Abstract
Many studies report that maxillofacial growth is influenced by genetic and environmental elements and that incorrect breathing, chewing, sucking, and swallowing are promoting factors of malocclusion. This study aims to evaluate the function and the influence of the tongue positions in patients with Angle class III malocclusion, maxillary hypoplasia, and posterior crossbite. One hundred patients, aged between 6 and 12 years old, were enrolled for the study. In the first group, patients with a diagnosis of class III malocclusion, affected by maxillary hypoplasia, skeletal class III, and posterior dental crossbite were recruited. In the control group, not treated patients with no malocclusion, skeletal class I, and without posterior dental crossbite were selected. Regarding atypical deglutition, no statistical differences were reported between the two groups, and 14% of patients reported ankyloglossia. Statistical differences were found in tongue rest position and during the execution of “hold and pull” and “chuck” exercises. Results obtained in this observational study showed that the clinician (orthodontist or general dentist) should analyze the presence/absence of atypical swallowing, the anatomical and functional aspects, and the tongue behavior in the rest position.
1. Introduction
Previous studies report that maxillofacial growth is influenced by genetic and environmental elements and that incorrect breathing, chewing, sucking, and swallowing are promoting factors of malocclusion [1,2]. The clinical presence of anterior open bite, skeletal class II or class III, is often associated with orofacial dysfunctions [2,3]. Moreover, some studies document the important role of abnormal swallowing in the relapse of the orthodontic treatment [4,5].
Several authors affirm that abnormal deglutition starts as a compensation mechanism derived from a preexisting malocclusion. Others instead evidence how abnormal swallowing has the tendency to exacerbate malocclusions and to negatively influence the ongoing orthodontic treatment [6,7,8,9].
According to developmental physiology, a distinction is drawn between infantile, mature, and inconstant swallowing [10]. Infantile or visceral swallowing is characterized by a forward movement of the tongue which promotes a continuous boost against the lingual surfaces of the anterior teeth. This clinical situation is physiological until 4 years, while afterward, it is considered dysfunctional and usually associated with malocclusions. On the other hand, a mature or somatic swallowing pattern is characterized by a cranial movement of the tongue, and the resulting boost is addressed on the incisive papilla. The maturation from a visceral to a somatic deglutition is gradual, and the transitional period is defined as inconstant swallowing.
Swallowing patterns have been linked to environmental factors [11], tongue position and thrust, mouth breathing, and nonnutritive oral habits. The presence of altered swallowing can also be attributed to ankyloglossia, or tongue-tie: a congenital oral anomaly characterized by an abnormally short lingual frenulum and which negatively affects the growth and development of the stomatognathic system [12].
Cayley et al. determined that children with an incorrect swallowing pattern may rarely touch the anterior part of the palate with the tip of the tongue [13]. In addition, lingual muscle action is interrelated with mandibular motility and position [14]. Patients with skeletal class III malocclusion have the highest rate of abnormal swallowing, as Fuhrmann and Diedrich in 1994 evaluated by using video-based B-mode ultrasound methods [15].
Within a dysfunctional swallowing pattern, close attention must be paid to the tongue rest position. Anterior open bite is the predominant type of malocclusion in children aged between 6 and 8 years old [3,16,17,18,19]. Proffit et al. measured the force levels of the tongue against upper incisors and palate during rest position and normal swallowing. They stated that the tongue resting point was a more important contributing factor than the swallowing position in developing dental arch form [20,21,22]. Moreover, the results from the cinematic-magnetic resonance imaging analysis described horizontal tongue movement among these individuals and the tendency of placing the tongue between teeth while speaking and swallowing [23].
When oral dysfunction remains untreated, orofacial myofunctional disorder (OMD) may occur.
OMD includes dysfunction of the lips, jaw, tongue, and/or oropharynx that interferes with the normal growth and the development and functions of the other oral structures. The lack of intervention during the critical periods may result in malocclusion and inadequate facial development [24,25,26].
