Oral Health in Migrants: An Observational Study on the Oral Health Status of a Migrant Cohort Coming from Middle- and Low-Income Countries
Abstract
:1. Introduction
2. Materials and Methods
2.1. Clinical Methods
2.2. Statistical Methods
3. Results
4. Discussion
5. Limitations of the Study
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Batra, M.; Gupta, S.; Erbas, B. Oral health beliefs, attitudes, and practices of South Asian migrants: A systematic review. Int. J. Environ. Res. Public Health 2019, 16, 1952. [Google Scholar] [CrossRef] [Green Version]
- Arora, G.; Mackay, D.F.; Conway, D.I.; Pell, J.P. Ethnic differences in oral health and use of dental services: Cross-sectional study using the 2009 Adult Dental Health Survey. BMC Oral Health 2016, 17, 1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- IOM UN Migration. World Migration Report 2022. Available online: https://worldmigrationreport.iom.int/wmr-2022-interactive (accessed on 18 April 2022).
- United Nations, Department of Economic and Social Affairs, Population Division. In International Migration Report 2017: Highlights; ST/ESA/SER.A/404; United Nations: New York, NY, USA, 2017.
- Eurostat. Statistic Explained Migration and Migrant Population Statistics. Data Extracted in March 2022. Available online: https://ec.europa.eu (accessed on 16 April 2022).
- Zucoloto, M.L.; Maroco, J.; Alvares Duarte Bonini Campos, J. Impact of oral health on health-related quality of life: A cross-sectional study. BMC Oral Health 2016, 16, 55. [Google Scholar] [CrossRef]
- Sulaiman, L.; Saub, R.; Adinar Baharuddin, N.; Hasnur Safii, S.; Gopal Krishna, V.; Bartold, P.M.; Vaithilingam, R.D. Impact of Severe Chronic Periodontitis on Oral Health-related Quality of Life. Oral Health Prev. Dent. 2019, 17, 365–373. [Google Scholar] [CrossRef] [PubMed]
- Kane, S.F. The effects of oral health on systemic health. Gen. Dent. 2017, 65, 30–34. [Google Scholar] [PubMed]
- Gamonal, J.; Bravo, J.; Malheiros, Z.; Stewart, B.; Morales, A.; Cavalla, F.; Gomez, M. Periodontal disease, and its impact on general health in Latin America. Section I: Introduction part I. Braz Oral Res. 2020, 34 (Suppl. S1), e024. [Google Scholar] [CrossRef]
- Jin, L.J.; Lamster, I.B.; Greenspan, J.S.; Pitts, N.B.; Scully, C.; Warnakulasuriya, S. Global burden of oral diseases: Emerging concepts, management, and interplay with systemic health. Oral Dis. 2015, 22, 609–619. [Google Scholar] [CrossRef]
- Oral Health. 2014. Available online: https://www.healthypeople.gov/2020/leading-health-indicators/2020-lhi-topics/Oral-Health (accessed on 15 April 2022).
