Herbst Appliance Reinforced with an Hybrid Hyrax Expander and Two Miniscrews in the Lower Arch: Case Report
Abstract
:1. Introduction
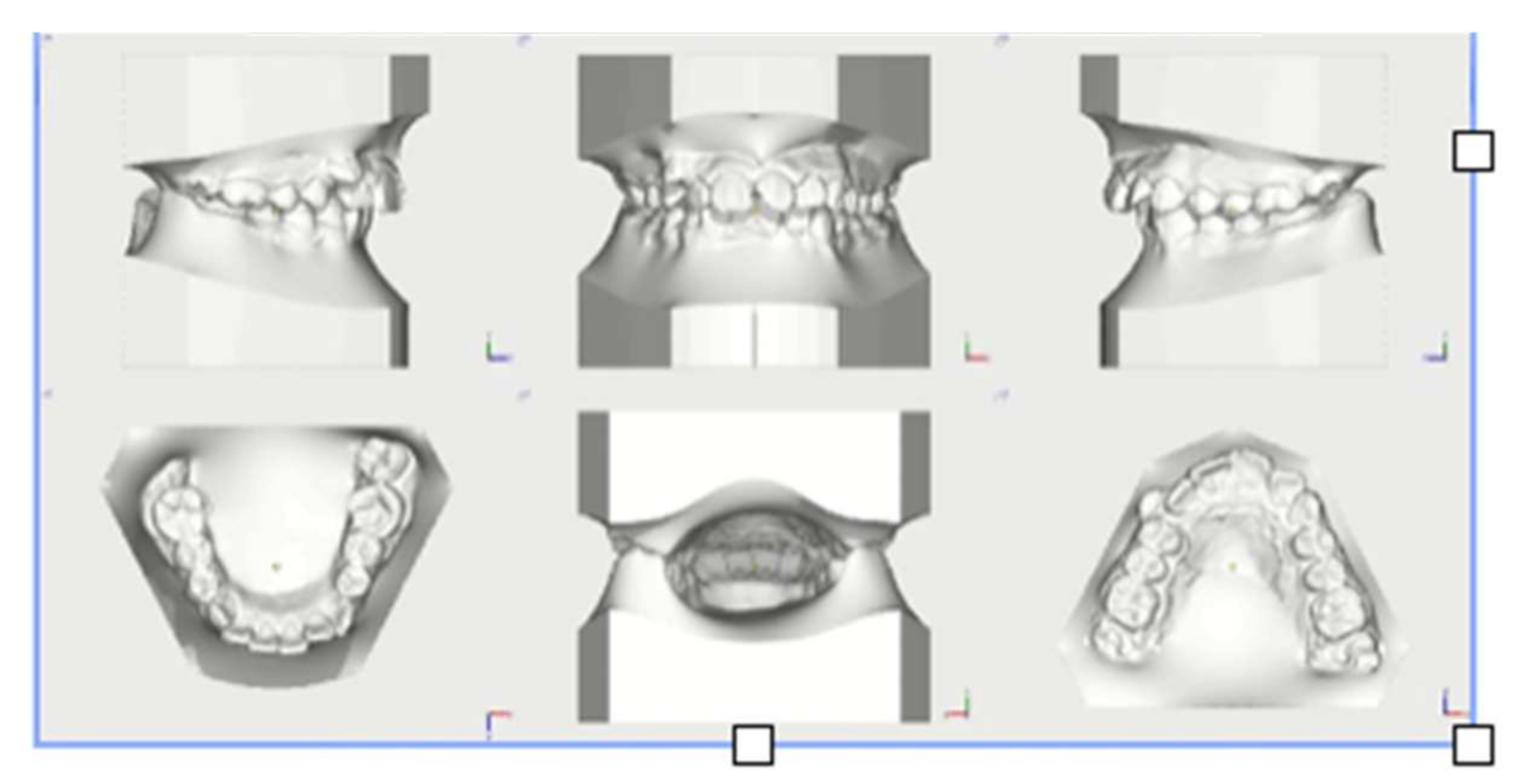
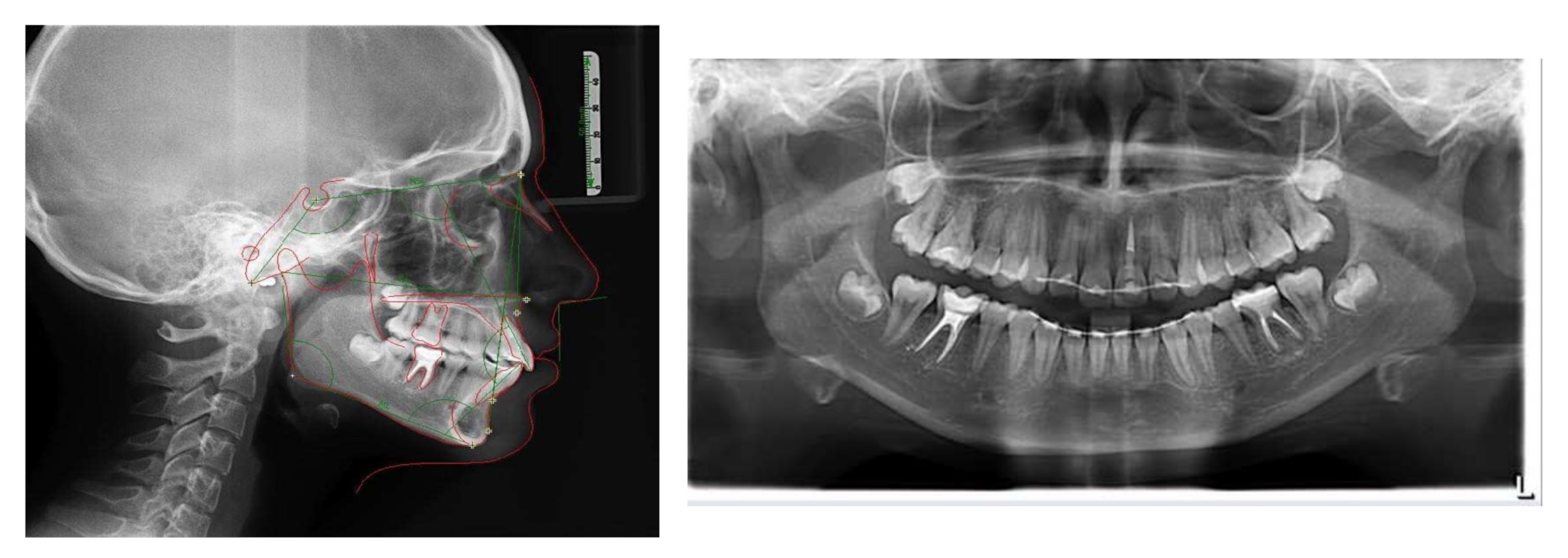
2. Diagnosis and Etiology
3. Treatment Objectives
- -
- Recovery of the sagittal and transverse dimensions of the upper arch
- -
- Correction of skeletal Class II
- -
- Space recovery for alignment 1.3
- -
- Resolution of Class II molar and canine relationships
- -
- Resolution of deep bite
- -
- Alignment and leveling, correction of the lower Spee curve
- -
- Occlusion finishing
- -
- Retention.
4. Treatment Alternatives
5. Treatment Progress
6. Treatment Results
7. Discussion
8. Summary and Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Proffit, W.R.; Fields, H.W.; Moray, L.J. Prevalence of malocclusion and orthodontic treatment need in the United States: Estimates from the NHANES-III survey. Int. J. Adult Orthod. Orthognath. Surg. 1998, 13, 97–106. [Google Scholar]
- Cozza, P.; Baccetti, T.; Franchi, L.; De Toffol, L.; McNamara, J.A., Jr. Mandibular changes produced by functional appliances in Class II malocclusion: A systematic review. Am. J. Orthod. Dentofac. Orthop. 2006, 129, 599.e1–599.e12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McNamara, J.A., Jr.; Brudon, W.L. Orthodontics and Dentofacial Orthopedics; Needham Press Inc.: Ann Arbor, MI, USA, 2001; p. 73. [Google Scholar]
- Lund, D.I.; Sandler, P.J. The effects of Twin Blocks: A prospective controlled study. Am. J. Orthod. Dentofac. Orthop. 1998, 113, 104–110. [Google Scholar] [CrossRef]
- Janson, G.R.; Toruño, J.L.A.; Martins, D.R.; Henriques, J.F.C.; De Freitas, M.R. Class II treatment effects of the Fränkel appliance. Eur. J. Orthod. 2003, 25, 301–309. [Google Scholar] [CrossRef] [Green Version]
- Pancherz, H. Treatment of Class II malocclusions by jumping the bite with the Herbst appliance: A cephalometric investigation. Am. J. Orthod. 1979, 76, 423–441. [Google Scholar] [CrossRef]
- Wigal, T.; Dischinger, T.; Martin, C.; Razmus, T.; Gunel, E.; Ngan, P. Stability of Class II treatment with an edgewise crowned Herbst appliance in the early mixed dentition: Skeletal and dental changes. Am. J. Orthod. 2011, 240, 211–223. [Google Scholar] [CrossRef] [PubMed]
