Contact Lens-Based Microchannel Rings for Detecting Ocular Hypertension
Abstract
1. Introduction
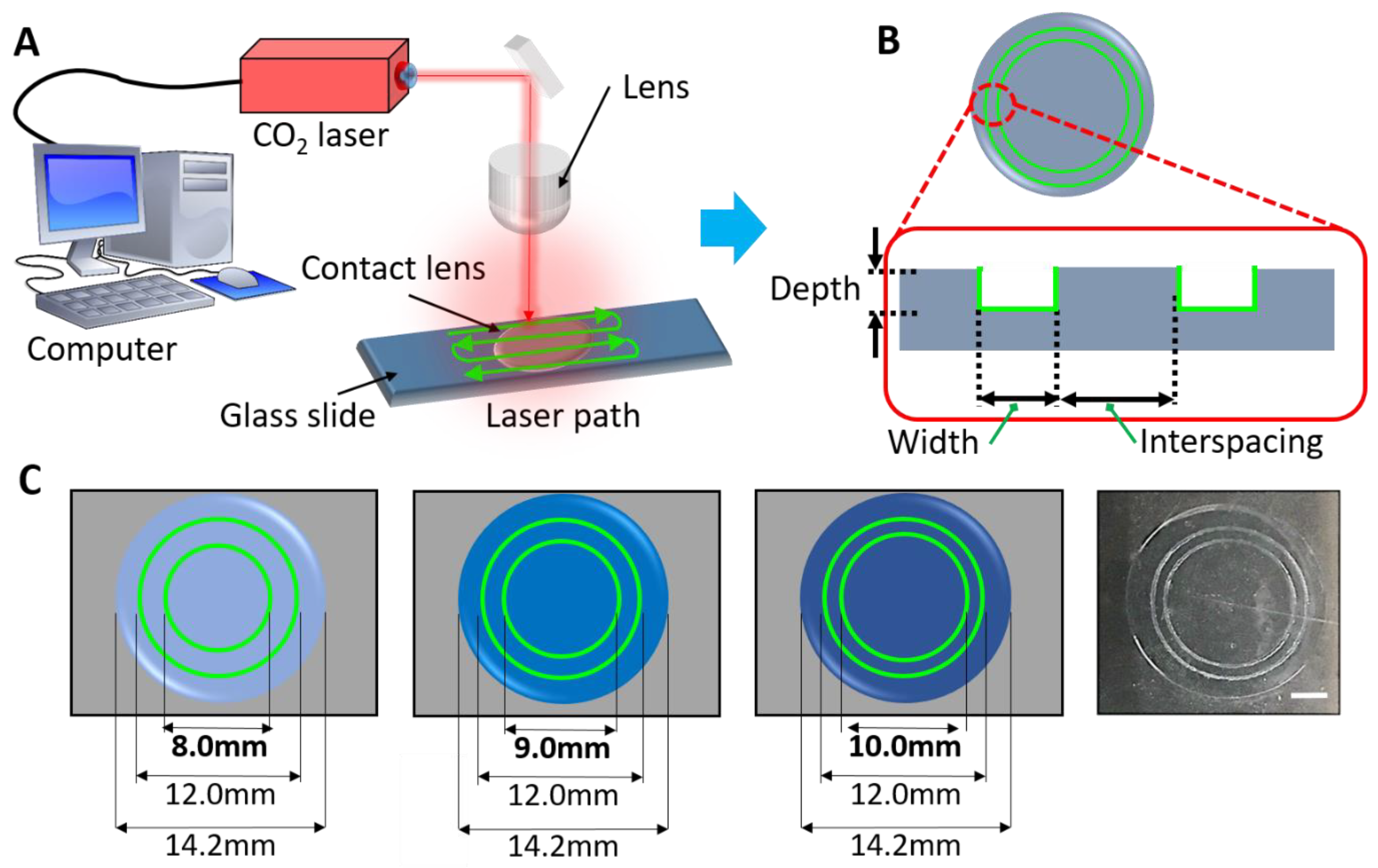
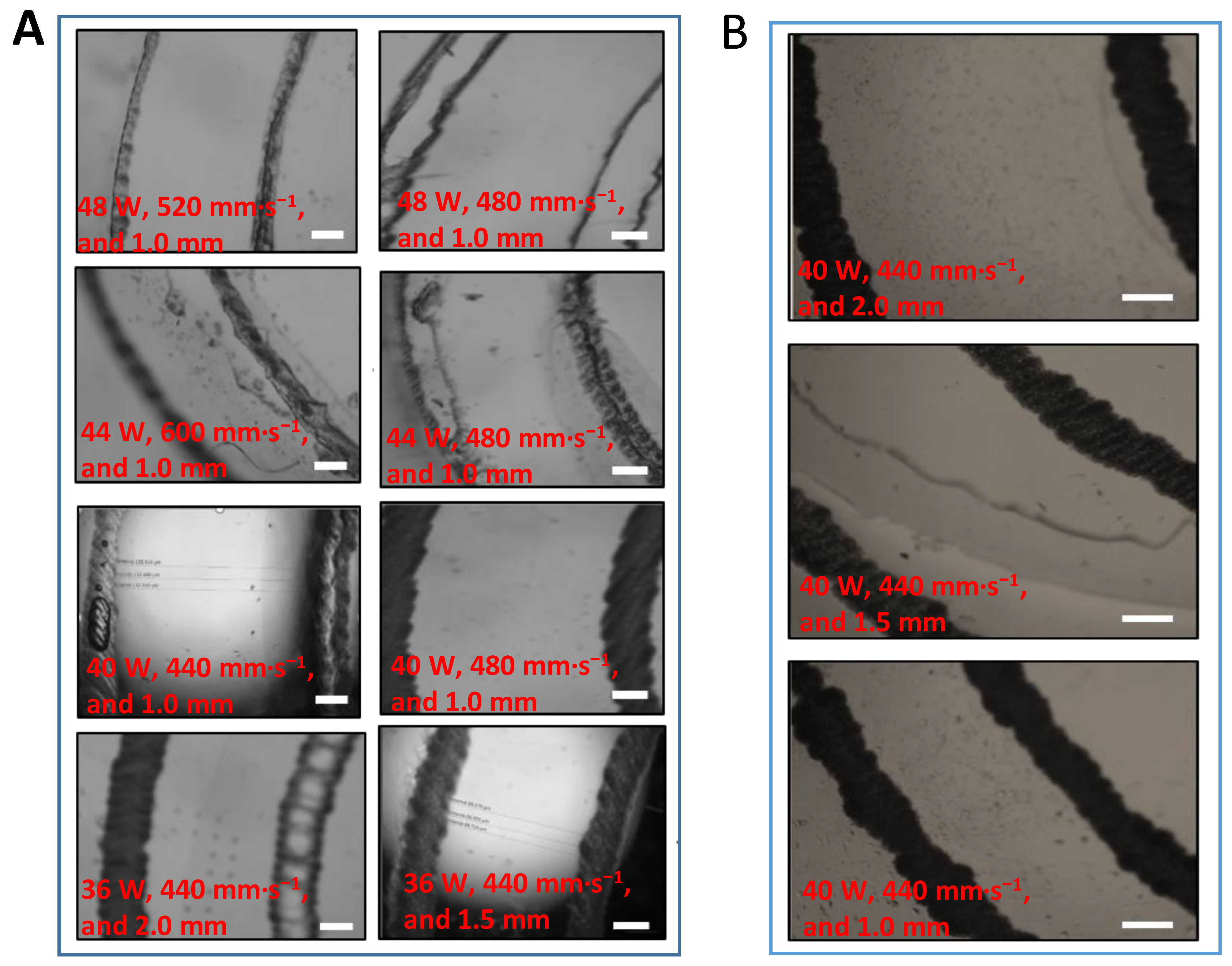
2. Materials and Methods
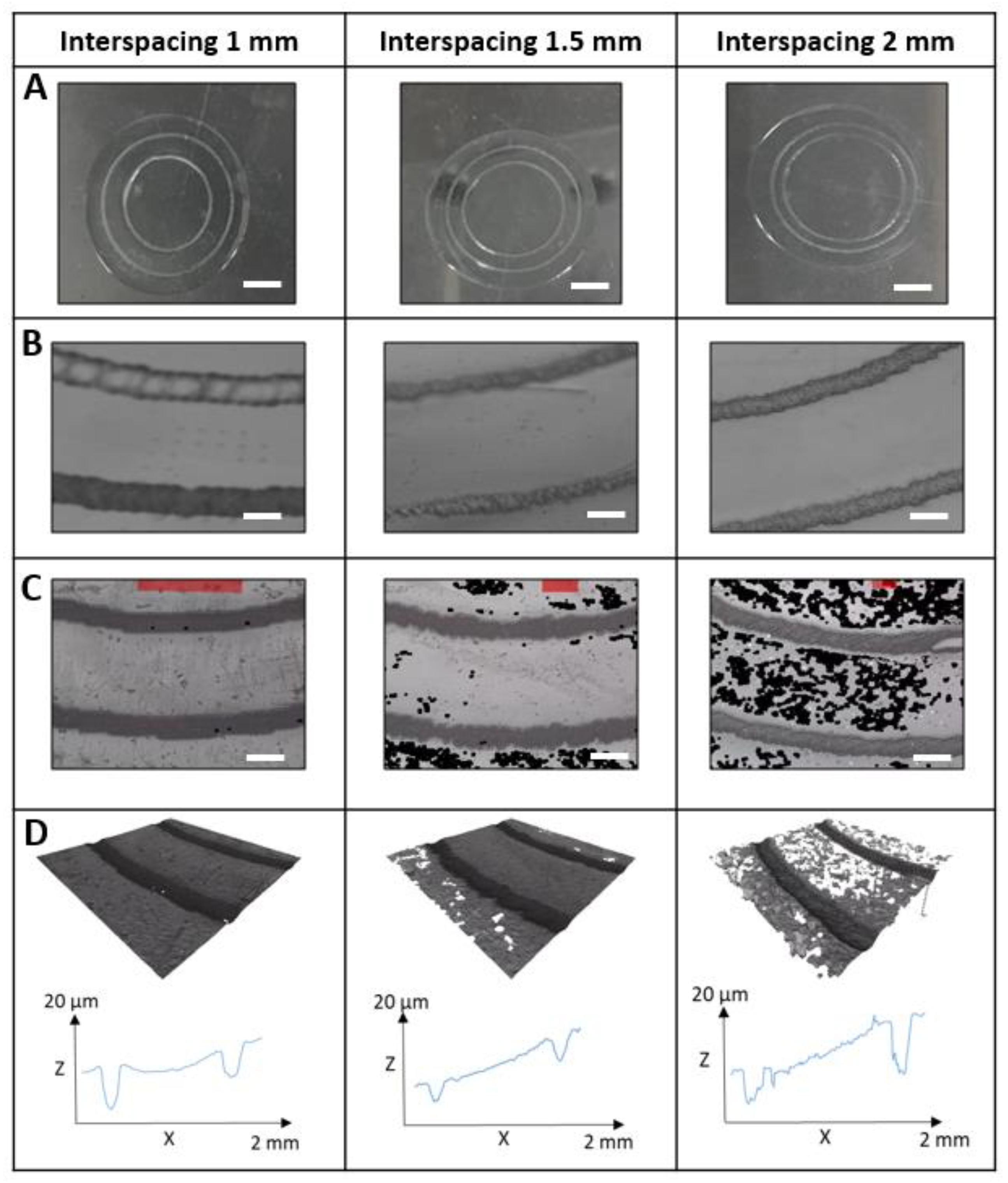
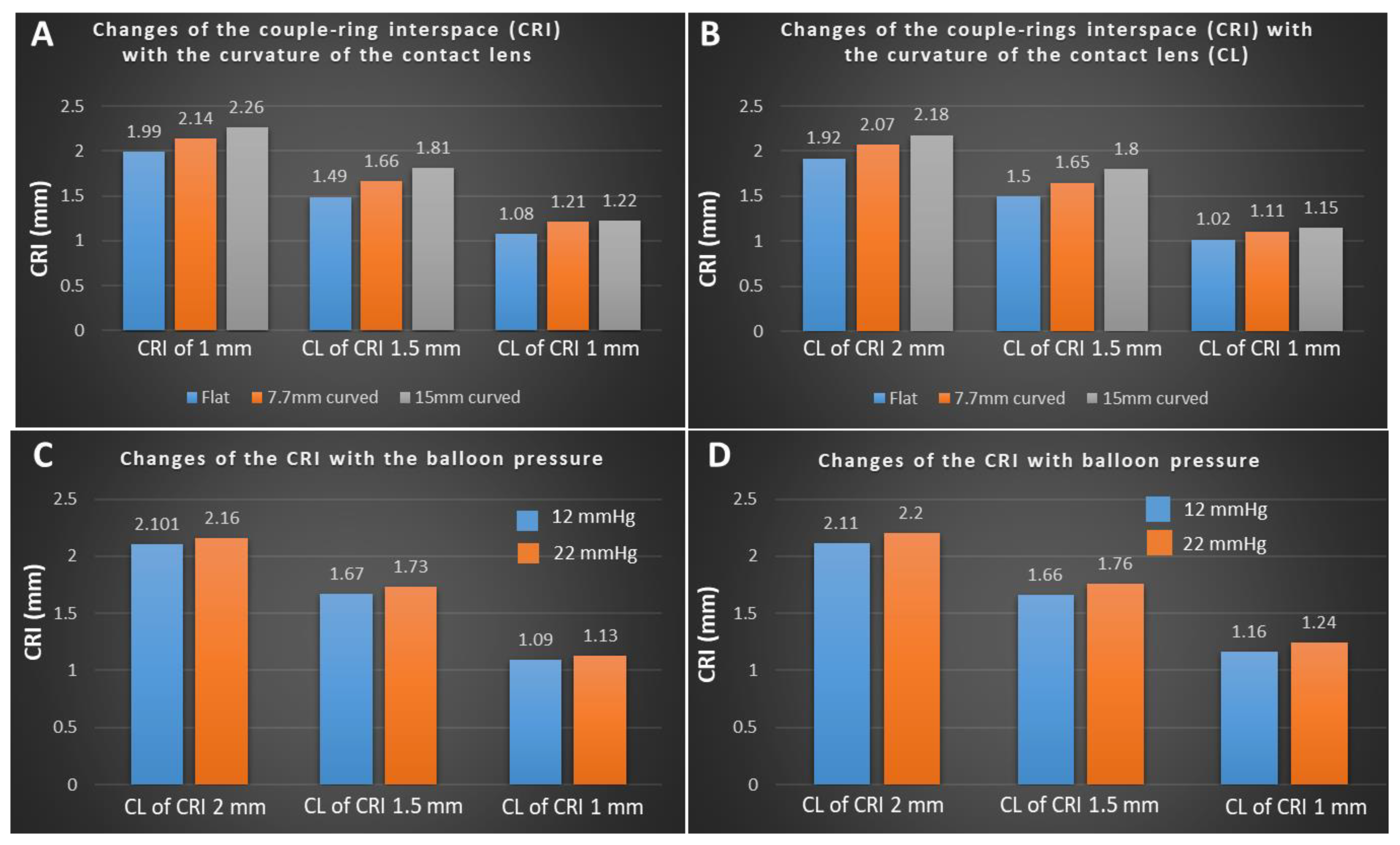
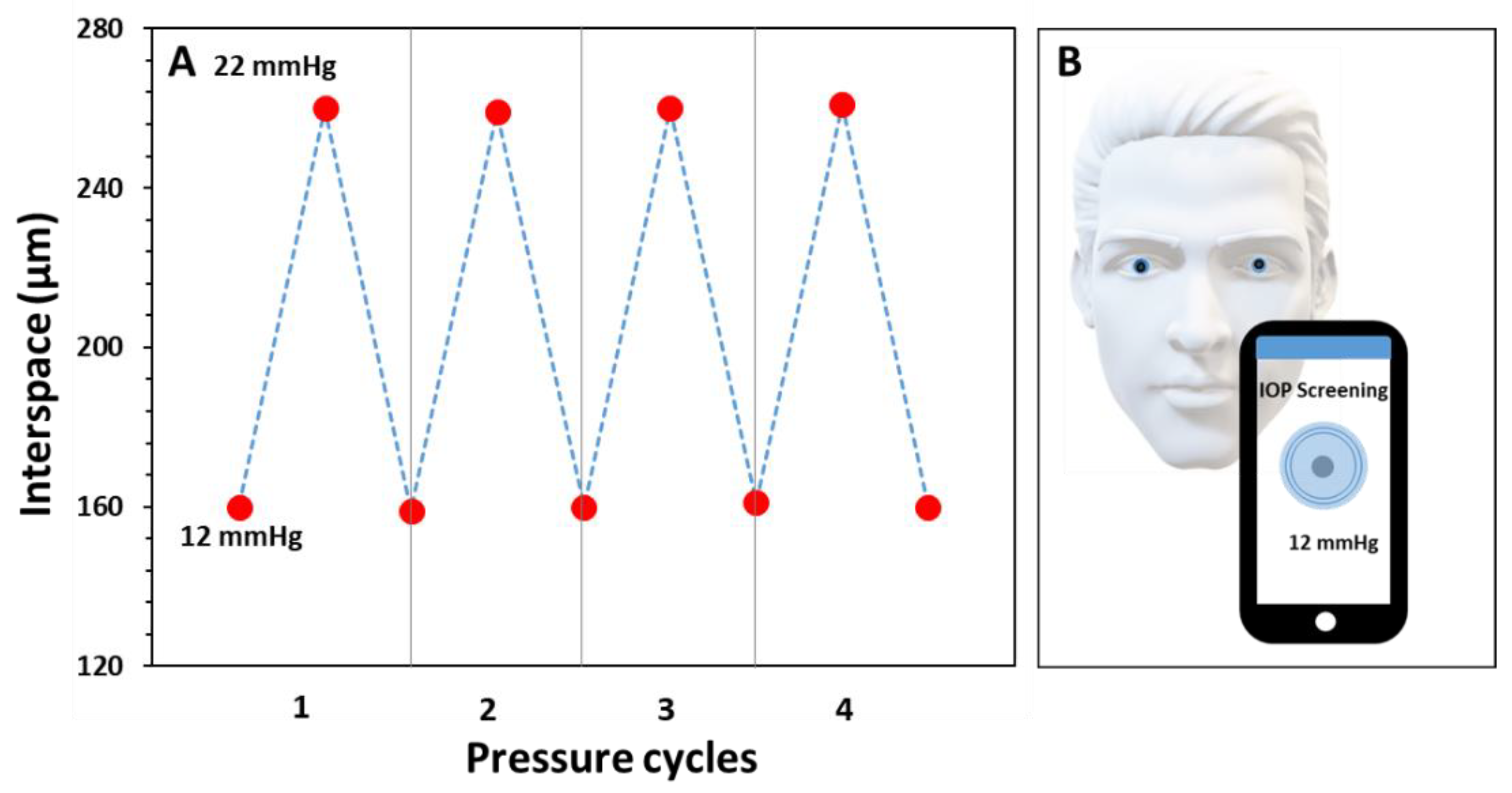
3. Results and Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Liu, J.; Roberts, C.J. Influence of corneal biomechanical properties on intraocular pressure measurement: Quantitative analysis. J. Cataract. Refract. Surg. 2005, 31, 146–155. [Google Scholar] [CrossRef] [PubMed]
- Moreddu, R.; Mahmoodi, N.; Kassanos, P.; Vigolo, D.; Mendes, P.M.; Yetisen, A.K. Stretchable Nanostructures as Optomechanical Strain Sensors for Ophthalmic Applications. ACS Appl. Polym. Mater. 2021, 3, 5416–5424. [Google Scholar] [CrossRef]