- Kandelman, D.; Arpin, S.; Baez, R.J.; Baehni, P.C.; Petersen, P.E. Oral health care systems in developing and developed countries. Periodontology 2000 2012, 60, 98–109. [Google Scholar] [CrossRef] [PubMed]
- WHO. The WHO Health Promotion Glossary; WHO: Geneva, Switzerland, 1998. [Google Scholar]
- Dao, T.H.; Docquier, F.; Maurel, M.; Schaus, P. Global migration in the twentieth and twenty-first centuries: The unstoppable force of demography. Rev. World Econ. 2021, 157, 417–449. [Google Scholar] [CrossRef]
- Lauritano, D.; Moreo, G.; Carinci, F.; Campanella, V.; Della Vella, F.; Petruzzi, M. Oral Health Status among Migrants from Middle- and Low-Income Countries to Europe: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 12203. [Google Scholar] [CrossRef]
- Riza, E.; Karnaki, P.; Gil-Salmerón, A.; Zota, K.; Ho, M.; Petropoulou, M.; Katsas, K.; Garcés-Ferrer, J.; Linos, A. Determinants of Refugee and Migrant Health Status in 10 European Countries: The Mig-HealthCare Project. Int. J. Environ. Res. Public Health 2020, 17, 6353. [Google Scholar] [CrossRef]
- Lebano, A.; Hamed, S.; Bradby, H.; Gil-Salmerón, A.; Durá-Ferrandis, E.; Garcés-Ferrer, J.; Azzedine, F.; Riza, E.; Karnaki, P.; Zota, D.; et al. Migrants’ and refugees’ health status and healthcare in Europe: A scoping literature review. BMC Public Health 2020, 20, 1039. [Google Scholar] [CrossRef]
- Scholten, P.; Entzinger, H.; Penninx, R. Integrating Immigrants in Europe: Research-Policy Dialogues; IMISCOE Research Series; Springer: Berlin/Heidelberg, Germany, 2015. [Google Scholar] [CrossRef] [Green Version]
- Skeie, M.S.; Riordan, P.J.; Klock, K.S.; Espelid, I. Parental risk attitudes and caries-related behaviours among immigrant and western native children in Oslo. Commun. Dent. Oral Epidemiol. 2006, 34, 103–113. [Google Scholar] [CrossRef]
- Dahlan, R.; Badri, P.; Saltaji, H.; Amin, M. Impact of acculturation on oral health among immigrants and ethnic minorities: A systematic review. PLoS ONE 2019, 14, e0212891. [Google Scholar] [CrossRef] [Green Version]
- Gao, X.L.; McGrath, C. A review on the oral health impacts of acculturation. J. Immigr. Minor. Health 2011, 13, 202–213. [Google Scholar] [CrossRef] [Green Version]
- Pabbla, A.; Duijster, D.; Grasveld, A.; Sekundo, C.; Agyemang, C.; van der Heijden, G. Oral Health Status, Oral Health Behaviours and Oral Health Care Utilisation Among Migrants Residing in Europe: A Systematic Review. J. Immigr. Minor. Health 2021, 23, 373–388. [Google Scholar] [CrossRef]
- Serna, C.A.; Sanchez, J.; Arevalo, O.; Tomar, S.L.; McCoy, V.; Devieux, J.; De La Rosa, M.; Bastida, E. Self-reported factors associated with dental care utilization among Hispanic migrant farmworkers in South Florida. J. Public Health Dent. 2020, 80, 186–193. [Google Scholar] [CrossRef]
- Svensson, I.; Gustafsson, J.; Uleskog, U.; Mathisson, C.; Mollai, N.; Kahlmeter, A.; Matsson, L. Oral condition and background factors in Somali immigrant children newly arrived in Sweden. Swed. Dent. J. 2016, 40, 153–164. [Google Scholar]
- Reza, M.; Amin, M.S.; Sgro, A.; Abdelaziz, A.; Ito, D.; Main, P.; Azarpazhooh, A. Oral Health Status of Immigrant and Refugee Children in North America: A Scoping Review. J. Can. Dent. Assoc. 2016, 82, 1488–2159. [Google Scholar]
- Brzoska, P.; Erdsiek, F.; Waury, D. Enabling and Predisposing Factors for the Utilization of Preventive Dental Health Care in Migrants and Non-Migrants in Germany. Front. Public Health 2017, 5, 201. [Google Scholar] [CrossRef] [Green Version]
- Tiwari, T.; Albino, J. Acculturation and Pediatric Minority Oral Health Interventions. Dent. Clin. N. Am. 2017, 61, 549–563. [Google Scholar] [CrossRef] [PubMed]
