Effectiveness of Prone Positioning in Patients with COVID-19-Related Acute Respiratory Distress Syndrome Undergoing Invasive Mechanical Ventilation
Abstract
1. Introduction
1.1. Acute Respiratory Distress Syndrome
1.2. Prone Position
1.3. Coronavirus
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| PP | Prone position |
| ECMO | Extracorporeal oxygenation membrane |
| MMSS | Upper limbs |
| MMII | Lower limbs |
| PaO₂ | Partial pressure of oxygen in arterial blood |
| PaCO₂ | Partial pressure of carbon dioxide in arterial blood |
| ARDS | Acute respiratory distress syndrome |
| ICU | Intensive care unit |
| MV | Mechanical ventilation |
| IMV | Invasive mechanical ventilation |
| NIMV | Non-invasive mechanical ventilation |
Appendix A
| Authors; Year | Type of Study | Patients | Conclusion |
|---|---|---|---|
| Kim W, Kang B, Chung C, Park S, Oh J, Park S, et al., 2018 | Analytical. Of Cohorts. Retrospective | 62 | PP position before ECMO was not associated with an increase in mortality in patients with severe ARDS. The group on PP had a lower mean maximum inspiratory pressure; similarly, the dynamic conduction pressure was also lower before ECMO. |
| Guérin C, Albert RK, Beitler J, Gattinoni L, Jaber S, Marini JJ, et al., 2020 | Bibliographic review | 34 | The PP position has been shown to be effective in patients with moderate to severe ARDS who present IMV, showing a marked improvement in arterial blood gases. This improvement is due to an improvement in the ventilation/perfusion ratio. In non-intubated patients, this position has begun to be used, but studies are lacking to confirm its favorable impact. The main complications are pressure ulcers and facial edema. |
| Weiss TT, Cerda F, Scott JB, Kaur R, Sungurlu S, Mirza SH, et al., 2020 | Analytical. Of Cohorts. Retrospective. | 42 | The prone position improves oxygenation in patients with ARDS secondary to COVID-19 who require IMV. This improvement occurred from the second and third cycles of prone decubitus in those surviving patients. This was not the case in those who ended up needing ECMO therapy or who died, who had little or no response to pronation cycles. |
| Peko L, Barakat-Johnson M, Gefen A.; 2020 | Analytical. Cases and Controls. | 1 case and 1 control | The application of prophylactic dressings of multiple layers of soft silicone foam on the forehead and chin in PP patients notably reduces the load on the soft facial tissues by more than 50%, in both sites, compared with not putting any type of protection. This study supports, for the first time, the nursing practice of this type of dressings in prone patients, both in the operating room and in the ICU. |
| Ibarra G, Rivera A, Fernandez-Ibarburu B, Lorca-García, Gacia-Ruano A; 2020 | Analytical. Cases and Controls. | 57 cases and 17 controls | The position of PP in ARDS has been shown to decrease mortality, but this position leads to the appearance of PUs. The most frequent location is the face (for medical devices, TET and NGS) and the pressure itself on the bony prominences. Within the face, the most frequent areas are as follows: cheek (18%), chin (16%), and forehead (8%). The frequency of these lesions was as follows: stage II (64%) and I (28%). Patients with grade IV PU ended up dying, so these lesions are considered preterm event markers. The best treatment for PUs is prevention. |
| Martel T, Orgill DP.; 2020 | Narrative Review | 30 | The position of PP is related to higher survival rates in patients with SARS-CoV-2. However, this posture increases the risk of PU appearance by three times compared with the supine position. This because of the limitations in carrying out postural changes, the presence of medical devices on the face, and the increase in tissue moisture and facial edema. In addition to PP, COVID-19 produces a cytokine storm, with consequent endothelial dysfunction and ischemia, which further enhances the appearance of these types of lesions. |
