Meeting 24 h Movement Guidelines and Health-Related Quality of Life in Youths during the COVID-19 Lockdown
Abstract
:1. Introduction
2. Materials and Methods
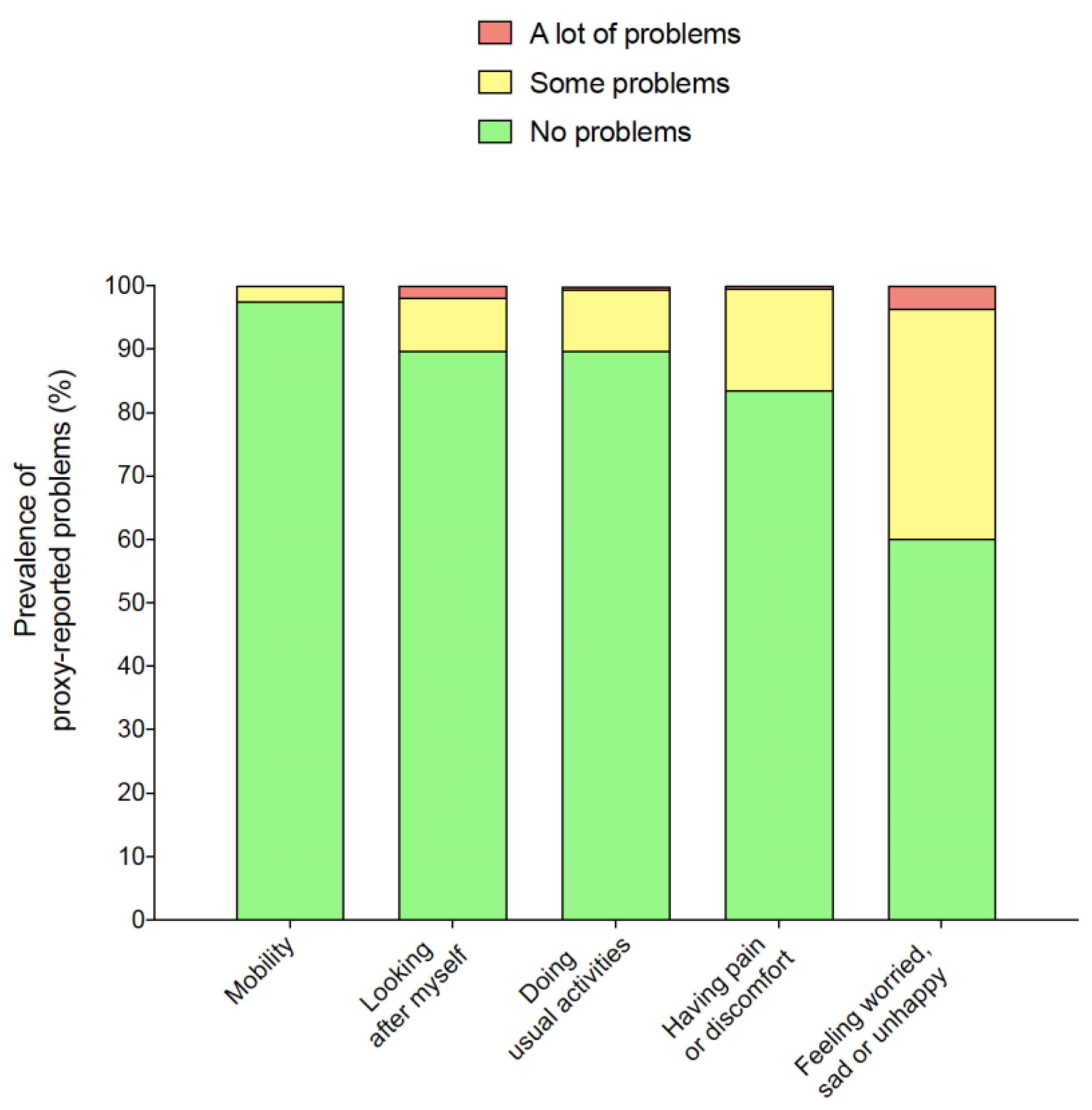
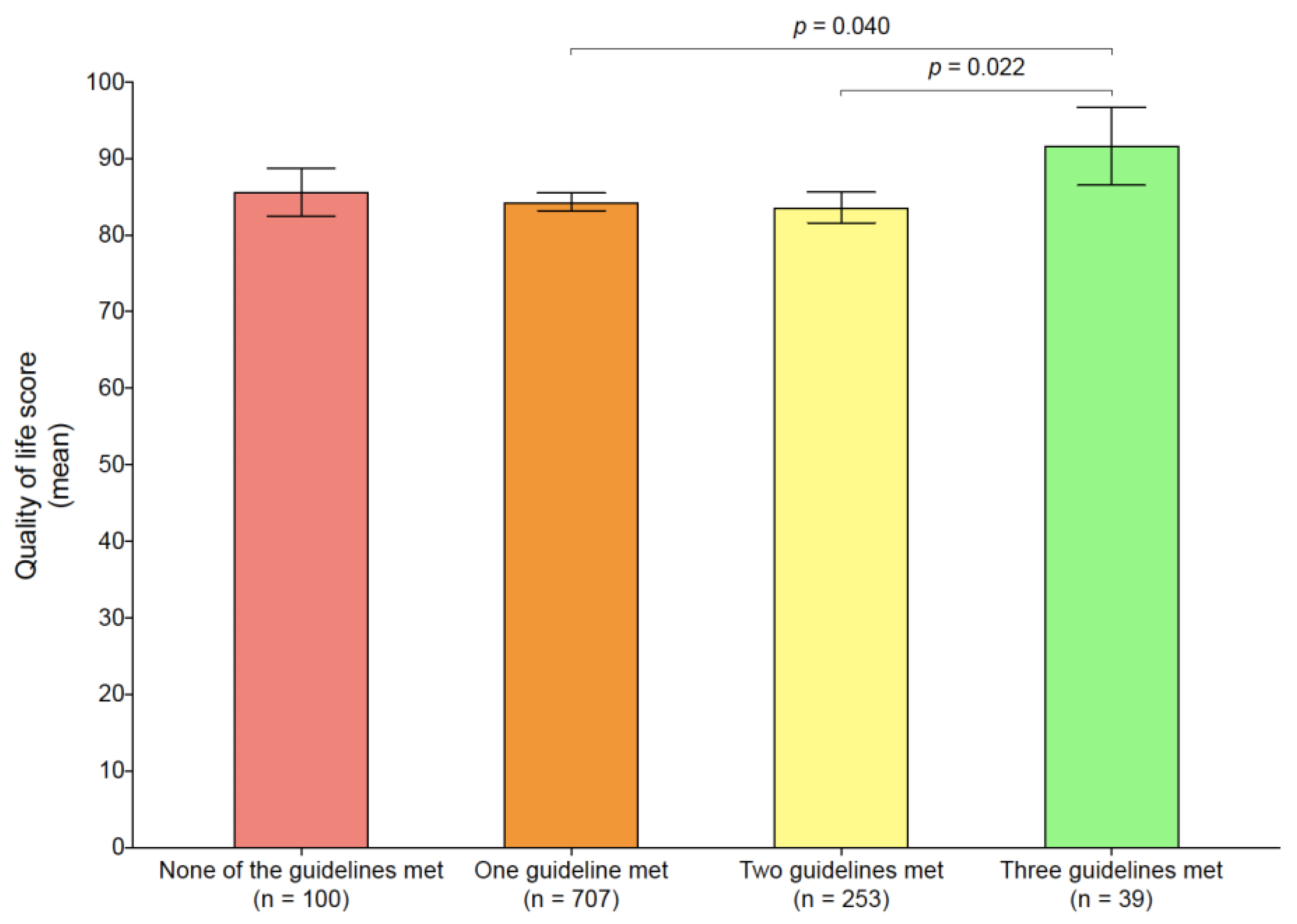
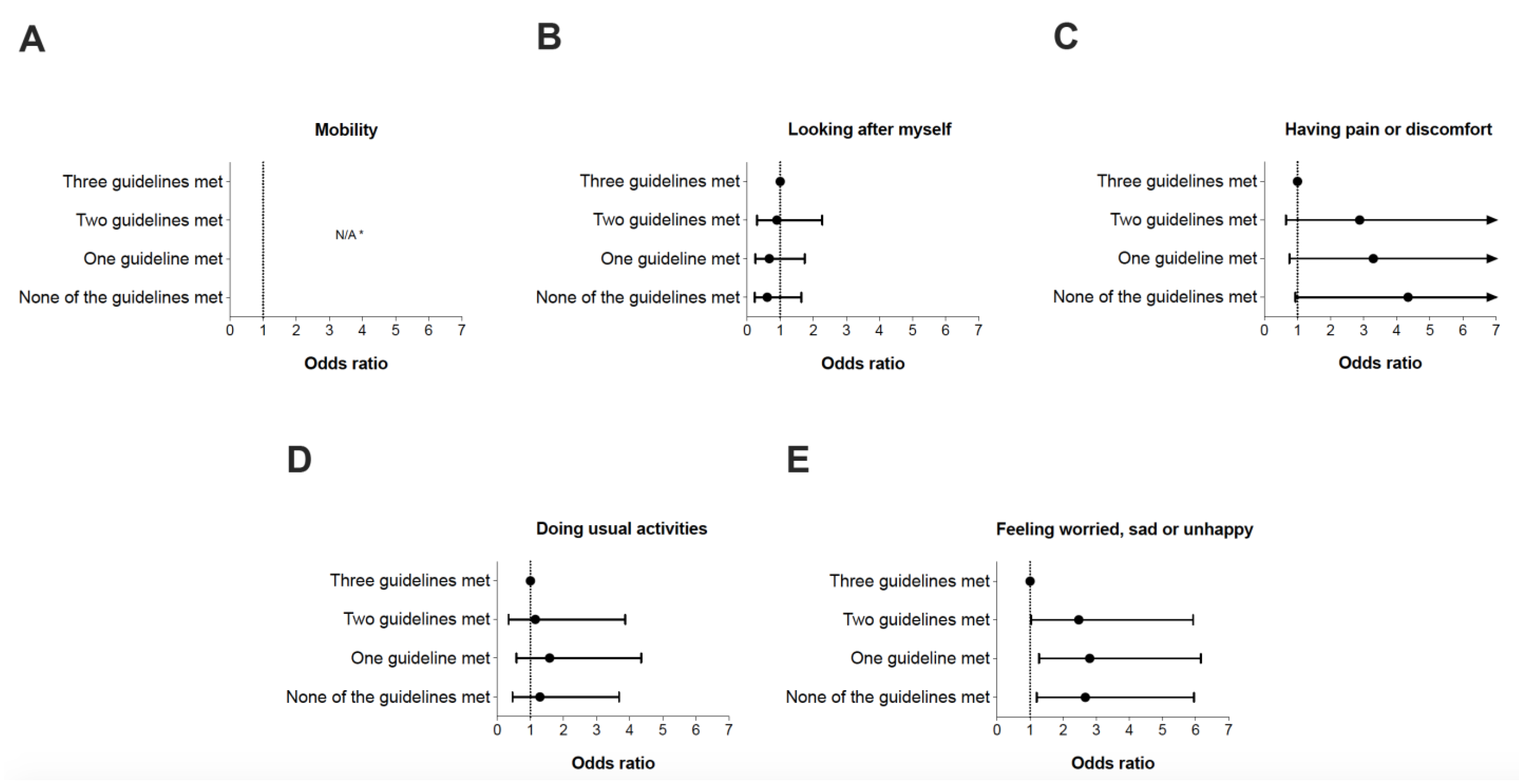
3. Results
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Coronavirus Disease 2019 (COVID-19): Situation Report-99; WHO: Geneva, Switzerland, 2020.
- Paterson, D.C.; Ramage, K.; Moore, S.A.; Riazi, N.; Tremblay, M.S.; Faulkner, G. Exploring the Impact of COVID-19 on the Movement Behaviors of Children and Youth: A Scoping Review of Evidence after the First Year. J. Sport Health Sci. 2021, 10, 675–689. [Google Scholar] [CrossRef]
- Tremblay, M.S.; Carson, V.; Chaput, J.-P.P.; Connor Gorber, S.; Dinh, T.; Duggan, M.; Faulkner, G.; Gray, C.E.; Grube, R.; Janson, K.; et al. Canadian 24-Hour Movement Guidelines for Children and Youth: An Integration of Physical Activity, Sedentary Behaviour, and Sleep. Appl. Physiol. Nutr. Metab. 2016, 41, S311–S327. [Google Scholar] [CrossRef]
- Khan, A.; Lee, E.-Y.; Tremblay, M.S. Meeting 24-h Movement Guidelines and Associations with Health Related Quality of Life of Australian Adolescents. J. Sci. Med. Sport 2021, 24, 468–473. [Google Scholar] [CrossRef] [PubMed]
