H.; Mariadoss, A.V.A.; Wang, M.-H. Metabolite profiling of methanolic extract of Gardenia jaminoides by LC-MS/MS and GC-MS and its anti-diabetic, and anti-oxidant activities. Pharmaceuticals 2021, 14, 102. [Google Scholar] [CrossRef]
- Karakaya, S.; Bingol, Z.; Koca, M.; Dagoglu, S.; Pınar, N.M.; Demirci, B.; Gulcin, İ.; Brestic, M.; Sytar, O. Identification of non-alkaloid natural compounds of Angelica purpurascens (Avé-Lall.) Gilli. (Apiaceae) with cholinesterase and carbonic anhydrase inhibition potential. Saudi Pharm. J. 2020, 28, 1–14. [Google Scholar] [CrossRef]
- Gutiérrez-Grijalva, E.P.; Picos-Salas, M.A.; Leyva-López, N.; Criollo-Mendoza, M.S.; Vazquez-Olivo, G.; Heredia, J.B. Flavonoids and phenolic acids from oregano: Occurrence, biological activity and health benefits. Plants 2017, 7, 2. [Google Scholar] [CrossRef]
- Servili, M.; Sordini, B.; Esposto, S.; Urbani, S.; Veneziani, G.; Maio, I.D.; Selvaggini, R.; Taticchi, A. Biological activities of phenolic compounds of extra virgin olive oil. Antioxidants 2013, 3, 1–23. [Google Scholar] [CrossRef] [PubMed]
- Basit, A.; Ahmad, S.; Naeem, A.; Usman, M.; Ahmed, I.; Shahzad, M.N. Chemical profiling of Justicia vahlii Roth.(Acanthaceae) using UPLC-QTOF-MS and GC-MS analysis and evaluation of acute oral toxicity, antineuropathic and antioxidant activities. J. Ethnopharmacol. 2022, 287, 114942. [Google Scholar] [CrossRef] [PubMed]
- Widiyarti, G.; Fitrianingsih, W. Phytochemical constituents and free radical scavenging activity of Madang Gatal (Schima wallichii) Choisy stem bark. Pharmacogn. J. 2019, 11. [Google Scholar] [CrossRef]
- Karthikeyan, S.C.; Velmurugan, S.; Donio, M.B.S.; Michaelbabu, M.; Citarasu, T. Studies on the antimicrobial potential and structural characterization of fatty acids extracted from Sydney rock oyster Saccostrea glomerata. Ann. Clin. Microbiol. Antimicrob. 2014, 13, 332. [Google Scholar] [CrossRef]
- Yáñez, D.A.C.; Gagneten, M.; Leiva, G.E.; Malec, L.S. Antioxidant activity developed at the different stages of Maillard reaction with milk proteins. LWT 2018, 89, 344–349. [Google Scholar] [CrossRef]
- Price, N.P.; Bischoff, K.M.; Leathers, T.D.; Cossé, A.A.; Manitchotpisit, P. Polyols, not sugars, determine the structural diversity of anti-streptococcal liamocins produced by Aureobasidium pullulans strain NRRL 50380. J. Antibiot. 2017, 70, 136–141. [Google Scholar] [CrossRef] [PubMed]
- Rubab, M.; Chelliah, R.; Saravanakumar, K.; Barathikannan, K.; Wei, S.; Kim, J.-R.; Yoo, D.; Wang, M.-H.; Oh, D.-H. Bioactive Potential of 2-Methoxy-4-vinylphenol and Benzofuran from Brassica oleracea L. var. capitate f, rubra (Red Cabbage) on Oxidative and Microbiological Stability of Beef Meat. Foods 2020, 9, 568. [Google Scholar] [CrossRef]
- Abu-Lafi, S.; Rayan, M.; Masalha, M.; Abu-Farich, B.; Al-Jaas, H.; Abu-Lafi, M.; Rayan, A. Phytochemical composition and biological activities of wild Scolymus maculatus L. Medicines 2019, 6, 53. [Google Scholar] [CrossRef]
- Kiruthiga, B.; Kumar, P.S. Potential impacts of various coastal locales on the phytochemical landscape in sand dune flora calotropis giganteawhite across the coleroon valley. Plant Arch. 2019, 19, 2173–2187. [Google Scholar]
