Abstract
Background Acute bacterial conjunctivitis (ABC) is a relatively common medical condition caused by different pathogens. Although it rarely threatens vision, it is one of the most common conditions that cause red eyes and may be accompanied by discomfort and discharge. The study aimed to identify and characterize inpatients with ABC treated with topical antibiotics. Methods The EHRead® technology, based on natural language processing (NLP) and machine learning, was used to extract and analyze the clinical information in the electronic health records (EHRs) of antibiotic-treated patients with conjunctivitis and admitted to five hospitals in Spain between January 2014 and December 2018. Categorical variables were described by frequency, whereas numerical variables included the mean, standard deviation, median, and quartiles. Results From a source population of 2,071,812 adult patients who attended the participating hospitals in the study period, 11,110 patients diagnosed with acute conjunctivitis were identified. Six thousand five hundred eighty-three patients were treated with antibiotics, comprising the final study population. Microbiology was tested only on 12.1% of patients. Antibiotics, mainly tobramycin, and corticosteroids, mainly dexamethasone, were usually prescribed. NSAIDs were also used in about 50% of patients, always combined with antibiotics. Conclusions The present study provided a realistic representation of the hospital practice concerning managing patients with acute antibiotic-treated conjunctivitis. The diagnosis is usually based on the clinical ground, microbiology is rarely tested, few bacteria species are involved, and local antibiotics are frequently associated with corticosteroids and/or NSAIDs. Moreover, this study provided clinically relevant outcomes, based on new technology, that could be applied in clinical practice.
1. Introduction
Conjunctivitis is caused by inflammation or infection of the conjunctiva. Although it rarely threatens vision, it is one of the most common disorders that cause red eyes and is also characterized by discomfort and discharge [1]. Acute conjunctivitis is a common disease that may affect subjects of any age [2]. The prevalence of conjunctivitis depends on its underlying causes, which may be influenced by different factors, including the patient’s age, comorbidity, lifestyle, and season of the year [3].
Approximately 20% to 70% of infectious conjunctivitis is thought to be viral, and 65% to 90% of viral conjunctivitis is caused by adenoviruses, which are most prevalent in the summer [4]. On the other hand, allergic conjunctivitis is most frequent in spring and summer and may affect about 10–15% of the population [5].
Acute bacterial conjunctivitis is the second most common cause of infectious conjunctivitis and is responsible for the majority (50–75%) of cases in children [6]. It is observed more frequently from December through April [7]. The incidence of acute bacterial conjunctivitis in the United States has been estimated at 135 in 10,000 inhabitants (i.e., 4 million people per year) [8]. This infection can be contracted directly from infected individuals or abnormal native conjunctival microbiota, contaminated fingers, urogenital spread, and fomites. Additionally, compromised tear production, disruption of the natural epithelial barrier, trauma, and immunosuppressed status may predispose to acute bacterial conjunctivitis. The most common pathogens for acute bacterial conjunctivitis in adults are staphylococcal species, Streptococcus pneumoniae, and Haemophilus influenzae [9]. In children, the disease is often caused by H. influenzae, S. pneumoniae, and Moraxella catarrhalis [9]. From a clinical standpoint, acute bacterial conjunctivitis is self-limiting, typically lasting 7 to 10 days. However, treatment with antibiotic eye drops is associated with better clinical and microbiological remission rates than placebo [10]. Therefore, management with topical antibiotics is desirable in fast recovery, reduction of relapses, and prevention of potential sight-threatening complications.
In clinical trials focused on acute conjunctivitis, patient recruitment is challenging, as effective and timely recruitment of a valid number of patients is essential for the successful trial completion generation of robust results [11]. Indeed, challenges in patient recruitment are the most prominent reason for clinical trial delays [12], in turn negatively impacting the entire drug development process. However, this issue could be tackled by introducing a technology-assisted method for identifying patients and defining the current care pathways of individuals diagnosed with acute bacterial conjunctivitis who could benefit from inclusion in a clinical trial.
