Abstract
The delivery of healthcare from a distance, also known as telemedicine, has evolved over the past 50 years, changing the way healthcare is delivered globally. Its integration into numerous domains has permitted high-quality care that transcends the obstacles of geographic distance, lack of access to health care providers, and cost. Ultrasound is an effective diagnostic tool and its application within telemedicine has advanced substantially in recent years, particularly in high-income settings and low-resource areas. The literature in Pubmed from 1960–2020 was assessed with the keywords “ultrasound”, “telemedicine”, “ultrasound remote”, and “tele-ultrasound” to conduct a SWOT analysis (strengths, weaknesses, opportunities, and threats). In addressing strengths and opportunities, we emphasized practical aspects, such as the usefulness of tele-ultrasound and the cost efficiency of it. Furthermore, aspects of medical education in tele-ultrasound were considered. When it came to weaknesses and threats, we focused on issues that may not be solved immediately, and that require careful consideration or further development, such as new software that is not yet available commercially.
1. Introduction
The term telemedicine was coined in the 1970s to describe the practice of delivering health care services through the use of information and communications technology, whereby geographic distance is not as constraining, as in the case of traditional medical practice. Telemedicine is not only used to exchange valid information for the diagnosis, treatment, and prevention of disease and injuries and research and evaluation, but also for the continuing the education of healthcare providers to advance individual and community health [1,2].
Telemedicine has been shown to improve access to healthcare and reduce costs, especially in areas with a limited healthcare infrastructure due to geographical barriers [3]. Recently, increased digitalization and the development of telehealth applications have finally reached the field of medical imaging. As telemedicine has evolved over the last few decades, ultrasound technology matured in parallel [4]. Ultrasound became a bedside tool in the 1990s that physicians, such as those who work in the emergency department, could use regularly because it is a fast, robust, and reliable way of determining a patient’s status at the outset of treatment. Tele-ultrasound is defined as the use of ultrasound with telecommunications and/or an additional instructor who is telemedically connected to the process. The utilization of tele-ultrasound has been rapidly increasing worldwide since the 1990s and is commonly used for emergency, abdominal, and obstetrical ultrasound by general practitioners in remote areas worldwide. One of the beneficiaries of this is other doctors, but in a broader sense, it benefits patients as well. Moreover, it can be a cost-saving measure as it eliminates both long transportation times and extra doctor visits. A lack of access to ultrasound doctors, despite technological advancements and mobile devices with high bandwidth that allow for seamless live-image transmission, is a concern in both low-income and high-income countries. Moreover, the main challenge in telemedicine remains an organizational one, knowing how and when to take advantage of the technology.
Tele-Ultrasound in a Historical Context
According to the World Health Organization (WHO), in clinical situations, medical imaging is needed to make a diagnosis in 20–30% of cases, and ultrasound and/or conventional radiography are sufficient for 80–90% of those cases. However, two thirds of the world population does not have any access to medical imaging [5].
The beginnings of tele-ultrasound date back to the era of space exploration in the 1960s, when the first remote ultrasound scans were carried out on astronauts with remote guidance from experts in the Mission Control Center [6] (Figure 1). Those ultrasound systems were capable of high-definition sonographic imaging for the cardiac, vascular, general, abdominal, thoracic, and musculoskeletal systems, among others (Ashot 2006).
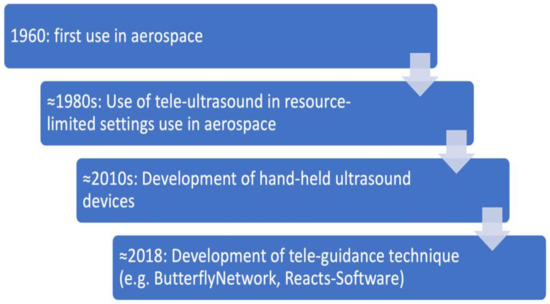
Figure 1.
Timeline of use of tele-ultrasound.
The technology remains relevant in aeronautics and recently several studies have assessed the use of ultrasound by non-physician crew members at the International Space Station, which entailed prior training in ultrasound [6,7,8,9,10].
