Development of a Novel Passive-Dynamic Custom AFO for Drop-Foot Patients: Design Principles, Manufacturing Technique, Mechanical Properties Characterization and Functional Evaluation
Abstract
:1. Introduction
2. Materials and Methods
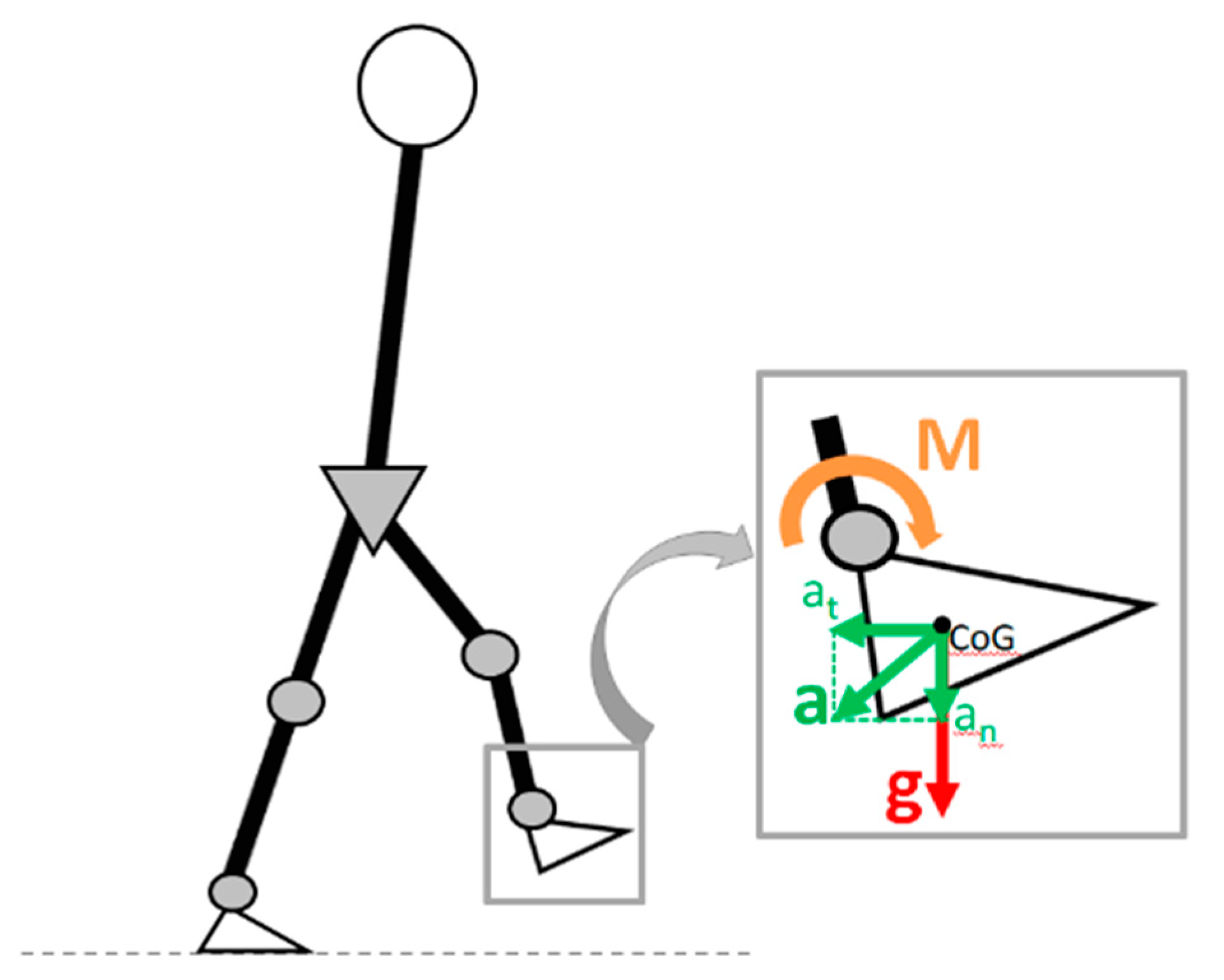
2.1. Custom PD-AFO Design and Production
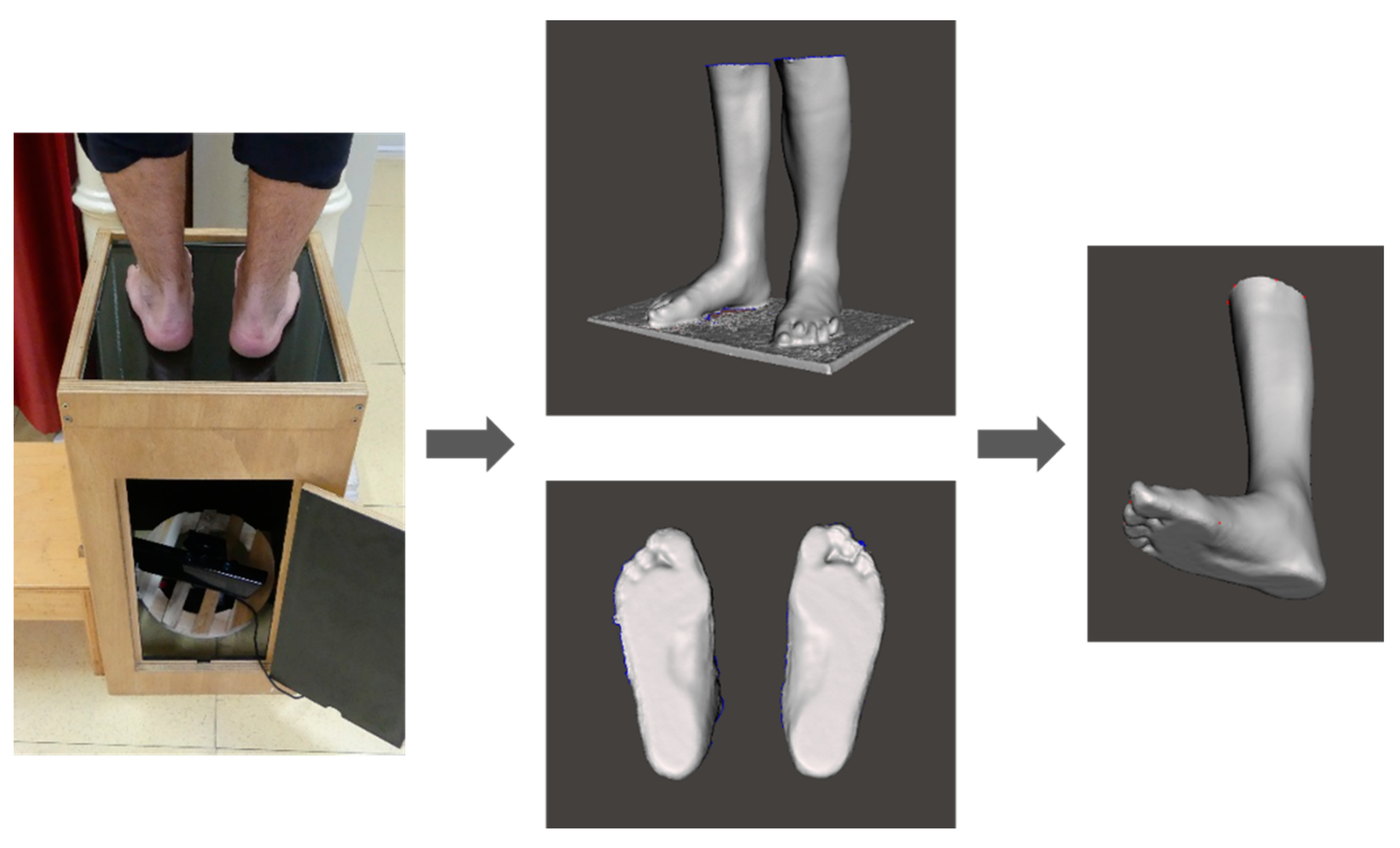
2.1.1. Foot and Leg Scanning
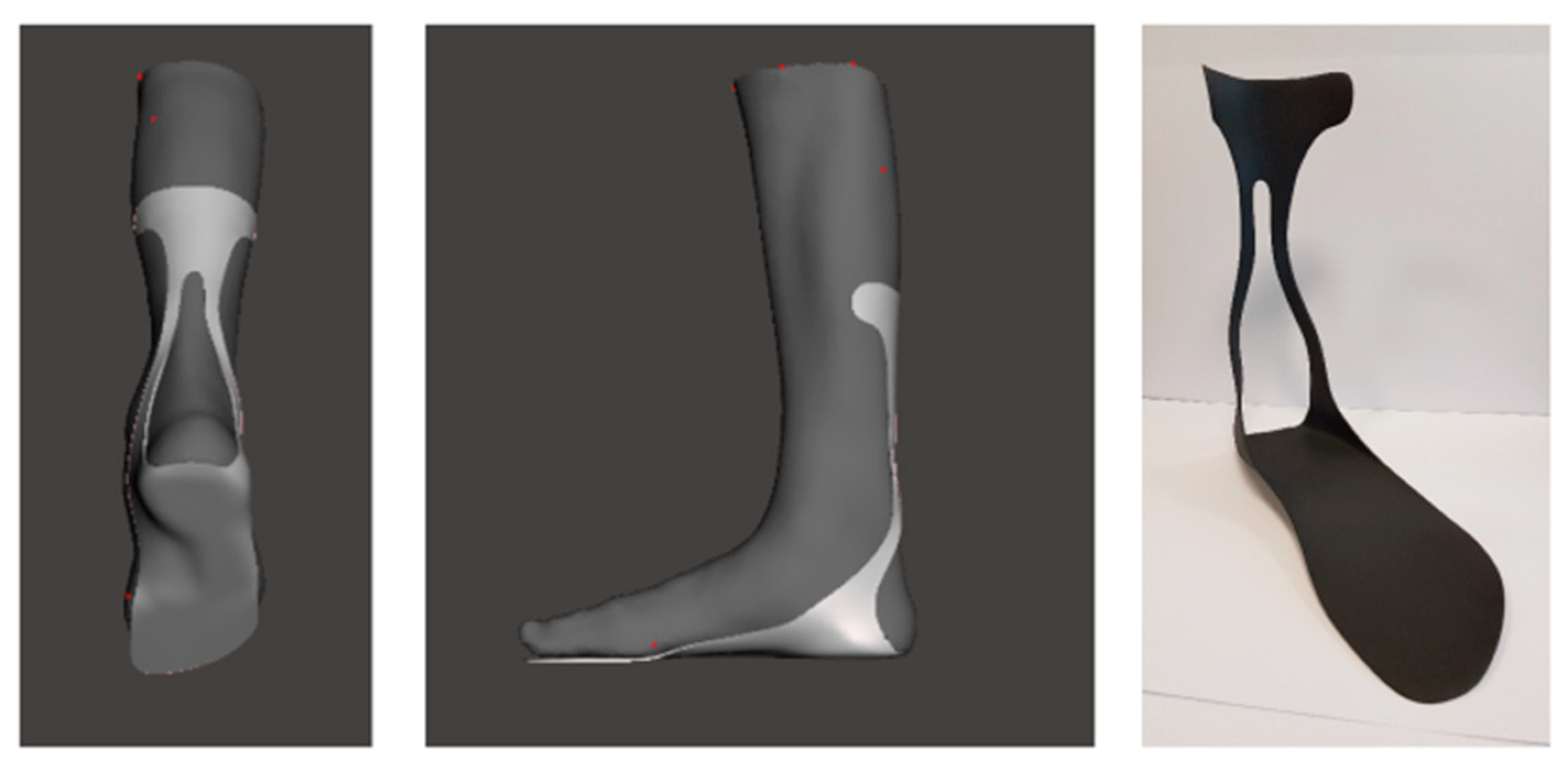
2.1.2. 3D Design
2.1.3. Additive Manufacturing
2.2. Pilot Study
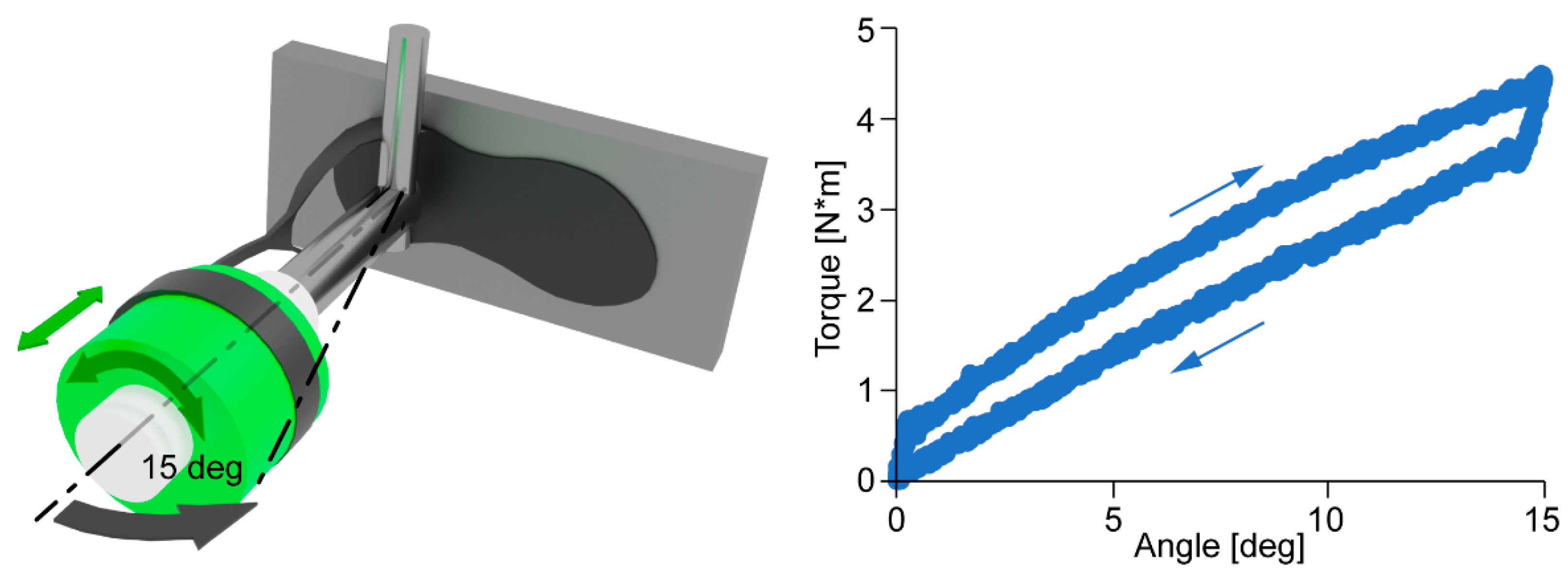
2.2.1. AFO Mechanical Properties Characterization
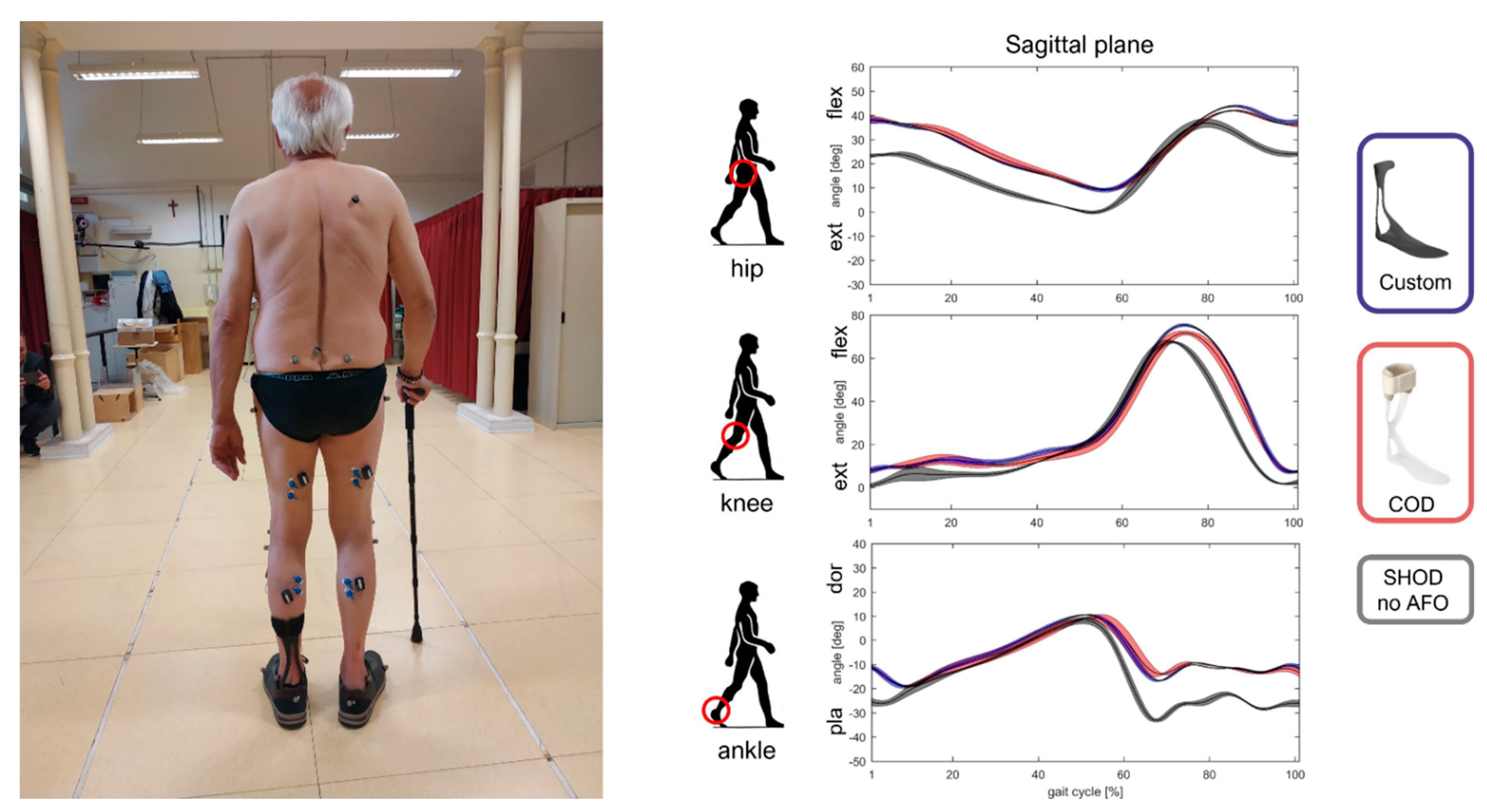
2.2.2. Functional and Comfort Evaluation
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Johnson, C.A.; Burridge, J.H.; Strike, P.W.; Wood, D.E.; Swain, I.D. The Effect of Combined Use of Botulinum Toxin Type A and Functional Electric Stimulation in the Treatment of Spastic Drop Foot after Stroke: A Preliminary Investigation. Arch. Phys. Med. Rehabil. 2004, 85, 902–909. [Google Scholar] [CrossRef] [PubMed]
- Winters, T.F.; Gage, J.R.; Hicks, R. Gait Patterns in Spastic Hemiplegia in Children and Young Adults. J. Bone Jt. Surgery. Am. Vol. 1987, 69, 437–441. [Google Scholar] [CrossRef] [Green Version]
