Abstract
Background: Transurethral resection of the prostate (TURP) is the gold-standard treatment for benign prostatic hyperplasia (BPH). However, laser surgery techniques (e.g., photoselective vaporization of the prostate (PVP), holmium laser, thulium laser enucleation of the prostate (HoLEP or ThuLEP)), and minimally invasive treatment options (e.g., UroLift) are increasingly replacing TURP. This study seeks to report the annual incidence, management trends, and costs of BPH procedures in the U.S. Methods: Data analyses of U.S. health insurance claims from 2004 to 2017, collected from the de-identified Optum Clinformatics Claims Database, were performed to determine the number of BPH patients and the treatment selected. Results: A total of 51,448 patients underwent BPH procedures from 2004 to 2017. There was a significant increase in the annual rate from 770 in 2004 to 6571 in 2017. The mean patient age (±SD) increased from 67.6 years old (±8.4) in 2004 to 73.4 years old (±8.4) in 2017. More than 60% of patients underwent cystourethroscopy and a post-void residual urine check for workup prior to surgical management. TURP was the most-common, and PVP was the second-most-common BPH procedure. Medical and total treatment costs increased, while the detection rate of prostate cancer after BPH surgery gradually decreased from 19.87% in 2004 to 5.78% in 2017. Conclusions: Our study demonstrates a recent trend in BPH management that replaces the traditional TURP technique with alternative methods. Due to rising costs, future studies should assess whether these newer methods are cost effective over the long term.
1. Introduction
Benign prostatic hyperplasia (BPH) is a common condition afflicting male patients, who may suffer from related lower urinary tract symptoms (LUTS), such as frequency, nocturia, and urgency. Several mechanisms have been reported to affect and aggravate LUTS in BPH patients, including age-related impairment of blood flow in pelvic organs and aggravation in bladder dysfunction [1]. If LUTS are medically uncorrectable, surgical treatment should be considered for otherwise healthy male patients, who suffer from moderate-to-severe outlet-obstructive symptoms.
Transurethral resection of the prostate (TURP) is the gold standard for surgical treatment of BPH [2]. However, technological advancements in medical device development have provided many alternative surgical options, including photoselective vaporization of the prostate (PVP), holmium laser enucleation of the prostate (HoLEP), thulium laser enucleation of the prostate (ThuLEP), and UroLift. Furthermore, some studies have shown that there are favorable outcomes for using these new BPH surgical techniques instead of TURP [3,4,5,6].
In more detail, HoLEP and ThuLEP have demonstrated similar disobstruction outcomes with a comparable International Prostate Symptom Score (IPSS) improvement at both mid- and long-term follow-up, while similarly improving the overall quality of life (QoL) outcomes [7]. Despite these surgical options, which are still considered as possible alternatives (if the equipment and surgical expertise are available) according to international guidelines, the information regarding the safety profile resulting from the short- and long-term follow-up is in favor of laser-assisted enucleating or vaporesection techniques, making these a possible game changer in case of fragile patients or for those receiving anticoagulant or antiplatelet therapy [8]. Moreover, Salciccia et al. [9] have recently demonstrated how these new available endoscopic surgical techniques, including PVP, can be valid for an outpatient setting, thus, expanding the potentiality of application and the wide distribution of the techniques when compared to TURP.
However, these newer modalities, in many cases, may be far more expensive than traditional TURP, and there are few contemporary studies that analyze and compare these costs [10]. Moreover, we have few data regarding the total overall costs incurred from the BPH workup utilized to confirm the need for surgical treatment. Therefore, the aim of our study is to present the annual rates of BPH surgery and to analyze recent trends in the utilization of newer surgical modalities and any changes in medical costs related to these treatments over a 15-year period in the U.S.