From space, the focus has shifted to earth. Here, especially in remote areas in New Zealand and Sub-Saharan Africa, tele-ultrasound has proven successful. Focusing mainly on emergency ultrasound [11] and Point-Of-Care Ultrasound (POCUS), it has been shown that remotely-guided Focused Assessment with Sonography for Trauma (FAST) ultrasound examinations with minimally trained health care workers are possible and effective [12,13]. In obstetrics and gynecology, several successful prenatal tele-ultrasound projects have been described in literature [14,15]. Many countries harbor only a small number of qualified fetal-medicine specialists who are capable of pre-natal ultrasound imaging, which does not adequately cover demand, but which is highly significant in diagnosing and preventing potential birth defects. Studies, mainly from remote areas such as rural Australia, have tried to identify the need for fetal therapy [16].
Tele-ultrasound performed in resource-limited settings can produce satisfactory images of diagnostic relevance which have an impact on medical treatment and outcomes [17].
2. Materials and Methods
A systematic review of the literature was conducted. The databases searched were Medline (1950 to October 2020) and Embase (1980 to October 2020), the Cochrane Library, all sections, and the Web of Science with Conference Proceedings (1970 to 2020). The searches were not limited by language. Auto-alerts in Medline were also run during the course of the review. Reference lists of relevant articles were also checked.
All relevant randomized controlled trials (RCTs) or quasi-RCTs were included. Due to the small number of RCTs, we also included nonrandomized studies (NRSs). Prospective observational studies with controls, retrospective matched-pair studies, and comparative studies from well-defined registries/databases were also included.
The terms to be examined were “ultrasound”, “telemedicine”, “ultrasound remote”, and “tele-ultrasound”, which helped to complete a SWOT (strengths, weaknesses, opportunities, threats) analysis (Figure 2).
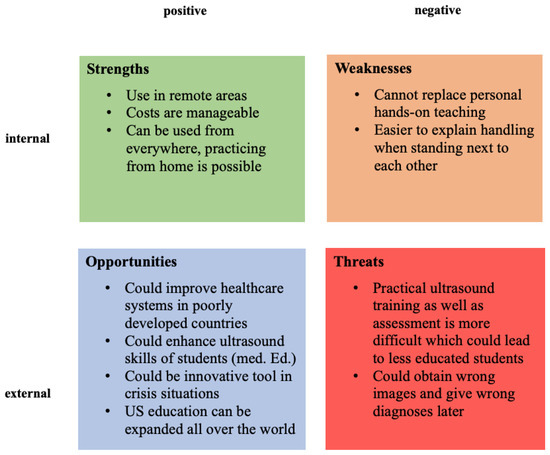
Figure 2.
SWOT analysis of the use of tele-ultrasound.
Strengths and opportunities were considered based on practical aspects such as the practicality of using tele-ultrasound and cost efficiency. Additionally, aspects of medical education related to tele-ultrasounds were discussed.
When we analyzed weaknesses and threats, we focused on issues that are unlikely to be resolved immediately and which may require thorough consideration or further development, such as new software that has not yet been commercially released. All articles were screened for positive statements on approval by a local ethics committee, adherence to guidelines for animal care, and/or obtaining informed consent.
The present study is a review of previously published studies, and institutional review board approval and patient consent were not necessary. Only human studies with a full text in English were assessed for inclusion. Studies without detailed methods and results sections were excluded.
3. Results
3.1. Practicality of Use
Tele-ultrasound can be used in urban as well as in rural areas. It can improve the healthcare system and patient outcomes, especially in under-resourced areas [17]. From the point of view of medical education, it can enhance ultrasound skills and establish a basic knowledge of ultrasound. By expanding this method with tele-applications, practical ultrasound could be taught anywhere in the world.
In times of pandemics, such as COVID-19, with social distancing regulations and isolation measures, it can help to ease the pressure on healthcare systems by providing diagnostic alternatives. Rapid technical development and competition in the field of medical software engineering have made the cost of tele-ultrasound manageable. Even low-cost, readily available tools such as web interfaces or commercial messenger tools can be used for tele-supported ultrasound, with the advantage of being independent of any special setting and providing the flexibility to perform ultrasound when and wherever it may be necessary [18]. Recently, new software applications have been introduced that support the teaching of knobology and handling of the probe. Thus, one can even practice at home, independently of any course sessions (Figure 3).