- Xiong, X.; Dalziel, K.; Carvalho, N.; Xu, R.; Huang, L. Association between 24-Hour Movement Behaviors and Health-Related Quality of Life in Children. Qual. Life Res. 2022, 31, 231–240. [Google Scholar] [CrossRef] [PubMed]
- Vaquero-Solís, M.; Tapia-Serrano, M.A.; Hortigüela-Alcalá, D.; Jacob-Sierra, M.; Sánchez-Miguel, P.A. Health Promotion through Movement Behaviors and Its Relationship with Quality of Life in Spanish High School Adolescents: A Predictive Study. Int. J. Environ. Res. Public Health 2021, 18, 7550. [Google Scholar] [CrossRef]
- Carson, V.; Chaput, J.-P.; Janssen, I.; Tremblay, M.S. Health Associations with Meeting New 24-Hour Movement Guidelines for Canadian Children and Youth. Prev. Med. 2017, 95, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Tapia-Serrano, M.A.; Sevil-Serrano, J.; Sánchez-Miguel, P.A.; López-Gil, J.F.; Tremblay, M.S.; García-Hermoso, A. Prevalence of Meeting 24-Hour Movement Guidelines from Pre-School to Adolescence: A Systematic Review and Meta-Analysis Including 387,437 Participants and 23 Countries. J. Sport Health Sci. 2022, 11, 427–437. [Google Scholar] [CrossRef] [PubMed]
- The WHOQOL Group. The World Health Organization Quality of Life Assessment (WHOQOL): Position Paper from the World Health Organization. Soc. Sci. Med. 1995, 41, 1403–1409. [Google Scholar] [CrossRef]