- Solankee, A.; Prajapati, Y. An efficient synthesis of some new fluorine containing acetyl pyrazoline and isoxazole derivatives and their antibacterial activity. Rasayan J. Chem. 2009, 2, 23–27. [Google Scholar]
- Singh, B.R. Antibacterial activity of glycerol, lactose, maltose, mannitol, raffinose and xylose. Noto-Are Med. 2014, 17223318. [Google Scholar]
- Singla, P.; Luxami, V.; Paul, K. Synthesis, in vitro antitumor activity, dihydrofolate reductase inhibition, DNA intercalation and structure–activity relationship studies of 1, 3, 5-triazine analogues. Bioorg. Med. Chem. Lett. 2016, 26, 518–523. [Google Scholar] [CrossRef] [PubMed]
- Carballeira, N.M.; Reyes, E.D.; Sostre, A.; Rodríguez, A.D.; Rodríguez, J.L.; González, F.A. Identification of the novel antimicrobial fatty acid (5 Z, 9 Z)-14-methyl-5, 9-pentadecadienoic acid in Eunicea succinea. J. Nat. Prod. 1997, 60, 502–504. [Google Scholar] [CrossRef]
- Larbie, C. Tetrapleura tetraptera of Ghanaian origin: Phytochemistry, antioxidant and antimicrobial activity of extracts of plant parts. J. Pharm. Res. Int. 2020, 32, 78–96. [Google Scholar]
- Fadipe, L.A.; Haruna, A.; Mohammed, I. Antibacterial activity of 1, 2-benzenedicarboxylic acid, dioctyl ester isolated from the ethyl acetate soluble sub-portion of the unripe fruits of Nauclea latifolia. 2014. [Google Scholar]
- Boadu, A.; Nlooto, M.; Karpoormath, R. Spondias mombin: In Silico Screening of 1, 2-Benzenedicarboxylic Acid, Butyl 2-Methylpropyl Ester (Fragment of Geraniin) as Anti-Marburg virus agent. Authorea Prepr. 2022. [Google Scholar]
- Harper, D.; Gilbert, R.; O’Connor, T.; Kinchington, D.; Mahmood, N.; Mcllhinney, R.; Jeffries, D. Antiviral activity of 2-hydroxy fatty acids. Antivir. Chem. Chemother. 1996, 7, 138–141. [Google Scholar] [CrossRef][Green Version]
- Vijayakumar, S.; Divya, M.; Vaseeharan, B.; Chen, J.; Biruntha, M.; Silva, L.P.; Durán-Lara, E.F.; Shreema, K.; Ranjan, S.; Dasgupta, N. Biological Compound Capping of Silver Nanoparticle with the Seed Extracts of Blackcumin (Nigella sativa): A Potential Antibacterial, Antidiabetic, Anti-inflammatory, and Antioxidant. J. Inorg. Organomet. Polym. Mater. 2021, 31, 624–635. [Google Scholar] [CrossRef]
- Al-Hajj, N.Q.M.; Sharif, H.R.; Aboshora, W.; Wang, H. In vitro and in vivo evaluation of antidiabetic activity of leaf essential oil of Pulicaria inuloides-Asteraceae. 2016. [Google Scholar] [CrossRef]
- Bu, T.; Liu, M.; Zheng, L.; Guo, Y.; Lin, X. α-glucosidase inhibition and the in vivo hypoglycemic effect of butyl-isobutyl-phthalate derived from the Laminaria japonica rhizoid. Phytother. Res. 2010, 24, 1588–1591. [Google Scholar] [CrossRef] [PubMed]
- Emmanuel, O.; Uche, M.E.; Dike, E.D.; Etumnu, L.R.; Ugbogu, O.C.; Ugbogu, E.A. A review on Garcinia kola Heckel: Traditional uses, phytochemistry, pharmacological activities, and toxicology. Biomarkers 2021, 27, 101–117. [Google Scholar] [CrossRef]
- Reddy, G.A. Synthesis and Evaluation of Newer Quinoline Derivatives of Thiazolidinediones For Their Antidiabetic Activity l. Srikanth, n. Raghunandan1, p. Srinivas2 and g. Reddy. Available online: https://citeseerx.ist.psu.edu/document?repid=rep1&type=pdf&doi=3d403a7e4ab106153263a65f51de7597ad26a796 (accessed on 17 November 2022).