This study aims to evaluate the function and influence of the tongue positions in patients with Angle class III malocclusion, maxillary hypoplasia, and posterior crossbite.
2. Materials and Methods
One hundred patients, aged between 6 and 12 years old, were enrolled between September 2018 and January 2020 in the Department of Orthodontics of the Dental School of Turin. Patients were randomly divided into two groups: patients with a diagnosis of class III malocclusion, affected by maxillary hypoplasia, skeletal class III and without posterior dental crossbite (Group 1—G1) and not treated patients, with no malocclusion diagnosticated, skeletal class I and without posterior dental crossbite as the control group (Group 2—G2). Informed consent was obtained from all subjects involved in the study.
G1 (23 Females and 27 Males) and G2 (21 Females and 29 Males) underwent detailed anamnesis and intraoral and extraoral clinical examinations. An anamnestic questionnaire was submitted to the patients’ parents focusing on the type of neonatal feeding (breastfeeding or formula feeding), respiratory and masticatory patterns, presence of noxious habits, headache, respiratory or otorhinolaryngology illnesses. An accurate extraoral and intraoral inspection was performed by one expert dentist and a speech therapist, and the inter-judge reliability was discussed until agreement. The clinical evaluation was conducted observing the lips and the position of the tongue in deglutition and the rest position. The lingual frenulum and the tongue position during the pronunciation of established phonemes were also observed. Moreover, the presence or not of a posterior crossbite was registered.
The exam was a clinical evaluation. It was made with soft and liquid-solid consistencies. The lips were spread manually or with a special mask to evaluate the linguistic kinetics and view the act of swallowing.
The following table was completed by a single speech therapist in the Italian language in Figure 1 and is reported in the English version. The table was a modified version of the one proposed in 2011 by Schindler et al. [27,28,29]. The analyses performed in the current study were focused on the orthodontic topics of the table related to tongue functions and morphology. The other items of the table are relevant for a complete analysis, but they are a matter of speech therapist interest.
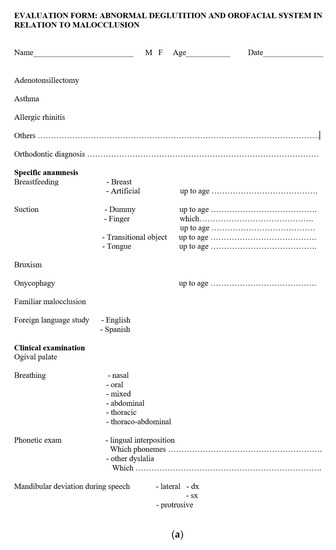

Figure 1.
(a) Functional tongue analysis—Part 1 (b) Functional tongue analysis—Part 2.
One single expert speech therapist explained two myofunctional exercises to the patients, and they were clinically observed while performing them to analyze the correct functionality of the tongue and the perioral tissues. According to Garliner et al. and Saccomanno et al. [30,31], the tongue exercises requested were the following:
- -
- The “hold and pull” exercise works on the midpoint of the tongue. The tip of the tongue and the midpoint are placed against the palate; the mandible is gradually opened with the front and midpoint of the tongue held against the hard palate. The purpose of this exercise is to accustom the front and midpoint of the tongue to the correct position during the swallowing act. This is also an excellent exercise for the slight stretching of the lingual frenulum [30].
- -
- The lifting of the tip of the tongue just behind the retro incisal papilla. Attach the posterior part of the tongue to the palate. Breathe in air between the tongue and the palate to create a vacuum. Slowly open the mouth, hold this position for 5 s, then detach the tongue from the palate, producing an explosive sound similar to a “CHUCK”. This “notching” exercise is meant to observe the tone of the muscles of the tongue and the floor of the mouth [31].
Statistical Analysis
The results were elaborated using the OpenEpi (www.OpenEpi.com) calculation program. A chi-square test was applied to assess the statistically significant difference between groups (p < 0.05) to evaluate the effect of anatomical and functional characteristics on the malocclusion considered. Descriptive data are summarized in Table 1.

Table 1.
Description of main characteristics of patients.