- Barrios-Muriel, J.; Romero-Sánchez, F.; Alonso-Sánchez, F.J.; Salgado, D.R. Advances in Orthotic and Prosthetic Manufacturing: A Technology Review. Materials 2020, 13, 295. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Waterval, N.F.J.; Brehm, M.A.; Harlaar, J.; Nollet, F. Individual Stiffness Optimization of Dorsal Leaf Spring Ankle–Foot Orthoses in People with Calf Muscle Weakness Is Superior to Standard Bodyweight-Based Recommendations. J. Neuroeng. Rehabil. 2021, 18, 97. [Google Scholar] [CrossRef]
- Kerkum, Y.L.; Buizer, A.I.; van den Noort, J.C.; Becher, J.G.; Harlaar, J.; Brehm, M.A. The Effects of Varying Ankle Foot Orthosis Stiffness on Gait in Children with Spastic Cerebral Palsy Who Walk with Excessive Knee Flexion. PLoS ONE 2015, 10, e0142878. [Google Scholar] [CrossRef] [Green Version]
- Russell Esposito, E.; Blanck, R.V.; Harper, N.G.; Hsu, J.R.; Wilken, J.M. How Does Ankle-Foot Orthosis Stiffness Affect Gait in Patients with Lower Limb Salvage? Clin. Orthop. Relat. Res. 2014, 472, 3026–3035. [Google Scholar] [CrossRef] [Green Version]