2. Materials and Methods
The current study was performed with approval from the Center for Population Health Science at Stanford University in the U.S. Patient data collected from the Optum Clinformatics Data Mart Claims Database were derived from commercial and Medicare Advantage health insurance claims. Optum Clinformatics Data Mart is a database comprised of administrative health claims submitted for payment by providers and pharmacies. These claims are verified, adjudicated, adjusted, and de-identified. Data are included for only those covered lives, roughly 70 million over a 14-year period, with both medical and prescription drug coverage. Costs are standardized to create standard prices across all provider services. International Classification of Disease Ninth and Tenth Revisions, Clinical Modification (ICD-9-CM, ICD-10-CM) codes, and Current Procedural Terminology (CPT) codes were used to identify the study cohort, treatments, and comorbidities. A comprehensive list of ICD-9/10 and CPT codes summarizing the analytical steps for the data analysis and inclusion/exclusion criteria are presented in Supplementary File S1. This method has been used in other studies [11,12,13,14], and, given de-identified information, this study was deemed exempt from informed consent requirements by the Stanford University Medical Center Institutional Review Board.
Patients who had undergone BPH surgery (index date) between 2004 and 2017 in the U.S. were reviewed. As per primary aim, only those patients with an associated code for specific BPH surgical procedure were included (i.e., TURP, HoLEP, ThuLEP, UroLift). Trends and distribution over the years of enrolment were analyzed and reported for each single procedure over the time of database enrolment across the U.S. Moreover, as per inclusion criteria, subjects at least 50 years old, with at least 6 months enrolment time before, and 1 month after the index date were further assessed leading to the final of n = 82,458 men. Additionally, patients were considered eligible per final enrolment, only if they had a least one urodynamic, cystourethroscopy, USG, biopsy, uroflowmetry, or surgical urological procedure treatment code. Overall, this led to the final cohort composition of n = 51,448 men.
Per the secondary aim of the study, we reviewed the trends in adoption of various diagnostic methods for BPH including urodynamic studies, cystourethroscopy, transrectal ultrasound, prostatic biopsy, uroflowmetry, and the measurement of post-void residual urine volume (PVR). The collected data included patient age, race, household income, educational status, and co-morbidities. In addition, the annual costs of BPH diagnostic and treatment modalities were reviewed from the database for both diagnostic and therapeutic BPH-related procedures. All costs were standardized based on Medicare Relative Value Units and other pricing methods, adjusting for inflation. Finally, incidental diagnoses of prostate cancer (PCa) detected during BPH procedures were recorded over the years to depict the trends in cancer detection and the median prostate specific antigen (PSA) values associated with BPH patients ultimately addressed to surgical disobstruction.
Statistical Analysis
Patient demographics and the socio-economic and clinical characteristics for those who received diagnostic and/or therapeutic BPH-related procedures were summarized by mean values (standard deviation (SD)), or median values (inter-quartile range (IQR)). Temporal trends with descriptive statistics on the adoption of each explored diagnostic procedure for BPH were presented to assess the number of cases by year and the relative percentages of each adopted procedure. Additionally, temporal trends in median cost per diagnosis and/or treatment were presented and plotted to show the yearly trajectory of the different procedures reviewed. Incidental PCa findings and associated PSA values were recorded and compared by temporal trends.
3. Results
The overall number of subjects reviewed included 51,448 patients. Table 1 shows the patients’ characteristics of age, race, household incomes, and educational status by BPH surgery year.

Table 1.
Annual characteristics of patients undergoing benign prostatic hyperplasia surgery.
The majority of patients were White. Interestingly, both the lowest and highest household incomes each carried a high proportion of all BPH patients. The mean age for BPH surgical patients gradually increased annually from 67.6 years in 2004 to 73.4 in 2017.
Table 2 indicates a slight increase in the cost of BPH diagnostic tools.

Table 2.
Annual numbers and costs of diagnostic procedures.
Apart from the stationary cost of diagnosis, the total number of diagnostic approaches for determining BPH surgery has increased steadily (Figure 1).
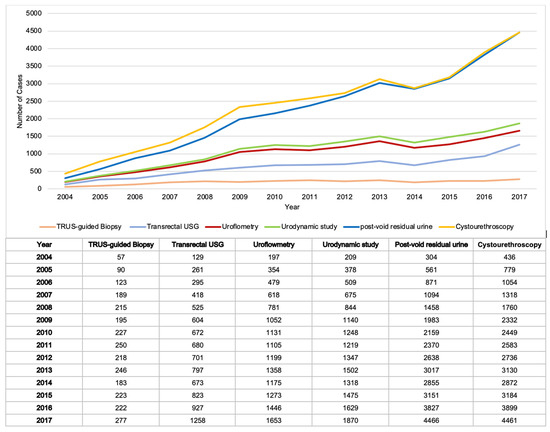
Figure 1.