In light of the above, the analysis of vast amounts of real-world data (RWD) holds great potential to improve our understanding of conjunctivitis by providing a clinical description and overview of the patient’s journey. The clinical information in patients’ Electronic Health Records (EHRs) represents an important source of RWD. Remarkably, recent studies have underscored the value of the unstructured narratives jotted down by physicians in EHRs to describe patients’ clinical characteristics, management, epidemiological data, and disease prognosis [13,14,15,16,17,18,19]. However, to date, no study has used artificial intelligence to identify and characterize patients with acute bacterial conjunctivitis in large population samples.
SAVANA’s EHRead® is a new technology based on natural language processing (NLP) and machine learning to extract, organize, and analyze the unstructured clinical information health professionals in patients’ EHRs [20,21,22,23]. Therefore, the primary objective was to identify patients with acute bacterial conjunctivitis in general hospitals, mainly considering the percentage of patients managed in the Accident & Emergency (A&E) Room and Ophthalmology Unit using this new technology.
2. Materials and Methods
2.1. Study Design
The study was multicenter, retrospective, and observational based on the secondary use of the unstructured data captured in EHRs (Figure 1).
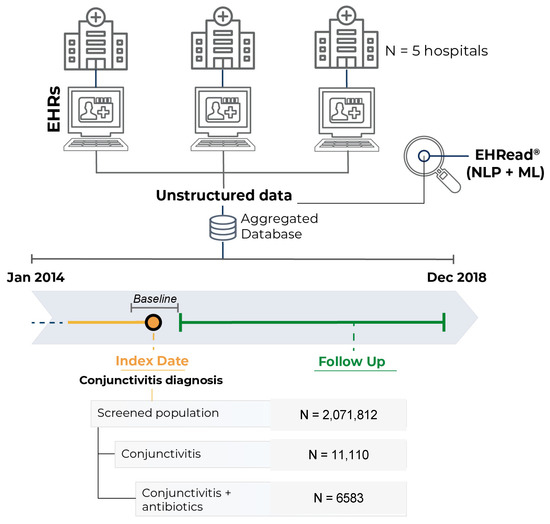
Figure 1.
Study design and timeline. Unstructured data from patients’ EHRs was extracted and organized into an aggregated database with the EHRead® technology. The Index Date was defined as the timepoint when diagnosis of conjunctivitis and antibiotic treatment were first identified within the EHRs of the patients. The follow-up period ranged from the Index Date to the end of the study period or the last data point available. Total number of patients with available EHRs, the number of patients with conjunctivitis, and the subset of patients with conjunctivitis treated with antibiotics in the participating hospitals from 1 January 2014 to 31 December 2018 are shown.
A cross-sectional analysis of all patients was performed at the time of inclusion (hereafter referred to as index date), defined as the first time in the study period (1 January 2014, and 31 December 2018) when the patient fulfilled all inclusion criteria and no exclusion criteria.
In all cases, the index date coincided with the first acute conjunctivitis diagnosis, requiring antibiotic treatment, registered in EHRs. Of note, patients diagnosed outside the study period were excluded from the analyses. The follow-up period spanned the time from the index date to the last EHR available for each patient within the study period.
2.2. Data Source
The data source is the free-text information in the EHRs of 5 hospitals from the Spanish National Healthcare Network, namely: Puerta del Hierro Hospital (Madrid), University Clinic of Navarra (Pamplona), Infanta Leonor University Hospital (Madrid), Infanta Sofía University Hospital (Madrid), and Rio Hortega Hospital (Valladolid). In addition, the study collected clinical data in outpatient clinical reports, hospital discharge reports, emergency reports, prescriptions, and other medical reports from all available services and departments in each participating site (including inpatient hospital, outpatient hospital, and emergency service).
2.3. Objectives
In addition to the primary objective, the secondary objectives included: (i) the profile, demographics, and clinical and disease characteristics of patients with conjunctivitis; (ii) the percentage of patients diagnosed with conjunctivitis in terms of the type of infection: clinical diagnosis of acute bacterial conjunctivitis, diagnosis of acute bacterial conjunctivitis microbiologically confirmed and the percentage of positive swab results; (iii) the follow-up visits in patients diagnosed with acute bacterial conjunctivitis; and (iv) the number of patients that performed a follow-up visit and how many days after the 1st visit, and which physician visit the patient (Ophthalmologist or A&E physician).