- Dufek, J.S.; Neumann, E.S.; Hawkins, M.C.; O’Toole, B. Functional and Dynamic Response Characteristics of a Custom Composite Ankle Foot Orthosis for Charcot-Marie-Tooth Patients. Gait Posture 2014, 39, 308–313. [Google Scholar] [CrossRef]
- Bartonek, Å.; Eriksson, M.; Gutierrez-Farewik, E.M. Effects of Carbon Fibre Spring Orthoses on Gait in Ambulatory Children with Motor Disorders and Plantarflexor Weakness. Dev. Med. Child Neurol. 2007, 49, 615–620. [Google Scholar] [CrossRef]
- Meyns, P.; Kerkum, Y.L.; Brehm, M.A.; Becher, J.G.; Buizer, A.I.; Harlaar, J. Ankle Foot Orthoses in Cerebral Palsy: Effects of Ankle Stiffness on Trunk Kinematics, Gait Stability and Energy Cost of Walking. Eur. J. Paediatr. Neurol. 2020, 26, 68–74. [Google Scholar] [CrossRef]
- Creylman, V.; Muraru, L.; Pallari, J.; Vertommen, H.; Peeraer, L. Gait Assessment during the Initial Fitting of Customized Selective Laser Sintering Ankle Foot Orthoses in Subjects with Drop Foot. Prosthet. Orthot. Int. 2013, 37, 132–138. [Google Scholar] [CrossRef] [Green Version]
