Print and Try Technique: 3D-Printing of Teeth with Complex Anatomy a Novel Endodontic Approach
Abstract
1. Introduction
2. Case Description
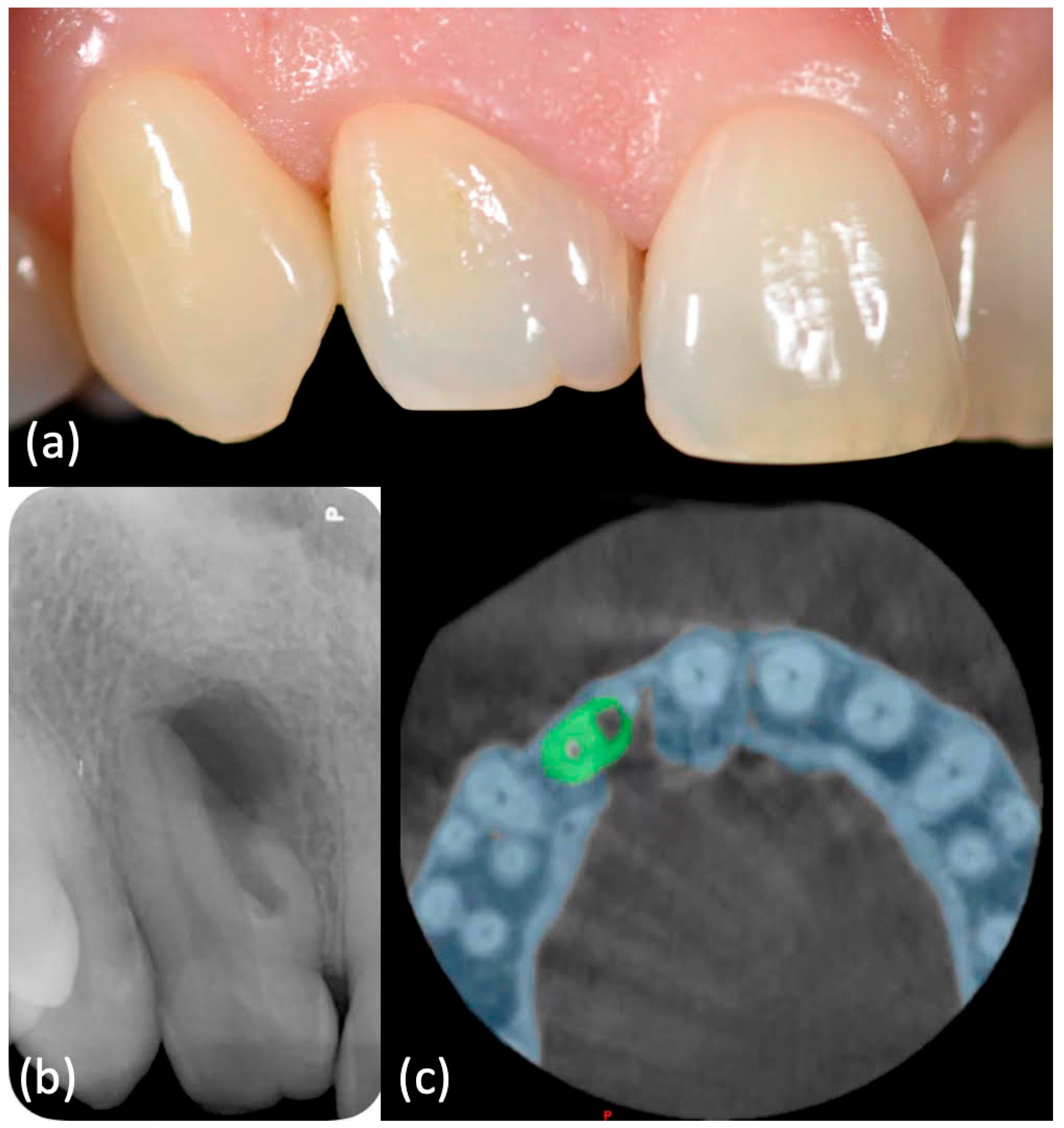
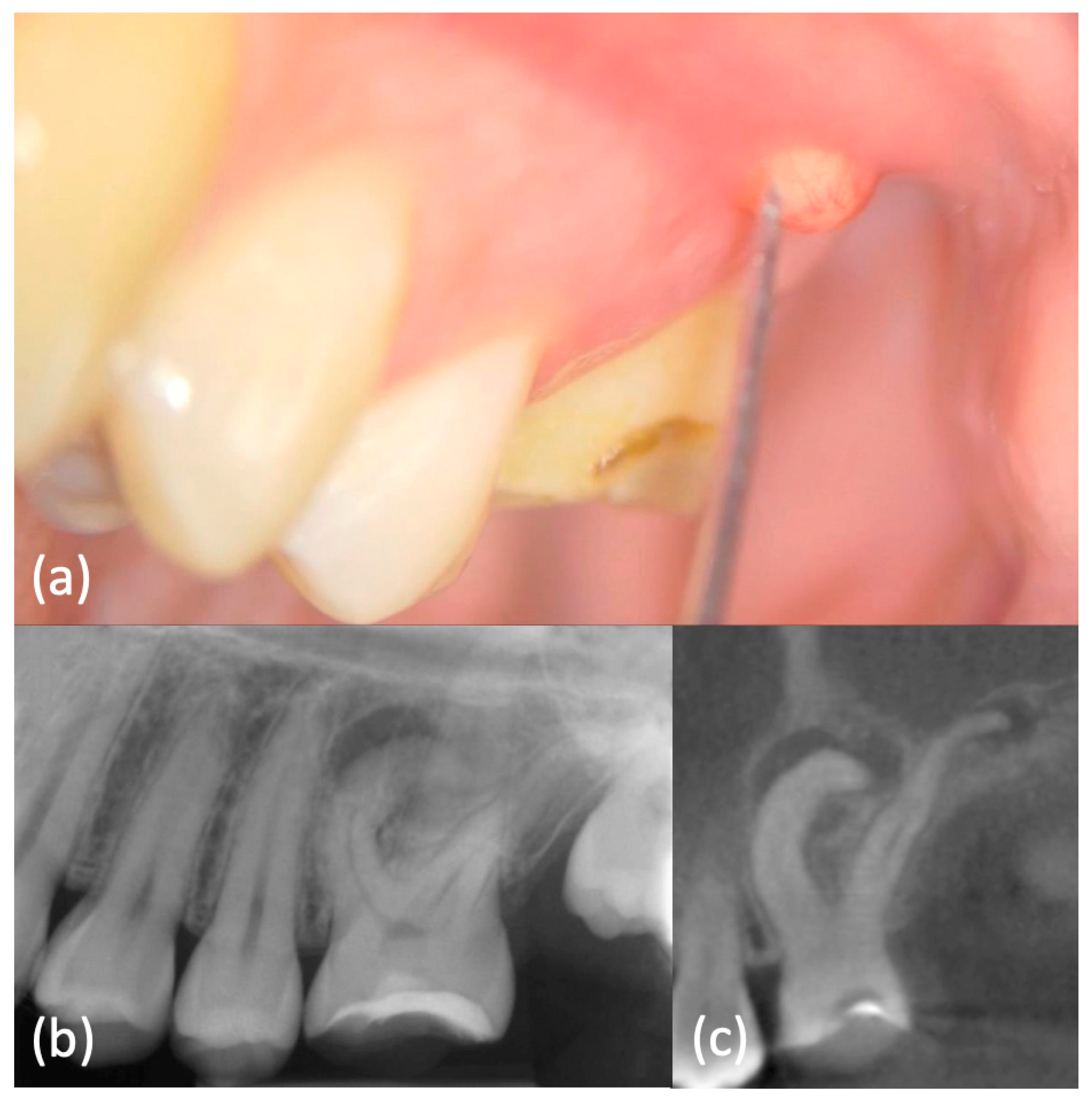
2.1. Case 1
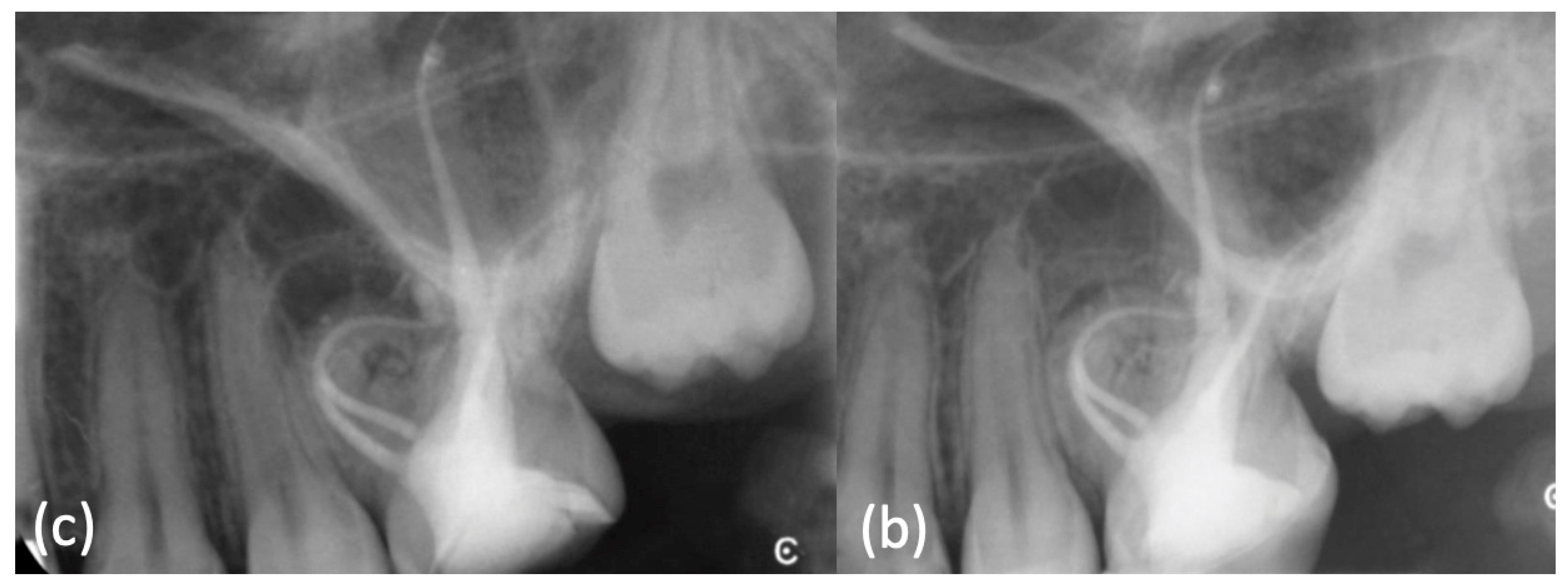
2.2. Case 2
3. Discussion
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Peters, O.A. Current challenges and concepts in the preparation of root canal systems: A review. J. Endod. 2004, 30, 559–567. [Google Scholar] [CrossRef]
- Schäfer, E.; Bürklein, S. Impact of nickel-titanium instrumentation of the root canal on clinical outcomes: A focused review. Odontology 2012, 100, 130–136. [Google Scholar] [CrossRef]
- Tomson, P.L.; Simon, S.R. Contemporary Cleaning and Shaping of the Root Canal System. Prim. Dent. J. 2016, 5, 46–53. [Google Scholar] [CrossRef]
- Siqueira, J.F., Jr. Strategies to treat infected root canals. J. Calif. Dent. Assoc. 2001, 29, 825–837. [Google Scholar]
- Haapasalo, M.; Shen, Y.; Wang, Z.; Gao, Y. Irrigation in endodontics. Br. Dent. J. 2014, 216, 299–303. [Google Scholar] [CrossRef] [PubMed]
- Veríssimo, D.M.; do Vale, M.S. Methodologies for assessment of apical and coronal leakage of endodontic filling materials: A critical review. J. Oral. Sci. 2006, 48, 93–98. [Google Scholar] [PubMed]
- Ng, Y.L.; Mann, V.; Rahbaran, S.; Lewsey, J.; Gulabivala, K. Outcome of primary root canal treatment: Systematic review of the literature—Part 2. Influence of clinical factors. Int. Endod. J. 2008, 41, 6–31. [Google Scholar] [CrossRef]
- Ng, Y.L.; Mann, V.; Gulabivala, K. A prospective study of the factors affecting outcomes of nonsurgical root canal treatment: Part 1: Periapical health. Int. Endod. J. 2011, 44, 583–609. [Google Scholar] [CrossRef]
- Ng, Y.L.; Mann, V.; Gulabivala, K. A prospective study of the factors affecting outcomes of non-surgical root canal treatment: Part 2: Tooth survival. Int. Endod. J. 2011, 44, 610–625. [Google Scholar] [CrossRef] [PubMed]