Graph of annual numbers of diagnostic procedures.
Post-void residual urine and cystourethroscopy were among the diagnostic tools with the greatest increases over the study period, with post-void residual measurements increasing from 304 cases in 2004 to 4466 in 2007 and cystourethroscopy increasing from 436 cases in 2004 to 4461 in 2007. On the contrary, TRUS-guided biopsy was the procedure with the smallest amount of increase, going from 57 cases in 2004 to 277 in 2007.
In Table 3, recent changes in the surgical modalities for treating BPH have been identified.

Table 3.
Annual numbers and costs of surgical treatment.
The total number of treated cases was 31,801, 20,313, 2061, 1280, and 507 for TURP, PVP, HOLEP/ThULEP, Urolift, and ASC, respectively. Although there is still an annual increasing trend in the total number of cases for which TURP is the method of BPH treatment, the proportion of those undergoing TURP demonstrates an annually decreasing trend. Among BPH laser surgeries, PVP has been the most-common modality since 2017 (Figure 2).
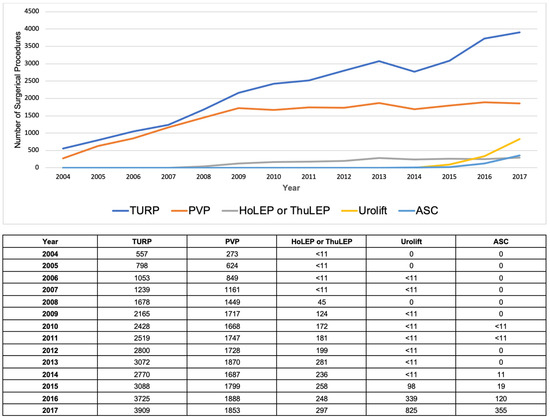
Figure 2.
Graph of annual numbers of surgical procedures.
The total number of BPH diagnosis was 44,820, and the median cost for each procedure was USD 1459, USD 1875, USD 1419, USD 3284, and USD 3590 for TURP, PVP, HOLEP/ThULEP, Urolift, and ASC, respectively. The median overall cost was USD 2471. With regard to the costs of treating BPH surgically, the diagnostic and treatment costs demonstrate annual increases, as shown in Table 4, with the slope of costs becoming steeper in the last 4 years (Figure 3).

Table 4.
Annual overall medical costs related to surgery.
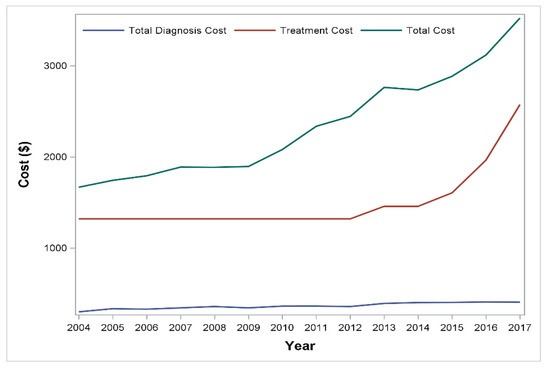
Figure 3.
Graph of annual medical costs related to surgery.
Between 2007 and 2012, the number of incidentally detected prostate cancer diagnoses during BPH surgery for which PSA data was available was very low; therefore, the rate of cancer detection between 2007 and 2012 could not be estimated. However, in comparing the outcomes of cancer detection in 2004 to those in 2017, the probability of incidentally detected prostate cancer during surgery demonstrated an annual decrease, as shown in Table 5.

Table 5.
Analysis of incidentally detected prostate cancer.