- Mavroidis, C.; Ranky, R.G.; Sivak, M.L.; Patritti, B.L.; DiPisa, J.; Caddle, A.; Gilhooly, K.; Govoni, L.; Sivak, S.; Lancia, M.; et al. Patient Specific Ankle-Foot Orthoses Using Rapid Prototyping. J. Neuroeng. Rehabil. 2011, 8, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lewallen, J.; Miedaner, J.; Amyx, S.; Sherman, J. Effect of Three Styles of Custom Ankle Foot Orthoses on the Gait of Stroke Patients While Walking on Level and Inclined Surfaces. J. Prosthet. Orthot. 2010, 22, 78–83. [Google Scholar] [CrossRef]
- Sienko Thomas, S.; Buckon, C.E.; Jakobson-Huston, S.; Sussman, M.D.; Aiona, M.D. Stair Locomotion in Children with Spastic Hemiplegia: The Impact of Three Different Ankle Foot Orthosis (AFOs) Configurations. Gait Posture 2002, 16, 180–187. [Google Scholar] [CrossRef]
- Waterval, N.F.J.; Nollet, F.; Harlaar, J.; Brehm, M.A. Modifying Ankle Foot Orthosis Stiffness in Patients with Calf Muscle Weakness: Gait Responses on Group and Individual Level. J. Neuroeng. Rehabil. 2019, 16, 147. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kerkum, Y.L.; Philippart, W.; Houdijk, H. The Effects of Footplate Stiffness on Push-off Power When Walking with Posterior Leaf Spring Ankle-Foot Orthoses. Clin. Biomech. 2021, 88, 105422. [Google Scholar] [CrossRef] [PubMed]
