1. Introduction
The number of total joint replacements has increased over the last years, and the number of associated revision surgeries will also increase [
1]. Based on register data, aseptic loosening is one of the most common causes for revision surgery [
1,
2]. In the case of total knee arthroplasty, more than 83% of all implantations performed are cemented [
2]. For total hip arthroplasty, there is regional prevalence in relation to implant fixation technique. Thus, according to the Swedish register, 57.5% of primary total hip arthroplasties are cemented [
3]. Specifically, the registers for hip arthroplasty vary in percentages between the different fixation techniques [
1,
2]. In both hip arthroplasty and knee arthroplasty, the hybrid fixation, i.e., the combination of cemented prosthesis parts with uncemented parts, is also a frequently used technique [
2]. Especially in elderly people, cement is commonly used.
Revision surgery is a challenging procedure for both the surgeon and the patient. For example, when revising a cemented hip stem, it is common to remove the complete cement mantle from the femur. Different methods can be used to remove the cement, for example, with ultrasonic waves. However, the gold standard is still the mechanical removal of the cement. This, however, can be challenging and can entail some complications in cement removal [
4].
Among other things, the risk of blood loss and the risk of bone perforation or even fracture is high [
5,
6,
7]. Removing the remaining bone cement often is time-consuming, which can lead to intraoperative complications [
8]. To improve this, Greenwald et al. considered a different approach than removing all the existing cement [
9]. They suggested to remain the cement and implant the new stem with a thin layer of bone cement on the old cement mantle if the original bone cement mantle is well-fixed and integrated into the femur. This approach is known as the cement-in-cement technique (also known as in-cement or cement-within-cement). After removing the femoral stem, the existing cement mantle is checked for possible damage. If damage is found, a conventional method has to be used. If a fully intact cement mantle is present, the surface is prepared by a burr then cleaned and dried so that the new bone cement has no contamination and a stable connection can be formed. After all these preparations, the new stem can be cemented into the femur. The use of the cement-in-cement technique has increased over the years [
10,
11,
12]. The advantages of this technique are less host bone stock loss, less blood loss and a lower risk of femoral perforation or even fracture [
5,
6,
7]. In addition, a cement-in-cement revision needs less time because cement removal is time-consuming [
5,
13,
14]. This is a medical as well as a financial advantage due to a shorter time under narcotics and also the personal and room resources are used less [
8]. However, only a few biomechanical studies on the strength between two cement layers exist. Testing the bending strength of different cement combinations was done, concentrated on the shear strength between the two layers [
15]. However, the influence of different aging points was not considered. Liddle et al. investigated the shear strength while using different techniques to prepare the cement-in-cement interface [
16]. A preparation with an ultrasonic device showed lower shear bond strength. In an experimental in vitro study, we investigated the effect of cement aging on a cement-in-cement revision construct. For this purpose, we used a four-point bending test to compare the bending strength of different cement-in-cement constructs over different times of bone cement aging.
2. Materials and Methods
We analyzed the influence of cement aging on a cement-in-cement revision construct using the bending strength as the evaluation criterion. For the study, we used Palacos R+G (Heraeus, Hanau, Germany) and SmartSet MV (DePuy Synthes, Warsaw, IN, USA) bone cement. The monomer of both cement types contains 98% of methy methacrylate and 2% N,N-dimethyl-p-toluidine. The cement powder of the Palacos R+G bone cement contains 81.9% of poly (methylacrylate, methyl methacrylate), 15% zirconium dioxide, 1% hydrous benzoyl peroxide, and 2.1% gentamicin sulphate. The compositions of the SmartSet MV powder contain 67% Polymetyl Methacrylate, 21.1% Methyl Methaacrylate/Styrene Copolymer, 1.9% Benzoyl Peroxide, and 10% Barium Sulfate. A total amount of 112 samples were prepared and tested from both types of cement. The samples were divided into four groups, and each group was differed into four examination times. In two of the four groups, cement-in-cement revision constructs were applied. This resulted in the groups Palacos–Revision and Smartset–Revision. The groups, Palacos–Reference and SmartSet–Reference, served as aged-only reference groups. The time of examination results from four different aging states. According to ISO 5833:2002-05, the first point in time was 24 ± 2 h after sample preparation [
17]. The further examinations were 4 weeks plus 1 day, 4 weeks plus 3 days, and 4 weeks plus 10 days. A set of 7 specimens was tested at each investigation time point for each group.