- Varni, J.W.; Seid, M.; Kurtin, P.S. PedsQLTM 4.0: Reliability and Validity of the Pediatric Quality of Life InventoryTM Version 4.0 Generic Core Scales in Healthy and Patient Populations. Med. Care 2001, 39, 800–812. [Google Scholar] [CrossRef] [PubMed]
- Riley, A.W.; Spiel, G.; Coghill, D.; Döpfner, M.; Falissard, B.; Lorenzo, M.J.; Preuss, U.; Ralston, S.J.; ADORE Study Group. Factors Related to Health-Related Quality of Life (HRQoL) among Children with ADHD in Europe at Entry into Treatment. Eur. Child Adolesc. Psychiatry 2006, 15, i38–i45. [Google Scholar] [CrossRef]
- Sampasa-Kanyinga, H.; Standage, M.; Tremblay, M.S.; Katzmarzyk, P.T.; Hu, G.; Kuriyan, R.; Maher, C.; Maia, J.; Olds, T.; Sarmiento, O.L.; et al. Associations between Meeting Combinations of 24-h Movement Guidelines and Health-Related Quality of Life in Children from 12 Countries. Public Health 2017, 153, 16–24. [Google Scholar] [CrossRef]
- Nobari, H.; Fashi, M.; Eskandari, A.; Villafaina, S.; Murillo-Garcia, Á.; Pérez-Gómez, J. Effect of COVID-19 on Health-Related Quality of Life in Adolescents and Children: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 4563. [Google Scholar] [CrossRef] [PubMed]
- Currie, C.; Molcho, M.; Boyce, W.; Holstein, B.; Torsheim, T.; Richter, M. Researching Health Inequalities in Adolescents: The Development of the Health Behaviour in School-Aged Children (HBSC) Family Affluence Scale. Soc. Sci. Med. 2008, 66, 1429–1436. [Google Scholar] [CrossRef]
