1. Introduction
A lateral cephalometric radiograph is a diagnostic tool that serves as a Gold Standard in assessing soft and hard tissue before an orthognathic surgery, using a list of standard-specific structures.
Orthodontic treatment planning also relies, among other factors, on cephalometric radiographs, as these have become one of the most critical tools in the diagnostic process [
1,
2].
Some of the structures seen in cephalometric radiographs are as follows [
1,
2,
3]:
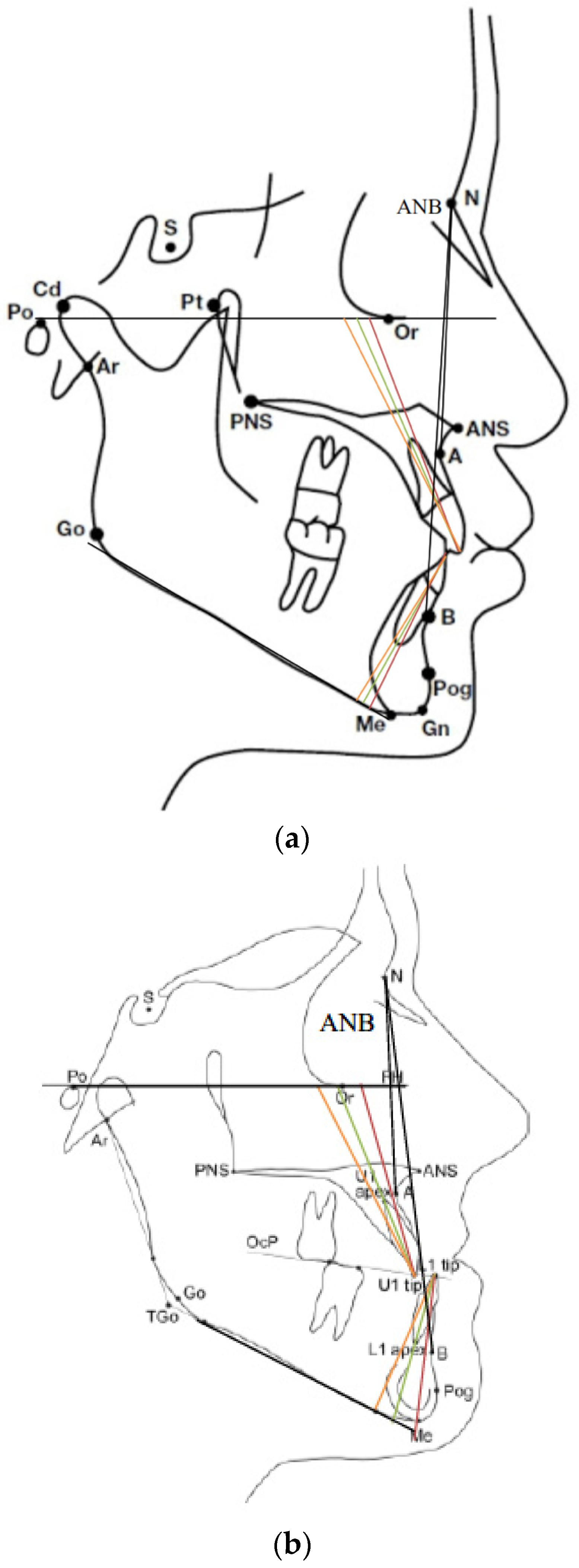
A Point: The most concave point anteriorly on the maxillary alveolar ridge;
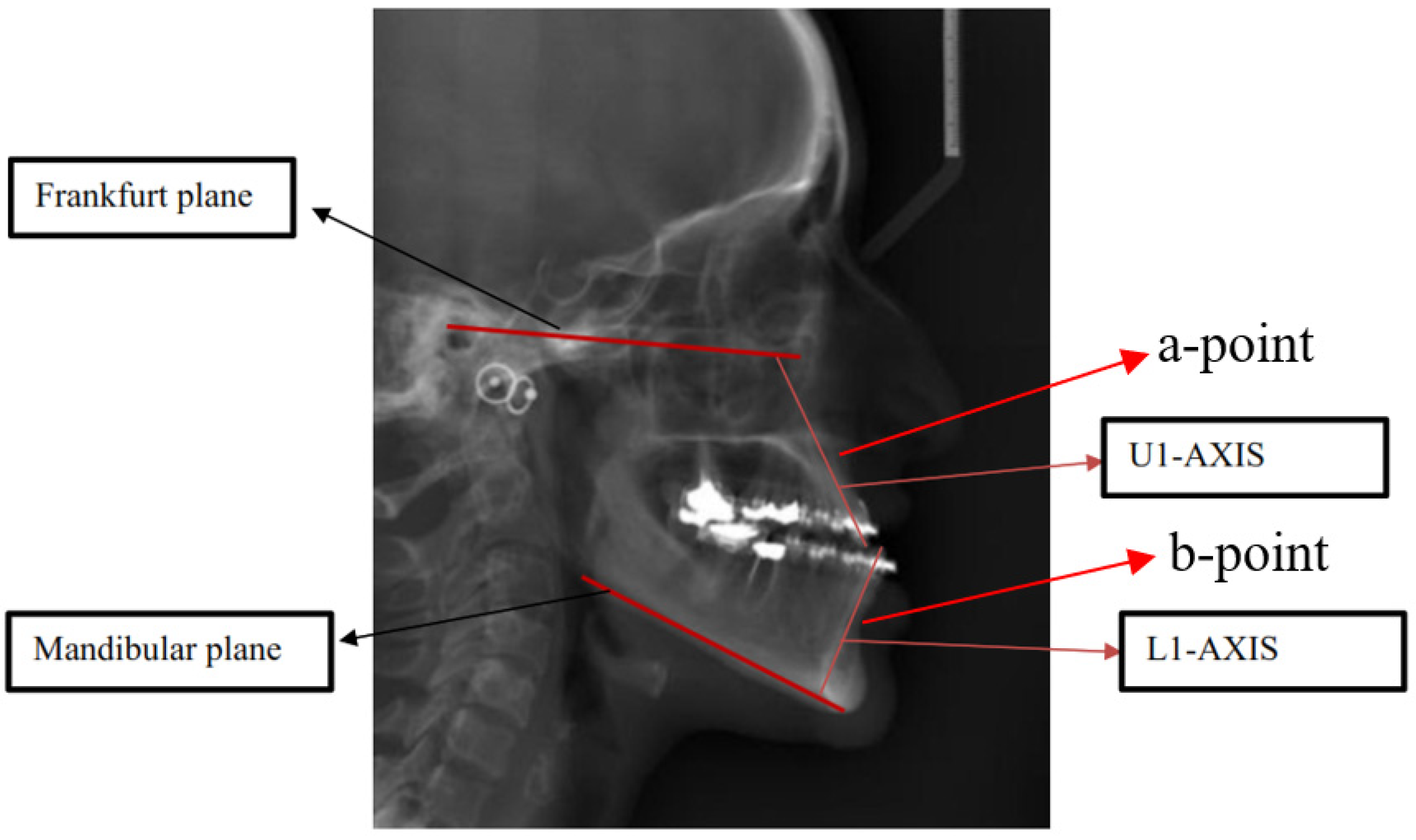
B Point: The most concave point of the profile from the Gonion to the mandibular alveolar ridge (
Figure 1);
Nasion (N): The most concave point on the frontonasal suture (
Figure 2).
According to Angle’s Classification of malocclusions, a Class-III occlusion is defined as a condition in which the mandibular first molar is positioned anterior to the maxillary molar without specifying the angle of the occlusal plane [
4,
5]. The classification of the initial occlusion did not reference the skeletal structure. Over the years, Angle’s Classification was extended, for diagnostic purposes, to facial structure classification as well:
Class-I: Orthognathic (straight) profile, demonstrating two normally and harmoniously developed jaws, where dentition is also set according to Angle’s Class-I relations as specified above (
Figure 3a).
The skeletal class I is considered if two of the following are the case:
