Characterization of Infant Cardiopulmonary Resuscitation Delivery with Range Sensor Feedback on Performance
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
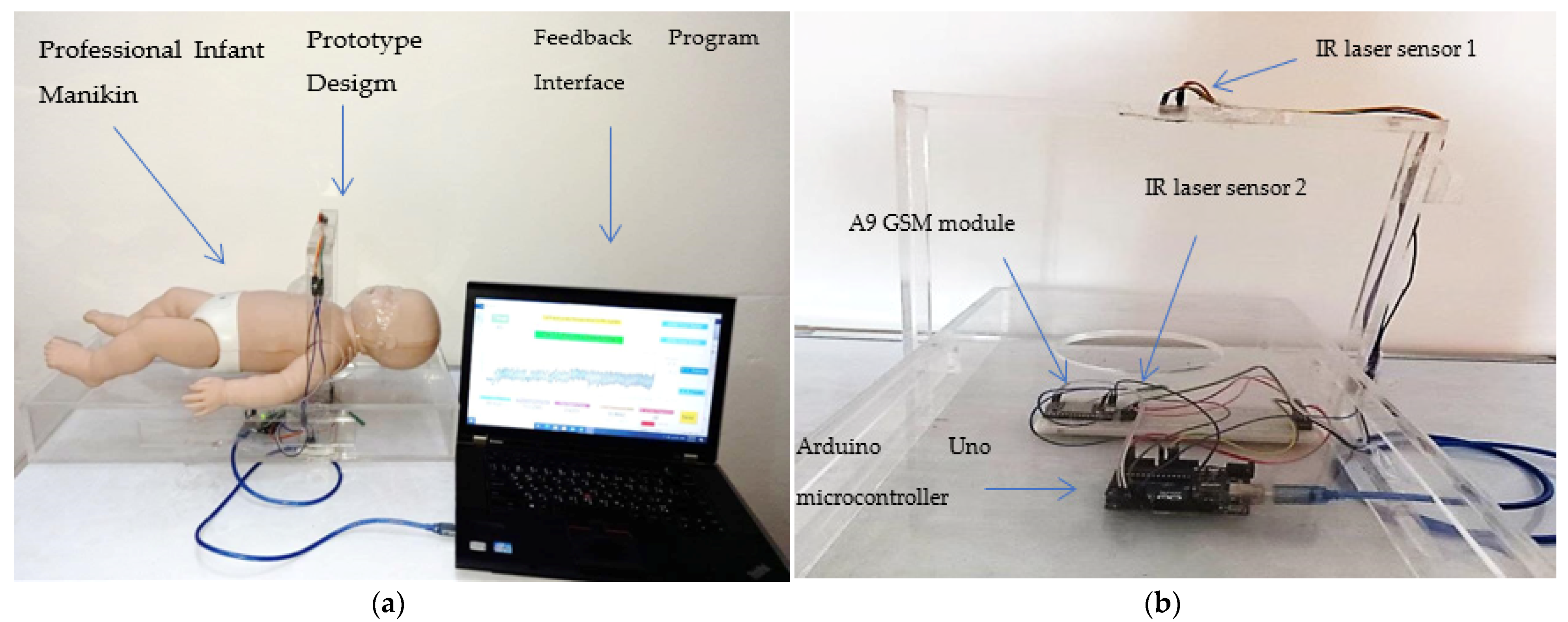
2.2. Experimental Setup
3. Results
3.1. CPR Performance with No-Feedback and with Real-Time Feedback System
3.1.1. Chest Compression Depth
3.1.2. Chest Release Force
3.1.3. Compression Rate
3.1.4. Compression Duty Cycle
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mendler, M.R.; Weber, C.; Hassan, M.A.; Huang, L.; Waitz, M.; Mayer, B.; Hummler, H.D. Effect of Different Respiratory Modes on Return of Spontaneous Circulation in a Newborn Piglet Model of Hypoxic Cardiac Arrest. Neonatology 2015, 109, 22–30. [Google Scholar] [CrossRef] [PubMed]
- Solevåg, A.L.; Schmölzer, G.M.; O’Reilly, M.; Lu, M.; Lee, T.-F.; Hornberger, L.K.; Nakstad, B.; Cheung, P.-Y. Myocardial perfusion and oxidative stress after 21% vs. 100% oxygen ventilation and uninterrupted chest compressions in severely asphyxiated piglets. Resuscitation 2016, 106, 7–13. [Google Scholar] [CrossRef]
- Cunningham, L.M.; Mattu, A.; O’Connor, R.E.; Brady, W.J. Cardiopulmonary resuscitation for cardiac arrest: The importance of uninterrupted chest compressions in cardiac arrest resuscitation. Am. J. Emerg. Med. 2012, 30, 1630–1638. [Google Scholar] [CrossRef] [PubMed]
- Nolan, J. High-quality cardiopulmonary resuscitation. Curr. Opin. Crit. Care 2014, 20, 227–233. [Google Scholar] [CrossRef] [PubMed]
- Dorfsman, M.L.; Menegazzi, J.J.; Wadas, R.J.; Auble, T.E. Two-thumb vs. two-finger chest compression in an infant model of prolonged cardiopulmonary resuscitation. Acad. Emerg. Med. 2000, 7, 1077–1082. [Google Scholar] [CrossRef]
- Tsou, J.-Y.; Kao, C.-L.; Chang, C.-J.; Tu, Y.-F.; Su, F.-C.; Chi, C.-H. Biomechanics of two-thumb versus two-finger chest compression for cardiopulmonary resuscitation in an infant manikin model. Eur. J. Emerg. Med. 2020, 27, 132–136. [Google Scholar] [CrossRef]
- Alkhafaji, F.M.; Khalid, G.A.; Al-Naji, A. Application of Cardiopulmonary Resuscitation Mechanism in Infant Population: A Short Review. IOP Conf. Ser. Mater. Sci. Eng. 2021, 1105, 012077. [Google Scholar] [CrossRef]
- Menegazzi, J.J.; Auble, T.E.; Nicklas, K.A.; Hosack, G.M.; Rack, L.; Goode, J.S. Two-thumb versus two-finger chest compression during CPR in a swine infant model of cardiac arrest. Ann. Emerg. Med. 1993, 22, 240–243. [Google Scholar] [CrossRef]
- Houri, P.K.; Frank, L.R.; Menegazzi, J.J.; Taylor, R. A randomized, controlled trial of two-thumb vs two-finger chest compression in a swine infant model of cardiac arrest [see comment]. Prehosp. Emerg. Care 1997, 1, 65–67. [Google Scholar] [CrossRef]