- Abbirami, E.; Selvakumar, M.; Dinesh Kumar, L.; Guna, R.; Sivasudha, T. Identification of novel drug-like compounds from Momordica cymbalaria as PPAR-γ agonists: A molecular docking study. AJEAT 2019, 8, 71–74. [Google Scholar] [CrossRef]
- Wang, J.C.; Hu, S.H.; Wang, J.T.; Chen, K.S.; Chia, Y.C. Hypoglycemic effect of extract of Hericium erinaceus. J. Sci. Food Agric. 2005, 85, 641–646. [Google Scholar] [CrossRef]
- Bharti, S.K.; Krishnan, S.; Kumar, A.; Kumar, A. Antidiabetic phytoconstituents and their mode of action on metabolic pathways. Ther. Adv. Endocrinol. Metab. 2018, 9, 81–100. [Google Scholar] [CrossRef] [PubMed]
- Zuo, A.-R.; Dong, H.-H.; Yu, Y.-Y.; Shu, Q.-L.; Zheng, L.-X.; Yu, X.-Y.; Cao, S.-W. The antityrosinase and antioxidant activities of flavonoids dominated by the number and location of phenolic hydroxyl groups. Chin. Med. 2018, 13, 51. [Google Scholar] [CrossRef] [PubMed]
- Younis, M.M.; Ayoub, I.M.; Mostafa, N.M.; El Hassab, M.A.; Eldehna, W.M.; Al-Rashood, S.T.; Eldahshan, O.A. GC/MS Profiling, Anti-Collagenase, Anti-Elastase, Anti-Tyrosinase and Anti-Hyaluronidase Activities of a Stenocarpus sinuatus Leaves Extract. Plants 2022, 11, 918. [Google Scholar] [CrossRef] [PubMed]
- Khurshid, U.; Ahmad, S.; Rehman, T.; Arshad, M.A.; Pervaiz, I.; Saba, S. GC-MS analysis, DPPH & enzyme inhibition assays of Trianthema triquetra Rottl. and Willd. growing in Pakistan. Lat. Am. J. Pharm. 2019, 38, 1181–1187. [Google Scholar]
- Saeki, H.; Oikawa, A. Effects of pH and type of sugar in the medium on tyrosinase activity in cultured melanoma cells. J. Cell. Physiol. 1978, 94, 139–145. [Google Scholar] [CrossRef]
- Nguyen, D.; Nguyen, D.H.; Hwa-La, L.; Lee, H.-B.; Shin, J.-H.; Kim, E.-K. Inhibition of melanogenesis by dioctyl phthalate isolated from Nigella glandulifera Freyn. J. Microbiol. Biotechnol. 2007, 17, 1585–1590. [Google Scholar]
- Barker, A.J.; Gibson, K.H.; Grundy, W.; Godfrey, A.A.; Barlow, J.J.; Healy, M.P.; Woodburn, J.R.; Ashton, S.E.; Curry, B.J.; Scarlett, L. Studies leading to the identification of ZD1839 (Iressa™): An orally active, selective epidermal growth factor receptor tyrosine kinase inhibitor targeted to the treatment of cancer. Bioorg. Med. Chem. Lett. 2001, 11, 1911–1914. [Google Scholar] [CrossRef]
- Fukai, S.; Tanimoto, S.; Maeda, A.; Fukuda, H.; Okada, Y.; Nomura, M. Pharmacological activity of compounds extracted from persimmon peel (Diospyros kaki THUNB.). J. Oleo Sci. 2009, 58, 213–219. [Google Scholar] [CrossRef]
- Titan, S.M.; Venturini, G.; Padilha, K.; Goulart, A.C.; Lotufo, P.A.; Bensenor, I.J.; Krieger, J.E.; Thadhani, R.I.; Rhee, E.P.; Pereira, A.C. Metabolomics biomarkers and the risk of overall mortality and ESRD in CKD: Results from the Progredir Cohort. PLoS ONE 2019, 14, e0213764. [Google Scholar] [CrossRef]