| Perrillat A, Foletti JM, Lacagne AS, Guyot L, Graillon N.; 2020 | Descriptive. Number of cases. | 2 | PP facilitates recruitment of the dorsal lung regions, increases lung volume at the end of expiration, and reduces alveolar bypass. In the prevention of facial PUs, it is recommended to use a specific head cushion, gels, or silicone dressings; change the position of the head 2–3 times during each session; close the eyelids with occlusive dressings; and correct the systemic parameters that prevent healing (hypoxemia, anemia, or malnutrition). Treatment consists of debridement of the necrotic tissue and promoting its healing with dressings: vaseline (linitul) or alginate gauze if the wound is highly exudative. |
| Sleiwah A, Nair G, Mughal M, Lancaster K, Ahmad I.; 2020 | Analytical. Cohorts. Retrospective. | 60 | PP is a strategy that increases arterial oxygenation and decreases the difference between perfusion and ventilation. Facial pressure ulcers are complications. These are prevented by replacing commercial ETT restraints with white cloth tape and treated with silicone foam dressings, paraffin gauze, or clonamphenicol (non-surgical). |
| Singh C, Tay J, Shoqirat N.; 2020 | Descriptive. Cross-sectional. | 4 | All admitted patients were evaluated according to the Braden scale. Even applying preventive measures such as postural changes and pillows and other devices to relieve pressure areas, extensive ulcers appeared, so more extensive studies are needed to define the best way to prevent these injuries. |
| Carrillo R, Mejía L, Monares E, Chavarría U, Díaz A, Ayala M, et al., 2020 | Bibliographic review | 21 | The prone position demonstrated a significant improvement in alveolar recruitment (PaO2/FiO2 ratio of 120 mmHg in the supine position to 182 mmHg in the prone position) in those patients with IMV in the supine position in the ICU. |
| Concha P, Treso-Geira M, Esteve-Sala C.; 2021 | Descriptive. Number of cases. Retrospective | 17 | Prolonged pronation sessions, with an average of almost 48 h, showed greater efficacy in terms of mortality, in relation to those of 8 or 16 h a day that had been carried out. However, this increase in time increases the risk of the appearance of pressure ulcers, facial edema, and eye difficulties. |
| Chen Y, Zhang J, Feng H, Wan F, Zhang Y, Tan L.; 2021 | Bibliographic review | 40 | The prone position for long periods of time is a feasible and safe treatment to prolong the survival time of patients with COVID-19 disease, who are in the ICU, intubated, and mechanically ventilated. |
| Qadri SK, Ng P, Toh TSW, Loh SW, Tan HL, Lin CB, Fan E, Lee JH.; 2020 | Systematic review | 1899 | Based on the findings of our review, we recommend the prone position in patients with moderate to severe COVID-19 ARDS as per existing guidelines. A trial of the prone position should be considered for non-intubated COVID-19 patients with hypoxemic respiratory failure, as long as this does not result in a delay in intubation. |
| Langer T, Brioni M, Guzzardella A, Carlesso E, Cabrini L, Castelli G, Dalla Corte F, et al., 2021 | Analytical. Of Cohorts. Retrospective. | 1057 | During the COVID-19 pandemic, the prone position has been widely adopted to treat mechanically ventilated patients with respiratory failure. The majority of patients improved their oxygenation during prone position, most likely owing to a better ventilation perfusion matching. |
| Vollenberg R, Matern P, Nowacki T, Fuhrmann V, Padberg JS, Ochs K, Schütte-Nütgen K, et al., 2021 | Prospective bicentric study. | 13 | The PP significantly improves oxygenation in COVID-19 ARDS patients. The data suggest that they also benefit most from an early PP. A decrease in minute ventilation may result in fewer PaCO2 responders. LC may be a predictive outcome parameter in COVID-19 patients. Trial registration: retrospectively registered. |
| Lucchini A, Bambi S, Mattiussi E, Elli S, Villa L, Bondi H, Rona R, Fumagalli R, Foti G.; 2020 | Single-center, retrospective, observational study | 98 | The onset rate of complications given by the use of prone position in ARDS patients is similar to data reported by previous literature. The implementation of a dedicated protocol in specialized centers and the involvement of five trained and skilled professionals while moving the patient in the prone position are recommended to prevent the occurrence of similar adverse events. |
