Percutaneous Electrical Nerve Stimulation (PENS) as a Rehabilitation Approach for Reducing Mixed Chronic Pain in Patients with Musculoskeletal Disorders
Abstract
1. Introduction
2. Musculoskeletal Disorders Characterized by Mixed Chronic Pain
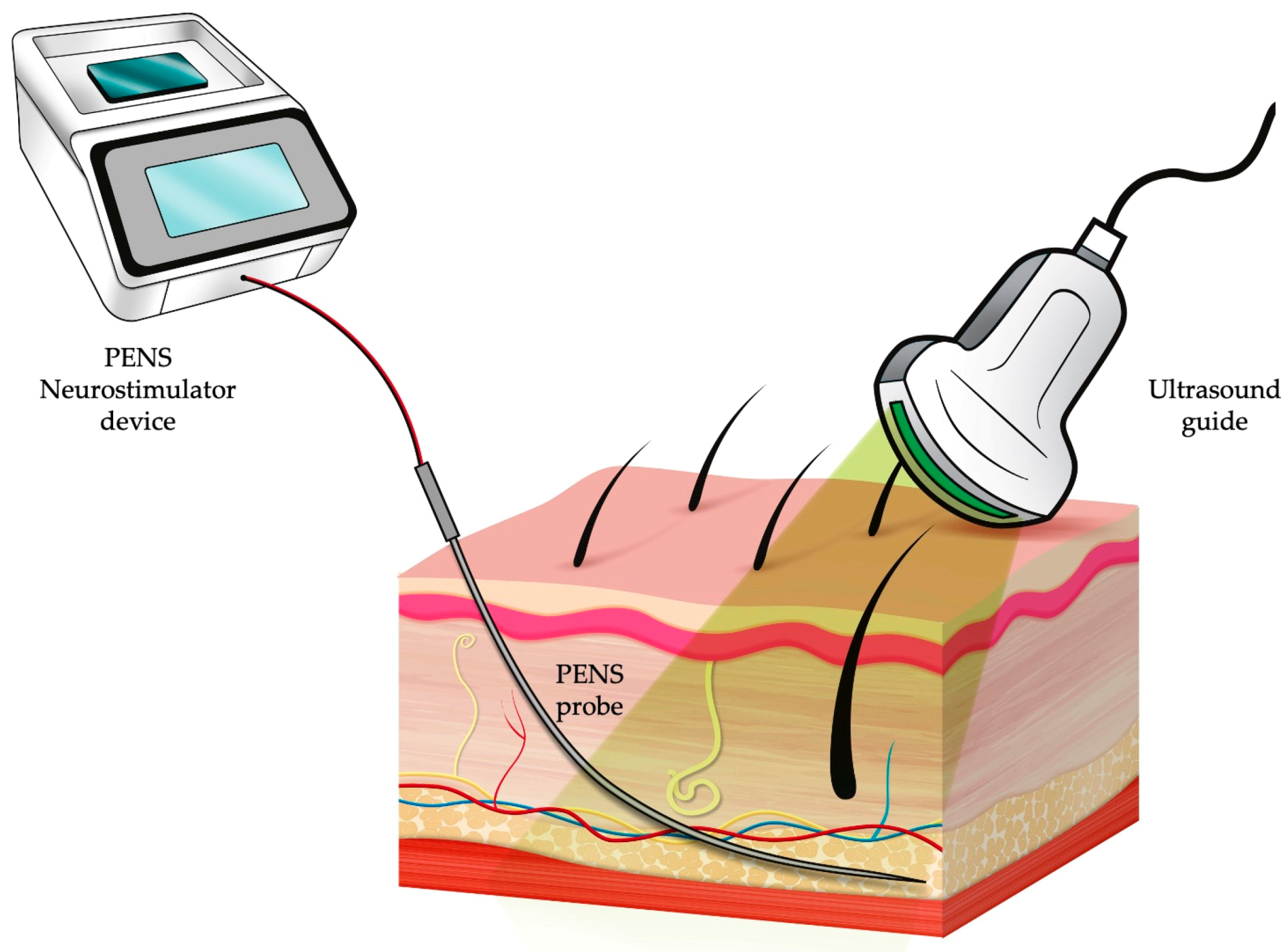
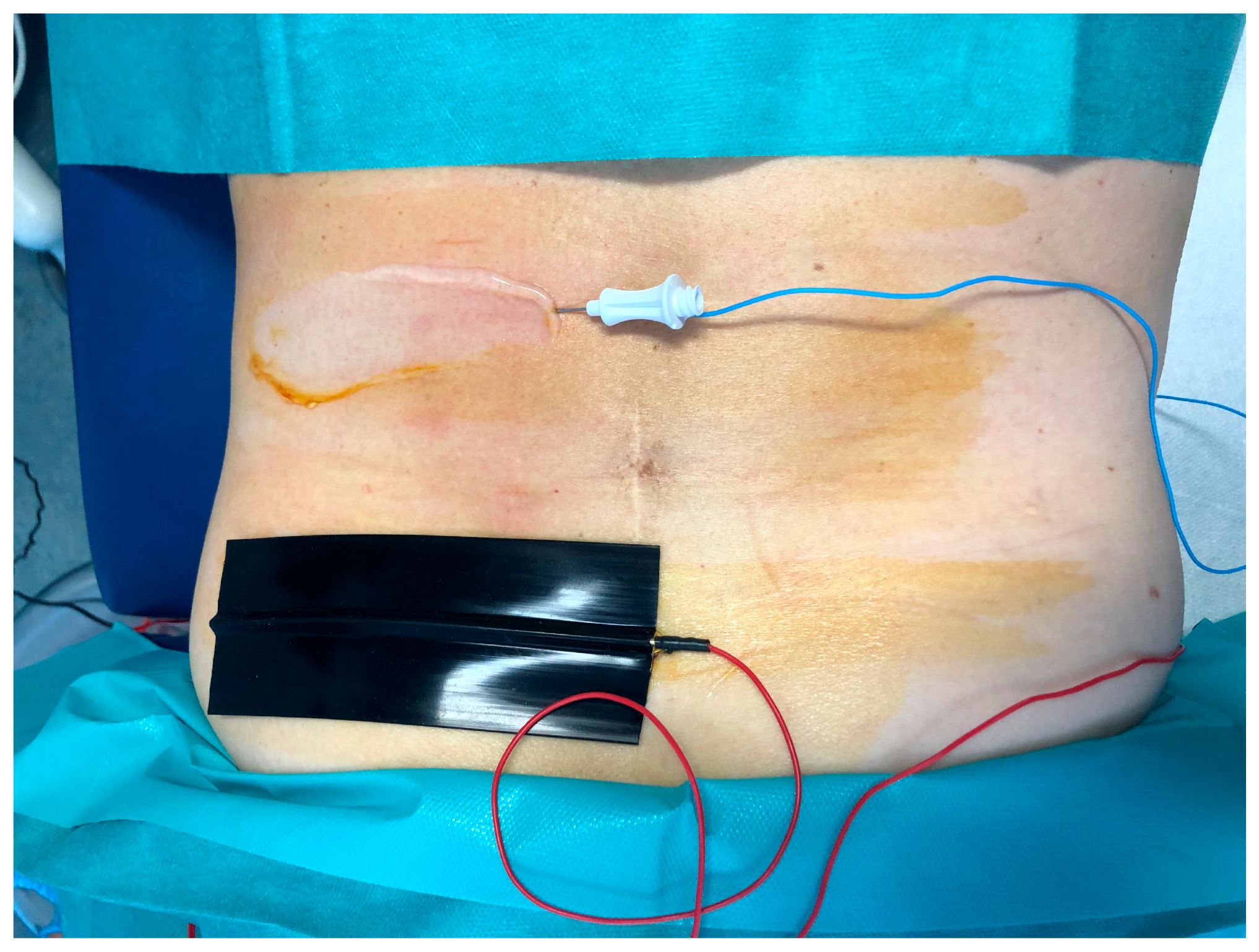
3. Percutaneous Electrical Nerve Stimulation (PENS)
4. PENS for Low Back Pain
5. PENS for Chronic Knee Pain
6. Other Applications and Future Perspectives
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kosek, E.; Cohen, M.; Baron, R.; Gebhart, G.F.; Mico, J.A.; Rice, A.S.; Rief, W.; Sluka, A.K. Do we Need a Third Mechanistic Descriptor for Chronic Pain States? Pain 2016, 157, 1382–1386. [Google Scholar] [CrossRef]
- Freynhagen, R.; Parada, H.A.; Calderon-Ospina, C.A.; Chen, J.; Rakhmawati Emril, D.; Fernández-Villacorta, F.J.; Franco, H.; Ho, K.Y.; Lara-Solares, A.; Li, C.C.; et al. Current Understanding of the Mixed Pain Concept: A Brief Narrative Review. Curr. Med. Res. Opin. 2019, 35, 1011–1018. [Google Scholar] [CrossRef]