2.4. Study Population
The study population comprised all adult patients diagnosed with conjunctivitis and treated with antibiotics during the study period, according to the information captured from the EHRs. Patients with any eye-related diagnosis other than conjunctivitis, including blepharitis and keratitis, were excluded from the study.
2.5. Extraction of the Unstructured Information from EHRs
Unstructured clinical data were extracted using the EHRead® technology, which uses NLP and machine learning tools to extract the clinical free text from de-identified and processed EHRs [20,21,22,23,24,25]. Briefly, EHRead® can capture numerical values and physicians’ notes and translate these into usable variables, thus enabling the reuse of information in large-scale clinical records collections. Patients’ information is analyzed and expressed utilizing concepts that contain the most significant data in the text. The terminology considered by EHRead® is based on SNOMED CT and includes codes, concepts, synonyms, and standard definitions used in clinical documentation [24,25].
2.6. External Validation of EHRead®’s Performance
The ability of the NLP system to identify key variables associated with the study disease in patients’ EHRs was assessed as previously described [25]. Briefly, a comparison between a physician-annotated set of EHRs (i.e., the “gold standard”) and the output of EHRead® was carried out independently at each hospital site to ensure data quality. Two designated expert physicians from each hospital annotated a set of randomly selected records. In addition, a third physician reviewed the annotations made and resolved any possible discrepancies among the two evaluators (“gold standard”). The “output vs. gold standard” comparison was assessed in the standard evaluation metrics of Precision, Recall, and their harmonic mean (F1-score).
2.7. Statistical Data Analyses
Categorical variables were described via frequency tables, whereas numerical variables were summarized using tables that include the mean, standard deviation (SD), median, and interquartile range (Q1, Q3). Missing data were handled according to the nature of the data collection process; lack of information (i.e., unavailable data in patients’ EHRs) was considered a ‘true zero’ for binary variables (e.g., absence of comorbidity). Still, it was treated as missing data for numerical variables (e.g., laboratory values). All analyses were performed using “R” software, version 4.0.2.
2.8. Ethical Considerations
This study was classified as a ‘non-post-authorization study’ by the Spanish Agency of Medicines and Health Products (AEMPS). However, it was approved by the Institutional Review Board (IRB) of each participating hospital. All methods and analyses were conducted in compliance with local legal and regulatory requirements and generally accepted research practices described in the Helsinki Declaration in its latest edition and Good Pharmacoepidemiology Practices. Data were analyzed from anonymized EHRs and aggregated in an irreversibly dissociated manner. Thus, individual patient consent was not required in the study.
3. Results
3.1. Study Population and Linguistic Validation of the System
From a source population of 2,071,812 adult patients who attended the participating hospitals in the study period, 11,110 patients diagnosed with acute conjunctivitis were identified. Six thousand five hundred eighty-three patients were treated with antibiotics, comprising the final study population (Figure 1). Conjunctivitis was diagnosed in the Emergency and Ophthalmology departments in 29% and 20.8% of patients. The remaining patients (41.9%) were diagnosed in different clinical units across the participating hospitals, including internal medicine, cardiology, surgery, orthopedics, and others.
Before proceeding to analyze the variables of interest in the present study, external validation of the reading performance by the NLP system was performed.
3.2. Characterization of the Target Population
The demographic and clinical characteristics of the study population are summarized in Table 1.

Table 1.
Demographic data and clinical characteristics of patients with acute bacterial conjunctivitis diagnosed on a clinical ground.
The median (Q1, Q3) age was 53 (37.5, 72), with two-thirds of the sample under 65 years of age and a slight predominance of the female gender (57.1%). The most diagnosed comorbidities in antibiotics-treated patients with conjunctivitis included hypertension (50.8%), dyslipidemia (39.9%), and cancer (23.7%). Regarding ocular comorbidities, the most frequent disorders were glaucoma (5.2%) and myopia (4.8%).