4. Discussion
The increase in average life expectancy results in a greater occurrence of functional disorders in aging male patients, with BPH representing one of the most-common and bothersome diseases of aging males, creating an adverse effect on patients’ quality of life. Moreover, lower urinary tract symptoms are strongly associated with aging. This was clearly demonstrated in different series and countries, including the Florey Adelaide Male Ageing Study from Australia, where there was a marked effect of age, with 31.5% of men aged 70–80 years reported some degree of bothersome LUTS, compared to 13.4% of the youngest-aged men in the cohort [15]. While some functional decline of the lower urinary tract undoubtedly occurs, with aging being an independent predictor, some other risk factors indirectly correlated with aging processes, such as abdominal fat mass, plasma glucose, obstructive sleep apnea, HDL cholesterol, and energy intake may produce an incremental effect on the intensity of the symptoms, thus potentially shortening the time to the need for surgical management [16]. Additionally, Stroup et al. investigated the adverse events related to BPH in the U.S. from 1998 to 2008 and reported significant sequelae, including acute renal failure, bladder stones, and urinary retention [17].
For BPH treatment, there are several options—medical, surgical, and procedural management [18,19]. In general, surgical treatment is utilized in medically refractory BPH and TURP and has been the traditional gold standard of surgical treatment [20,21]. However, newer procedures have recently come to the forefront, with some suggesting that HoLEP is potentially a new gold standard of BPH surgery, as it can also treat obstruction caused by high-intensity focused ultrasound (HIFU) treatment for prostate cancer [22,23]. Recently, UroLift was introduced as a minimally invasive, office-based treatment for BPH, which has shown favorable surgical outcomes [24,25]. Although we demonstrate that TURP is still the most-common surgery to treat BPH in the U.S. (Figure 2), the number of UroLift procedures has increased remarkably in recent years. The total medical costs related to BPH surgery demonstrate an annual increase, likely from increasing costs of non-TURP options, and it remains to be seen if this trend continues, as other alternative procedures continue with more widespread adoption.
There are some interesting trends worth mentioning during the study period. With regards to age, the mean age of those who underwent BPH surgery demonstrated a gradual increase from 67.4 years old in 2004 to 73.4 years old in 2017 (Table 1). In terms of racial differences, we find no disparity among races, which supports the results from a previous study [26]. The increasing age of patients undergoing procedural intervention may reflect increasing safety in BPH treatments and greater efficacy of medical treatments, with the decision of clinicians to delay the need for surgical intervention until later in the disease course.
The diagnostic workup prior to BPH procedural management and the studies used are not standardized, so controversy exists regarding what is necessary. These studies include post-void residual measurement, urodynamics, cystourethroscopy, and transrectal ultrasound [27]. We find that cystourethroscopy is the most-common diagnostic tool prior to surgery. The second-most-common diagnostic tool is a PVR, and two-thirds of patients in our study underwent both cystourethroscopy and a PVR. These studies showed consistency throughout the study period and as such, costs of this workup remained low and stable.
Our study also demonstrates a steady decrease in the detection of incidental prostate cancer. Several studies have also reported a decrease in incidentally detected prostate cancer due to earlier PSA screening [18,28]. In terms of incidentally detected prostate cancer during BPH surgery, the detection rate reported by a selection of studies ranges from 21% to 4.8% [18]. The reasons for the decrease in incidental diagnoses are not clear, but there are a couple of possible reasons. It may be that the more-frequent use of an MRI to detect occult prostate cancer prior to BPH procedures has resulted in more upfront prostate cancer diagnoses, requiring more radical treatment. Moreover, the higher utilization of procedures that do not submit tissue for pathologic diagnosis such as PVP or Urolift could also lower the incidental detection rate.
Several limitations of the present study warrant mention. As the dataset is administrative in nature, relying on accurate coding of diagnoses and procedures, there is a possibility of misclassification. Additionally, procedures done prior to access to insurance and entry into the database may not have been captured. In addition, in keeping with the administrative nature of the dataset, no staging or information regarding BPH including prostate volume, catheterization time, and/or indolent vs. non-indolent incidental PCa diagnosis were available, which could limit our ability to assess the indication for surgical excision and related oncological outcomes. Despite the limitations, our study provides an analysis of population-based data previously not studied, revealing important clinical information about changing trends in the surgical management of BPH in the U.S. To the best of our knowledge, this unique insight contributes to the comprehensive understanding of overall recent U.S. trends in the surgical treatment of BPH in real clinical practice across the country.