2.1. Cement Aging
According to ISO 5833:2002-05, the first point in time for testing the bending strength of the samples was 24 ± 2 h (24 h) at room conditions of 23 ± 1 °C [
17]. The specimens were stored under dry conditions also at a room temperature of 23 ± 1 °C. A baseline aging of 4 weeks was performed for all other examination time points. For the baseline aging, the cement samples were stored in an incubator for 4 weeks in a saline solution (0.9% NaCl) at 37 ± 1 °C [
18]. The groups, Palacos–Revision and Smartset–Revision, were removed from the incubator after 4 weeks of base aging, and the cement-in-cement revision construct was applied. Subsequently, the samples were returned to the aging process. The second test time was after 4 weeks base aging plus adding 1 day of aging (4W + 1d), also at 37 ± 1 °C in the saline solution (0.9% NaCl). The third test was after 4 weeks base aging plus 3 days (4W + 3d) of additional aging, and the fourth examination time was after 4 weeks of base aging plus 10 days (4W + 10d). All the groups of revisions and references had an identical aging process (
Table 1).
2.2. Cementing Procedure
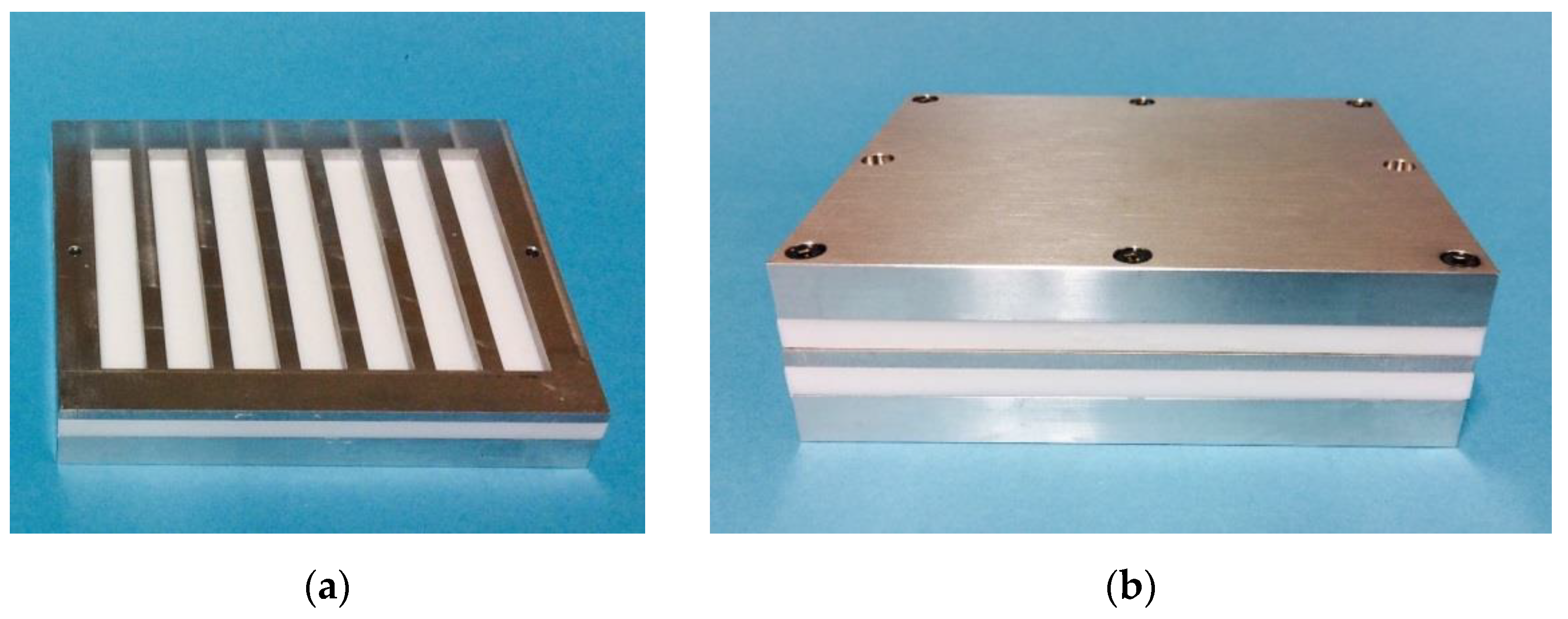
According to the ISO 5833:2002-05, the specimen size is defined as a rectangular bar with a length of 75 ± 0.2 mm, a width of 10 ± 0.2 mm, and a total thickness of 3.3 ± 0.2 mm [
17]. To form the cement specimens, the bone cement was filled into a mold. To smooth the surfaces, the bottom and the top plate of the mold were covered with a heat-stable polyester film (Tartan transparency film 901, 3M, Saint Paul, MN, USA) in combination with a PTFE (polytetrafluoroethylene) plate (
Figure 1).