- Vertucci, F.J. Root canal anatomy of the human permanent teeth. Oral. Surg. Oral. Med. Oral. Pathol. 1984, 58, 589–599. [Google Scholar] [CrossRef]
- Weine, F.S.; Healey, H.J.; Gerstein, H.; Evanson, L. Canal configuration in the mesiobuccal root of the maxillary first molar and its endodontic significance. Oral. Surg. Oral. Med. Oral. Pathol. 1969, 28, 419–425. [Google Scholar] [CrossRef]
- Park, J.W.; Lee, J.K.; Ha, B.H.; Choi, J.H.; Perinpanayagam, H. Three-dimensional analysis of maxillary first molar mesiobuccal root canal configuration and curvature using micro-computed tomography. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. Endod. 2009, 108, 437–442. [Google Scholar] [CrossRef]
- Kim, Y.; Chang, S.W.; Lee, J.K.; Chen, I.P.; Kaufman, B.; Jiang, J.; Cha, B.Y.; Zhu, Q.; Safavi, K.E.; Kum, K.Y. A micro-computed tomography study of canal configuration of multiple-canalled mesiobuccal root of maxillary first molar. Clin. Oral. Investig. 2013, 17, 1541–1546. [Google Scholar] [CrossRef] [PubMed]
- Martins, J.N.R.; Marques, D.; Francisco, H.; Caramês, J. Gender influence on the number of roots and root canal system configuration in human permanent teeth of a Portuguese subpopulation. Quintessence Int. 2018, 49, 103–111. [Google Scholar]
- Martins, J.N.R.; Ordinola-Zapata, R.; Marques, D.; Francisco, H.; Caramês, J. Differences in root canal system configuration in human permanent teeth within different age groups. Int. Endod. J. 2018, 51, 931–941. [Google Scholar] [CrossRef] [PubMed]
- Martins, J.N.R.; Marques, D.; Silva, E.; Caramês, J.; Versiani, M.A. Prevalence Studies on Root Canal Anatomy Using Cone-beam Computed Tomographic Imaging: A Systematic Review. J. Endod. 2019, 45, 372–386. [Google Scholar] [CrossRef]
- Valenti-Obino, F.; Di Nardo, D.; Quero, L.; Miccoli, G.; Gambarini, G.; Testarelli, L.; Galli, M. Symmetry of root and root canal morphology of mandibular incisors: A cone-beam computed tomography study in vivo. J. Clin. Exp. Dent. 2019, 11, e527–e533. [Google Scholar] [CrossRef]