Regarding ocular comorbidities, the most commonly diagnosed eye conditions were glaucoma (5.2%), myopia (4.8%), diabetic retinopathy (3%), presbyopia, and astigmatism (1.2%).
The median follow-up period was 1.8 (IQR 0.36–11.4) months. Patients had a median of one conjunctivitis episode; 4.4% (n = 287) had two conjunctivitis episodes, and 1% (n = 66) had three conjunctivitis episodes. The median time between the first and second conjunctivitis episodes was 3 and 4 months.
3.3. Microbiology Results and Conjunctivitis-Related Signs and Symptoms
Table 2 reports the clinical characteristics: microbiology was tested in 810 (12.3%) patients, and bacterial conjunctivitis was confirmed in 795 (12.1%).

Table 2.
Microbiological findings.
The polymicrobial infection affected 32.3% of patients. The most common bacteria detected by culture were Gram-negative bacilli (37.2%), S pneumoniae (35.1%), S aureus (23.8%), Pseudomonas (13.8%), and Enterobacteriaceae (11.3%).
Table 3 summarizes the frequency of signs and symptoms reported for patients with acute bacterial conjunctivitis: 74.6% of patients had conjunctival hyperemia, 42.7% had ocular itching, and 20.8% had lacrimation.

Table 3.
Signs and symptoms in patients with acute bacterial conjunctivitis.
3.4. Treatments
Table 4 shows the most common topical medications used for treating acute bacterial conjunctivitis.

Table 4.
Topical medications used for treating acute bacterial conjunctivitis.
Topical combined treatments were widespread; most patients used different fixed combined products.
Tobramycin was the most prescribed antibiotic, both alone (70.3%) and combined with dexamethasone (53.4%). Moreover, in 73.8% of the patients, corticosteroids were prescribed, mainly dexamethasone (60.2%). Interestingly, we observed that in 68.2% of the patients, a concurrent combination of antibiotics and corticosteroids was reported, and a combination of tobramycin and dexamethasone was found in 53.4% of the population. NSAIDs were also prescribed in about 50% of patients, always in fixed combination with antibiotics.
3.5. Visits
Regarding physician visits, 2277 (34.6%) patients were seen at the A&E departments, and 1549 (23.5%) patients were seen at the Ophthalmological departments.
4. Discussion
Although acute bacterial conjunctivitis is known as a common medical condition worldwide, there is a lack of population-based incidence studies, which leads to inaccurate data regarding its true epidemiology [26,27]. First, there is a clinical ambiguity among infectious and non-infectious conjunctivitis, and between acute viral and bacterial conjunctivitis [26]. Because a high number of patients self-medicate or delay or decline to seek medical care, and inaccurate diagnosis in the primary medical care setting is frequent [27]. In the present patient series, 29% of the cases were detected in the emergency department of the participating hospitals, and only 5.7% of the patients presented more than one episode.
Despite acute bacterial conjunctivitis (ABC) is a common medical condition, the current study showed that the number of patients with acute conjunctivitis treated with topical antibiotics was relatively low over five years. This low frequency depends on two main reasons. First, the study concerned in-hospital patients. Second, patients with acute conjunctivitis usually refer to the practitioner or pharmacist but rarely to the ophthalmologist or emergency room, except for the severe presentation.
The present study provided a series of interesting outcomes that may reflect what happens in the daily hospital practice. Patients managed by A&E doctors are more than patients visited by ophthalmologists. It could depend on clinical severity and prompt availability of A&E physicians. Moreover, acute conjunctivitis may also occur during hospitalization in every specialistic unit.
The relatively old age (54.8 years) probably depends on the global population, including inpatients; consistently, comorbidity frequencies were typical for the mean age.
Notably, antibiotics were always used in patients with suspected acute bacterial conjunctivitis, even if the prescription was performed on a clinical ground in the vast majority of patients (about 90%). Microbiology was tested only in 12.1% of patients, likely the most severe, as the percentage of positive cultures was dramatically high (near 100%). Gram-negative bacteria were very frequent (37%); S pneumoniae and S aureus were prevalent, probably by self-contamination. Consequently, aminoglycosides (mostly tobramycin) were the most commonly prescribed topical antibiotics.