- Gálvez, R.; Marsal, C.; Vidal, J.; Ruiz, M.; Rejas, J. Cross-Sectional Evaluation of Patient Functioning and Health-Related Quality of Life in Patients with Neuropathic Pain Under Standard Care Conditions. Eur. J. Pain 2007, 11, 244–255. [Google Scholar] [CrossRef]
- Rauck, R.L.; Cohen, S.P.; Gilmore, C.A.; North, J.M.; Kapural, L.; Zang, R.H.; Grill, J.H.; Boggs, J.W. Treatment of Post-Amputation Pain with Peripheral Nerve Stimulation. Neuromodulation 2014, 17, 188–197. [Google Scholar] [CrossRef] [PubMed]
- Gilmore, C.A.; Kapural, L.; McGee, M.J.; Boggs, J.W. Percutaneous Peripheral Nerve Stimulation for Chronic Low Back Pain: Prospective Case Series With 1 Year of Sustained Relief Following Short-Term Implant. Pain Pract. 2020, 20, 310–320. [Google Scholar] [CrossRef]
- Ilfeld, B.M.; Gilmore, C.A.; Grant, S.A.; Bolognesi, M.P.; Del Gaizo, D.J.; Wongsarnpigoon, A.; Boggs, J.W. Ultrasound-guided Percutaneous Peripheral Nerve Stimulation for Analgesia following Total Knee Arthroplasty: A Prospective Feasibility Study. J. Orthop. Surg. Res. 2017, 12, 4. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.P.; Gilmore, C.A.; Rauck, R.L.; Lester, D.D.; Trainer, R.J.; Phan, T.; Kapural, L.; North, J.M.; Crosby, N.D.; Boggs, J.W. Percutaneous Peripheral Nerve Stimulation for the Treatment of Chronic Pain Following Amputation. Mil. Med. 2019, 184, 267–274. [Google Scholar] [CrossRef]
- Ahmed, H.E.; Craig, W.F.; White, P.F.; Huber, P. Percutaneous Electrical Nerve Stimulation (PENS): A Complementary Therapy for the Management of Pain Secondary to Bony Metastasis. Clin. J. Pain. 1998, 14, 320–323. [Google Scholar] [CrossRef] [PubMed]
- Barroso, U., Jr.; de Azevedo, A.R.; Cabral, M.; Veiga, M.L.; Braga, A.A.N.M. Percutaneous Electrical Stimulation for Overactive Bladder in Children: A Pilot Study. J. Pediatr. Urol. 2019, 15, e1–e38. [Google Scholar] [CrossRef]
- IASP Announces Revised Definition of Pain—IASP. Available online: https://www.iasp-pain.org/PublicationsNews/NewsDetail.aspx?ItemNumber=10475 (accessed on 14 November 2020).