3. Results
Complete results are collected in Table 2.

Table 2.
Number of patients per group (G1 class III, n. 50, G2 class I, n. 50) with atypical swallowing, Ankyloglossia, and incapacity to have a correct rest position and to correctly perform the exercise. Statistical analysis using the chi-square test.
3.1. Atypical Swallowing
Analyzing the behavior of the tongue during the swallowing, on behalf of 100 patients, 32 patients in G1 (64%) and 26 in G2 (52%) presented atypical deglutition. No statistical differences were reported between the two groups (p = 0.234).
3.2. Ankyloglossia
Observing the tongue anatomy, the presence of an abnormally short lingual frenulum was reported in 14% of the patients: 12 in G1 (24%) and 2 in G2 (4%) (p = 0.004).
3.3. Rest Position
Regarding the position of the tongue in the rest position, 38 patients in G1 (76%) and 16 in G2 (32%) showed an anomalous position. Statistical differences were found between G1 and G2 (p < 0.05).
3.4. “Hold and Pull” Exercise
Patients that could not correctly perform the “hold and pull” exercise were found in both groups, with statistical differences (p = 0.05): 31 in G1 (62%) and 21 in G2 (42%).
3.5. “Chuck” Exercise
Nearly half of G1 could not correctly perform the exercise (24 out of 50 patients, 48%), whereas the majority of G2 (42 out of 50 patients, 84%) were able to achieve the “Chuck” exercise (p = 0.001).
4. Discussion
In the present study, the analysis of the swallowing pattern showed no statistically different results between patients with class III malocclusion and controls. Whereas the altered rest position of the tongue was significant in patients with skeletal class III. The results obtained were in accordance with Proffitt et al. and Gorgulu et al. [22,32]. The last author described a more inferior and anterior position of the tongue in patients with class III malocclusion and showed that the bolus transfer was actually different. However, the results may be due to the prevailing infantile and inconstant swallowing between 6 and 12 years old and could have reasonably interfered in our observations on the atypical swallowing.
In the past, one of the major issues has been the oversimplification of the concept of myofunctional anamnesis and therapy. It is still a debated subject, and more clinical and academic research should be encouraged. Thus, many authors report the need to establish neuromuscular balance to achieve stable esthetic and functional goals [12].
Ankyloglossia is characterized by the tethering of the tongue to the floor of the mouth resulting in a forward push of the low postured tongue. This often results in the growth of the mandible in a prognathic manner [33]. The outcomes of this study showed a significant correlation between the presence of a short frenulum and a class III malocclusion. In addition, Pompéia et al. in 2017 affirmed that ankyloglossia could be associated with occlusal problems and craniofacial development and that early diagnosis and treatment provide a better prognosis in the treatment of class III malocclusions [12,34].
If the maxillary growth is restricted, it could often result in a diminished lingual volume. The inadequacy of the intraoral space of the tongue may lead to an inferior positioning of it and a prognathic force on the mandible [33].
The growth and development of the orofacial musculature should be emphasized as its disorder constitutes an unfavorable factor in the management of malocclusion [33]. The two exercises requested during the present study were useful to introduce a more clinical myofunctional registration. The incorrect accomplishment of both the “hold and pull” and the “chuck” exercise [30,31] was significant in Group 1. The patients who could not perform the exercises correctly presented incoordination in tongue movement and praxil lingual competence. Furthermore, the missed achievement of the first suggested a disturbed function of the sublingual glands.
A stomatognathic system is a functional unit characterized by temporomandibular joint, dental and skeletal components, soft tissues, and masticatory muscles. The harmony between these structures enhances different functional tasks, such as speaking, chewing, and swallowing, and interferes with maxillofacial growth [34,35,36].
The present study may enhance the relationship between the myofunctional disorders and class III malocclusion, characterized by maxillary hypoplasia, with a posterior crossbite. As a result of statistically significant outcomes, it is reasonable to recommend during anamnestic procedures that a correct approach should be to consider the overall myofunctional structures besides the tongue movements during the swallowing act.