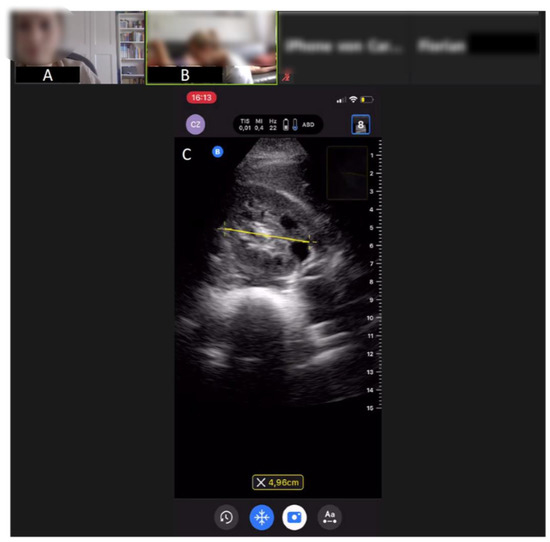
Figure 3.
Ultrasound image from a tele-didactic ultrasound teaching study on abdominal ultrasound from the medical faculty of the University of Bonn, Germany. (A) Peer tutor, (B) student exercising ultrasound on another student, (C) ultrasound image of the right kidney, which will be improved via tele-guidance by the peer tutor. An experienced ultrasonographer is also online in order to assist if any questions arise.
3.2. Cost Efficiency
In the scenario of real-time tele-ultrasound consultations and tele-education, savings in the conventional costs of patient transfer (e.g., transfer from GP to clinic) and human resources (e.g., clinical specialist in remote areas) need to be balanced against accruing telecommunication costs. An Australian study demonstrated that tele-ultrasound can result in a net saving of AUD 6340 and, at the same time, enabled almost four times the number of consultations than if the service had not been available [19]. In this study, a real-time fetal tele-ultrasound consultation service had been implemented and integrated into the daily clinical practice. Patients in Townsville could be assessed by subspecialists in Brisbane, 1500 km away, using the service. Ninety percent of the babies born during the 90 tele-ultrasound consultations for the first 71 patients showed good outcome data. The existence of all key anomalies and diagnoses was established in this study. Without telemedicine, 24 of the 71 patients would have been physically referred to Brisbane. Thus, this study underlined the cost effectiveness of the practice in a rural region.
As technology improves, wireless networks and cell phone access become more reliable, and companies such as Apple, Skype and many start-ups provide commercially available real-time audiovisual software in compliance with patient protection laws such as the American HIPAA (“Health Insurance Portability and Accountability Act”), making tele-ultrasound a feasible proposition.
Cost is a commonly expressed concern regarding tele-ultrasound with a special emphasis on the need for affordable tele-ultrasound platforms to make its use feasible. In the literature, numerous studies have used telemedicine platforms with open-source, low-cost, commercially available software such as over-the-counter hardware and low-cost portable ultrasound machines to minimize costs. Two studies explored the issue from the patients’ perspective and found that the introduction of tele-ultrasound was associated with lower out-of-pocket costs for the patient due to a reduced need for travel to larger medical centers with formal imaging capacity [15,20]. In another study, e-learning was found to be more effective than conventional education and superior to self-learning for enhancing novice learners’ ultrasound technical skills without increasing their workload [21].
3.3. Medical Education
In terms of medical education, e-learning can serve as both a self-study tool, as well as a teaching device, when used in conjunction with colleagues or supervisors. With the emergence of faster network technology (5G/6G) and mobile app platforms for live interaction and handheld ultrasound devices, tele-ultrasound and new fields of applications in pre-clinical settings and outpatient areas such as midwifery, geriatric facilities, and therapeutic use will be enabled with these developments [22].