- Mouradian, W.E.; Huebener, C.E.; Ramos-Gomez, F.; Slavkin, H.C. Beyond access: The role of family and community in children’s oral health. J. Dent. Educ. 2007, 71, 619–631. [Google Scholar] [CrossRef]
- Moradi, G.; Mohamadi Bolbanabad, A.; Moinafshar, A.; Adabi, H.; Sharafi, M.; Zareie, B. Evaluation of Oral Health Status Based on the Decayed, Missing and Filled Teeth (DMFT) Index. Iran. J. Public Health 2019, 48, 2050–2057. [Google Scholar] [CrossRef] [PubMed]
- Broadbent, J.M.; Thomson, W.M. For debate: Problems with the dmf index pertinent to dental caries data analysis. Commun. Dent. Oral Epidemiol. 2005, 33, 400–409. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roland, E.; Gueguen, G.; Longis, M.J.; Boiselle, J. Validation of the reproducibility of the dmf index used in bucco-dental epidemiology and evaluation of its 2 clinical forms. World Health Stat. Q. 1994, 47, 44–61. [Google Scholar]
- Pitts, N.B.; Ekstrand, K.R. International Caries Detection and Assessment System (ICDAS) and its International Caries Classification and Management System (ICCMS)—Methods for staging of the caries process and enabling dentists to manage caries. Commun. Dent. Oral Epidemiol. 2013, 41, e41–e52. [Google Scholar] [CrossRef] [PubMed]
- Nazir, M.; Al-Ansari, A.; Al-Khalifa, K.; Alhareky, M.; Gaffar, B.; Almas, K. Global Prevalence of Periodontal Disease and Lack of Its Surveillance. Sci. World J. 2020, 2020, 2146160. [Google Scholar] [CrossRef] [PubMed]
- Benigeri, M.; Brodeur, J.M.; Payette, M.; Charbonneau, A.; Ismaïl, A.I. Community periodontal index of treatment needs and prevalence of periodontal conditions. J. Clin. Periodontol. 2000, 27, 308–312. [Google Scholar] [CrossRef]
- Warnakulasuriya, S.; Kujan, O.; Aguirre-Urizar, J.M.; Bagan, J.V.; González-Moles, M.A.; Kerr, A.R.; Lodi, G.; Weber Mello, F.; Monteiro, L.; Ogden, G.R.; et al. Oral potentially malignant disorders: A consensus report from an international seminar on nomenclature and classification, convened by the WHO Collaborating Centre for Oral Cancer. Oral Dis. 2021, 27, 1862–1880. [Google Scholar] [CrossRef] [PubMed]
- Muthukumar, S.; Suresh, R. Community periodontal index of treatment needs index: An indicator of anaerobic periodontal infection. Indian J. Dent. Res. 2009, 20, 423–425. [Google Scholar] [CrossRef]
- Cutress, T.W.; Ainamo, J.; Sardo-Infirri, J. The community periodontal index of treatment needs (CPITN) procedure for population groups and individuals. Int. Dent. J. 1987, 37, 222–233. [Google Scholar]
- Severino, M.; Caruso, S.; Ferrazzano, G.F.; Pisaneschi, A.; Fiasca, F.; Caruso, S.; De Giorgio, S. Prevalence of Early Childhood Caries (ECC) in a paediatric italian population: An epidemiological study. Eur. J. Paediatr. Dent. 2021, 22, 189–198. [Google Scholar] [CrossRef]
- Campus, G.; Solinas, G.; Cagetti, M.G.; Senna, A.; Minelli, L.; Majori, S.; Montagna, M.T.; Reali, D.; Castiglia, P.; Strohmenger, L. National Pathfinder Survey of 12-Year-Old Children’s Oral Health in Italy. Caries Res. 2007, 41, 512–517. [Google Scholar] [CrossRef]
- Ferrazzano, G.F.; Cantile, T.; Sangianantoni, G.; Ingenito, A.; Rengo, S.; Alcidi, B.; Spagnuolo, G. Oral health status and Unmet Restorative Treatment Needs (UTN) in disadvantaged migrant and not migrant children in Italy. Eur. J. Paediatr. Dent. 2019, 20, 10–14. [Google Scholar] [CrossRef] [PubMed]
- van Meijeren-van Lunteren, A.W.; Wolvius, E.B.; Raat, H.; Jaddoe, V.W.V.; Kragt, L. Ethnic background and children’s oral health-related quality of life. Qual. Life Res. 2019, 28, 1783–1791. [Google Scholar] [CrossRef] [Green Version]
- OurWorldinData. Available online: https://ourworldindata.org/grapher/daily-per-capita-caloric-supply (accessed on 27 May 2022).