5. Conclusions
Our study demonstrates that TURP is still the most-common surgical treatment of BPH in the U.S. However, there is a rising trend in the number of BPH cases that are treated with alternative surgical methods in place of TURP. Furthermore, the total medical costs related to surgical treatment are also increasing. Future studies with long-term follow-up should assess whether these newer options are indeed cost-effective.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/app12178697/s1.
Author Contributions
Conceptualization, F.D.G., J.K.O., W.K. (Wansuk Kim), A.S, S.S., S.L. (Shufeng Li) and B.I.C.; data curation, F.D.G., J.K.O., S.B., E.N., P.H.S., W.K. (Wansuk Kim), S.Y.K., G.E.M., K.H.Y., H.J.C., S.L. (Sinyeong Lee), E.D.B., C.M.S., B.P., W.K. (Wojciech Krajewski), A.G., M.F., F.C., R.A., F.B., A.M., G.M.B., S.L. (Shufeng Li), S.C. and B.I.C.; formal analysis, F.D.G., J.K.O., S.B., K.H.Y., H.J.C., S.L. (Sinyeong Lee), S.S., E.D.B., V.A., C.M.S., B.P., W.K. (Wojciech Krajewski), M.F., F.C., R.A., F.B., A.M., G.M.B., S.L. (Shufeng Li), S.C. and B.I.C.; investigation, J.K.O., S.B., P.H.S., W.K. (Wansuk Kim), S.Y.K., H.J.C., S.S., W.K. (Wojciech Krajewski), M.F., F.B., A.M., S.L. (Shufeng Li), S.C. and B.I.C.; methodology, J.K.O., E.N., P.H.S., G.E.M., K.H.Y., S.L. (Sinyeong Lee), A.S., V.A., C.M.S., B.P., W.K. (Wojciech Krajewski), A.G., M.F., F.C., S.D.P., F.B., G.M.B., S.L. (Shufeng Li) and B.I.C.; supervision, F.D.G., A.S., E.D.B., A.M., S.L. (Shufeng Li), S.C. and B.I.C.; validation, S.Y.K., S.L. (Shufeng Li) and B.I.C.; visualization, G.E.M. and V.A.; writing—original draft, F.D.G., S.D.P., R.A., S.L. (Shufeng Li) and B.I.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not available.
Informed Consent Statement
Not available.
Data Availability Statement
Not available.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Shimizu, S.; Tsounapi, P.; Shimizu, T.; Honda, M.; Inoue, K.; Dimitriadis, F.; Saito, M. Lower urinary tract symptoms, benign prostatic hyperplasia/benign prostatic enlargement and erectile dysfunction: Are these conditions related to vascular dysfunction? Int. J. Urol. 2014, 21, 856–864. [Google Scholar] [PubMed]
- Das, A.K. Techniques and innovative technologies for the treatment of BPH. Can. J. Urol. 2019, 26, 1. [Google Scholar]
- Huang, S.W.; Tsai, C.Y.; Tseng, C.S.; Shih, M.C.; Yeh, Y.C.; Chien, K.L.; Pu, Y.S.; Tu, Y.K. Comparative efficacy and safety of new surgical treatments for benign prostatic hyperplasia: Systematic review and network meta-analysis. BMJ 2019, 367, l5919. [Google Scholar] [PubMed]
- Busetto, G.M.; Del Giudice, F.; D’Agostino, D.; Romagnoli, D.; Minervini, A.; Rocco, B.; Antonelli, A.; Celia, A.; Schiavina, R.; Cindolo, L.; et al. Efficacy and safety of Finasteride (5 alpha-reductase inhibitor) monotherapy in patients with benign prostatic hyperplasia: A critical review of the literature. Arch. Ital. Urol. Androl. 2020, 91, 205–210. [Google Scholar] [CrossRef]
- Kim, J.H.; Shim, S.R.; Khandwala, Y.; Del Giudice, F.; Sorensen, S.; Chung, B.I. Risk of Depression after 5 Alpha Reductase Inhibitor Medication: Meta-Analysis. World J. Men’s Health 2020, 38, 535–544. [Google Scholar] [CrossRef]
- Busetto, G.M.; Del Giudice, F.; Maggi, M.; Antonini, G.; D’Agostino, D.; Romagnoli, D.; Del Rosso, A.; Giampaoli, M.; Corsi, P.; Palmer, K.; et al. Surgical blood loss during holmium laser enucleation of the prostate (HoLEP) is not affected by short-term pretreatment with dutasteride: A double-blind placebo-controlled trial on prostate vascularity. Aging 2020, 12, 4337–4347. [Google Scholar] [CrossRef]
- 7. EAU Guidelines. Management of Non-Neurogenic Male Lower Urinary Tract Symptoms (LUTS), incl. Benign Prostatic Ob-struction (BPO) E. Available online: https://uroweb.org/guidelines/management-of-non-neurogenic-male-luts (accessed on 1 August 2022).