The existing literature indicates that e-learning can provide an effective way of improving educational outcomes for healthcare professionals. Several studies have shown that tele-learning methods lead to similar results to traditional, face-to-face, teacher-centered instruction [23]. Especially when it comes to the field of tele-ultrasound, didactic concepts are particularly important. Theoretical ultrasound knowledge can be learned using a “flipped classroom”, a didactic format of blended learning, whereby students acquire knowledge at home and put it into practice during classes. In the past, attempts to offer targeted, individualized learning environments were abandoned due to the excessive expenditure of money. Nowadays, software-based, highly individualized learning is the norm rather than the exception and has shifted the paradigm. In this ongoing educational evolution, tele-ultrasound devices have several crucial advantages over traditional stationary ultrasound systems. Tele-ultrasound devices are connected to the internet, and interaction between every active participant is made easier, which simplifies communication and ideally speeds up the learning process. The internet, of course, provides access to a plethora of teaching and learning software. The combination of being continuously interconnected, elaborate software, and sufficient computing power has paved the way towards a personalized learning experience. The latest applications and web-based learning platforms can observe and track user profiles. In this way, individual learning behavior can be analyzed and optimized. Especially, theoretical ultrasound knowledge and knobology can be taught in this manner.
However, practical tele-guided ultrasound teaching and assessment comes with costs and challenges. In addition to purchasing the ultrasound equipment, the teacher and student need a video-based platform to show and see the student’s performance and the position of the transducer. Furthermore, the real-time sonogram must be streamed in order to give the student instructions during the training. However, the limited evidence base of this relatively new field of medical education demands further research to corroborate its efficacy in comparison with conventional teaching methods (Table 1).

Table 1.
Virtual ultrasound education requirements.
The most common components such as the handling and orientation of the probe, as well as image adjustments, may be evaluated with video footage that is recorded and reviewed afterwards or via a live stream.
These applications can be upgraded by augmented reality devices and experimental visual guidance tools that enhance the tele-guided experience and enable a more realistic method of learning [24]. Visual guidance is a computer-assisted method of demonstrating to an examiner the movement of the ultrasound probe as it is manipulated over a patient’s body toward a desired anatomical location.
The latest technical advancement in the field of tele-ultrasound is tele-guided ultrasound, which enhances and enables tele-educational tools in a more precise way. Tele-guided ultrasound means that someone is controlling the ultrasound probe and has access to all device settings remotely. For assessing not only image quality, but also the proficiency of the tele-mentored ultrasound image acquisition some studies have combined different tools.
Furthermore, progress is being made in educational tele-guidance tools. These serve as image quality indicators that provide real-time feedback from the physician on the healthcare worker’s scan technique. These tools aim to improve the quality and speed of the captured images. Thus, education in medical ultrasound can be expanded in remote areas if basic equipment (US machine, Internet, and telemedicine software) is available.
As an example of the use of tele-ultrasound in medical teaching, a tele-didactic ultrasound course was designed by Höhne et al. [25] in light of the current COVID-19 pandemic and the end of classical classroom teaching, which was previously considered vital in ultrasound training. The purpose of the study was to determine if online ultrasound teaching was effective. It also aimed to identify a suitable evaluation approach for evaluating US skills from afar. This pilot study demonstrated the effectiveness of online lectures in the context of ultrasound medical education. Furthermore, it illustrates that teleguided ultrasound training is feasible and should be addressed in medical schools, as well as the learning possibilities of tele-digital ultrasound.
3.4. Weaknesses and Threats
As far as weaknesses and threats are concerned, we analyzed issues that might need further development or deep consideration, such as new software that is not yet commercially available in comparison to traditional ultrasound (Table 2). Generally, in a tele-scenario with a remote expert, securing the multidimensional problem of “transducer angles”, “transducer position”, “patient body posture”, and “patient breathing state” may be difficult. Furthermore, the device settings, device type, and transducer type all have an impact on whether or not a representation is useful. As a result, the use of tele-ultrasound may be contingent not only on the technological infrastructure and individual abilities of the two linked examiners, but also on the capacity of the two remote persons to interact successfully as a team.

Table 2.
Advantages and disadvantages of conventional ultrasound versus tele-ultrasound.