- Okada, M.; Kawamura, M.; Kaihara, Y.; Matsuzaki, Y.; Kuwahara, S.; Ishidori, H.; Miura, K. Influence of parents’ oral health behaviour on oral health status of their school children: An exploratory study employing a causal modelling technique. Int. J. Paediatr. Dent. 2002, 12, 101–108. [Google Scholar] [CrossRef]
- Mustafa, M.; Nasir, E.F.; Nordrehaug Åstrøm, A. Attitudes toward brushing children’s teeth—A study among parents with immigrant status in Norway. Int. J. Paediatr. Dent. 2021, 31, 80–88. [Google Scholar] [CrossRef] [PubMed]
- Ke, X.; Zhang, L.; Li, Z.; Tang, W. Inequality in health service utilization among migrant and local children: A cross-sectional survey of children aged 0–14 years in Shenzhen, China. BMC Public Health 2020, 20, 1668. [Google Scholar] [CrossRef]
- Julihn, A.; Cunha Soares, F.; Hjern, A.; Dahllöf, G. Development level of the country of parental origin on dental caries in children of immigrant parents in Sweden. Acta Paediatr. 2021, 110, 2405–2414. [Google Scholar] [CrossRef]
- Borrell, L.N.; Beck, J.D.; Heiss, G. Socioeconomic Disadvantage and Periodontal Disease: The Dental Atherosclerosis Risk in Communities Study. Am. J. Public Health 2006, 96, 332–339. [Google Scholar] [CrossRef] [PubMed]



| Country | Total N. | Parents’ Country of Birth N. | Child’s Country of Birth (Aged between 3 and 17) N. | Adult Subject’s Country of Birth (Aged between 18 and 37) N. |
|---|---|---|---|---|
| Egypt | 42 | 28 | 11 | 3 |
| Peru | 36 | 28 | 7 | 1 |
| Ecuador | 13 | 12 | / | 1 |
| The Philippines | 12 | 11 | / | 1 |
| Tunisia | 4 | 2 | 1 | 1 |
| Morocco | 10 | 9 | / | 1 |
| Montenegro | 3 | 3 | / | / |
| Bangladesh | 5 | 4 | 1 | / |
| Pakistan | 1 | / | 1 | / |
| Algeria | 1 | 1 | / | / |
| Romania | 13 | 10 | 1 | 2 |
| Sri Lanka | 6 | 5 | 1 | / |
| Nepal | 1 | 1 | / | / |
| Moldavia | 5 | 4 | 1 | / |
| Albania | 13 | 11 | / | 2 |
| Turkey | 2 | 2 | / | / |
| Kosovo | 2 | 2 | / | / |
| Senegal | 3 | 3 | / | / |