- Mashyakhy, M.; Gambarini, G. Root and Root Canal Morphology Differences Between Genders: A Comprehensive in-vivo CBCT Study in a Saudi Population. Acta Stomatol. Croat. 2019, 53, 213–246. [Google Scholar] [CrossRef]
- Ratanajirasut, R.; Panichuttra, A.; Panmekiate, S. A Cone-beam Computed Tomographic Study of Root and Canal Morphology of Maxillary First and Second Permanent Molars in a Thai Population. J. Endod. 2018, 44, 56–61. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.C.; Cheng, W.C.; Chung, M.P.; Su, C.C.; Weng, P.W.; Cathy Tsai, Y.W.; Chiang, H.S.; Yeh, H.W.; Chung, C.H.; Shieh, Y.S.; et al. Complicated Root Canal Morphology of Mandibular Lateral Incisors Is Associated with the Presence of Distolingual Root in Mandibular First Molars: A Cone-beam Computed Tomographic Study in a Taiwanese Population. J. Endod. 2018, 44, 73–79. [Google Scholar] [CrossRef]
- Alfawaz, H.; Alqedairi, A.; Alkhayyal, A.K.; Almobarak, A.A.; Alhusain, M.F.; Martins, J.N.R. Prevalence of C-shaped canal system in mandibular first and second molars in a Saudi population assessed via cone beam computed tomography: A retrospective study. Clin. Oral. Investig. 2019, 23, 107–112. [Google Scholar] [CrossRef]
- Gambarini, G.; Piasecki, L.; Ropini, P.; Miccoli, G.; Di Nardo, D.; Testarelli, L. Cone-beam computed tomographic analysis on root and canal morphology of mandibular first permanent molar among multiracial population in Western European population. Eur. J. Dent. 2018, 12, 434–438. [Google Scholar] [CrossRef][Green Version]
- Patel, S.; Brown, J.; Pimentel, T.; Kelly, R.D.; Abella, F.; Durack, C. Cone beam computed tomography in Endodontics—a review of the literature. Int. Endod. J. 2019, 52, 1138–1152. [Google Scholar] [CrossRef]
- European Society of Endodontology; Patel, S.; Durack, C.; Abella, F.; Roig, M.; Shemesh, H.; Lambrechts, P.; Lemberg, K. European Society of Endodontology position statement: The use of CBCT in endodontics. J. Endod. 2014, 47, 502–504. [Google Scholar] [CrossRef] [PubMed]