- Gravas, S. Hot Topics in the Clinical Practice Guidelines for Treatment of Male Lower Urinary Tract Symptoms due to Benign Prostatic Obstruction. Eur. Urol. Focus 2022, 8, 396–398. [Google Scholar] [CrossRef]
- Salciccia, S.; Del Giudice, F.; Maggi, M.; Eisenberg, M.L.; Chung, B.I.; Conti, S.L.; Kasman, A.M.; Vilson, F.L.; Ferro, M.; Lucarelli, G.; et al. Safety and Feasibility of Outpatient Surgery in Benign Prostatic Hyperplasia: A Systematic Review and Meta-Analysis. J. Endourol. 2021, 35, 395–408. [Google Scholar] [CrossRef]
- DeWitt-Foy, M.E.; Gill, B.C.; Ulchaker, J.C. Cost Comparison of Benign Prostatic Hyperplasia Treatment Options. Curr. Urol. Rep. 2019, 20, 45. [Google Scholar] [CrossRef]
- Chung, K.J.; Kim, J.H.; Min, G.E.; Park, H.K.; Li, S.; Del Giudice, F.; Han, D.H.; Chung, B.I. Changing Trends in the Treatment of Nephrolithiasis in the Real World. J. Endourol. 2019, 33, 248–253. [Google Scholar] [CrossRef]
- Cheung, H.; Wang, Y.; Chang, S.L.; Khandwala, Y.S.; Del Giudice, F.; Chung, B.I. Adoption of Robot-Assisted Partial Nephrectomies: A Population-Based Analysis of U.S. Surgeons from 2004 to 2013. J. Endourol. 2017, 31, 886–892. [Google Scholar] [CrossRef] [PubMed]
- Del Giudice, F.; van Uem, S.; Li, S.; Vilson, F.L.; Sciarra, A.; Salciccia, S.; Busetto, G.M.; Maggi, M.; Tiberia, L.; Viscuso, P.; et al. Contemporary Trends of Systemic Neoadjuvant and Adjuvant Intravesical Chemotherapy in Patients With Upper Tract Urothelial Carcinomas Undergoing Minimally Invasive or Open Radical Nephroureterectomy: Analysis of US Claims on Perioperative Outcomes and Health Care Costs. Clin. Genitourin. Cancer 2021, 20, 198.e1–198.e9. [Google Scholar] [CrossRef]
- Chung, B.I.; Leow, J.J.; Gelpi-Hammerschmidt, F.; Wang, Y.; Del Giudice, F.; De, S.; Chou, E.P.; Song, K.H.; Almario, L.; Chang, S.L. Racial Disparities in Postoperative Complications After Radical Nephrectomy: A Population-based Analysis. Urology 2015, 85, 1411–1416. [Google Scholar] [CrossRef] [PubMed]
- Martin, S.A.; Members of the Florey Adelaide Male Ageing Study; Haren, M.T.; Marshall, V.R.; Lange, K.; Wittert, G.A. Prevalence and factors associated with uncomplicated storage and voiding lower urinary tract symptoms in community-dwelling Australian men. World J. Urol. 2010, 29, 179–184. [Google Scholar] [CrossRef]
- Ng, M.; Baradhi, K.M. Benign Prostatic Hyperplasia. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar] [PubMed]
- Stroup, S.P.; Palazzi-Churas, K.; Kopp, R.; Parsons, J.K. Trends in adverse events of benign prostatic hyperplasia (BPH) in the USA, 1998 to 2008. Br. J. Urol. 2011, 109, 84–87. [Google Scholar] [CrossRef]