| Bolivia | 1 | 1 | / | / |
| Venezuela | 1 | / | / | 1 |
| Bosnia and Herzegovina | 1 | / | 1 | / |
| India | 3 | 3 | / | / |
| El Salvador | 7 | 4 | 3 | / |
| China | 6 | 6 | / | / |
| Ukraine | 6 | 4 | 2 | / |
| Cameroon | 1 | 1 | / | / |
| Mauritius | 1 | 1 | / | / |
| Saudi Arabia | 1 | 1 | / | / |
| Total | 200 | 158 | 30 | 12 |
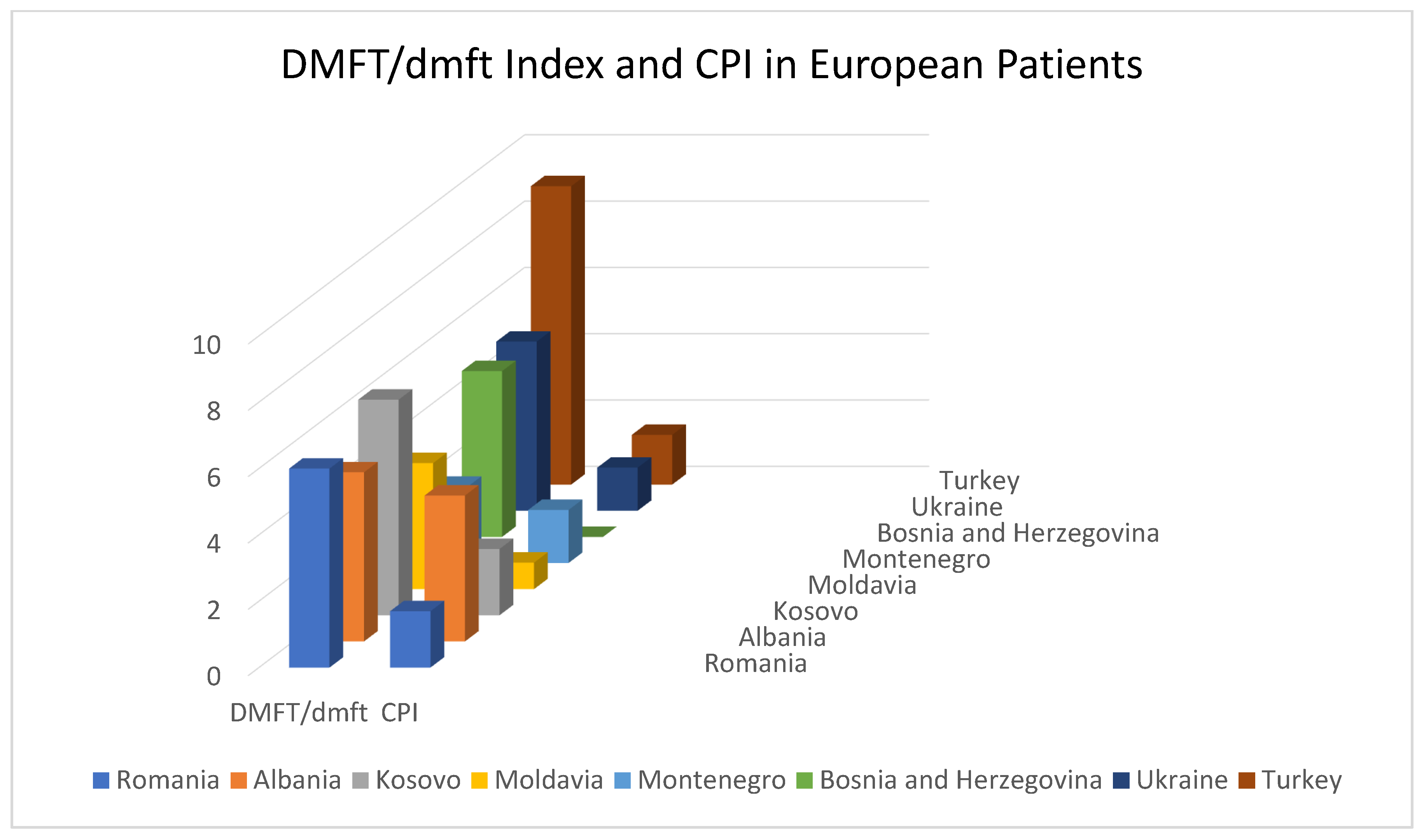
| Country of Birth | Population Sample | DMFT/dmft (M) | DMFT/dmft (SD) | CPI (M) | CPI (SD) |
|---|---|---|---|---|---|
| Egypt | 42 | 6.11 | 4.06 | 1.35 | 2.12 |
| Morocco | 10 | 4.6 | 4.29 | 0.4 | 0.66 |
| Tunisia | 4 | 2.5 | 1.5 | 3.5 | 2.29 |
| Algeria | 1 | 3 | - | 3 | - |
| Senegal | 3 | 3.66 | 0.94 | 0 | 0 |
| Cameroon | 1 | 3 | - | 1 | - |
| Mauritius | 1 | 4 | - | 0 | - |
| Peru | 36 | 3.805 | 2.83 | 1.08 | 1.73 |
| Ecuador | 13 | 3.61 | 2.09 | 1.69 | 2.39 |
| Venezuela | 1 | 5 | - | 5 | - |
| Bolivia | 1 | 6 | - | 0 | - |
| El Salvador | 7 | 5.42 | 4.74 | 1 | 1.60 |
| The Philippines | 12 | 5.41 | 4.03 | 1.5 | 1.89 |
| China | 6 | 7.16 | 3.43 | 0.5 | 1.11 |
| India | 3 | 5 | 1.41 | 1 | 1.41 |
| Sri Lanka | 6 | 1.5 | 1.5 | 0.66 | 1.49 |
| Nepal | 1 | 12 | - | 0 | - |
| Albania | 13 | 5.15 | 3.50 | 1.53 | 1.94 |
| Romania | 13 | 6 | 3.96 | 1.76 | 2.32 |
| Ukraine | 6 | 5.16 | 2.79 | 1.33 | 1.97 |
| Moldavia | 5 | 3.8 | 1.93 | 0.8 | 1.6 |
| Turkey | 2 | 9 | 3 | 1.5 | 1.5 |
| Montenegro | 3 | 2.33 | 0.47 | 1.66 | 2.35 |
| Bosnia and Herzegovina | 1 | 5 | - | 0 | - |
| Kosovo | 2 | 6.5 | 2.5 | 2 | 2 |
| Pakistan | 1 | 8 | - | 4 | - |
| Bangladesh | 5 | 7.6 | 3.38 | 2 | 1.26 |
| Saudi Arabia | 1 | 8 | - | 3 | - |
| Total | 200 | 5.28 | 2.23 | 1.4 | 1.24 |
| Age Range | Population Sample | DMFT/dmft (M) | DMFT/dmft (SD) | CPI (M) | CPI (SD) |
|---|---|---|---|---|---|
| 3–6 years old | 74 | 6.5 | 4.1 | 0.94 | 1.57 |
| 7–12 years old | 98 | 4.6 | 3.01 | 1.45 | 2.20 |
| 13–20 years old | 14 | 1.46 | 1.54 | 0.64 | 1.58 |
| 21–37 years old | 14 | 3.8 | 2.45 | 3.4 | 2.77 |