- Esposito, E.R.; Ruble, M.D.; Ikeda, A.J.; Wilken, J.M. The Effect of Custom Carbon Ankle-Foot Orthosis Alignment on Roll-over Shape and Center of Pressure Velocity. Prosthet. Orthot. Int. 2020, 45, 147–152. [Google Scholar] [CrossRef]
- Rogati, G.; Leardini, A.; Ortolani, M.; Caravaggi, P. Validation of a Novel Kinect-Based Device for 3D Scanning of the Foot Plantar Surface in Weight-Bearing. J. Foot Ankle Res. 2019, 12, 46. [Google Scholar] [CrossRef] [Green Version]
- Polkey, C.E. Book Reviews. In British Medical Bulletin, Aids to the Examination of the Peripheral Nervous System; Oxford Academic: Oxford, UK, 1977; Volume 33, p. 182. [Google Scholar]
- Bruening, D.; Richards, J.G. Skiing-Skating: Optimal Ankle Axis Position for Articulated Boots. Sports Biomech. 2005, 4, 215–225. [Google Scholar] [CrossRef]
- Leardini, A.; Sawacha, Z.; Paolini, G.; Ingrosso, S.; Nativo, R.; Benedetti, M.G. A New Anatomically Based Protocol for Gait Analysis in Children. Gait Posture 2007, 26, 560–571. [Google Scholar] [CrossRef]
- Grood, E.S.; Suntay, W.J. A Joint Coordinate System for the Clinical Description of Three-Dimensional Motions: Application to the Knee. J. Biomech. Eng. 1983, 105, 136–144. [Google Scholar] [CrossRef]