- Monroy, A.; Lithgow, G.J.; Alavez, S. Curcumin and neurodegenerative diseases. Biofactors 2013, 39, 122–132. [Google Scholar] [CrossRef] [PubMed]
- Barbosa, M.; Valentão, P.; Andrade, P.B. Bioactive compounds from macroalgae in the new millennium: Implications for neurodegenerative diseases. Mar. Drugs 2014, 12, 4934–4972. [Google Scholar] [CrossRef] [PubMed]
- Figueiredo-González, M.; Reboredo-Rodríguez, P.; González-Barreiro, C.; Carrasco-Pancorbo, A.; Simal-Gándara, J.; Cancho-Grande, B. Nutraceutical potential of phenolics from ‘brava’ and ‘mansa’ extra-virgin olive oils on the inhibition of enzymes associated to neurodegenerative disorders in comparison with those of ‘picual’ and ‘cornicabra’. Molecules 2018, 23, 722. [Google Scholar] [CrossRef] [PubMed]
- Mah, S.H.; Teh, S.S.; Ee, G.C.L. Anti-inflammatory, anti-cholinergic and cytotoxic effects of Sida rhombifolia. Pharm. Biol. 2017, 55, 920–928. [Google Scholar] [CrossRef]
- Kamireddy, K.; Chinnu, S.; Priyanka, P.; Rajini, P.; Giridhar, P. Neuroprotective effect of Decalepis hamiltonii aqueous root extract and purified 2-hydroxy-4-methoxy benzaldehyde on 6-OHDA induced neurotoxicity in Caenorhabditis elegans. Biomed. Pharmacother. 2018, 105, 997–1005. [Google Scholar] [CrossRef] [PubMed]
- Maqbool, M.; Manral, A.; Jameel, E.; Kumar, J.; Saini, V.; Shandilya, A.; Tiwari, M.; Hoda, N.; Jayaram, B. Development of cyanopyridine–triazine hybrids as lead multitarget anti-Alzheimer agents. Bioorg. Med. Chem. 2016, 24, 2777–2788. [Google Scholar] [CrossRef] [PubMed]
- Cho, Y.-R.; Chang, J.-Y.; Chang, H.-C. Production of γ-Aminobutyric Acid (GABA) by Lactobacillus buchneri isolated from Kimchi and its neuroprotective effect on neuronal cells. J. Microbiol. Biotechnol. 2007, 17, 104–109. [Google Scholar]
- Feng, W.; Wu, X.; Mao, G.; Zhao, T.; Wang, W.; Chen, Y.; Zhang, M.; Yang, L.; Wu, X. Neurological effects of subchronic exposure to dioctyl phthalate (DOP), lead, and arsenic, individual and mixtures, in immature mice. Environ. Sci. Pollut. Res. 2020, 27, 9247–9260. [Google Scholar] [CrossRef]
- Nipun, T.S.; Khatib, A.; Ibrahim, Z.; Ahmed, Q.U.; Redzwan, I.E.; Primaharinastiti, R.; Saiman, M.Z.; Fairuza, R.; Widyaningsih, T.D.; AlAjmi, M.F. GC-MS-and NMR-Based Metabolomics and Molecular Docking Reveal the Potential Alpha-Glucosidase Inhibitors from Psychotria malayana Jack Leaves. Pharmaceuticals 2021, 14, 978. [Google Scholar] [CrossRef] [PubMed]
- Chen, D.; Oezguen, N.; Urvil, P.; Ferguson, C.; Dann, S.M.; Savidge, T.C. Regulation of protein-ligand binding affinity by hydrogen bond pairing. Sci. Adv. 2016, 2, e1501240. [Google Scholar] [CrossRef]
- Lipinski, C.A. Lead-and drug-like compounds: The rule-of-five revolution. Drug Discov. Today Technol. 2004, 1, 337–341. [Google Scholar] [CrossRef] [PubMed]