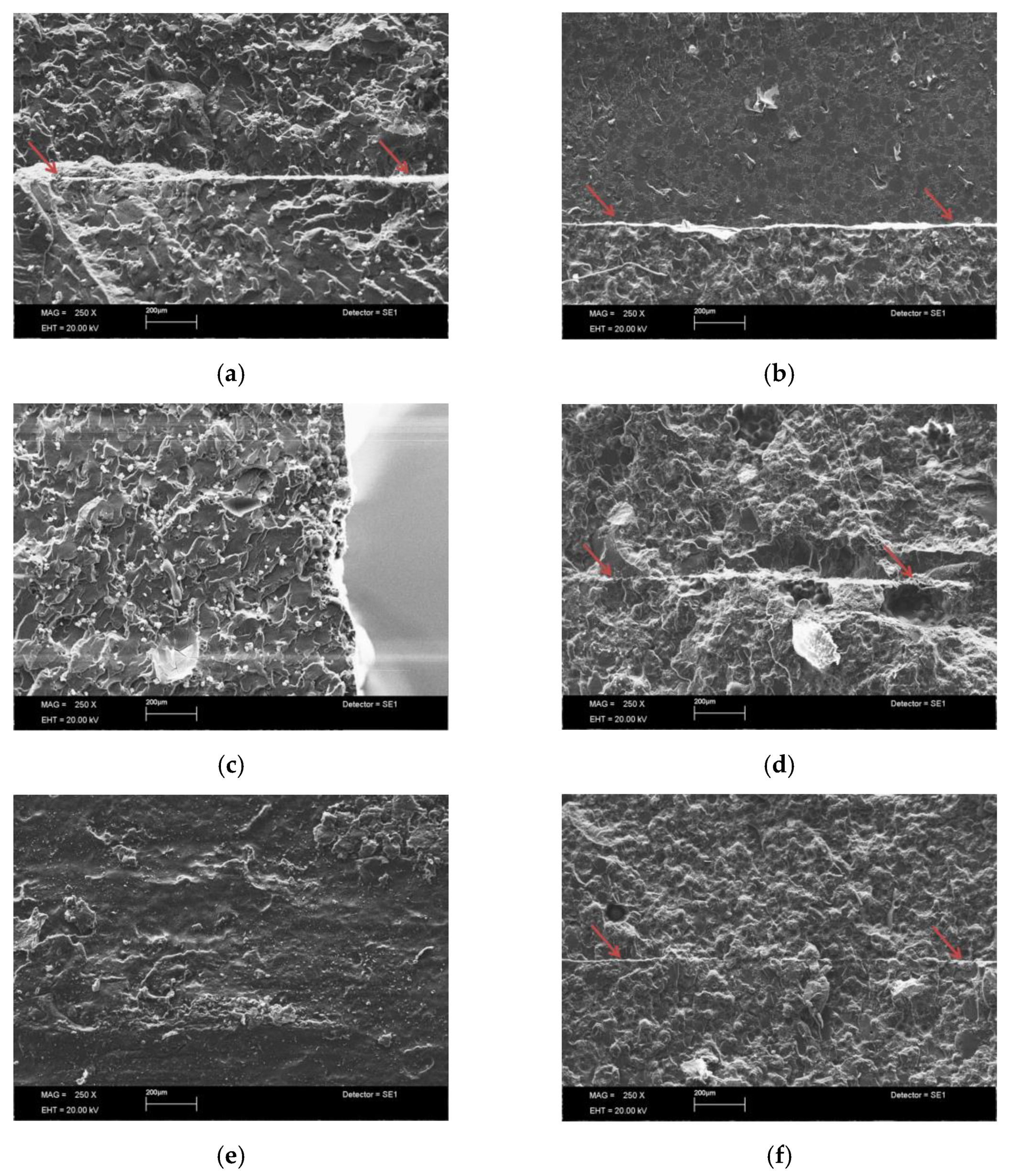
For the cement-in-cement revision construct, a mold with half-thickness (1.65 mm) was used. For cementing the revision group, after cement base aging, the cement specimens were placed in the full-thickness mold and cemented to their full thickness of 3.3 mm. A single cement unit was used for each group and each aging time. Each cementing procedure strictly followed the manufacturer’s instructions. All cement-mixing procedures were performed under vacuum (Vacuum mixing system, Optivac, Biomet, Warsaw, IN, USA) at a room temperature of 23 ± 1 °C and humidity of at least 40%. At the beginning of the application phase, the bone cement was applied into the molds. The time for application varied between the two kinds of cement (Palacos R+G 00:50 min; SmartSet MV 03:40 min). A cement gun was used to dispense the cement into the mold. A polyester film and the top plate with a PTFE plate were added, and then the molds were clamped for over an hour for fully curing the bone cement. After one hour in the clamping system, the top and bottom plates of the molds, including the polyester film, were removed, and the specimens were taken out of the molds. In the case of the revision groups, before adding the new layer of cement, the samples were dried with a compress. After the curing, all cement specimens were wet ground at the edges and top