- Woolf, C.J.; Ma, Q. Nociceptors—Noxious Stimulus Detectors. Neuron 2007, 55, 353–364. [Google Scholar] [CrossRef]
- Woolf, C.J. What is this Thing Called Pain? J. Clin. Investig. 2010, 120, 3742–3744. [Google Scholar] [CrossRef]
- Cavalli, E.; Mammana, S.; Nicoletti, F.; Bramanti, P.; Mazzon, E. The Neuropathic Pain: An Overview of the Current Treatment and Future Therapeutic Approaches. Int. J. Immunopathol. Pharmacol. 2019, 33, 2058738419838383. [Google Scholar] [CrossRef] [PubMed]
- Gierthmühlen, J.; Baron, R. Neuropathic Pain. Semin Neurol. 2016, 36, 462–468. [Google Scholar] [PubMed]
- Clauw, D.J.; Essex, M.N.; Pitman, V.; Jones, K.D. Reframing Chronic Pain as a disease, not a Symptom: Rationale and Implications for Pain Management. Postgrad. Med. 2019, 131, 185–198. [Google Scholar] [CrossRef]
- Taylor, R.S. Epidemiology of Refractory Neuropathic Pain. Pain Pract. 2006, 6, 22–26. [Google Scholar] [CrossRef]
- Iolascon, G.; de Sire, A.; Moretti, A.; Gimigliano, F. Complex Regional Pain Syndrome (CRPS) Type I: Historical Perspective and Critical Issues. Clin. Cases Miner. Bone Metab. 2015, 12 (Suppl. 1), 4–10. [Google Scholar] [CrossRef]
- de Sire, A.; Paoletta, M.; Moretti, A.; Brandi, M.L.; Iolascon, G. Complex Regional Pain Syndrome: Facts on Causes, Diagnosis and Therapy. Clin. Cases Miner. Bone Metab. 2018, 15, 166–172. [Google Scholar]
- Bernetti, A.; Agostini, F.; de Sire, A.; Mangone, M.; Tognolo, L.; Di Cesare, A.; Ruiu, P.; Paolucci, T.; Invernizzi, M.; Paoloni, M. Neuropathic Pain and Rehabilitation: A Systematic Review of International Guidelines. Diagnostics 2021, 11, 74. [Google Scholar] [CrossRef]
- Chaparro, L.E.; Wiffen, P.J.; Moore, R.A.; Gilron, I. Combination Pharmacotherapy for the Treatment of Neuropathic Pain in Adults. Cochrane Database Syst. Rev. 2012, 7, CD008943. [Google Scholar]
- Macone, A.; Otis, J.A.D. Neuropathic Pain. Semin Neurol. 2018, 38, 644–653. [Google Scholar]
- Meacham, K.; Shepherd, A.; Mohapatra, D.P.; Haroutounian, S. Neuropathic Pain: Central vs. Peripheral Mechanisms. Curr. Pain Headache Rep. 2017, 21, 28. [Google Scholar] [CrossRef]
- Romanò, C.L.; Romanò, D.; Lacerenza, M. Antineuropathic and Antinociceptive Drugs Combination in Patients with Chronic Low Back Pain: A Systematic Review. Pain Res. Treat. 2012, 2012, 154781. [Google Scholar] [CrossRef]
- French, H.P.; Smart, K.M.; Doyle, F. Prevalence of Neuropathic Pain in Knee or Hip Osteoarthritis: A Systematic Review and Meta-Analysis. Semin. Arthritis Rheum. 2017, 47, 1–8. [Google Scholar] [CrossRef] [PubMed]
- St John Smith, E. Advances in Understanding Nociception and Neuropathic Pain. J. Neurol. 2018, 265, 231–238. [Google Scholar] [CrossRef] [PubMed]
- Scascighini, L.; Toma, V.; Dober-Spielmann, S.; Sprott, H. Multidisciplinary Treatment for Chronic Pain: A Systematic Review of Interventions and Outcomes. Rheumatology 2008, 47, 670–678. [Google Scholar] [CrossRef]
- de Sire, A.; Baricich, A.; Minetto, M.A.; Cisari, C.; Invernizzi, M. Low Back Pain related to a Sacral Insufficiency Fracture: Role of Paravertebral Oxygen-Ozone Therapy in a Paradigmatic Case of Nociplastic Pain. Funct Neurol. 2019, 34, 119–122. [Google Scholar]
- Papuć, E.; Rejdak, K. The role of Neurostimulation in the Treatment of Neuropathic Pain. Ann. Agric. Environ. Med. 2013, 1, 14–17. [Google Scholar]
- Braz, J.; Solorzano, C.; Wang, X.; Basbaum, A.I. Transmitting Pain and Itch Messages: A Contemporary View of the Spinal Cord Circuits that Generate Gate Control. Neuron 2014, 82, 522–536. [Google Scholar] [CrossRef] [PubMed]