- Capogrosso, P.; Capitanio, U.; Vertosick, E.A.; Ventimiglia, E.; Chierigo, F.; Oreggia, D.; Moretti, D.; Briganti, A.; Vickers, A.J.; Montorsi, F.; et al. Temporal Trend in Incidental Prostate Cancer Detection at Surgery for Benign Prostatic Hyperplasia. Urology 2018, 122, 152–157. [Google Scholar] [CrossRef]
- Busetto, G.M.; Giovannone, R.; Antonini, G.; Rossi, A.; Del Giudice, F.; Tricarico, S.; Ragonesi, G.; Gentile, V.; De Berardinis, E. Short-term pretreatment with a dual 5α-reductase inhibitor before bipolar transurethral resection of the prostate (B-TURP): Evaluation of prostate vascularity and decreased surgical blood loss in large prostates. Br. J. Urol. 2014, 116, 117–123. [Google Scholar] [CrossRef]
- Lokeshwar, S.D.; Harper, B.T.; Webb, E.; Jordan, A.; Dykes, T.A.; Neal, D.E., Jr.; Terris, M.K.; Klaassen, Z. Epidemiology and treatment modalities for the management of benign prostatic hyperplasia. Transl. Androl. Urol. 2019, 8, 529–539. [Google Scholar] [PubMed]
- Sønksen, J.; Barber, N.J.; Speakman, M.J.; Berges, R.; Wetterauer, U.; Greene, D.; Sievert, K.-D.; Chapple, C.R.; Montorsi, F.; Patterson, J.M.; et al. Prospective, Randomized, Multinational Study of Prostatic Urethral Lift Versus Transurethral Resection of the Prostate: 12-month Results from the BPH6 Study. Eur. Urol. 2015, 68, 643–652. [Google Scholar] [CrossRef]
- Ene, C.; Geavlete, P.; Geavlete, B. What’s new in bipolar TURP for surgical management of BPH? Chirurgia 2020, 115, 307–313. [Google Scholar]
- Michalak, J.; Tzou, D.; Funk, J. HoLEP: The gold standard for the surgical management of BPH in the 21(st) Century. Am. J. Clin. Exp. Urol. 2015, 3, 36–42. [Google Scholar] [PubMed]
- Horiuchi, A.; Muto, S.; Horie, S. Holmium laser enucleation of the prostate followed by high-intensity focused ultrasound treat-ment for patients with huge prostate adenoma and localized prostate cancer: 5-year follow-up. Prostate Int. 2016, 4, 49–53. [Google Scholar] [PubMed]
- Christidis, D.; McGrath, S.; Perera, M.; Manning, T.; Bolton, D.; Lawrentschuk, N. Minimally invasive surgical therapies for benign prostatic hypertrophy: The rise in minimally invasive surgical therapies. Prostate Int. 2017, 5, 41–46. [Google Scholar] [CrossRef] [PubMed]
- Pettaway, C.A.; Lamerato, L.E.; Eaddy, M.T.; Edwards, J.K.; Hogue, S.L.; Crane, M.M. Benign prostatic hyperplasia: Racial differences in treatment patterns and prostate cancer prevalence. Br. J. Urol. 2011, 108, 1302–1308. [Google Scholar] [CrossRef]
- Braeckman, J.; Denis, L. Management of BPH then 2000 and now 2016–From BPH to BPO. Asian. J. Urol. 2017, 4, 138–147. [Google Scholar] [PubMed]
- Otto, B.; Barbieri, C.; Lee, R.; Te, A.E.; Kaplan, S.A.; Robinson, B.; Chughtai, B. Incidental Prostate Cancer in Transurethral Resection of the Prostate Specimens in the Modern Era. Adv. Urol. 2014, 2014, 627290. [Google Scholar] [CrossRef] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).