faces using 400-grade emery paper (Hermes, Hamburg, Germany). All cement samples were examined radiologically for possible air inclusions. Exclusion criteria were air inclusions or deviations from the required geometry. As described in the ISO, the unground bottom surface was used as the tensile face during the four-point bending test. The samples of the revision bone cement were examined with a scanning electron microscope (SEM, LEO 440 with EDS detector Oxford X-Max 80, Leo, Oberkochen, Germany) at a magnification ×250 to evaluate the fracture surface between the two cement layers.
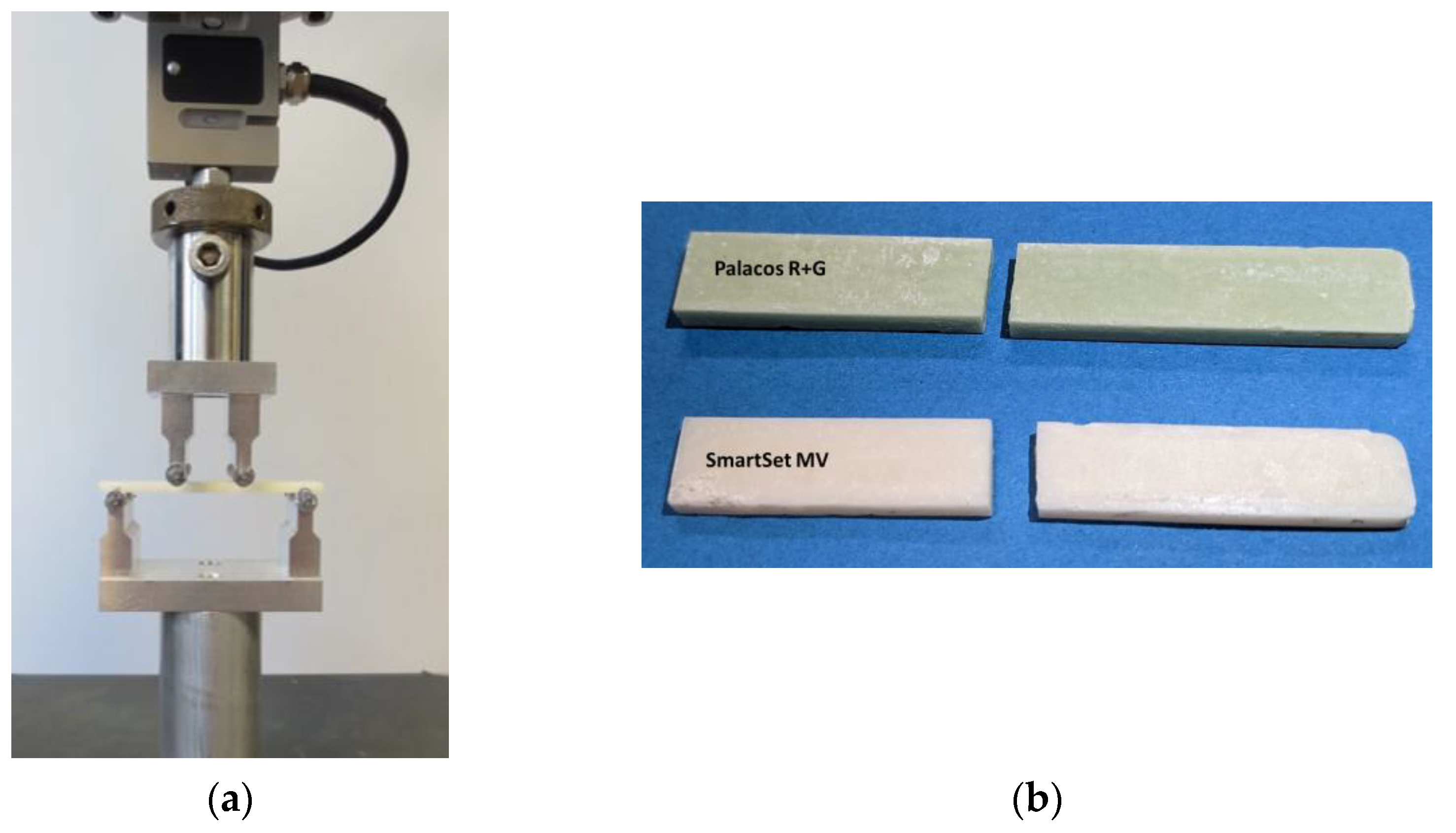
2.3. Bending Strength
The bending strength was determined using a four-point bending test as described in ISO 5833:2002-05 and in ISO 16402:2008-05 [
17,
19]. The sample dimensions were measured before testing. Each measurement was performed three times with an accuracy of ± 0.1 mm, and an average value was calculated for the respective sample geometry. The four-point bending tests were carried out with a material testing machine (Zwick/Roell Z005, Ulm, Germany) and a cross-head speed of 5 mm/min (
Figure 2). The force on the central loading points was increased, starting from zero until the specimen broke. The deflection of the specimen was recorded as a function of the applied force. For each tested specimen, the bending strength was calculated using the following equation:
. Where
F is the force at break (in N),
b is the average measured width of the specimen (in mm),
h is the average thickness of specimen (in mm), and
a is the distance between the inner and outer loading points. According to the ISO 5833:2002-05, the distance between the outer and inner loading points was 20 mm [
17].
2.4. Statistical Analysis
For statistical analysis, the software SPSS 25 (IBM Inc., Armonk, New York, NY, USA) was used. A descriptive analysis (arithmetic mean, standard deviation, minimum, and maximum) was performed. With the Shapiro–Wilk test, the normal distribution of the data was confirmed. Therefore, a repeated-measures ANOVA of independent variables was applied. To compare the groups, an ANOVA with a Bonferroni correction was used. A p-value of <0.05 was considered significant.
4. Discussion
The arthroplasty registries show an increase in joint arthroplasties. Related to this, the incidences of revisions are increasing too, while the aseptic loosening of the endoprosthesis is still the main cause [
1]. Despite the positive long-term prognosis of cemented endoprostheses, a revision is a challenging task. Due to the previous implant, in revisions, the loss of bone is already processed. To avoid or at least minimize possible complications, the cement-in-cement technique can be an alternative for hip or knee revision surgery.