- Colloca, L.; Ludman, T.; Bouhassira, D.; Baron, R.; Dickenson, A.H.; Yarnitsky, D.; Freeman, R.; Truini, A.; Attal, N.; Finnerup, N.B.; et al. Neuropathic Pain. Nat. Rev. Dis. Primers 2017, 3, 17002. [Google Scholar] [CrossRef] [PubMed]
- Tsuda, M.; Koga, K.; Chen, T.; Zhuo, M. Neuronal and Microglial Mechanisms for Neuropathic Pain in the Spinal Dorsal Horn and Anterior Cingulate Cortex. J. Neurochem. 2017, 141, 486–498. [Google Scholar] [CrossRef]
- Nelson, T.S.; Fu, W.; Donahue, R.R.; Corder, G.F.; Hökfelt, T.; Wiley, R.G.; Taylor, B.K. Facilitation of Neuropathic Pain by the NPY Y1 Receptor-Expressing Subpopulation of Excitatory Interneurons in the Dorsal Horn. Sci. Rep. 2019, 9, 7248. [Google Scholar] [CrossRef] [PubMed]
- Shaparin, N.; Gritsenko, K.; Garcia-Roves, D.F.; Shah, U.; Schultz, T.; DeLeon-Casasola, O. Peripheral Neuromodulation for the Treatment of Refractory Trigeminal Neuralgia. Pain Res. Manag. 2015, 20, 63–66. [Google Scholar] [CrossRef] [PubMed]
- Chakravarthy, K.; Nava, A.; Christo, P.J.; Williams, K. Review of Recent Advances in Peripheral Nerve Stimulation (PNS). Curr. Pain Headache Rep. 2016, 20, 60. [Google Scholar] [CrossRef] [PubMed]
- Rossi, M.; DeCarolis, G.; Liberatoscioli, G.; Iemma, D.; Nosella, P.; Nardi, L.F. A Novel Mini-invasive Approach to the Treatment of Neuropathic Pain: The PENS Study. Pain Phys. 2016, 19, E121–E128. [Google Scholar]
- Overview|Percutaneous Electrical Nerve Stimulation for Refractory Neuropathic Pain|Guidance|NICE. Available online: https://www.nice.org.uk/guidance/ipg450 (accessed on 7 November 2020).
- Ilfeld, B.M.; Gabriel, R.A.; Said, E.T.; Monahan, A.M.; Sztain, J.F.; Abramson, W.B.; Khatibi, B.; Finneran, J.J.; Jaeger, P.T.; Schwartz, A.K.; et al. Ultrasound-Guided Percutaneous Peripheral Nerve Stimulation: Neuromodulation of the Femoral Nerve for Postoperative Analgesia Following Ambulatory Anterior Cruciate Ligament Reconstruction: A Proof of Concept Study. Neuromodulation 2019, 22, 621–629. [Google Scholar] [CrossRef]
- Wilson, R.D.; Gunzler, D.D.; Bennett, M.E.; Chae, J. Peripheral Nerve Stimulation Compared with Usual Care for Pain Relief of Hemiplegic Shoulder Pain: A Randomized Controlled Trial. Am. J. Phys. Med. Rehabil. 2014, 93, 17–28. [Google Scholar] [CrossRef]
- Chakravarthy, M.; Prashanth, A.; George, A. Evaluation of Percutaneous Electrical Nerve Stimulation of the Auricle for Relief of Postoperative Pain Following Cesarean Section. Med. Acupunct. 2019, 31, 281–288. [Google Scholar] [CrossRef]
- Dionne, C.E.; Dunn, K.M.; Croft, P.R.; Nachemson, A.L.; Buchbinder, R.; Walker, B.F.; Wyatt, M.; Cassidy, J.D.; Rossignol, M.; Leboeuf-Yde, C.; et al. A Consensus Approach Toward the Standardization of Back Pain Definitions for Use in Prevalence Studies. Spine 2008, 33, 95–103. [Google Scholar] [CrossRef]
- Hartvigsen, J.; Hancock, M.J.; Kongsted, A.; Louw, Q.; Ferreira, M.L.; Genevay, S.; Hoy, D.; Karppinen, J.; Pransky, G.; Sieper, J.; et al. What Low Back Pain is and Why We Need to Pay Attention. Lancet 2018, 391, 2356–2367. [Google Scholar] [CrossRef]
- Gimigliano, F.; De Sire, A.; Gastaldo, M.; Maghini, I.; Paoletta, M.; Pasquini, A.; Boldrini, P.; Selb, M.; Prodinger, B.; Abbamonte, M.; et al. Use of the International Classification of Functioning, Disability and Health Generic-30 Set for the characterization of outpatients: Italian Society of Physical and Rehabilitative Medicine Residents Section Project. Eur. J. Phys. Rehabil. Med. 2019, 55, 258–264. [Google Scholar] [CrossRef]