0.3 < ANB < 4.8;
0 < Overjet < 5.0;
−1.3 < Wits < 2.4.
Angle Class I Molar/canine in one side, 170 < profile < 178;
Class-II: underdeveloped mandible relative to the maxilla. A prognathic (convex) profile;
The skeletal class II is considered if 2 of the following are the case:
ANB > or =4.8;
Overjet > or =5.0;
Wits > or =2.4.
Angle Class II Molar/canine in one side, convex profile < or =170;
Class-III: Underdeveloped mandible relative to the maxilla and/or overdeveloped mandible relative to the maxilla, including asymmetries [
7] [
Figure 3b]:
The skeletal class I is considered if 2 of the following are the case:
ANB < or =0.3;
Overjet < or =0;
Wits < or =−1.3.
Angle Class III Molar/canine in one side, concave profile > or =178;
In this paper, we chose to focus on Class-III Skeletal Deformities; therefore, we wish to specify that, in such cases, it is essential first to diagnose the nature of the defect, as well as the abnormal jaw: whether the mandible is overdeveloped or instead the maxilla is underdeveloped or both options are combined. Making such a diagnosis, in addition to the clinical examination, relies on cephalometric analysis. Various indices facilitate the assessment of mandibular or maxillary deviation from the norm relative to the base of the skull. One of the traditional indices is Steiner’s Index, which measures the position of the jaws relative to the base of the skull: checking whether their position reflects normal development and, if not, the severity of the defect [
8].