Polytherapy, such as using two or more medications, was predominant as almost all patients took more medications. In particular, the most common association was antibiotic plus corticosteroid. Namely, the fixed combination of tobramycin with dexamethasone was prevalent as used by half of the patients. Interestingly, topical corticosteroids, mainly dexamethasone, were also commonly used. Interestingly, non-steroidal anti-inflammatory drugs (NSAIDs) were frequently prescribed, as more than half of the patients used them. However, NSAIDs were always used associated with antibiotics or antibiotics and corticosteroids.
Hyperemia, itching, and lacrimation were the most frequent signs and symptoms. The low frequency of discharge might depend on problems regarding the translation from Spanish to English and the terms used in the clinical reports. Usually, patients experience a single episode, and the follow-up visit occurs within one month.
Therefore, the present study provided a realistic depiction of daily hospital practice. However, a series of limitations should be considered for the study. First, the results presented in the current study report were based on the unstructured, free-text narratives jotted down by physicians and other healthcare professionals in patients’ EHRs. Therefore, the present findings were limited by how physicians accurately describe patients’ status in their medical records. Second, this study was a data-driven, retrospective analysis based on the reorganization and analysis of already existing clinical data collected in natural settings. In this context, even if multiple records are available for a given patient within the selected time points, the availability of the desired variables in those records cannot be guaranteed. In the present study, this limitation explains the loss of patients during follow-up and the reported missing data points across variables. Third, the quality and validity of our results rely on the completeness and accuracy of EHRs. The lack of standardization in EHRs in terms of the type of collected data across disciplines, use of standard vs. in-house medical terminology, omitted information, or misuse of sections in the records represent a methodological challenge [28]. In addition, this study was based on attended patients in the hospital, and high percentage of patients with acute conjunctivitis usually refer to the practitioner or pharmacist, but rarely to the ophthalmologist except for patients with prolonged symptoms, poor response, or severe disease presentation [26,29,30]. Finally, bacterial conjunctivitis was presumed in all patients with conjunctivitis and antibiotic prescription, thus a potential overestimation of the incidence of acute bacterial conjunctivitis might have occurred [26].
Although most fields are well suited to perform EHR-based studies, the successful application of AI and big data to access and analyze EHRs depends on a multidisciplinary effort to improve how clinicians document their routine practice in patients’ records. In this line, raising awareness among healthcare professionals about the importance of EHR completeness will undoubtedly boost the quality of medical research and ultimately improve patient care and hospital resource management.
In addition, this study investigated a topic scarcely explored in Spain [31,32]. Therefore, the findings provided updated data on the relevance of acute bacterial conjunctivitis in that country.
5. Conclusions
The present study provided a realistic representation of the hospital practice concerning managing patients with acute antibiotic-treated conjunctivitis. The diagnosis is usually based on the clinical ground, microbiology is rarely tested, few bacteria species are involved, and local antibiotics are frequently associated with corticosteroids and/or NSAIDs. Moreover, this study was the first to use a new artificial intelligence technology to identify and characterize patients with acute bacterial conjunctivitis in a large sample population. In addition, this study provided clinically relevant information as based on innovative and robust methodology. Thus, the results could be applied in clinical practice.
Author Contributions
Conceptualization, N.V.S., M.M. and A.G.-L.; methodology, T.C. and M.M.M.; writing—review and editing, G.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research was partially sponsored by NTC, Milan, Italy.
Institutional Review Board Statement
This study was classified as a ‘non-post-authorization study’ by the Spanish Agency of Medicines and Health Products (AEMPS). However, it was approved by the Institutional Review Board (IRB) of each participating hospital.
Informed Consent Statement
Informed consent was obtained from the patients.