3.5. Image Quality
A quality assessment tool was developed a few years ago to standardize sonographic B-images [26]. As an important feature, it attempts to quantify the sonographer’s influence with regard to the final image quality. This method can also be adopted for tele-ultrasound. Furthermore, the examiner’s skill, as well as the patient’s current state and cooperation, are all known to influence ultrasound imaging. Gallstones, for example, may only be scanned when the patient is in a precise inspiratory position and with extremely specific transducer angles and placements. As a result, even in the absence of tele-transmission, the imaging result is not always consistent. When two examiners look at the same patient, they will almost always produce different visuals and, in some situations, diagnoses. This general weakness naturally also has an influence on the use of ultrasound in telemedicine and must always be taken into account in all applications.
The latest developments in the field of telecommunication have paved the way for several attempts to test tele-ultrasound with mobile device application [22] or via web-based applications [27]. These studies have shown that commercially available video chat software can transmit high-quality and clinically useful ultrasound images. For nearly every anatomic location assessed in these studies, images obtained by means of this method were non-inferior to images obtained directly from a stationary ultrasound machine. There were also mobile ultrasound apps that went beyond simply projecting live images, with built-in tools to grade the images that study participants took and determined whether they passed or failed.
Data transfer rates have come a long way since the early stages of telemedicine two decades ago, when devices with a bandwidth of 2 Mbit/s were used successfully for obstetric tele-ultrasound [15]. Nowadays, the transmission of real-time ultrasound video footage to a remote iPhone using inexpensive technology is feasible, as shown in the literature. It can be accomplished without the loss of image quality and a minimal delay and works even with 3G mobile connection [28].
3.6. Safety of Data
As the value of personalized data increases and cheap data storage is abundantly available, telemedicine companies can record and analyze a complete set of parameters longitudinally in real-time, which is an unprecedented feat in the history of medicine. However, patients’ access to and control over these stored data are not always guaranteed. In Western societies, where people are wary of privacy violations, these developments should spark an intense public discourse, which seems to lag behind the staggering pace of the technological advancement.
In a tele-guided setting, there are several ways to document the obtained images and results. There are various ultrasound documentation programs on portable devices and guidelines on how to appropriately document an ultrasound examination [29]. Moreover, there are cloud-based monitoring systems that do not require bedside supervision and documentation, which may enhance the ability of physicians to study and document ultrasound images [30]. Data protection is an important issue related to these cloud-based documentation applications. Although recent cloud-based products comply with EU regulations regarding data privacy and protection, this remains a hot topic.
4. Artificial Intelligence and Tele-Ultrasound
Excellent-quality ultrasound images serve as the foundation for expert interpretation. Artificial intelligence (AI) is emerging to provide a means for autonomously gathering images, even for the uninitiated. Obstetricians have perfected the art of capturing and evaluating fetal images for pregnancy monitoring. Startup enterprises in the United States and Europe have acquired regulatory approval to advise inexperienced clinicians to take images for clinical purposes using AI guidance. The ultrasound probe is put on the patient after entering information such as the patient’s height, weight, and gender. The clinician is then instructed on how to move the probe (clockwise, counterclockwise, up, or down), and the picture is autocaptured as soon as the best image is detected.
There is still a scarcity of validation data for high-quality images acquired using this method. According to trials conducted by nurses with no previous echocardiography experience who used this equipment on hundreds of patients, high-quality video photographs may be obtained well over 90% of the time. That result holds true for images of organs that are not constantly moving, such as the heart, and should be more suited for AI algorithmic direction. Researchers are collecting massive amounts of ultrasound images from a range of patients to assist and drive algorithm development even further. These images will be linked to ground-truth diagnoses and verified clinical results. The implications of AI-assisted ultrasound guiding may be crucial for all practitioners in the future. For example, an emergency room doctor may snap a photograph of any region of a patient’s body and then send the video loop to a radiologist for interpretation. Deep learning algorithms for exact ultrasound interpretations are being investigated in the meantime; however, they are still in the early phases of development [31]. The advantages might be extended to rural regions, as well as middle- and low-income nations, where worker capacity or skill in image capture may be limited or non-existent, democratizing imaging technology. More widespread clinical use of smartphone ultrasonography has begun in rural Africa and India, and AI guidance for image capture may be adopted soon. In the COVID-19 outbreak, new uses of AI guidance have lately been seen [32]. Researchers are using deep learning approaches to develop algorithms for automating acquisition and severity evaluations to help in real-time clinical decision-making. If fully confirmed, the easily available objective image data might assist in the diagnosis, triage, and surveillance of seriously sick patients. In the future, a patient with heart failure may transmit to their doctor a clinical grade echo of their heart, whereas a person with acute stomach discomfort might obtain targeted photographs that indicated a kidney stone.