- Wu, G.; Siegler, S.; Allard, P.; Kirtley, C.; Leardini, A.; Rosenbaum, D.; Whittle, M.; D’Lima, D.D.; Cristofolini, L.; Witte, H.; et al. ISB Recommendation on Definitions of Joint Coordinate System of Various Joints for the Reporting of Human Joint Motion—Part I: Ankle, Hip, and Spine. International Society of Biomechanics. J. Biomech. 2002, 35, 543–548. [Google Scholar] [CrossRef]
- Kobayashi, T.; Leung, A.K.L.; Hutchins, S.W. Techniques to Measure Rigidity of Ankle-Foot Orthosis: A Review. J. Rehabil. Res. Dev. 2011, 48, 565–576. [Google Scholar] [CrossRef] [PubMed] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Caravaggi, P.; Zomparelli, A.; Rogati, G.; Baleani, M.; Fognani, R.; Cevolini, F.; Fanciullo, C.; Cinquepalmi, A.; Lullini, G.; Berti, L.; et al. Development of a Novel Passive-Dynamic Custom AFO for Drop-Foot Patients: Design Principles, Manufacturing Technique, Mechanical Properties Characterization and Functional Evaluation. Appl. Sci. 2022, 12, 4721. https://doi.org/10.3390/app12094721