| Phytochemical Class | Test Carried Out [19] | Results |
|---|---|---|
| Primary | ||
| Carbohydrates | Molisch’s test | +++ |
| Amino acids | Ninhydrin test | +++ |
| Secondary | ||
| Alkaloids | Dragendroff’s test | ++ |
| Tannins | Lead acetate test | +++ |
| Polyphenols | Ferric chloride test | +++ |
| Flavonoids | Alkaline reagent test | +++ |
| Saponins | Froth test | ++ |
| Bioactive Content | Antioxidant Activity (IC50) | ||
|---|---|---|---|
| TPC (mg GAE/g) | TFC (mg QE/g) | DPPH (mg/mL) | FRAP (mg/mL) |
| 119.6 ± 0.12 | 45.5 ± 0.19 | 0.356 ± 0.02 | 0.234 ± 0.03 |
| Tested Strains | Tested Extract Conc. (mg/mL) | Tested Extract Zone of Inhibition (mm) | Standard: Amoxicillin + Clavulanic Acid (1 mg/mL) Zone of Inhibition (mm) |
|---|---|---|---|
| Gram-Positive | |||
| Bacillus subtilis | 5 | 4 | 22 |
| 10 | 7 | ||
| 20 | 9 | ||
| Bacillus pumilus | 5 | N/A | 23 |
| 10 | 7 | ||
| 20 | 14 | ||
| Staphylococcus aureus | 5 | N/A | 22 |
| 10 | 12 | ||
| 20 | 16 | ||
| Staphylococcus epidermidis | 5 | N/A | 24 |
| 10 | N/A | ||
| 20 | N/A | ||
| Micrococcus luteus | 5 | 5 | 24 |
| 10 | 9 | ||
| 20 | 16 | ||
| Pseudomonas aeruginosa | 5 | 6 | NA |
| 10 | 10 | ||
| 20 | 17 | ||
| Gram-Negative | |||
| Escherichia coli | 5 | N/A | 23 |
| 10 | N/A | ||
| 20 | N/A | ||
| Bordetella bronchiseptica | 5 | N/A | 24 |
| 10 | 7 | ||
| 20 | 12 |
| Strains | Hemagglutination Titer Count | ||
|---|---|---|---|
| Control | Standard (Acyclovir) | Z. pentandra | |
| H9 | 1024 | 0 | 0 |
| IBV | 1024 | 0 | 2 |
| NDV | 1024 | 0 | 4 |
| α-Glucosidase Inhibition | Acetylcholinesterase Inhibition | Tyrosinase Inhibition | |||
|---|---|---|---|---|---|
| Z. pentandra | Standard (Acarbose) | Z. pentandra | Standard (Eserine) | Z. pentandra | Standard (Kojic Acid) |
| 10.0 ± 0.08 | 5.87 ± 0.01 | 38.3 ± 0.08 | 1.21 ± 0.02 | 20.7 ± 0.07 | 1.04 ± 0.02 |
| Sr No. | Compounds | H-Bond Interacting Amino Acids | Binding Affinity (kcal/mol) |
|---|---|---|---|
| 1 | 2-hydroxy-n-(2-phenylethyl) benzamide | LYS A:242, GLY A:274 | −8.1 |
| 2 | Lactose | ALA A:270, ASN A: 275, ASN A:277, GLY A:274, PHE A:246, TYR A:249 | −7.1 |
| 3 | Acarbose (standard) | GLN A:392, LYS A:395, THR A:448, PHE A:282, SER A:145 | −8.1 |
| Sr No. | Compounds | H-Bond Interacting Amino Acids | Binding Affinity (kcal/mol) |
|---|---|---|---|
| 1 | γ-sitosterol | N/A | −11.5 |
| 2 | 2-hydroxy-n-(2 phenylethyl)benzamide | GLY B:121, TYR B:124 | −9.4 |
| 3 | Eserin (standard) | TRP B:286 | −8.4 |
| Sr No. | Compounds | H-Bond Interacting Amino Acids | Binding Affinity (kcal/mol) |
|---|---|---|---|
| 1 | 2-hydroxy-n-(2-phenylethyl)benzamide | ASN A:205 | −7.2 |
| 2 | γ-sitosterol | N/A | −6.9 |
| 3 | Kojic acid (standard) | GLU A:195, HIS A:60 | −5.4 |