- Haque, I.U.; Udassi, J.P.; Udassi, S.; Theriaque, D.W.; Shuster, J.J.; Zaritsky, A.L. Chest compression quality and rescuer fatigue with increased compression to ventilation ratio during single rescuer pediatric CPR. Resuscitation 2008, 79, 82–89. [Google Scholar] [CrossRef]
- Whitelaw, C.C.; Slywka, B.; Goldsmith, L. Comparison of a two-finger versus two-thumb method for chest compressions by healthcare providers in an infant mechanical model. Resuscitation 2000, 43, 213–216. [Google Scholar] [CrossRef]
- Merchant, R.M.; Topjian, A.A.; Panchal, A.R.; Cheng, A.; Aziz, K.; Berg, K.M.; Lavonas, E.J.; Magid, D.J. Part 1: Executive Summary: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2020, 142, S337–S357. [Google Scholar] [CrossRef] [PubMed]
- De Caen, A.R.; Kleinman, M.E.; Chameides, L.; Atkins, D.L.; Berg, R.A.; Berg, M.D.; Bhanji, F.; Biarent, D.; Bingham, R.; Coovadia, A.H. Part 10: Paediatric basic and advanced life support: International consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Resuscitation 2010, 81, 213–259. [Google Scholar] [CrossRef] [PubMed]
- Atkins, D.L.; Berger, S.; Duff, J.P.; Gonzales, J.C.; Hunt, E.A.; Joyner, B.L.; Maeney, P.A.; Niles, D.E.; Samson, R.A.; Schexnayder, S.M. Part 11: Pediatric basic life support and cardiopulmonary resuscitation quality: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2015, 132, S519–S525. [Google Scholar] [CrossRef] [PubMed]
- Biarent, D.; Bingham, R.; Eich, C.; López-Herce, J.; Maconochie, I.; Rodríguez-Núnez, A.; Rajka, T.; Zideman, D. European Resuscitation Council Guidelines for Resuscitation 2010 Section 6. Paediatric life support. Resuscitation 2010, 81, 1364–1388. [Google Scholar] [CrossRef] [PubMed]
- Atkins, D.L.; Berger, S. Improving Outcomes from Out-of-Hospital Cardiac Arrest in Young Children and Adolescents. Pediatr. Cardiol. 2011, 33, 474–483. [Google Scholar] [CrossRef]
- Bardai, A.; Berdowski, J.; van der Werf, C.; Blom, M.T.; Ceelen, M.; van Langen, I.M.; Tijssen, J.G.; Wilde, A.A.; Koster, R.W.; Tan, H.L. Incidence, Causes, and Outcomes of Out-of-Hospital Cardiac Arrest in Children A Comprehensive, Prospective, Population-Based Study in the Netherlands. J. Am. Coll. Cardiol. 2011, 57, 1822–1828. [Google Scholar] [CrossRef]
- Udassi, J.P.; Udassi, S.; Theriaque, D.W.; Shuster, J.J.; Zaritsky, A.L.; Haque, I.U. Effect of alternative chest compression techniques in infant and child on rescuer performance. Pediatr. Crit. Care Med. 2009, 10, 328–333. [Google Scholar] [CrossRef]
- Martin, P.; Theobald, P.; Kemp, A.; Maguire, S.; Maconochie, I.; Jones, M. Real-time feedback can improve infant manikin cardiopulmonary resuscitation by up to 79%—A randomised controlled trial. Resuscitation 2013, 84, 1125–1130. [Google Scholar] [CrossRef]