| Female | 110 | 4.5 | 3.12 | 1.45 | 2.15 |
| Male | 90 | 5.61 | 4.10 | 1.15 | 1.67 |
| Secondary School | 35 | 5.7 | 3.4 | 2.1 | 2.4 |
| High School | 132 | 4.8 | 3.7 | 1.1 | 1.8 |
| University | 32 | 4.7 | 2.8 | 0.8 | 1.5 |
| Educational Level | DMFT/dmft (M) | DMFT/dmft (SD) | SS | df | MS | F | p-Value |
|---|---|---|---|---|---|---|---|
| Secondary School | 5.7 | 3.4 | |||||
| High School | 4.8 | 3.7 | 23.57 | 2 | 11.78 | 0.92632 * | 0.397728 * |
| University | 4.7 | 2.8 | |||||
| CPI (M) | CPI (SD) | SS | df | MS | F | p-Value | |
| Secondary School | 2.1 | 2.4 | |||||
| High School | 1.1 | 1.8 | 35.90 | 2 | 17.95 | 4.85511 ** | 0.00874 ** |
| University | 0.8 | 1.5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lauritano, D.; Moreo, G.; Martinelli, M.; Campanella, V.; Arcuri, C.; Carinci, F. Oral Health in Migrants: An Observational Study on the Oral Health Status of a Migrant Cohort Coming from Middle- and Low-Income Countries. Appl. Sci. 2022, 12, 5774. https://doi.org/10.3390/app12125774
Lauritano D, Moreo G, Martinelli M, Campanella V, Arcuri C, Carinci F. Oral Health in Migrants: An Observational Study on the Oral Health Status of a Migrant Cohort Coming from Middle- and Low-Income Countries. Applied Sciences. 2022; 12(12):5774. https://doi.org/10.3390/app12125774
Chicago/Turabian StyleLauritano, Dorina, Giulia Moreo, Marcella Martinelli, Vincenzo Campanella, Claudio Arcuri, and Francesco Carinci. 2022. "Oral Health in Migrants: An Observational Study on the Oral Health Status of a Migrant Cohort Coming from Middle- and Low-Income Countries" Applied Sciences 12, no. 12: 5774. https://doi.org/10.3390/app12125774
APA StyleLauritano, D., Moreo, G., Martinelli, M., Campanella, V., Arcuri, C., & Carinci, F. (2022). Oral Health in Migrants: An Observational Study on the Oral Health Status of a Migrant Cohort Coming from Middle- and Low-Income Countries. Applied Sciences, 12(12), 5774. https://doi.org/10.3390/app12125774