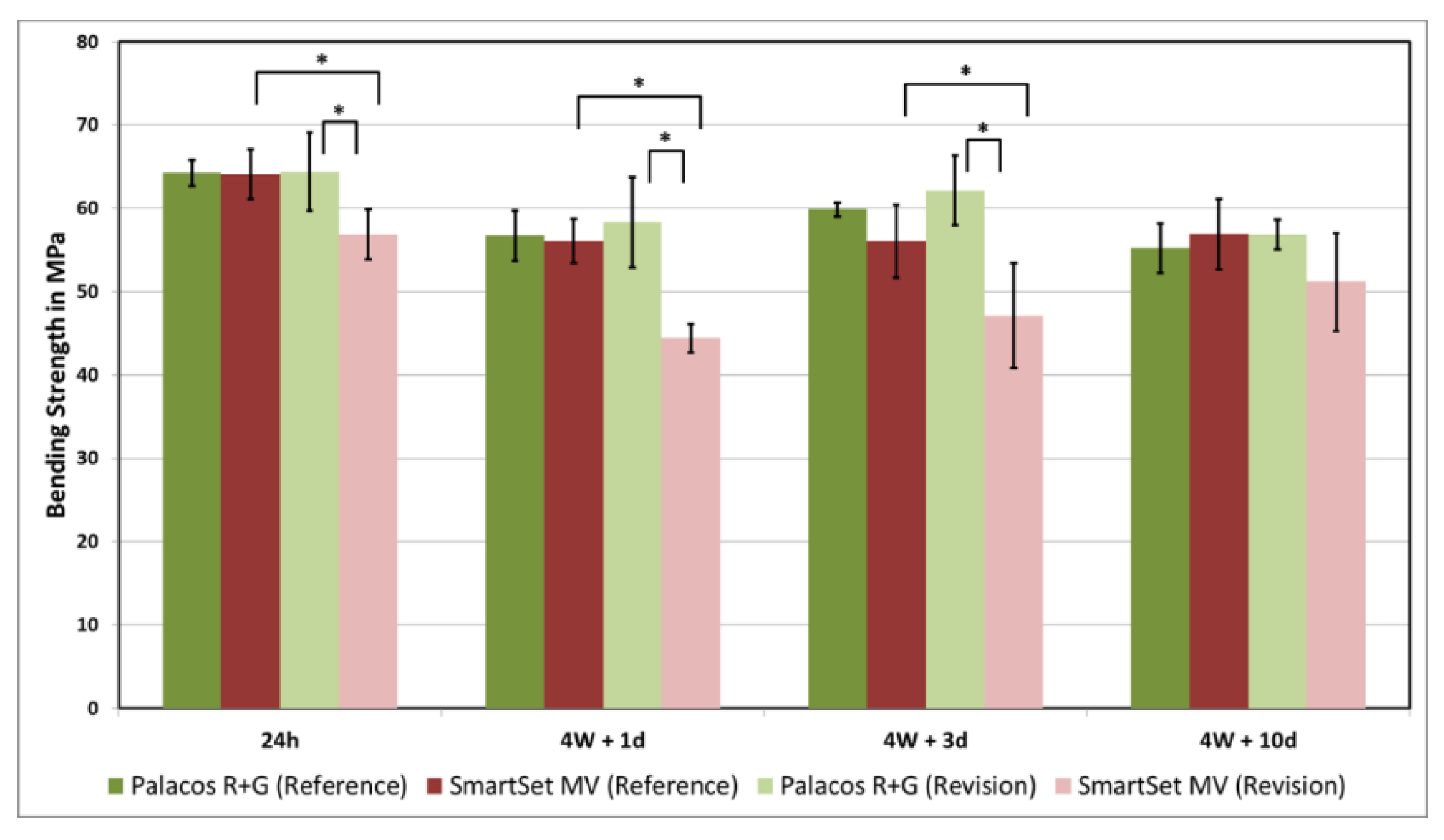
In our experimental in vitro study, the bone cement Palacos R+G showed no significant difference between the reference group and the revision group at any testing time. The mean value of the reference and revision groups with Palacos R+G bone cement also had a bending strength of more than 50 MPa, which is recommended by ISO 5833:2002-05 [
17]. A revision with the cement-in-cement technique and the bone cement Palacos R+G appears to be comparable to a standard cement layer under standardized conditions without the contamination of blood and lipids.