The surgical treatment in such cases is a mandibular setback, maxillary advancement, or a combination of both, respective of facial cephalometric radiograph analysis findings, study models, and the patient’s complaint [
9].
Patients with Class-III facial structure usually demonstrate characteristics of natural dental or dentoalveolar compensation at the time of their admittance. This is expressed in the proclination of the maxillary incisors and retroclination of mandibular incisors. These angles are measured relative to the accepted reference lines, FH and NA for maxillary teeth, and NB and MP for mandibular teeth.
These abnormal tendencies facilitate better functions and help disguise dentofacial deformity. Diagnosing compensatory severity is also based on the calculation of the longitudinal axis of Upper incisor U1 and Lower incisor L1 relative to the FH and MP planes, respectively, using Steiner’s cephalometric radiograph analysis (
Figure 1).
When surgical treatment is planned, one should act to eliminate the existing natural or orthodontic dental compensation and exacerbate the dental gap to make it compatible with the skeletal opening [
10].
Therefore, the ortho-surgical treatment of Class-III deformities comprises orthodontic preparation, a surgical correction, and, subsequent to recovery from surgery, final orthodontic involvement for occlusal processing. The pre-operation orthodontic preparation should be coordinated with the surgical plan so that normal occlusion is achieved upon the completion of the surgical action.
Incomplete or imperfect correction of compensation of the maxillary and mandibular incisors may impact both the quality of the skeletal result and the quality of the final occlusion result of the surgery [
11,
12].
2. Materials and Methods
After receiving the approval of the Tel-Aviv University Ethics Committee, 100 cephalometric radiographs were collected from radiography centers and 50 of those radiographs were of patients with normal facial structures (Class-I = Orthognathic) and the other 50 radiographs were of patients with specific skeletal deformities as radiographed before their orthodontic preparation before surgery began. Radiograph inclusion criteria were as follows (Relative Class-III = Prognathic): lack of previous orthodontic treatment and the absence of syndromes, including Cleft Palate. The cases selected were in the age range of 20–30, characteristic of the age of Ortho-Surgery patients. All personal data were erased from the radiographs by the experimenter. Subsequently, two lines signifying the Frankfort Horizontal Plane and the Inferior Border of the Mandibular Plane, as well as reference points (B) point, (A) point, and (N) Nasion, were drawn on all 100 radiographs (
Figure 2). The severity of the deformity was calculated according to Steiner’s Analysis as the angle between points A and B and Point N [
13]. Next, the researcher provided the 100 radiographs in random order (not according to the skeletal diagnosis of the patient) to each of the participants. Demonstration and instruction were provided to all participating physicians, after which each participant marked the longitudinal axis of the upper incisor (U1) relative to the Frankfort Horizontal Plane (FH) and the longitudinal axis of the lower incisor (L1) relative to the Inferior Border of the Mandibular Plane (MP) on all 100 radiographs.
After all the above-mentioned marked presentations were obtained, the following angles were calculated respective to the different markings:
U1 TO FRANKFURT PLANE;
L1 TO MANDIBULAR PLANE;
U1 TO NA;
L1 TO NB;
ANB.
Angle calculation was performed using the Cephninja
® angle calculation application, and the results were gathered and maintained in a separate table for each participant. After all angle results were collected, they were statistically analyzed with SPSS
®IBM software to calculate the average Standard Error in each measurement among the different examiners (SE). (
Table 1) Next, a statistical analysis (
t-test) and Bonferroni correction for multiple comparisons between the Class-I patient group (Orthognathic) and the Class-III patient group (Prognathic) were performed:
U1 TO FRANKFURT PLANE (Class-III versus Class-I);
L1 TO MANDIBULAR PLANE (Class-III versus Class-I);
U1 TO NA (Class-III versus Class-I);
L1 TO NB (Class-III versus Class-I).
Pearson’s correlation was conducted between ANB versus STD results in each one of the groups.
3. Results
The results are summarized in
Table 1:
The variability of the U1-NA angle in Class-III is higher than the variability of U1-NA in Class-I
p = 0.00, df = 1, t(49) = −5.019 (
Figure 4).
The variability of angle L1-NB in Class-III is higher than that of L1-NB in Class-I
p = 0.02, d f= 1, t(49) = −2.879 (
Figure 4).
The variability of angle L1 to MP in Class-III is higher than that of Class-I
p = 0.014, df = 1, t(49) = −2.803 (
Figure 4).
The variability of angle U1 To FH was higher than that of Class-I
p = 0.026, df = 1, t(49) = −2.57 (
Figure 4 and
Figure 5).