- World Health Organization. WHO Child Growth Standards: Length/Height-for-Age, Weight-for-Age, Weight-for-Length, Weight-for-Height and Body Mass Index-for-Age; Methods and Development; De Onis, M., Ed.; WHO Press: Geneva, Switzerland, 2006; ISBN 978-92-4-154693-5.
- Onis, M.; Onyango, A.W.; Borghi, E.; Siyam, A.; Nishida, C.; Siekmann, J. Development of a WHO Growth Reference for School-Aged Children and Adolescents. Bull. World Health Organ. 2007, 85, 660–667. [Google Scholar] [CrossRef]
- Prochaska, J.J.; Sallis, J.F.; Long, B. A Physical Activity Screening Measure for Use With Adolescents in Primary Care. Arch. Pediatr. Adolesc. Med. 2001, 155, 554. [Google Scholar] [CrossRef]
- Vicente-Rodríguez, G.; Rey-López, J.P.; Martín-Matillas, M.; Moreno, L.A.; Wärnberg, J.; Redondo, C.; Tercedor, P.; Delgado, M.; Marcos, A.; Castillo, M.; et al. Television Watching, Videogames, and Excess of Body Fat in Spanish Adolescents: The AVENA Study. Nutrition 2008, 24, 654–662. [Google Scholar] [CrossRef]
- World Health Organization. Guidelines on Physical Activity, Sedentary Behaviour, and Sleep for Children under 5 Years of Age; WHO Press: Geneva, Switzerland, 2019; ISBN 978-92-4-155053-6.