| Sr No. | Best-Docked Compounds | Lipinski’s Rule | Solubility | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| HBD | HBA | MWT | Lipophilicity | M.R | LR | ESOL Class | Ali Class | Silicos-IT Class | ||
| 1 | 2-hydroxy-n-(2-phenylethyl)benzamide | 2 | 4 | 166.13 | 0.84 | 40.36 | 0 | Very soluble | Very soluble | Soluble |
| 2 | 1,2-benzenedicarboxylic acid | 2 | 2 | 241.29 | 2.71 | 70.76 | 0 | Soluble | Moderately soluble | Moderately soluble |
| 3 | [1,3] diazepan-2,4-dione | 2 | 2 | 128.13 | −0.35 | 38.26 | 0 | Highly soluble | Highly soluble | Soluble |
| 4 | Lactose | 8 | 11 | 342.3 | −3.84 | 69.35 | 2 | Highly soluble | Highly soluble | Soluble |
| 5 | Tricyclo[4.3.1.1(3,8)]undecane-1-carboxylic acid | 1 | 2 | 194.27 | 2.51 | 54.97 | 0 | Soluble | Soluble | Soluble |
| 6 | cis-(−)-carvone-5,6-oxide | 0 | 2 | 166.22 | 1.84 | 46.8 | 0 | Very soluble | Very soluble | Soluble |
| 7 | Phthalic acid, bis-7-methyloctyl ester | 0 | 4 | 418.61 | 6.7 | 125.91 | 1 | Poorly soluble | Poorly soluble | Poorly soluble |
| 8 | γ-sitosterol | 1 | 1 | 414.71 | 7.19 | 133.23 | 1 | Poorly soluble | Poorly soluble | Poorly soluble |
| 9 | Dioctyl phthalate | 0 | 4 | 390.56 | 6.3 | 116.3 | 1 | Poorly soluble | Poorly soluble | Poorly soluble |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shahid, A.; Khan, K.u.R.; Rao, H.; Aati, H.Y.; Sherif, A.E.; Khan, D.A.; Basit, A.; Umair, M.; Mueed, A.; Esatbeyoglu, T.; et al. Phytochemical Profiling of the Ethanolic Extract of Zaleya pentandra L. Jaffery and Its Biological Activities by In-Vitro Assays and In-Silico Molecular Docking. Appl. Sci. 2023, 13, 584. https://doi.org/10.3390/app13010584
Shahid A, Khan KuR, Rao H, Aati HY, Sherif AE, Khan DA, Basit A, Umair M, Mueed A, Esatbeyoglu T, et al. Phytochemical Profiling of the Ethanolic Extract of Zaleya pentandra L. Jaffery and Its Biological Activities by In-Vitro Assays and In-Silico Molecular Docking. Applied Sciences. 2023; 13(1):584. https://doi.org/10.3390/app13010584
Chicago/Turabian StyleShahid, Afia, Kashif ur Rehman Khan, Huma Rao, Hanan Y. Aati, Asmaa E. Sherif, Duraiz Ahmed Khan, Abdul Basit, Muhammad Umair, Abdul Mueed, Tuba Esatbeyoglu, and et al. 2023. "Phytochemical Profiling of the Ethanolic Extract of Zaleya pentandra L. Jaffery and Its Biological Activities by In-Vitro Assays and In-Silico Molecular Docking" Applied Sciences 13, no. 1: 584. https://doi.org/10.3390/app13010584
APA StyleShahid, A., Khan, K. u. R., Rao, H., Aati, H. Y., Sherif, A. E., Khan, D. A., Basit, A., Umair, M., Mueed, A., Esatbeyoglu, T., & Korma, S. A. (2023). Phytochemical Profiling of the Ethanolic Extract of Zaleya pentandra L. Jaffery and Its Biological Activities by In-Vitro Assays and In-Silico Molecular Docking. Applied Sciences, 13(1), 584. https://doi.org/10.3390/app13010584