5. Discussion
The rapidly evolving technology will likely promote the widespread implementation of tele-ultrasound procedures, especially in remote areas and in the first-responder setting. Further investigation of real-time image transfer and communication paradigms in prehospital scenarios and practical applications is warranted. Pocket and other portable ultrasound machines are the most commonly used ultrasound devices for tele-ultrasound. The potential impact of tele-ultrasound is substantial when considering both the scope of clinical fields of application (e.g., respiratory failure, hemodynamic compromise, procedural guidance) and the number of stakeholders (e.g., patients, providers, health systems). Technologically speaking, ultrasound machines have become smaller, more portable, and durable, and the relative cost has decreased dramatically. Smartphones are ubiquitous, and dozens of software applications run seamlessly on them simultaneously. Therefore, smartphones are capable of functioning as affordable handheld telemedicine platforms. Finally, global connectivity is steadily increasing, particularly wireless cellular and internet access. These advances have made tele-ultrasound feasible and have given it a durable competitive advantage compared to conventional ultrasound, which will boost its application in the near future.
Nevertheless, tele-guided ultrasound education also carries some weaknesses and risks. No tele-ultrasound module can fully replace real hands-on learning experiences. Although one can try to teach the handling of the probe via tele-guidance, it is easier to do this physically next to a student. The digital distance, which provides some benefits, appears as a barrier that cannot be eradicated when using tele-ultrasound. Therefore, tele-ultrasound is an option for remote or poorly developed areas, as well as an innovative tool in crisis situations.
The practical usefulness of tele-ultrasound has become more entrenched and advanced in the medical setting in recent years. A distinction must be made between tele-ultrasound and the pure transmission of ultrasound images, which does not have the aspects of real-time data transmission with a corresponding second examiner. Particularly in the field of medical teaching, there is a specific difference between these two modalities.
Tele-ultrasound is on the advance, especially in the next few years, due to further progress in digitalization and technical miniaturization. Global pandemics, such as the current COVID-19 pandemic, have particularly marked and shaped this use of technology.
Author Contributions
Conceptualization, F.R. and V.S.S.; methodology, F.R.; software; investigation, F.R. and E.H.; resources, F.R., E.H. and D.D.; data curation, F.R., E.H. and V.S.S.; writing—original draft preparation, F.R.; writing—review and editing, E.H. and D.D.; visualization, F.R. and D.D.; supervision, V.S.S.; project administration, F.R. and V.S.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- WHO. A Health Telematics Policy in Support of WHO’s Health-For-All Strategy for Global Health Development-Report of the WHO Group Consultation on Health Telematics; World Health Organization: Geneva, Switzerland, 1997. [Google Scholar]
- Strehle, E.M.; Shabde, N. One hundred years of telemedicine: Does this new technology have a place in paediatrics? Arch. Dis. Child. 2006, 91, 956–959. [Google Scholar] [CrossRef]
- Bashshur, R.L. Telemedicine effects: Cost, quality, and access. J. Med. Syst. 1995, 19, 81–91. [Google Scholar] [CrossRef] [PubMed]
- Wootton, R. Recent advances: Telemedicine. BMJ 2001, 323, 557–560. [Google Scholar] [CrossRef] [PubMed]
- Smith, P.; Brebner, E. Tele-Ultrasound for Remote Areas. J. Telemed. Telecare 2002, 8, 80–81. [Google Scholar] [CrossRef] [PubMed]
- Sargsyan, A.E.; Hamilton, D.R.; Jones, J.A.; Melton, S.; Whitson, P.A.; Kirkpatrick, A.W.; Martin, D.; Dulchavsky, S.A. FAST at MACH 20: Clinical Ultrasound Aboard the International Space Station. J. Trauma Inj. Infect. Crit. Care 2005, 58, 35–39. [Google Scholar] [CrossRef] [PubMed]
- Ashot, E. The International Space Station Ultrasound Imaging Capability Overview for Prospective Users; NASA: Houston, TX, USA, 2006.