| Gleissman H, Forsgren A, Andersson E, Lindqvist E, Lipka Falck A, Cronhjort M, Dahlberg M, Günther M.; 2021 | Case series | 44 | Proning increased PaO2/FiO2, primarily in patients with PaO2/FiO2 of approximately <120 mm Hg, with a consistency over three sessions. No characteristic was associated with non-responding, which is why proning may be considered in most patients. Further study is required to evaluate mortality. |
| Shelhamer MC, Wesson PD, Solari IL, Jensen DL, Steele WA, Dimitrov VG, Kelly JD, Aziz S, et al., 2021 | Cohort study | 335 | Prone positioning in patients with moderate to severe ARDS due to COVID-19 is associated with reduced mortality and improved physiologic parameters. One in-hospital death could be averted for every eight patients treated. Replicating results and scaling the intervention are important, but prone positioning may represent an additional therapeutic option in patients with ARDS due to COVID-19. |
| Binda F, Marelli F, Galazzi A, Pascuzzo R, Adamini I, Laquintana D.; 2021 | Cohort study | 86 | Prone positioning is one strategy available for treating acute respiratory distress syndrome in patients with COVID-19. During this pandemic, prone positioning can be used extensively as rescue therapy, per a specific protocol, in ICU. |
| Ng JA, Miccile LA, Iracheta C, Berndt C, Detwiller M, Yuse C, Tolland J.; 2020 | Case report | 2 | The description of the development, operations, evolution, and utilization of a rehabilitation therapist prone team acts as a guide for future development and implementation. |
| Araújo MS, Santos MMPD, Silva CJA, Menezes RMP, Feijão AR, Medeiros SM.; 2021 | Systematic review | 12 | Positive outcomes outweighed complications. Various cycles of prone positioning are needed, which may cause potential work overload for the health staff. Therefore, an appropriate number of trained workers is necessary, in addition to specific institutional protocols to ensure patient safety in this context. |
References
- Ministry of Health, Government of Spain. Spanish Agency for Medicines and Health Products (AEMPS) Recommends the Authorization of the First Vaccine against COVID-19. 2020. Available online: https://www.aemps.gob.es/informa/notasinformativas/laaemps/2020-laaemps/la-ema-recomienda-la-autorizacion-de-la-primera-vacuna-frente-a-la-covid-19/ (accessed on 21 July 2021).
- Sweeney, R.M.; McAuley, D.F. Acute respiratory distress syndrome. Lancet 2016, 388, 2416–2430. [Google Scholar] [CrossRef]
- Luis, N.; Sánchez, I.; Bengoetxea, U.X.; Rodrigo, M.P.; García, J.M.; Aguilera, L. Síndrome de distrés respiratorio agudo: Revisión a propósito de la definición de Berlín. Rev. Española de Anestesiología y Reanimación 2014, 61, 319–327. [Google Scholar]
- Cardinal-Fernández, P.; Correger, E.; Villanueva, J.; Rios, F. Distrés respiratorio agudo: Del síndrome a la enfermedad. Med. Intensiva 2016, 40, 169–175. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez, R.D.; Ordoñez, S.A.; Gómez, J.L.; Camargo, M.E. Decúbito prono en el Síndrome de Dificultad Respiratoria Aguda, de la fisiología a la práctica clínica. Rev. Méd. UIS 2016, 29, 81–101. [Google Scholar]
- Mitchell, D.A.; Seckel, M.A. Acute respiratory distress syndrome and prone positioning. AACN Adv. Crit. Care 2018, 29, 415–425. [Google Scholar] [CrossRef] [PubMed]
- Pham, T.; Rubenfeld, G.D. The epidemiology of Acute Respiratory Distress Syndrome. A 50th Bithday Review. Am. J. Respir. Adn Crit. Care Med. 2017, 195, 860–870. [Google Scholar] [CrossRef]
- García, J.; Piqueras, J.; Ortiz, M.C.; Martínez, M.C.; Carrilero, C.; Torralba, M.; Cebrian, E.; Cuesta, M.C.; Murcia, I. Protocolo maniobra de decúbito prono en el servicio de medicina intensiva. Castilla la Mancha (SESCAM). 2018. Available online: https://www.chospab.es/publicaciones/protocolosEnfermeria/documentos/1fa4f12fc6244e81de4663b061ec9a5e.pdf (accessed on 21 July 2021).