Data Availability Statement
The data are available on request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Leibowitz, H.M. The red eye. N. Engl. J. Med. 2000, 343, 345–351. [Google Scholar] [CrossRef] [PubMed]
- Udeh, B.L.; Schneider, J.E.; Ohsfeldt, R.L. Cost effectiveness of a point-of-care test for adenoviral conjunctivitis. Am. J. Med. Sci. 2008, 336, 254–264. [Google Scholar] [CrossRef] [PubMed]
- Azari, A.A.; Barney, N.P. Conjunctivitis: A systematic review of diagnosis and treatment. JAMA 2013, 310, 1721–1729. [Google Scholar] [CrossRef] [PubMed]
- Epling, J. Bacterial conjunctivitis. BMJ Clin. Evid. 2012, 2012, 704. [Google Scholar]
- Bielory, B.P.; O’Brien, T.P.; Bielory, L. Management of seasonal allergic conjunctivitis: Guide to therapy. Acta Ophthalmol. 2012, 90, 399–407. [Google Scholar] [CrossRef] [PubMed]
- Hovding, G. Acute bacterial conjunctivitis. Acta Ophthalmol. 2008, 86, 5–17. [Google Scholar] [CrossRef]
- Alfonso, S.A.; Fawley, J.D.; Alexa Lu, X. Conjunctivitis. Prim. Care 2015, 42, 325–345. [Google Scholar] [CrossRef]
- Smith, A.F.; Waycaster, C. Estimate of the direct and indirect annual cost of bacterial conjunctivitis in the United States. BMC Ophthalmol. 2009, 9, 13. [Google Scholar] [CrossRef]
- Azari, A.A.; Arabi, A. Conjunctivitis: A Systematic Review. J. Ophthalmic Vis. Res. 2020, 15, 372–395. [Google Scholar] [CrossRef]
- Sheikh, A.; Hurwitz, B.; van Schayck, C.P.; McLean, S.; Nurmatov, U. Antibiotics versus placebo for acute bacterial conjunctivitis. Cochrane Database Syst. Rev. 2012, 9, CD001211. [Google Scholar] [CrossRef]
- Lovato, L.C.; Hill, K.; Hertert, S.; Hunninghake, D.B.; Probstfield, J.L. Recruitment for controlled clinical trials: Literature summary and annotated bibliography. Control Clin. Trials 1997, 18, 328–352. [Google Scholar] [CrossRef] [PubMed]
- McDonald, A.M.; Knight, R.C.; Campbell, M.K. What influences recruitment to randomised controlled trials? A review of trials funded by two UK funding agencies. Trials 2006, 7, 9. [Google Scholar] [CrossRef] [PubMed]
- Sheikhalishahi, S.; Miotto, R.; Dudley, J.T.; Lavelli, A.; Rinaldi, F.; Osmani, V. Natural Language Processing of Clinical Notes on Chronic Diseases: Systematic Review. JMIR Med. Inform. 2019, 7, e12239. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, B.A.; Navar, A.M.; Pencina, M.J.; Ioannidis, J.P. Opportunities and challenges in developing risk prediction models with electronic health records data: A systematic review. J. Am. Med. Inform. Assoc. 2017, 24, 198–208. [Google Scholar] [CrossRef] [PubMed]
- Luo, Y.; Thompson, W.K.; Herr, T.M. Natural Language Processing for EHR-Based Pharmacovigilance: A Structured Review. Drug Saf. 2017, 40, 1075–1089. [Google Scholar] [CrossRef]
- Izquierdo, J.L.; Almonacid, C.; González, Y. The Impact of COVID-19 on Patients with Asthma. Eur. Res. J. 2020, 57, 2003142. [Google Scholar] [CrossRef]
- Ancochea, J.; Izquierdo, J.L.; Medrano, I.H.; Porras, A.; Serrano, M.; Lumbreras, S.; Del Rio-Bermudez, C.; Marchesseau, S.; Salcedo, I.; Zubizarreta, I.; et al. Evidence of gender differences in the diagnosis and management of COVID-19 patients: An analysis of Electronic Health Records using Natural Language Processing and machine learning. J. Women Health 2021, 30, 393–404. [Google Scholar] [CrossRef]
- Izquierdo, J.L.; Ancochea, J.; Soriano, J.B. Clinical Characteristics and Prognostic Factors for Intensive Care Unit Admission of Patients With COVID-19: Retrospective Study Using Machine Learning and Natural Language Processing. J. Med. Internet Res. 2020, 22, e21801. [Google Scholar] [CrossRef]