- Ruf, S.; Pancherz, H. Herbst/multibracket appliance treatment of Class II division 1 malocclusions in early and late adulthood. A prospective cephalometric study of consecutively treated subjects. Eur. J. Orthod. 2006, 28, 352–360. [Google Scholar] [CrossRef] [Green Version]
- Pancherz, H.; Hansen, K. Mandibular anchorage in Herbst treatment. Eur. J. Orthod. 1988, 10, 149–164. [Google Scholar] [CrossRef] [PubMed]
- Gönner, U.; Özkan, V.; Jahn, E.; Toll, D.E. Effect of the MARA appliance on the position of the lower anteriors in children, adolescents and adults with Class II malocclusion. J. Orofac. Orthop./Fortschr. Kieferorthopädie 2007, 68, 397–412. [Google Scholar] [CrossRef] [PubMed]
- Servello, D.F.; Fallis, D.W.; Alvetro, L. Analysis of Class II patients, successfully treated with the straight-wire and Forsus appliances, based on cervical vertebral maturation status. Angle Orthod. 2015, 85, 80–86. [Google Scholar] [CrossRef]
- Manni, A.; Pasini, M.; Mazzotta, L.; Mutinelli, S.; Nuzzo, C.; Grassi, F.R. Comparison between an acrylic splint Herbst and an acrylic splint miniscrew-Herbst for mandibular incisors proclination control. Int. J. Dent. 2014, 2014, 173–187. [Google Scholar] [CrossRef] [Green Version]
- Manni, A.; Mutinelli, S.; Pasini, M.; Mazzotta, L.; Cozzani, M. Herbst appliance anchored to miniscrews with 2 types of ligation: Effectiveness in skeletal Class II treatment. Am. J. Orthod. Dentofac. Orthop. 2016, 149, 871–880. [Google Scholar] [CrossRef] [PubMed]
- Manni, A.; Migliorati, M.; Calzolari, C.; Silvestrini-Biavati, A. Herbst appliance anchored to miniscrews in the upper and lower arches vs standard Herbst: A pilot study. Am. J. Orthod. Dentofac. Orthop. 2019, 156, 617–625. [Google Scholar] [CrossRef] [PubMed]
- Manni, A.; Mutinelli, S.; Cerruto, C.; Cozzani, M. Influence of incisor position control on the mandibular response in growing patients with skeletal Class II malocclusion. Am. J. Orthod. Dentofac. Orthop. 2021, 159, 594–603. [Google Scholar] [CrossRef] [PubMed]
- Unal, T.; Celikoglu, M.; Candirli, C. Evaluation of the effects of skeletal anchoraged Forsus FRD using miniplates inserted on mandibular symphysis: A new approach for the treatment of Class II malocclusion. Angle Orthod. 2015, 85, 413–419. [Google Scholar] [CrossRef] [PubMed]