- Realini, T.; Weinreb, R.N.; Wisniewski, S. Short-term repeatability of diurnal intraocular pressure patterns in glaucomatous individuals. Ophthalmology 2011, 118, 47–51. [Google Scholar] [CrossRef] [PubMed]
- Barkana, Y.; Anis, S.; Liebmann, J.; Tello, C.; Ritch, R. Clinical utility of intraocular pressure monitoring outside of normal office hours in patients with glaucoma. Arch. Ophthalmol. 2006, 124, 793–797. [Google Scholar] [CrossRef]
- Mansouri, K.; Medeiros, F.A.; Tafreshi, A.; Weinreb, R.N. Continuous 24-hour monitoring of intraocular pressure patterns with a contact lens sensor: Safety, tolerability, and reproducibility in patients with glaucoma. Arch. Ophthalmol. 2012, 130, 1534–1539. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.H.; Zhang, X.; Kripke, D.F.; Weinreb, R.N. Twenty-four-hour intraocular pressure pattern associated with early glaucomatous changes. Investig. Ophthalmol. Vis. Sci. 2003, 44, 1586–1590. [Google Scholar] [CrossRef]
- Kida, T.; Liu, J.H.; Weinreb, R.N. Effect of 24-hour corneal biomechanical changes on intraocular pressure measurement. Investig. Ophthalmol. Vis. Sci. 2006, 47, 4422–4426. [Google Scholar] [CrossRef]
- Liu, J.H.; Weinreb, R.N. Monitoring intraocular pressure for 24 h. Br. J. Ophthalmol. 2011, 95, 599–600. [Google Scholar] [CrossRef]
- Hughes, E.; Spry, P.; Diamond, J. 24-hour monitoring of intraocular pressure in glaucoma management: A retrospective review. J. Glaucoma 2003, 12, 232–236. [Google Scholar] [CrossRef]
- Renard, E.; Palombi, K.; Gronfier, C.; Pepin, J.L.; Noel, C.; Chiquet, C.; Romanet, J.P. Twenty-four hour (Nyctohemeral) rhythm of intraocular pressure and ocular perfusion pressure in normal-tension glaucoma. Investig. Ophthalmol. Vis. Sci. 2010, 51, 882–889. [Google Scholar] [CrossRef]