- Gambarini, G.; Galli, M.; Stefanelli, L.V.; Di Nardo, D.; Morese, A.; Seracchiani, M.; De Angelis, F.; Di Carlo, S.; Testarelli, L. Endodontic Microsurgery Using Dynamic Navigation System: A Case Report. J. Endod. 2019, 45, 1397–1402. [Google Scholar] [CrossRef] [PubMed]
- Gambarini, G.; Galli, M.; Morese, A.; Abduljabbar, F.; Seracchiani, M.; Stefanelli, L.V.; Giovarruscio, M.; Di Nardo, D.; Testarelli, L. Digital Design of Minimally Invasive Endodontic Access Cavity. Appl. Sci. 2020, 10, 3513. [Google Scholar] [CrossRef]
- Patel, S.; Brown, J.; Semper, M.; Abella, F.; Mannocci, F. European Society of Endodontology position statement: Use of cone beam computed tomography in Endodontics: European Society of Endodontology (ESE) developed by. J. Endod. 2019, 52, 1675–1678. [Google Scholar] [CrossRef]
- Patel, S.; Patel, R.; Foschi, F.; Mannocci, F. The Impact of Different Diagnostic Imaging Modalities on the Evaluation of Root Canal Anatomy and Endodontic Residents’ Stress Levels: A Clinical Study. J. Endod. 2019, 45, 406–413. [Google Scholar] [CrossRef]
- Kim, G.B.; Lee, S.; Kim, H.; Yang, D.H.; Kim, Y.H.; Kyung, Y.S.; Kim, C.S.; Choi, S.H.; Kim, B.J.; Ha, H.; et al. Three-Dimensional Printing: Basic Principles and Applications in Medicine and Radiology. Korean J. Radiol. 2016, 17, 182–197. [Google Scholar] [CrossRef]
- Reymus, M.; Fotiadou, C.; Kessler, A.; Heck, K.; Hickel, R.; Diegritz, C. 3D printed replicas for endodontic education. Int. Endod. J. 2019, 52, 123–130. [Google Scholar] [CrossRef] [PubMed]
- Sokolowski, A.A.; Sokolowski, A.A.; Kammerhofer, J.; Madreiter-Sokolowski, C.T.; Payer, M.; Koller, M.; Jakse, N.; Wegscheider, W.A. Accuracy assessment of 3D-printed tooth replicas. Int. J. Comput. Dent. 2019, 22, 321–329. [Google Scholar] [CrossRef]