- Qaseem, A.; Wilt, T.J.; McLean, R.M.; Forciea, M.A. Clinical Guidelines Committee of the American College of Physicians. Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline from the American College of Physicians. Ann. Intern. Med. 2017, 166, 514–530. [Google Scholar] [CrossRef]
- Urits, I.; Burshtein, A.; Sharma, M.; Testa, L.; Gold, P.A.; Orhurhu, V.; Viswanath, O.; Jones, M.R.; Sidransky, M.A.; Spektor, B.; et al. Low Back Pain, a Comprehensive Review: Pathophysiology, Diagnosis, and Treatment. Curr. Pain Headache Rep. 2019, 23, 23. [Google Scholar] [CrossRef] [PubMed]
- Akhtar, M.W.; Karimi, H.; Gilani, S.A. Effectiveness of Core Stabilization Exercises and Routine Exercise Therapy in Management of Pain in Chronic Non-Specific Low Back Pain: A Randomized Controlled Clinical Trial. Pak. J. Med. Sci. 2017, 33, 1002–1006. [Google Scholar] [CrossRef]
- Wu, L.C.; Weng, P.W.; Chen, C.H.; Huang, Y.Y.; Tsuang, Y.H.; Chiang, C.J. Literature Review and Meta-Analysis of Transcutaneous Electrical Nerve Stimulation in Treating Chronic Back Pain. Reg. Anesth. Pain Med. 2018, 43, 425–433. [Google Scholar] [CrossRef]
- de Sire, A.; Agostini, F.; Lippi, L.; Mangone, M.; Marchese, S.; Cisari, C.; Bernetti, A.; Invernizzi, M. Oxygen-Ozone Therapy in the Rehabilitation Field: State of the Art on Mechanisms of Action, Safety and Effectiveness in Patients with Musculoskeletal Disorders. Biomolecules. 2021, 11, 356. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, R.L.; Lee, W.C. One-Shot Percutaneous Electrical Nerve Stimulation vs. Transcutaneous Electrical Nerve Stimulation for Low Back Pain: Comparison of Therapeutic Effects. Am. J. Phys. Med. Rehabil. 2002, 81, 838–843. [Google Scholar] [CrossRef] [PubMed]
- Yokoyama, M.; Sun, X.; Oku, S.; Taga, N.; Sato, K.; Mizobuchi, S.; Takahashi, T.; Morita, K. Comparison of Percutaneous Electrical Nerve Stimulation with Transcutaneous Electrical Nerve Stimulation for Long-Term Pain Relief in Patients with Chronic Low Back Pain. Anesth. Analg. 2004, 98, 1552–1556. [Google Scholar] [CrossRef] [PubMed]
- Weiner, D.K.; Perera, S.; Rudy, T.E.; Glick, R.M.; Shenoy, S.; Delitto, A. Efficacy of Percutaneous Electrical Nerve Stimulation and Therapeutic Exercise for Older Adults with Chronic Low Back Pain: A Randomized Controlled Trial. Pain 2008, 140, 344–357. [Google Scholar] [CrossRef]
- McDonough, C.M.; Jette, A.M. The Contribution of Osteoarthritis to Functional Limitations and Disability. Clin. Geriatr. Med. 2010, 26, 387–399. [Google Scholar] [CrossRef]
- Iolascon, G.; Gimigliano, F.; Moretti, A.; De Sire, A.; Migliore, A.; Brandi, M.L.; Piscitelli, P. Early Osteoarthritis: How to Define, Diagnose, and Manage. A Systematic Review. Eur. Geriatr. Med. 2017, 8, 383–396. [Google Scholar] [CrossRef]
- McAlindon, T.E.; Bannuru, R.; Sullivan, M.C.; Arden, N.K.; Berenbaum, F.; Bierma-Zeinstra, S.M.; Hawker, G.A.; Henrotin, Y.; Hunter, D.J.; Kawaguchi, H.; et al. OARSI Guidelines for the Non-Surgical Management of Knee Osteoarthritis. Osteoarthr. Cartil. 2014, 22, 363–388. [Google Scholar] [CrossRef]
- de Sire, A.; de Sire, R.; Petito, V.; Masi, L.; Cisari, C.; Gasbarrini, A.; Scaldaferri, F.; Invernizzi, M. Gut-Joint Axis: The Role of Physical Exercise on Gut Microbiota Modulation in Older People with Osteoarthritis. Nutrients 2020, 12, 574. [Google Scholar] [CrossRef] [PubMed]