The cooperation between different healthcare professionals is the success key to growing patient therapies. The role of the orthodontists, pediatric dentists, and speech therapists is to analyze and diagnose all of the aspects of the stomatognathic system, including teeth, lips, respiration pattern, tongue, and deglutition. Therefore, after the interception of a pathologic alteration, it is suggested to send the patient to the specialist. The interconnection between dentist and speech and language therapist is mandatory in solving both initial and complex malocclusions in growing patients.
5. Conclusions
On behalf of the complete diagnosis of the development of malocclusions, every aspect of the patient should be considered with caution. Within the experimental limits, results obtained in this observational study showed that the tongue position in patients with Angle class III malocclusion, maxillary hypoplasia, and posterior crossbite seemed to influence malocclusion. Therefore, the clinician (orthodontist or general dentist) should analyze not only the presence/absence of atypical swallowing but also anatomical aspects, such as ankyloglossia and the behavior of the tongue in the rest position, and functional aspects, such as the correct execution of certain logopedic exercises (i.e., “hold and pull” and “chuck”).
Author Contributions
Conceptualization, T.C. and A.D.; methodology, A.D.; validation, A.D., T.C., and S.P.; formal analysis, T.C.; investigation, A.D.; resources, J.C.; data curation, J.C.; writing—original draft preparation, S.P. and M.C.D.; writing—review and editing, M.C.D. and T.C.; supervision, A.D., T.C., and J.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval were waived for this study, because it was an observational study.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Paolantonio, E.G.; Ludovici, N.; Saccomanno, S.; La Torre, G.; Grippaudo, C. Association between oral habits, mouth breathing and malocclusion in Italian preschoolers. Eur. J. Paediatr. Dent. 2019, 20, 204–208. [Google Scholar] [CrossRef] [PubMed]
- Iwasaki, T.; Sato, H.; Suga, H.; Takemoto, Y.; Inada, E.; Saitoh, I.; Kakuno, E.; Kanomi, R.; Yamasaki, Y. Relationships among nasal resistance, adenoids, tonsils, and tongue posture and maxillofacial form in Class II and Class III children. Am. J. Orthod. Dentofac. Orthop. Off. Publ. Am. Assoc. Orthod. Const. Soc. Am. Board Orthod. 2017, 151, 929–940. [Google Scholar] [CrossRef]
- Stahl, F.; Grabowski, R. Orthodontic findings in the deciduous and early mixed dentition--inferences for a preventive strategy. J. Orofac. Orthop. 2003, 64, 401–416. [Google Scholar] [CrossRef]
- Brückl, H.; Träger, E. Untersuchungen über Art und Häufigkeit anormaler Schluckgewohnheiten. Fortschritte der Kieferorthopädie 1962, 23, 197–202. [Google Scholar] [CrossRef]
- Graber, T.M. The ‘three Ms’: Muscles, malformation, and malocclusion. Am. J. Orthod. 1963, 49, 418–450. [Google Scholar] [CrossRef]
- Maspero, C.; Prevedello, C.; Giannini, L.; Galbiati, G.; Farronato, G. Atypical swallowing: A review. Minerva Stomatol. 2014, 63, 217–227. [Google Scholar]
- Ichida, T.; Takiguchi, R.; Yamada, K. Relationship between the lingual-palatal contact duration associated with swallowing and maxillofacial morphology with the use of electropalatography. Am. J. Orthod. Dentofac. Orthop. Off. Publ. Am. Assoc. Orthod. Const. Soc. Am. Board Orthod. 1999, 116, 146–151. [Google Scholar] [CrossRef]