- Chervin, R.D.; Hedger, K.; Dillon, J.E.; Pituch, K.J. Pediatric Sleep Questionnaire (PSQ): Validity and Reliability of Scales for Sleep-Disordered Breathing, Snoring, Sleepiness, and Behavioral Problems. Sleep Med. 2000, 1, 21–32. [Google Scholar] [CrossRef]
- Wille, N.; Badia, X.; Bonsel, G.; Burström, K.; Cavrini, G.; Devlin, N.; Egmar, A.-C.; Greiner, W.; Gusi, N.; Herdman, M.; et al. Development of the EQ-5D-Y: A Child-Friendly Version of the EQ-5D. Qual. Life Res. 2010, 19, 875–886. [Google Scholar] [CrossRef]
- Gusi, N.; Perez-Sousa, M.A.; Gozalo-Delgado, M.; Olivares, P.R. Validez y fiabilidad de la versión proxy del EQ-5D-Y en español. An. Pediatría 2014, 81, 212–219. [Google Scholar] [CrossRef] [PubMed]
- Serra-Majem, L.; Ribas, L.; Ngo, J.; Ortega, R.M.; García, A.; Pérez-Rodrigo, C.; Aranceta, J. Food, Youth and the Mediterranean Diet in Spain. Development of KIDMED, Mediterranean Diet Quality Index in Children and Adolescents. Public Health Nutr. 2004, 7, 931–935. [Google Scholar] [CrossRef] [PubMed]
- Rollo, S.; Antsygina, O.; Tremblay, M.S. The Whole Day Matters: Understanding 24-Hour Movement Guideline Adherence and Relationships with Health Indicators across the Lifespan. J. Sport Health Sci. 2020, 9, 493–510. [Google Scholar] [CrossRef]
- Lubans, D.; Richards, J.; Hillman, C.; Faulkner, G.; Beauchamp, M.; Nilsson, M.; Kelly, P.; Smith, J.; Raine, L.; Biddle, S. Physical Activity for Cognitive and Mental Health in Youth: A Systematic Review of Mechanisms. Pediatrics 2016, 138, e20161642. [Google Scholar] [CrossRef] [PubMed]
- Fazeli, S.; Mohammadi Zeidi, I.; Lin, C.-Y.; Namdar, P.; Griffiths, M.D.; Ahorsu, D.K.; Pakpour, A.H. Depression, Anxiety, and Stress Mediate the Associations between Internet Gaming Disorder, Insomnia, and Quality of Life during the COVID-19 Outbreak. Addict. Behav. Rep. 2020, 12, 100307. [Google Scholar] [CrossRef] [PubMed]
- Knell, G.; Durand, C.P.; Kohl, H.W.; Wu, I.H.C.; Pettee Gabriel, K. Prevalence and Likelihood of Meeting Sleep, Physical Activity, and Screen-Time Guidelines Among US Youth. JAMA Pediatrics 2019, 173, 387. [Google Scholar] [CrossRef] [PubMed]
- McArthur, B.A.; Racine, N.; McDonald, S.; Tough, S.; Madigan, S. Child and Family Factors Associated with Child Mental Health and Well-Being during COVID-19. Eur. Child Adolesc. Psychiatry 2021. [Google Scholar] [CrossRef]
- Brown, D.M.Y.; Kwan, M.Y.W. Movement Behaviors and Mental Wellbeing: A Cross-Sectional Isotemporal Substitution Analysis of Canadian Adolescents. Front. Behav. Neurosci. 2021, 15, 736587. [Google Scholar] [CrossRef] [PubMed]
- López-Gil, J.F.; Roman-Viñas, B.; Aznar, S.; Tremblay, M.S. Meeting 24-h Movement Guidelines: Prevalence, Correlates, and Associations with Socioemotional Behavior in Spanish Minors. Scand. J. Med. Sci. Sports 2022, 32, 881–891. [Google Scholar] [CrossRef] [PubMed]
- Mitra, R.; Waygood, E.O.D.; Fullan, J. Subjective Well-Being of Canadian Children and Youth during the COVID-19 Pandemic: The Role of the Social and Physical Environment and Healthy Movement Behaviours. Prev. Med. Rep. 2021, 23, 101404. [Google Scholar] [CrossRef] [PubMed]