Caravaggi P, Zomparelli A, Rogati G, Baleani M, Fognani R, Cevolini F, Fanciullo C, Cinquepalmi A, Lullini G, Berti L, et al. Development of a Novel Passive-Dynamic Custom AFO for Drop-Foot Patients: Design Principles, Manufacturing Technique, Mechanical Properties Characterization and Functional Evaluation. Applied Sciences. 2022; 12(9):4721. https://doi.org/10.3390/app12094721
Chicago/Turabian StyleCaravaggi, Paolo, Alessandro Zomparelli, Giulia Rogati, Massimiliano Baleani, Roberta Fognani, Franco Cevolini, Cristina Fanciullo, Arianna Cinquepalmi, Giada Lullini, Lisa Berti, and et al. 2022. "Development of a Novel Passive-Dynamic Custom AFO for Drop-Foot Patients: Design Principles, Manufacturing Technique, Mechanical Properties Characterization and Functional Evaluation" Applied Sciences 12, no. 9: 4721. https://doi.org/10.3390/app12094721
APA StyleCaravaggi, P., Zomparelli, A., Rogati, G., Baleani, M., Fognani, R., Cevolini, F., Fanciullo, C., Cinquepalmi, A., Lullini, G., Berti, L., & Leardini, A. (2022). Development of a Novel Passive-Dynamic Custom AFO for Drop-Foot Patients: Design Principles, Manufacturing Technique, Mechanical Properties Characterization and Functional Evaluation. Applied Sciences, 12(9), 4721. https://doi.org/10.3390/app12094721