- Migliore, A.; Paoletta, M.; Moretti, A.; Liguori, S.; Iolascon, G. The Perspectives of Intra-Articular Therapy in the Management of Osteoarthritis. Expert Opin. Drug Deliv. 2020, 17, 1213–1226. [Google Scholar] [CrossRef]
- Bunt, C.W.; Jonas, C.E.; Chang, J.G. Knee Pain in Adults and Adolescents: The Initial Evaluation. Am. Fam Phys. 2018, 98, 576–585. [Google Scholar]
- Rabini, A.; De Sire, A.; Marzetti, E.; Gimigliano, R.; Ferriero, G.; Piazzini, D.B.; Iolascon, G.; Gimigliano, F. Effects of Focal Muscle Vibration on Physical Functioning in Patients with Knee Osteoarthritis: A Randomized Controlled Trial. Eur. J. Phys. Rehabil. Med. 2015, 51, 513–520. [Google Scholar] [PubMed]
- de Sire, A.; Stagno, D.; Minetto, M.A.; Cisari, C.; Baricich, A.; Invernizzi, M. Long-Term Effects of Intra-Articular Oxygen-Ozone Therapy Versus Hyaluronic Acid in Older People Affected by Knee Osteoarthritis: A Randomized Single-Blind Extension Study. J. Back Musculoskelet Rehabil. 2020, 33, 347–354. [Google Scholar] [CrossRef]
- Mariconda, C.; Megna, M.; Farì, G.; Bianchi, F.P.; Puntillo, F.; Correggia, C.; Fiore, P. Therapeutic Exercise and Radiofrequency in the Rehabilitation Project for Hip Osteoarthritis Pain. Eur. J. Phys. Rehabil. Med. 2020, 56, 451–458. [Google Scholar] [PubMed]
- Gato-Calvo, L.; Magalhaes, J.; Ruiz-Romero, C.; Blanco, F.J.; Burguera, E.F. Platelet-Rich Plasma in Osteoarthritis Treatment: Review of Current Evidence. Ther. Adv. Chronic Dis. 2019, 10, 2040622319825567. [Google Scholar] [CrossRef] [PubMed]
- He, D.P.; Zhang, J.; Bai, Z.F. Percutaneous Electrical Nerve Stimulation for Chronic Knee Pain: A Randomized, Sham-controlled Trial. Altern. Ther. Health Med. 2019, 25, 30–34. [Google Scholar]
- Fu, T.; Guang, H.J.; Gao, X.Z. Percutaneous Nerve Electrical Stimulation for Fatigue Caused by Chemotherapy for Cervical Cancer. Medicine 2018, 97, e12020. [Google Scholar]
- Ahmed, H.E.; White, P.F.; Craig, W.F.; Hamza, M.A.; Ghoname, E.S.; Gajraj, N.M. Use of Percutaneous Electrical Nerve Stimulation (PENS) in the Short-Term Management of Headache. Headache 2000, 40, 311–315. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Sire, A.; Ammendolia, A.; Lippi, L.; Farì, G.; Cisari, C.; Invernizzi, M. Percutaneous Electrical Nerve Stimulation (PENS) as a Rehabilitation Approach for Reducing Mixed Chronic Pain in Patients with Musculoskeletal Disorders. Appl. Sci. 2021, 11, 4257. https://doi.org/10.3390/app11094257
de Sire A, Ammendolia A, Lippi L, Farì G, Cisari C, Invernizzi M. Percutaneous Electrical Nerve Stimulation (PENS) as a Rehabilitation Approach for Reducing Mixed Chronic Pain in Patients with Musculoskeletal Disorders. Applied Sciences. 2021; 11(9):4257. https://doi.org/10.3390/app11094257
Chicago/Turabian Stylede Sire, Alessandro, Antonio Ammendolia, Lorenzo Lippi, Giacomo Farì, Carlo Cisari, and Marco Invernizzi. 2021. "Percutaneous Electrical Nerve Stimulation (PENS) as a Rehabilitation Approach for Reducing Mixed Chronic Pain in Patients with Musculoskeletal Disorders" Applied Sciences 11, no. 9: 4257. https://doi.org/10.3390/app11094257
APA Stylede Sire, A., Ammendolia, A., Lippi, L., Farì, G., Cisari, C., & Invernizzi, M. (2021). Percutaneous Electrical Nerve Stimulation (PENS) as a Rehabilitation Approach for Reducing Mixed Chronic Pain in Patients with Musculoskeletal Disorders. Applied Sciences, 11(9), 4257. https://doi.org/10.3390/app11094257