- Fujiki, T.; Takano-Yamamoto, T.; Noguchi, H.; Yamashiro, T.; Guan, G.; Tanimoto, K. A cineradiographic study of deglutitive tongue movement and nasopharyngeal closure in patients with anterior open bite. Angle Orthod. 2000, 70, 284–289. [Google Scholar] [CrossRef] [PubMed]
- Cheng, C.F.; Peng, C.L.; Chiou, H.Y.; Tsai, C.Y. Dentofacial morphology and tongue function during swallowing. Am. J. Orthod. Dentofac. Orthop. Off. Publ. Am. Assoc. Orthod. Const. Soc. Am. Board Orthod. 2002, 122, 491–499. [Google Scholar] [CrossRef]
- Van Dyck, C.; Dekeyser, A.; Vantricht, E.; Manders, E.; Goeleven, A.; Fieuws, S.; Willems, G. The effect of orofacial myofunctional treatment in children with anterior open bite and tongue dysfunction: A pilot study. Eur. J. Orthod. 2016, 38, 227–234. [Google Scholar] [CrossRef] [PubMed]
- Koletsi, D.; Makou, M.; Pandis, N. Effect of orthodontic management and orofacial muscle training protocols on the correction of myofunctional and myoskeletal problems in developing dentition. A systematic review and meta-analysis. Orthod. Craniofacial Res. 2018, 21, 202–215. [Google Scholar] [CrossRef] [PubMed]
- Pompéia, L.E.; Ilinsky, R.S.; Ortolani, C.; Faltin, K. Ankyloglossia and its influence on growth and development of the stomatognathic system. A influência da anquiloglossia no crescimento e desenvolvimento do sistema estomatognático. Revista Paulista de Pediatria Orgao Oficial da Sociedade de Pediatria de Sao Paulo 2017, 35, 216–221. [Google Scholar] [CrossRef]
- Cayley, A.S.; Tindall, A.P.; Sampson, W.J.; Butcher, A.R. Electropalatographic and cephalometric assessment of tongue function in open bite and non-open bite subjects. Eur. J. Orthod. 2000, 22, 463–474. [Google Scholar] [CrossRef][Green Version]
- Gil, H.; Fougeront, N. Tongue dysfunction screening: Assessment protocol for prescribers. J. Dentofac. Anom. Orthod. 2015, 18, 408. [Google Scholar] [CrossRef]
- Fuhrmann, R.A.; Diedrich, P.R. B-mode ultrasound scanning of the tongue during swallowing. Dento Maxillo Facial Radiol. 1994, 23, 211–215. [Google Scholar] [CrossRef] [PubMed]
- Tausche, E.; Luck, O.; Harzer, W. Prevalence of malocclusions in the early mixed dentition and orthodontic treatment need. Eur. J. Orthod. 2004, 26, 237–244. [Google Scholar] [CrossRef] [PubMed]
- Keski-Nisula, K.; Lehto, R.; Lusa, V.; Keski-Nisula, L.; Varrela, J. Occurrence of malocclusion and need of orthodontic treatment in early mixed dentition. Am. J. Orthod. Dentofac. Orthop. 2003, 124, 631–638. [Google Scholar] [CrossRef]
- Grippaudo, F.; Pantanali, F.; Paolantonio, E.G.; Grecolini, M.E.; Saulle, R.; La Torre, G.; Deli, R. Prevalence of malocclusion in Italian schoolchildren and orthodontic treatment need. European J. Pediatric Dent. 2013, 14, 314–318. [Google Scholar]
- Shalish, M.; Gal, A.; Brin, I.; Zini, A.; Ben-Bassat, Y. Prevalence of dental features that indicate a need for early orthodontic treatment. Eur. J. Orthod. 2013, 35, 454–459. [Google Scholar] [CrossRef]
- Proffit, W.R.; Chastain, B.B.; Norton, L.A. Linguopalatal pressure in children. Am. J. Orthod. 1969, 55, 154–166. [Google Scholar] [CrossRef]