- Mireku, M.O.; Barker, M.M.; Mutz, J.; Dumontheil, I.; Thomas, M.S.C.; Röösli, M.; Elliott, P.; Toledano, M.B. Night-Time Screen-Based Media Device Use and Adolescents’ Sleep and Health-Related Quality of Life. Environ. Int. 2019, 124, 66–78. [Google Scholar] [CrossRef] [PubMed]
- Hysing, M.; Pallesen, S.; Stormark, K.M.; Jakobsen, R.; Lundervold, A.J.; Sivertsen, B. Sleep and Use of Electronic Devices in Adolescence: Results from a Large Population-Based Study. BMJ Open 2015, 5, e006748. [Google Scholar] [CrossRef] [PubMed]
| Variables | Participants (n = 1099) | ||
|---|---|---|---|
| M/n | SD/% | CI95% | |
| Age (years) | 11.5 | 4.5 | 11.2–11.8 |
| Pre-schoolers | 146 | 13.3 | 11.3–15.3 |
| Children | 444 | 40.4 | 37.5–43.3 |
| Adolescents | 509 | 46.3 | 43.4–49.3 |
| Sex | |||
| Males | 576 | 52.4 | 49.5–55.4 |
| Females | 523 | 47.6 | 44.6–50.5 |
| Nationality | |||
| Spanish | 604 | 55.0 | 52.0–57.9 |
| Brazilian | 495 | 45.0 | 42.1–48.0 |
| Breadwinner’s educational level | |||
| University studies | 538 | 49.0 | 46.0–51.9 |
| No university studies | 561 | 51.0 | 48.1–54.0 |
| Socioeconomic status a | |||
| Low SES | 362 | 32.9 | 30.2–35.7 |
| Medium SES | 529 | 48.1 | 45.2–51.1 |
| High SES | 208 | 18.9 | 16.6–21.2 |
| FAS-III (score) | 7.5 | 2.3 | 7.4–7.6 |
| Anthropometric data | |||
| Weight (kg) | 43.0 | 19.5 | 41.8–44.2 |
| Height (cm) | 145.5 | 24.8 | 144.0–147.0 |
| BMI (z-score) | 0.9 | 2.0 | 0.8–0.9 |
| Nutritional status b | |||
| Overweight/Obesity | 467 | 42.5 | 39.6–45.4 |
| KIDMED (score) | 7.0 | 2.4 | 6.9–7.1 |
| 24 h movement guidelines | |||
| Met all three recommendations | 39 | 3.5 | 2.5–4.6 |
| Did not meet all three recommendations | 1060 | 96.5 | 95.4–97.5 |
| HRQoL (score out of 100) | 84.5 | 15.9 | 83.6–85.4 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
López-Gil, J.F.; Tremblay, M.S.; Tapia-Serrano, M.Á.; Tárraga-López, P.J.; Brazo-Sayavera, J. Meeting 24 h Movement Guidelines and Health-Related Quality of Life in Youths during the COVID-19 Lockdown. Appl. Sci. 2022, 12, 8056. https://doi.org/10.3390/app12168056
López-Gil JF, Tremblay MS, Tapia-Serrano MÁ, Tárraga-López PJ, Brazo-Sayavera J. Meeting 24 h Movement Guidelines and Health-Related Quality of Life in Youths during the COVID-19 Lockdown. Applied Sciences. 2022; 12(16):8056. https://doi.org/10.3390/app12168056
Chicago/Turabian StyleLópez-Gil, José Francisco, Mark S. Tremblay, Miguel Ángel Tapia-Serrano, Pedro Juan Tárraga-López, and Javier Brazo-Sayavera. 2022. "Meeting 24 h Movement Guidelines and Health-Related Quality of Life in Youths during the COVID-19 Lockdown" Applied Sciences 12, no. 16: 8056. https://doi.org/10.3390/app12168056
APA StyleLópez-Gil, J. F., Tremblay, M. S., Tapia-Serrano, M. Á., Tárraga-López, P. J., & Brazo-Sayavera, J. (2022). Meeting 24 h Movement Guidelines and Health-Related Quality of Life in Youths during the COVID-19 Lockdown. Applied Sciences, 12(16), 8056. https://doi.org/10.3390/app12168056