- Eissa, O.; El-Shennawy, M.; Gaballah, S.; El-Meehy, G.; El Bialy, T. Treatment outcomes of Class II malocclusion cases treated with miniscrew-anchored Forsus Fatigue Resistant Device: A randomized controlled trial. Angle Orthod. 2017, 87, 824–833. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bremen, J.; Ludwig, B.; Ruf, S. Anchorage loss due to Herbst mechanism-preventable through miniscrews? Eur. J. Orthod. 2015, 37, 462–466. [Google Scholar] [CrossRef] [Green Version]
- Tomblyn, T.; Rogers, M.; Martin, C.; Tremont, T.; Gunel, E.; Ngan, P. Cephalometric study of Class II Division 1 patients treated with an extended-duration, reinforced, banded Herbst appliance followed by fixed appliances. Am. J. Orthod. 2016, 150, 818–830. [Google Scholar] [CrossRef] [PubMed]
- Bock, N.C.; Gnandt, E.; Ruf, S. Occlusal stability after Herbst treatment of patients with retrognathic and prognathic facial types: A pilot study. Orofac. Orthop. 2016, 77, 160–167. [Google Scholar] [CrossRef] [PubMed]
- Souki, B.Q.; Vilefort, P.L.C.; Oliveira, D.D.; Andrade, I., Jr.; Ruellas, A.C.; Yatabe, M.S.; Nguyen, T.; Franchi, L.; McNamara, J.A., Jr.; Cevidanes, L.H.S. Three-dimensional skeletal mandibular changes associated with Herbst appliance treatment. Orthod. Craniofac. Res. 2017, 20, 111–118. [Google Scholar] [CrossRef]
- Van Laecken, R.; Martin, C.A.; Dischinger, T.; Razmus, T.; Ngan, P. Treatment effects of the edgewise Herbst appliance: A cephalometric and tomographic investigation. Am. J. Orthod. 2006, 130, 582–593. [Google Scholar] [CrossRef] [PubMed]
- Luzi, C.; Luzi, V.; Melsen, B. Mini-implants and the efficiency of Herbst treatment: A preliminary study. Prog. Orthod. 2013, 14, 21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Batista, K.B.; Lima, T. Herbst appliance with skeletal anchorage versus dental anchorage in adolescents with Class II malocclusion: Study protocol for a randomized controlled trial. Trials 2017, 18, 564. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ahn, H.W.; Kang, Y.G.; Jeong, H.J.; Park, Y.G. Palatal temporary skeletal anchorage devices (TSADs): What to know and how to do? Orthod. Craniofacial Res. 2021, 24, 66–74. [Google Scholar] [CrossRef]