- Kandasamy, J.; Theobald, P.S.; Maconochie, I.K.; Jones, M.D. Can real-time feedback improve the simulated infant cardiopulmonary resuscitation performance of basic life support and lay rescuers? Arch. Dis. Child. 2019, 104, 793–801. [Google Scholar] [CrossRef]
- Lakomek, F.; Lukas, R.-P.; Brinkrolf, P.; Mennewisch, A.; Steinsiek, N.; Gutendorf, P.; Sudowe, H.; Heller, M.; Kwiecien, R.; Zarbock, A.; et al. Erratum: Real-time feedback improves chest compression quality in out-of-hospital cardiac arrest: A prospective cohort study. Plos One 2020, 15, e0229431. [Google Scholar] [CrossRef]
- Abella, B.S.; Edelson, D.P.; Kim, S.; Retzer, E.; Myklebust, H.; Barry, A.M.; O’Hearn, N.; Hoek, T.L.V.; Becker, L.B. CPR quality improvement during in-hospital cardiac arrest using a real-time audiovisual feedback system. Resuscitation 2007, 73, 54–61. [Google Scholar] [CrossRef]
- Lin, Y.; Cheng, A.; Grant, V.J.; Currie, G.R.; Hecker, K.G. Improving CPR quality with distributed practice and real-time feedback in pediatric healthcare providers—A randomized controlled trial. Resuscitation 2018, 130, 6–12. [Google Scholar] [CrossRef] [PubMed]
- Krasteva, V.; Jekova, I.; Didon, J.-P. An audiovisual feedback device for compression depth, rate and complete chest recoil can improve the CPR performance of lay persons during self-training on a manikin. Physiol. Meas. 2011, 32, 687–699. [Google Scholar] [CrossRef] [PubMed]
- Gregson, R.K.; Cole, T.; Skellett, S.; Bagkeris, E.; Welsby, D.; Peters, M. Randomised crossover trial of rate feedback and force during chest compressions for paediatric cardiopulmonary resuscitation. Arch. Dis. Child. 2016, 102, 403–409. [Google Scholar] [CrossRef]
- Jiang, J.; Zou, Y.; Shi, W.; Zhu, Y.; Tao, R.; Jiang, Y.; Lu, Y.; Tong, J. Two-thumb–encircling hands technique is more advisable than 2-finger technique when lone rescuer performs cardiopulmonary resuscitation on infant manikin. Am. J. Emerg. Med. 2015, 33, 531–534. [Google Scholar] [CrossRef] [PubMed]
- Christman, C.; Hemway, R.J.; Wyckoff, M.H.; Perlman, J.M. The two-thumb is superior to the two-finger method for administering chest compressions in a manikin model of neonatal resuscitation. Arch. Dis. Child. Fetal Neonatal Ed. 2010, 96, F99–F101. [Google Scholar] [CrossRef] [PubMed]
- Huynh, T.K.; Hemway, R.J.; Perlman, J.M. The Two-Thumb Technique Using an Elevated Surface is Preferable for Teaching Infant Cardiopulmonary Resuscitation. J. Pediatr. 2012, 161, 658–661. [Google Scholar] [CrossRef]
- Kleinman, M.E.; De Caen, A.R.; Chameides, L.; Atkins, D.L.; Berg, R.A.; Berg, M.C.; Bhanji, F.; Biarent, D.; Bingham, R.; Coovadia, A.H. Part 10: Pediatric basic and advanced life support: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Circulation 2010, 122, 971093. [Google Scholar] [CrossRef]