- Graziani, D.; Soriano, J.B.; Del Rio-Bermudez, C. Characteristics and Prognosis of COVID-19 in Patients with COPD. J. Clin. Med. 2020, 9, 3259. [Google Scholar] [CrossRef]
- González-Juanatey, C.; Anguita-Sánchez, M.; Barrios, V.; Núñez-Gil, I.; Gómez-Doblas, J.J.; García-Moll, X. Assessment of medical management in Coronary Type 2 Diabetic patients with previous percutaneous coronary intervention in Spain: A retrospective analysis of electronic health records using Natural Language Processing. PLoS ONE 2022, 17, e0263277. [Google Scholar] [CrossRef]
- Gomollón, F.G.; Gisbert, J.P.; Guerra, I.; Montoto, C. Clinical Characteristics and Prognostic Factors for Crohn’s Disease Relapses using Natural Language Processing and Machine Learning—A Pilot Study. Eur. J. Gastroenterol. Hepatol. 2022, 34, 389–397. [Google Scholar] [CrossRef]
- Del Rio-Bermudez, C.; Medrano, I.H.; Yebes, L.; Poveda, J.L. Towards a symbiotic relationship between big data, artificial intelligence, and hospital pharmacy. J. Pharm. Policy Pract. 2020, 13, 75. [Google Scholar] [CrossRef]
- Canales, L.; Menke, S.; Marchesseau, S.; D’Agostino, A.; Del Rio-Bermudez, C.; Taberna, M. Assessing the Performance of Clinical Natural Language Processing Systems: Development of an Evaluation Methodology. JMIR Med. Inform. 2021, 9, e20492. [Google Scholar] [CrossRef] [PubMed]
- Espinosa-Anke, L.T.J.; Pardo, A.; Medrano, I.; Ureña, A.; Salcedo, I.; Saggion, H. Savana: A Global Information Extraction and Terminology Expansion Framework in the Medical Domain Procesamiento del Lenguaje Natural. Soc. Espanol. Proc. Nat. 2016, 57, 23–30. [Google Scholar]
- Benson, T. Principles of Health Interoperability HL7 and SNOMED; Springer: London, UK, 2012. [Google Scholar]
- Yeu, E.; Hauswirth, S. A Review of the Differential Diagnosis of Acute Infectious Conjunctivitis: Implications for Treatment and Management. Clin. Ophthalmol. 2020, 14, 805–813. [Google Scholar] [CrossRef] [PubMed]
- Rose, P. Management strategies for acute infective conjunctivitis in primary care: A systematic review. Expert Opin. Pharmacother. 2007, 8, 1903–1921. [Google Scholar] [CrossRef]
- Woodward, M.; Maganti, N.; Niziol, L.; Amin, S.; Hou, A.; Singh, K. Development and Validation of a Natural Language Processing Algorithm to Extract Descriptors of Microbial Keratitis from the Electronic Health Record. Cornea 2021, 40, 1548–1553. [Google Scholar] [CrossRef]
- Meaders, B.C.; Azar, J.M. Bacterial conjunctivitis: A review of therapies and approaches. Adv. NPs PAs 2012, 3, 25–29, 34. [Google Scholar]
- Mas-Tur, V.; Jawaid, I.; Poostchi, A.; Verma, S. Optometrist referrals to an emergency ophthalmology department: A retrospective review to identify current practise and development of shared care working strategies, in England. Eye 2021, 35, 1340–1346. [Google Scholar] [CrossRef] [PubMed]
- Orden Martínez, B.; Martínez Ruiz, R.; Millán Pérez, R. Bacterial conjunctivitis: Most prevalent pathogens and their antibiotic sensitivity. An. Pediatr. 2004, 61, 32–36. [Google Scholar] [CrossRef]
- Benitez-Del-Castillo, J.; Verboven, Y.; Stroman, D.; Kodjikian, L. The role of topical moxifloxacin, a new antibacterial in Europe, in the treatment of bacterial conjunctivitis. Clin. Drug Investig. 2011, 31, 543–557. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).