- Kwon, D.; Bouffard, J.A.; van Holsbeeck, M.; Sargsyan, A.E.; Hamilton, D.R.; Melton, S.L.; Dulchavsky, S.A. Battling fire and ice: Remote guidance ultrasound to diagnose injury on the International Space Station and the ice rink. Am. J. Surg. 2007, 193, 417–420. [Google Scholar] [CrossRef] [PubMed]
- Law, J.; Macbeth, P.B. Ultrasound: From Earth to Space. McGill J. Med. 2011, 13. [Google Scholar] [CrossRef]
- Marshburn, T.H.; Hadfield, C.A.; Sargsyan, A.E.; Garcia, K.; Ebert, D.; Dulchavsky, S.A. New Heights in Ultrasound: First Report of Spinal Ultrasound from the International Space Station. J. Emerg. Med. 2014, 46, 61–70. [Google Scholar] [CrossRef]
- Su, M.-J.; Ma, H.-M.; Ko, C.-I.; Chiang, W.-C.; Yang, C.-W.; Chen, S.-J.; Chen, R.; Chen, H.-S. Application of Tele-Ultrasound in Emergency Medical Services. Telemed. e-Health 2008, 14, 816–824. [Google Scholar] [CrossRef]
- Boniface, K.S.; Shokoohi, H.; Smith, E.R.; Scantlebury, K. Tele-ultrasound and paramedics: Real-time remote physician guidance of the Focused Assessment With Sonography for Trauma examination. Am. J. Emerg. Med. 2010, 29, 477–481. [Google Scholar] [CrossRef]
- Douglas, T.M.; Levine, A.R.; Olivieri, P.; McCurdy, M.T.; Papali, A.; Zubrow, M.T.; Rodick, K.M.; Hurley, J.M.; Verceles, A.C. Brief training increases nurses’ comfort using tele-ultrasound: A feasibility study. Intensiv. Crit. Care Nurs. 2018, 51, 45–49. [Google Scholar] [CrossRef]
- Ferlin, R.M.; Vaz-Oliani, D.M.; Ferreira, A.C.; Tristão, E.G.; Oliani, A.H. Tele-obstetric ultrasound: Analysis of first-trimester ultrasound images transmitted in realtime. J. Telemed. Telecare 2012, 18, 54–58. [Google Scholar] [CrossRef]
- Chan, F.Y.; Whitehall, J.; Hayes, L.; Taylor, A.; Soong, B.; Lessing, K.; Cincotta, R.; Cooper, D.; Stone, M.; Lee-Tannock, A.; et al. Minimum requirements for remote realtime fetal tele-ultrasound consultation. J. Telemed. Telecare 1999, 5, 171–176. [Google Scholar] [CrossRef]
- Soong, B.; Chan, F.Y.; Bloomfield, S.; Smith, M.; Watson, D. The fetal tele-ultrasound project in Queensland. Aust. Heal. Rev. 2002, 25, 67–73. [Google Scholar] [CrossRef]
- Britton, N.; Miller, M.A.; Safadi, S.; Siegel, A.; Levine, A.R.; McCurdy, M.T. Tele-Ultrasound in Resource-Limited Settings: A Systematic Review. Front. Public Health 2019, 7, 244. [Google Scholar] [CrossRef] [PubMed]
- Robertson, T.E.; Levine, A.R.; Verceles, A.C.; Buchner, J.A.; Lantry, J.H.; Papali, A.; Zubrow, M.T.; Colas, L.N.; Augustin, M.E.; McCurdy, M.T. Remote tele-mentored ultrasound for non-physician learners using FaceTime: A feasibility study in a low-income country. J. Crit. Care 2017, 40, 145–148. [Google Scholar] [CrossRef] [PubMed]
- Chan, F.Y.; Soong, B.; Watson, D.; Whitehall, J. Realtime fetal ultrasound by telemedicine in Queensland. A successful venture? J. Telemed. Telecare 2001, 7, 7–11. [Google Scholar] [CrossRef] [PubMed]
- Adambounou, K.; Adjenou, V.; Salam, A.P.; Farin, F.; N’Dakena, K.G.; Gbeassor, M.; Arbeille, P.; N’dakena, K.G. A Low-Cost Tele-Imaging Platform for Developing Countries. Front. Public Health 2014, 2, 135. [Google Scholar] [CrossRef]
- Suzuki, R.; Hui, J.; Loftsgard, T.O.; Riley, W.; Bushman, M.S. Does Tele-Education Work. In Point-Of-Care Ultrasound Training? A 3-Arm Randomized Trial Comparing Tele-Education, Conventional Education, And Self-Learning Methods; ATS Journals: New York, NY, USA, 2017; Volume 195, Available online: https://www.atsjournals.org/doi/abs/10.1164/ajrccm-conference.2017.195.1_MeetingAbstracts.A7295 (accessed on 17 December 2021).