4. Discussion
Class-III dentofacial deformities are intermaxillary skeletal gaps treated by Orthognathic surgery [
8]. In 1980, Bell, Proffitt, and white conducted a study concerning the surgical treatment in such cases and showed how determining a surgical treatment plan (mandibular setback or maxillary advancement or a combination of the two) is based on the analysis of facial cephalometric radiographs, model analysis, and the patient’s complaint [
13].
In 2009, Beth A Troy showed the importance of orthodontic treatment before the surgical procedure for de-compensation and after the surgical procedure for achieving optimal occlusion [
10].
Patients with Skeletal Class- III usually present a narrow maxilla; as part of presurgical treatment, the patients undergo treatment with SARPE (surgically assisted rapid palatal expansion) [
14].
In Kazumi Ohkubo’s study in 2016, the authors show the importance of calculating the angle of the incisors relative to jaw bases for planning Presurgical Operations (PSOs) according to the obtained values. In 2016, Jitesh Haryani maintained that, in cases where the Proclination of upper incisors is large, the extraction of premolars should be considered to achieve enough space for the correction of the incisor proclination and for decompensation of the maxillary teeth.
H.S. Baik 2000 shows that orthodontists need to be aware of the potential restriction and that an accurate analysis of the cephalometric radiograph is required to plan a proper course of treatment [
9,
15].
However, the condition in the mandible is different: In most prognathic cases, no extraction of mandibular teeth is performed, and de-compensation can be achieved without extractions [
16]. The mandibular incisors are usually in a lingual position and the purpose of de-compensation, in this case, is to return them to a more buccal position [
15,
16].
Therefore, cephalometric measurements are essential for correctly diagnosing and planning a combined ortho-surgical treatment. An accurate diagnosis of the angles of the incisors is part of the modus operandi on which the entire planning process of combined therapy of maxillofacial deformities is based [
1,
9].
In 2013, Do-Keun Kim emphasized the importance of planning surgeries and making decisions regarding the extraction of premolars. He showed that the values obtained through calculating angles in the cephalometric radiograph are essential parameters for making such decisions [
17].
Naturally, miscalculating these angles may lead to an incorrect decision. The more severe the deformity and the more radical the action needed, the less accurate the values obtained in the cephalometric analysis regarding incisor angles. Harris 1993 raises a question concerning the reason for this error. He hypothesizes that the longitudinal axis of the root of the upper incisor is not always the same as the axis of the crown according to the cephalometric analysis; therefore, there is an angle between the crown and the root; this angle is larger than the more lingually inclined the crown is, and the angle between the crown-root to the upper incisor is larger in the Class-III set of relations, a fact that causes great difficulty in identifying the appropriate longitudinal axis of the upper incisor. This conclusion has implications concerning the accuracy of the model on which the entire process of planning a combined treatment for maxillofacial deformities is based and may result in inaccurate overtreatment [
18].
To examine the accuracy of the model on which the entire planning process is based, ten physicians were provided 100 cephalometric radiographs (1000 measurements for each one of the parameters) to obtain a statistically significant index concerning the accuracy of measurement in Class-I compared to Class-III.
In line with the research hypothesis, we found that U1 measurements, which are an essential part of the diagnosis and ortho-surgical plan, suffer from a significant examiner-based bias that is greater in cases of facial deformity (Class-III = Prognathic) than in cases of normal facial structure (Class-I = Orthognathic) and is also greater in more severe cases.
On the other hand, concerning the mandible, the severity of the prognathic facial deformity was associated with examiner bias, although this finding is not statistically significant.
In 2020, a systematic review compared classical planning using a lateral cephalometric radiograph (conventional method) with a cone-beam computed tomography (CBCT) with intra-oral scans of the dental scans to perform virtual orthognathic planning, with significant accuracy relative to the latter [
19].
Moreover, AI is dominant in radiograph analyses in all medical fields.
In 2021, an evaluation of the accuracy of a computed deep-learning analysis of lateral cephalometric radiographs showed higher accuracy than conventional planning [
20].
5. Conclusions
Cephalometric measurements, essential for correct diagnosis and combined ortho-surgical treatment plan, suffer from significant examiner-based bias that is greater the more severe the deformity. This conclusion has implications for the accuracy of the method on which the entire combined maxillofacial deformity treatment plan is based.
To overcome inaccuracies in cephalometric analysis, the surgeon should use deep learning imaging analysis software such as Dolphin® or Cephx® to lessen human error. Still, CBCT is far superior for its three-dimensional superiority. By combining it with three-dimensional scanning of the dental casts, the surgeon can perform virtual planning with the help of AI programs to achieve much more accurate results.