- Lee, Y.H.; Kim, C.S.; Hong, S.P. Rate of visual field progression in primary open-angle glaucoma and primary angle-closure glaucoma. Korean J. Ophthalmol. 2004, 18, 106–115. [Google Scholar] [CrossRef] [PubMed]
- Ehlers, N.; Bramsen, T.; Sperling, S. Applanation tonometry and central corneal thickness. Acta Ophthalmol. 1975, 53, 34–43. [Google Scholar] [CrossRef]
- Leonardi, M.; Leuenberger, P.; Bertrand, D.; Bertsch, A.; Renaud, P. First steps toward noninvasive intraocular pressure monitoring with a sensing contact lens. Investig. Ophthalmol. Vis. Sci. 2004, 45, 3113–3117. [Google Scholar] [CrossRef] [PubMed]
- Lin, M.C.; Soliman, G.N.; Lim, V.A.; Giese, M.L.; Wofford, L.E.; Marmo, C.; Radke, C.; Polse, K.A. Scalloped channels enhance tear mixing under hydrogel contact lenses. Optom. Vis. Sci. 2006, 83, 874–878. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Creech, J.L.; Chauhan, A.; Radke, C.J. Dispersive Mixing in the Posterior Tear Film Under a Soft Contact Lens. Ind. Eng. Chem. Res. 2001, 40, 3015–3026. [Google Scholar] [CrossRef]
- Monticelli, M.V.; Chauhan, A.; Radke, C.J. The effect of water hydraulic permeability on the settling of a soft contact lens on the eye. Curr. Eye Res. 2005, 30, 329–336. [Google Scholar] [CrossRef]
- Weinreb, R.N.; Liu, J.H. Nocturnal rhythms of intraocular pressure. Arch. Ophthalmol. 2006, 124, 269–270. [Google Scholar] [CrossRef]
- Liu, J.H.; Medeiros, F.A.; Slight, J.R.; Weinreb, R.N. Diurnal and nocturnal effects of brimonidine monotherapy on intraocular pressure. Ophthalmology 2010, 117, 2075–2079. [Google Scholar] [CrossRef]
- Dunbar, G.E.; Shen, B.Y.; Aref, A.A. The Sensimed Triggerfish contact lens sensor: Efficacy, safety, and patient perspectives. Clin. Ophthalmol. 2017, 11, 875–882. [Google Scholar] [CrossRef]