- Kamio, T.; Hayashi, K.; Onda, T.; Takaki, T.; Shibahara, T.; Yakushiji, T.; Shibui, T.; Kato, H. Utilizing a low-cost desktop 3D printer to develop a “one-stop 3D printing lab” for oral and maxillofacial surgery and dentistry fields. 3D Print. Med. 2018, 4, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Hanafi, A.; Donnermeyer, D.; Schäfer, E.; Bürklein, S. Perception of a modular 3D print model in undergraduate endodontic education. Int. Endod. J. 2020, 53, 1007–1016. [Google Scholar] [CrossRef]
- Xu, H.D.; Miron, R.J.; Zhang, X.X.; Zhang, Y.F. Allogenic tooth transplantation using 3D printing: A case report and review of the literature. World J. Clin. Cases 2019, 7, 2587–2596. [Google Scholar] [CrossRef]
- Oehlers, F.A. Dens invaginatus (dilated composite odontome). I. Variations of the invagination process and associated anterior crown forms. Oral. Surg. Oral. Med. Oral. Pathol. 1957, 10, 1204–1218. [Google Scholar] [CrossRef]
- Ventola, C.L. Medical Applications for 3D Printing: Current and Projected Uses. Pharm. Ther. 2014, 39, 704–711. [Google Scholar]
- Gallacher, A.; Ali, R.; Bhakta, S. Dens invaginatus: Diagnosis and management strategies. Br. Dent. J. 2016, 221, 383–387. [Google Scholar] [CrossRef]
- Zhu, J.; Wang, X.; Fang, Y.; Von den Hoff, J.W.; Meng, L. An update on the diagnosis and treatment of dens invaginatus. Aust. Dent. J. 2017, 62, 261–275. [Google Scholar] [CrossRef]
- Shokouhinejad, N.; Nekoofar, M.H.; Ashoftehyazdi, K.; Zahraee, S.; Khoshkhounejad, M. Marginal adaptation of new bioceramic materials and mineral trioxide aggregate: A scanning electron microscopy study. Iran. Endod. J. 2014, 9, 144–148. [Google Scholar]
- Malcić, A.; Jukić, S.; Brzović, V.; Miletić, I.; Pelivan, I.; Anić, I. Prevalence of root dilaceration in adult dental patients in Croatia. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. Endod. 2006, 102, 104–109. [Google Scholar] [CrossRef]
- Nabavizadeh, M.; Sedigh Shamsi, M.; Moazami, F.; Abbaszadegan, A. Prevalence of root dilaceration in adult patients referred to shiraz dental school (2005–2010). J. Dent. 2013, 14, 160–164. [Google Scholar]