- Levine, A.R.; Buchner, J.A.; Verceles, A.C.; Zubrow, M.T.; Mallemat, H.A.; Papali, A.; McCurdy, M.T. Ultrasound images transmitted via FaceTime are non-inferior to images on the ultrasound machine. J. Crit. Care 2016, 33, 51–55. [Google Scholar] [CrossRef]
- Tomlinson, J.; Shaw, T.; Munro, A.; Johnson, R.; Madden, D.L.; Phillips, R.; McGregor, D. How does tele-learning compare with other forms of education delivery? A systematic review of tele-learning educational outcomes for health professionals. N. South. Wales Public Health Bull. 2013, 24, 70–75. [Google Scholar] [CrossRef] [PubMed]
- Sheehan, F.H.; Ricci, M.A.; Murtagh, C.; Clark, H.; Bolson, E.L. Expert visual guidance of ultrasound for telemedicine. J. Telemed. Telecare 2010, 16, 77–82. [Google Scholar] [CrossRef]
- Höhne, E.; Recker, F.; Schmok, E.; Brossart, P.; Raupach, T.; Schäfer, V.S. Conception and Feasibility of a Digital Tele-Guided Abdomen, Thorax, and Thyroid Gland Ultrasound Course for Medical Students (TELUS study). Ultraschall Med. -Eur. J. Ultrasound 2021. [Google Scholar] [CrossRef] [PubMed]
- Bahner, D.P.; Adkins, E.J.; Nagel, R.; Way, D.; Werman, H.A.; Royall, N.A. Brightness Mode Quality Ultrasound Imaging Examination Technique (B-QUIET): Quantifying Quality in Ultrasound Imaging. J. Ultrasound Med. 2011, 30, 1649–1655. [Google Scholar] [CrossRef]
- Yoo, S.K.; Kim, D.K.; Jung, S.M.; Kim, E.-K.; Lim, J.S.; Kim, J.H. Performance of a Web-based, realtime, tele-ultrasound consultation system over high-speed commercial telecommunication lines. J. Telemed. Telecare 2004, 10, 175–179. [Google Scholar] [CrossRef] [PubMed]
- Liteplo, A.S.; Noble, V.E.; Attwood, B. Real-time video transmission of ultrasound images to an iPhone. Crit. Ultrasound J. 2010, 1, 105–110. [Google Scholar] [CrossRef][Green Version]
- Dormagen, J.B.; Gaarder, M.; Drolsum, A. Standardized cine-loop documentation in abdominal ultrasound facilitates offline image interpretation. Acta Radiol. 2015, 56, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Canty, D.J.; Vijayakumar, R.; Royse, C.F. Cloud-based supervision of training in focused cardiac ultrasound-A scalable solution? Australas. J. Ultrasound Med. 2019, 22, 40–44. [Google Scholar] [CrossRef] [PubMed]
- Komatsu, M.; Sakai, A.; Dozen, A.; Shozu, K.; Yasutomi, S.; Machino, H.; Asada, K.; Kaneko, S.; Hamamoto, R. Towards Clinical Application of Artificial Intelligence in Ultrasound Imaging. Biomedicines 2021, 9, 720. [Google Scholar] [CrossRef] [PubMed]
- Cheema, B.S.; Walter, J.; Narang, A.; Thomas, J.D. Artificial intelligence–enabled POCUS in the COVID-19 ICU: A new spin on cardiac ultrasound. Case Rep. 2021, 3, 258–263. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).