- Kitamura, T.; Iwami, T.; Kawamura, T.; Nagao, K.; Tanaka, H.; Nadkarni, V.M.; Berg, R.A.; Hiraide, A. Conventional and chestcompression- only cardiopulmonary resuscitation by bystanders for children who have out-of-hospital cardiac arrests: A prospective, nationwide, populationbased cohort study. Lancet 2010, 375, 1347–1354. [Google Scholar] [CrossRef]
- López-Herce, J.; García, C.; Dominguez-Sampedro, P.; Rodriguez-Nunez, A.; Carrillo, A.; Calvo, C.; Delgado, M.A.; Spanish Study Group of Cardiopulmonary Arrest in Children. Outcome of Out-of-Hospital Cardiorespiratory Arrest in Children. Pediatr. Emerg. Care 2005, 21, 807–815. [Google Scholar] [CrossRef][Green Version]
- Udassi, S.; Udassi, J.P.; Lamb, M.A.; Theriaque, D.W.; Shuster, J.J.; Zaritsky, A.L.; Haque, I.U. Two-thumb technique is superior to two-finger technique during lone rescuer infant manikin CPR. Resuscitation 2010, 81, 712–717. [Google Scholar] [CrossRef]
- Reynolds, C.; Cox, J.; Livingstone, V.; Dempsey, E.M. Rescuer Exertion and Fatigue Using Two-Thumb vs. Two-Finger Method During Simulated Neonatal Cardiopulmonary Resuscitation. Front. Pediatr. 2020, 8, 133. [Google Scholar] [CrossRef]
- Millin, M.G.; Bogumil, D.; Fishe, J.N.; Burke, R.V. Comparing the two-finger versus two-thumb technique for single person infant CPR: A systematic review and meta-analysis. Resuscitation 2020, 148, 161–172. [Google Scholar] [CrossRef]
- Martin, P.S.; Kemp, A.M.; Theobald, P.; Maguire, S.A.; Jones, M.D. Do chest compressions during simulated infant CPR comply with international recommendations? Arch. Dis. Child. 2012, 98, 576–581. [Google Scholar] [CrossRef] [PubMed]





Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alkhafaji, F.M.; Khalid, G.A.; Al-Naji, A.; Hussein, B.M.; Chahl, J. Characterization of Infant Cardiopulmonary Resuscitation Delivery with Range Sensor Feedback on Performance. Appl. Sci. 2021, 11, 9813. https://doi.org/10.3390/app11219813
Alkhafaji FM, Khalid GA, Al-Naji A, Hussein BM, Chahl J. Characterization of Infant Cardiopulmonary Resuscitation Delivery with Range Sensor Feedback on Performance. Applied Sciences. 2021; 11(21):9813. https://doi.org/10.3390/app11219813
Chicago/Turabian StyleAlkhafaji, Farah M., Ghaidaa A. Khalid, Ali Al-Naji, Basheer M. Hussein, and Javaan Chahl. 2021. "Characterization of Infant Cardiopulmonary Resuscitation Delivery with Range Sensor Feedback on Performance" Applied Sciences 11, no. 21: 9813. https://doi.org/10.3390/app11219813
APA StyleAlkhafaji, F. M., Khalid, G. A., Al-Naji, A., Hussein, B. M., & Chahl, J. (2021). Characterization of Infant Cardiopulmonary Resuscitation Delivery with Range Sensor Feedback on Performance. Applied Sciences, 11(21), 9813. https://doi.org/10.3390/app11219813