- Proffit, W.R.; McGlone, R.E.; Barrett, M.J. Lip and tongue pressures related to dental arch and oral cavity size in Australian aborigines. J. Dent. Res. 1975, 54, 1161–1172. [Google Scholar] [CrossRef] [PubMed]
- Proffit, W.R. Equilibrium theory revisited: Factors influencing position of the teeth. Angle Orthod. 1978, 48, 175–186. [Google Scholar] [PubMed]
- Sayin, M.Ö.; Akin, E.; Karaçay, Ş.; Bulakbaşi, N. Initial effects of the tongue crib on tongue movements during deglutition: A cine-magnetic resonance imaging study. Angle Orthod. 2006, 76, 400–405. [Google Scholar]
- D’Onofrio, L. Oral dysfunction as a cause of malocclusion. Orthod. Craniofacial Res. 2009, 22 (Suppl. 1), 43–48. [Google Scholar] [CrossRef] [PubMed]
- Lucchese, A.; Bondemark, L.; Marcolina, M.; Manuelli, M. Changes in oral microbiota due to orthodontic appliances: A systematic review. J. Oral Microbiol. 2018, 10. [Google Scholar] [CrossRef] [PubMed]
- Lucchese, A.; Carinci, F.; Brunelli, G.; Monguzzi, R. Everstick® and Ribbond® fiber reinforced composites: Scanning Electron Microscope (SEM) comparative analysis. Eur. J. Inflamm. 2011, 9, 73–79. [Google Scholar]
- Schindler, O.; Ruoppolo, G.; Schindler, A.D. Deglutologia; Omega Edizioni: Torino, Italy, 2001. [Google Scholar]
- Traini, T.; Danza, M.; Zollino, I.; Altavilla, R.; Lucchese, A.; Sollazzo, V.; Trapella, G.; Brunelli, G.; Carinci, F. Histomorphometric evaluation of an immediately loaded implant retrieved from human mandible after 2 years. Int. J. Immunopathol. Pharmacol. 2011, 24, 31–36. [Google Scholar] [CrossRef]
- Rodriguez y Baena, R.; Pastorino, R.; Gherlone, E.F.; Perillo, L.; Lupi, S.M.; Lucchese, A. Histomorphometric Evaluation of Two Different Bone Substitutes in Sinus Augmentation Procedures: A Randomized Controlled Trial in Humans. Int. J. Oral Maxillofac. Implant. 2017, 32, 188–194. [Google Scholar] [CrossRef]
- Garliner, D. Myofunctional Therapy in Dental Practice, 2nd ed.; Bartel Dental Books Co., Inc.: New York, NY, USA, 1974; p. 36. [Google Scholar]
- Saccomanno, S.; Di Tullio, A.; D’Alatri, L.; Grippaudo, C. Proposal for a myofunctional therapy protocol in case of altered lingual frenulum. A pilot study. Eur. J. Paediatr. Dent. 2019, 20, 67–72. [Google Scholar] [CrossRef]
- Görgülü, S.; Sağdıç, D.; Akin, E.; Karaçay, S.; Bulakbası, N. Tongue movements in patients with skeletal Class III malocclusions evaluated with real-time balanced turbo field echo cine magnetic resonance imaging. Am. J. Orthod. Dentofac. Orthop. Off. Publ. Am. Assoc. Orthod. Const. Soc. Am. Board Orthod. 2011, 139, e405–e414. [Google Scholar] [CrossRef] [PubMed]
- Meenakshi, S.; Jagannathan, N. Assessment of lingual frenulum lengths in skeletal malocclusion. J. Clin. Diagn. Res. 2014, 8, 202–204. [Google Scholar] [CrossRef] [PubMed]
- Manuelli, M. A peaceful man. Prog. Orthod. 2012, 13, 1. [Google Scholar] [CrossRef]
- Gedrange, T.; Kunert-Keil, C.; Heinemann, F.; Dominiak, M. Tissue Engineering and Oral Rehabilitation in the Stomatognathic System. BioMed Res. Int. 2017, 4519568. [Google Scholar] [CrossRef]
- Bertossi, D.; Giampaoli, G.; Lucchese, A.; Manuelli, M.; Albanese, M.; Nocini, R.; Nocini, P.F. The skin rejuvenation associated treatment-Fraxel laser, Microbotox, and low G prime hyaluronic acid: Preliminary results. Lasers Med. Sci. 2019, 34, 1449–1455. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).