- Jafarzadeh, H.; Abbott, P.V. Dilaceration: Review of an endodontic challenge. J. Endod. 2007, 33, 1025–1030. [Google Scholar] [CrossRef] [PubMed]
- Elnaghy, A.M.; Elsaka, S.E.; Mandorah, A.O. In vitro comparison of cyclic fatigue resistance of TruNatomy in single and double curvature canals compared with different nickel-titanium rotary instruments. BMC Oral. Health 2020, 20, 38. [Google Scholar] [CrossRef] [PubMed]
- Riyahi, A.M.; Bashiri, A.; Alshahrani, K.; Alshahrani, S.; Alamri, H.M.; Al-Sudani, D. Cyclic Fatigue Comparison of TruNatomy, Twisted File, and ProTaper Next Rotary Systems. Int. J. Dent. 2020, 2020, 3190938. [Google Scholar] [CrossRef]






Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tonini, R.; Xhajanka, E.; Giovarruscio, M.; Foschi, F.; Boschi, G.; Atav-Ates, A.; Cicconetti, A.; Seracchiani, M.; Gambarini, G.; Testarelli, L.; et al. Print and Try Technique: 3D-Printing of Teeth with Complex Anatomy a Novel Endodontic Approach. Appl. Sci. 2021, 11, 1511. https://doi.org/10.3390/app11041511
Tonini R, Xhajanka E, Giovarruscio M, Foschi F, Boschi G, Atav-Ates A, Cicconetti A, Seracchiani M, Gambarini G, Testarelli L, et al. Print and Try Technique: 3D-Printing of Teeth with Complex Anatomy a Novel Endodontic Approach. Applied Sciences. 2021; 11(4):1511. https://doi.org/10.3390/app11041511
Chicago/Turabian StyleTonini, Riccardo, Edit Xhajanka, Massimo Giovarruscio, Federico Foschi, Giulia Boschi, Ayfer Atav-Ates, Andrea Cicconetti, Marco Seracchiani, Gianluca Gambarini, Luca Testarelli, and et al. 2021. "Print and Try Technique: 3D-Printing of Teeth with Complex Anatomy a Novel Endodontic Approach" Applied Sciences 11, no. 4: 1511. https://doi.org/10.3390/app11041511
APA StyleTonini, R., Xhajanka, E., Giovarruscio, M., Foschi, F., Boschi, G., Atav-Ates, A., Cicconetti, A., Seracchiani, M., Gambarini, G., Testarelli, L., & Pacifici, L. (2021). Print and Try Technique: 3D-Printing of Teeth with Complex Anatomy a Novel Endodontic Approach. Applied Sciences, 11(4), 1511. https://doi.org/10.3390/app11041511