- Liu, J.H.; Mansouri, K.; Weinreb, R.N. Estimation of 24-Hour Intraocular Pressure Peak Timing and Variation Using a Contact Lens Sensor. PLoS ONE 2015, 10, e0129529. [Google Scholar] [CrossRef]
- Chauhan, A.; Radke, C.J. Settling and deformation of a thin elastic shell on a thin fluid layer lying on a solid surface. J. Colloid Interface Sci. 2002, 245, 187–197. [Google Scholar] [CrossRef] [PubMed]

| TRIAL NUMBER | INTERSPACING (mm) | LASER POWER (W) | SCANNING SPEED (mm·s−1) |
|---|---|---|---|
| 1 | 1 | 48 | 520 |
| 2 | 48 | 480 | |
| 3 | 44 | 520 | |
| 4 | 44 | 480 | |
| 5 | 40 | 600 | |
| 6 | 40 | 440 | |
| 7 | 1.5 | 40 | 440 |
| 8 | 2 | 40 | 440 |
| 9 | 2 | 36 | 440 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alqurashi, Y.; Elsherif, M.; Moreddu, R.; Cieslak, M.; Dhaliwal, H.; Essa, K.; Butt, H. Contact Lens-Based Microchannel Rings for Detecting Ocular Hypertension. Appl. Sci. 2022, 12, 10661. https://doi.org/10.3390/app122010661
Alqurashi Y, Elsherif M, Moreddu R, Cieslak M, Dhaliwal H, Essa K, Butt H. Contact Lens-Based Microchannel Rings for Detecting Ocular Hypertension. Applied Sciences. 2022; 12(20):10661. https://doi.org/10.3390/app122010661
Chicago/Turabian StyleAlqurashi, Yousef, Mohamed Elsherif, Rosalia Moreddu, Magdalena Cieslak, Hemeth Dhaliwal, Khamis Essa, and Haider Butt. 2022. "Contact Lens-Based Microchannel Rings for Detecting Ocular Hypertension" Applied Sciences 12, no. 20: 10661. https://doi.org/10.3390/app122010661
APA StyleAlqurashi, Y., Elsherif, M., Moreddu, R., Cieslak, M., Dhaliwal, H., Essa, K., & Butt, H. (2022). Contact Lens-Based Microchannel Rings for Detecting Ocular Hypertension. Applied Sciences, 12(20), 10661. https://doi.org/10.3390/app122010661