| Saggittal Skeletal Relationships | ||||
|---|---|---|---|---|
| T0 | T1 | T2 | ||
| Maxillary Position S.N/A | 82° ± 3.5° | 81° | 82° | 81° |
| Mandible Position S.N/Pg | 80° ± 3.5° | 75° | 77° | 78° |
| A.N/Pg | 2° ± 2.5° | 6° | 6° | 2° |
| Vertical skeletal relationships | ||||
| S.N/ANS.PNS | 8° ± 3.0° | 8° | 8° | 9° |
| S.N/Go.Gn | 33° ± 2.5° | 29° | 30° | 32° |
| ANS.PNS/Go.Gn | 25° ± 6.0° | 22° | 22° | 23° |
| Dento-alveolar parameters | ||||
| +1/ANS.PNS | 110° ± 6.0° | 117° | 109° | 113° |
| −1/Go.GN | 94° ± 7.0° | 110° | 108° | 109° |
| −1/A.Pg (mm) | 2 +/−2 mm | 3 mm | 3 mm | 4 mm |
| Dental parameters | ||||
| Overjet (mm) | 3.5 ± 2.5 mm | 7 mm | 4 mm | 3 mm |
| Overbite (mm) | 2.5 ± 2.5 mm | 3 mm | 3 mm | 1 mm |
| 1s/1i | 132° ± 6.0° | 112° | 121° | 118° |
| Pancherz Analysis | |||
|---|---|---|---|
| T0 | T1 | T2 | |
| Is/OLp minus Ii/OLp | 7.2 mm | 4.2 mm | 2.8 mm |
| Ms/Olp minus Mi/OLp | 2.8 mm | 1.3 mm | −1.3 mm |
| Skeletal parameters | |||
| A/OLp | 68.1 mm | 72.6 mm | 71.5 mm |
| Pg/OLp | 64.8 mm | 70.3 mm | 70.0 mm |
| Cd/OLp | 10.4 mm | 9.5 mm | 10.4 mm |
| Pog/Olp + Cd/OLp | 75.2 mm | 79.9 mm | 80.5 mm |
| Dento-alveolar parameters | |||
| Is/OLp | 77.3 mm | 78.7 mm | 79.2 mm |
| Ii/OLp | 70.2 mm | 74.5 mm | 76.4 mm |
| Ms/OLp | 46.9 mm | 51.6 mm | 49.4 mm |
| Mi/OLp | 44.1 mm | 50.3 mm | 50.7 mm |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Migliorati, M.; Calzolari, C. Herbst Appliance Reinforced with an Hybrid Hyrax Expander and Two Miniscrews in the Lower Arch: Case Report. Appl. Sci. 2022, 12, 1552. https://doi.org/10.3390/app12031552
Migliorati M, Calzolari C. Herbst Appliance Reinforced with an Hybrid Hyrax Expander and Two Miniscrews in the Lower Arch: Case Report. Applied Sciences. 2022; 12(3):1552. https://doi.org/10.3390/app12031552
Chicago/Turabian StyleMigliorati, Marco, and Chiara Calzolari. 2022. "Herbst Appliance Reinforced with an Hybrid Hyrax Expander and Two Miniscrews in the Lower Arch: Case Report" Applied Sciences 12, no. 3: 1552. https://doi.org/10.3390/app12031552
APA StyleMigliorati, M., & Calzolari, C. (2022). Herbst Appliance Reinforced with an Hybrid Hyrax Expander and Two Miniscrews in the Lower Arch: Case Report. Applied Sciences, 12(3), 1552. https://doi.org/10.3390/app12031552