The SmartSet MV bone cement showed a different result between the reference and the revision groups. After only 4 weeks plus 10 days of aging, the bending strength did not differ significantly between the two groups. All aging points before showed that the revision group had a significantly decreased bending strength. Especially at the testing times of 4 weeks plus 1 day and 4 weeks plus 3 days, the mean value of the revision group was below the recommended 50 MPa.
While comparing the two kinds of cement, the references of the Palacos R+G and the SmartSet MV had similar values of bending strength. Therefore, there were no significant differences between the two reference groups at any testing time.
The SmartSet MV bone cement sample had a significantly lower performance than the Palacos R+G sample with the revision technique. The aging of a revision construct influenced the bending strength of the SmartSet MV more than Palacos R+G. Ayre et al. also showed that PMMA bone cements had a decrease in bending strength over the aging time [
18]. If the bone cement gets in contact with blood or lipids, it can further decrease the bending strength [
20,
21]. Further investigations have to be conducted.
In recent years, the use of the cement-in-cement technique has increased more and more. It showed promising clinical results. Quinlan et al. had an excellent outcome using the cement-in-cement technique [
22]. Other studies also showed results with the new technique and a decrease in complications due to the revision [
5,
13,
23,
24]. Sandiford et al. also investigated the cement-in-cement technique in multiple revised total hip replacements. Even though the results were less promising than other studies investigating the cement-in-cement technique, the outcome was still acceptable, especially for patients with a background with more comorbidity [
12]. A systematic review of Xará-Leite et al. in 2020 showed that the cement-in-cement technique is a useful option to minimize intraoperative complications and immediate postoperative morbidity, and the rate of implant survival also remains low [
10]. However, it is often unclear which cement was used in the primary arthroplasty, and therefore, different combinations of cements are possible.
Due to the time interval between the primary replacement and the revision and the possible change of hospital, the cement types may differ from each other. It is often unclear which bone cement was used in the primary replacement [
11].
A further problem could be the preparation of the old cement mantle. Liddle et al. analyzed the effect on the cement-in-cement interface when the old cement is ultrasonically prepared versus a preparation with a burr or no preparation of the cement mantle at all. The shear strength was significantly decreased while using an ultrasonic device. It is possible that the generated heat produces foam on top of the surface, which can lead to a weaker connection between the two bonding cement layers. [
16]
Dang et al. also investigated the strength between the connection of the old cement and the new cement [
15]. The question in their study was if there is an impact from combining two different kinds of cement and if the interface between the aged cement and the new one is the weakest point of this construct. However, the type of cement was not a significant factor for the flexural strength. Additionally, they found that the cement–cement interface is not the primary weakness in this study.
Even though the method of Dang et al. had similarities to our study, there is a relevant difference between them. The samples for the four-point bending test had a different layout than ours. They put the aged cement next to the new cement, instead of on top of each other. Both cement layers were aged the same time. In our study, we aged one layer 4 weeks and the new layer from an additional day to up to 10 days.
The bending strength of aged bone cement was also studied by Oonishi et al. [
25]. They performed a three-point bending test on in vivo-aged bone cement. As a result, there was a correlation between the time in situ and the bending strength. However, the impact of porosity and density should be considered. Our study showed that the time of aged cement has a significant impact on the bending strength.
This study also has limitations. Even though we used two different kinds of bone cement that are commonly used, it only represents these cements and cannot be replicated on all bone cements that are used for joint arthroplasties. For other bone cements, the process of polymerization can be different. Further investigations have to be conducted. The possible contamination of the cement with blood and bone marrow in vivo was not considered. The negative effect of contamination on stability is proven [
20,
21]. Contamination can reduce the bond stability by 99% [
26]. However, our study was performed under laboratory conditions. Further, it was found that if the bone cement is applied early onto the implant, the interface stability is increased by 72%, and a late application increases failure by 73% [
26].