- Mora-Arteaga, J.A.; Bernal-Ramírez, O.J.; Rodríguez, S.J. Efecto de la ventilación mecánica en posición prona en pacientes con síndrome de dificultad respiratoria aguda. Una revisión sistemática y metanálisis. Med. Intensiva 2015, 39, 352–365. [Google Scholar] [CrossRef] [PubMed]
- Campello, C.; Vidal, A.; Del Saz, M.I.; Tomás, A.; Villaescusa, M.C. La terapia decúbito prono desde la perspectiva de la enfermera de UCI: Una revisión integrativa. Rev. Científica De Enfermería 2015, 12, 1–16. [Google Scholar]
- Xu, Y.; Deng, X.; Han, Y.; Zhou, L.; He, W.; Chen, S.; Nong, L.; Huang, H.; Zhang, Y.; Yu, T.; et al. A multicenter restrospective review of prone position ventilation in treatment of severe human H7N9 Avian Flu. J. Pone 2015, 10, e0136520. [Google Scholar]
- Jové, E.; Villarrasa, A.; Ortiz, D. Análisis de las complicaciones del decúbito prono en el síndrome de distrés respiratorio agudo: Estándar de calidad, incidencia y factores relacionados. Enf. Intensiva 2017, 28, 125–134. [Google Scholar] [CrossRef] [PubMed]
- Huerta, Y.; Valencia, A.L. Cuidados de Enfermería durante la posición en decúbito prono al paciente con síndrome de dificultad respiratoria. Rev. Mex. Enf. 2020, 8, 70–75. [Google Scholar]
- González, C.A.; Rentería, F.J.; Martínez, R.; Wilfrido, U. Impacto del decúbito prono en el síndrome de insuficiencia respiratoria aguda en pacientes con COVID-19 bajo ventilación mecánica invasiva. Med. Crit. 2020, 34, 326–329. [Google Scholar]
- Loras, C.; Sanz, J.C. Información preliminar de las características virológicas del nuevo coronavirus SARS-CoV-2. REMASP 2020, 4, 1–10. [Google Scholar] [CrossRef][Green Version]
- Ruiz, A.; Jiménez, M. SARS-CoV-2 y pandemia de síndrome respiratorio agudo (COVID-19). Ars. Pharm. 2020, 61, 63–79. [Google Scholar]
- Maguiña, C.; Gastelo, R.; Tequen, A. El nuevo Coronavirus y la pandemia del COVID-19. Rev. Med. Hered. 2020, 31, 125–131. [Google Scholar] [CrossRef]
- Reina, J.; Fraile, P. Características virológicas y diagnóstico del SARS-COV-2. Med. Balear. 2020, 35, 62–68. [Google Scholar]
- Sotomayor, F.; Corbacho, J.M.; Valiente, A.M.; Benítez, Y.; Viera, T. Aspectos generales sobre la estructura del coronavirus del síndrome respiratorio agudo grave 2 (SARS CoV-2). Rev. Cubana Bioméd. 2020, 39, 867. [Google Scholar]
- Palacios, M.; Santos, E.; Velázquez, M.A.; León, M. COVID-19, una emergencia de salud pública mundial. Rev. Clin. Esp. 2021, 221, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Pareja, A.; Giménez, J.; Nicolau, A.; Bosch, C.; Caffaro, M.; Garí, A.; Fernández, G.L.; Jiménez, C.N.; Arbona, M.P.; Castell, M.S.; et al. Medidas de prevención y control de infecciones: El caso del SARS-CoV-2. Med. Balear. 2020, 35, 88–105. [Google Scholar]
- Flynn Makic, M.B. Prone Position of Patients With COVID-19 and Acute Respiratory Distress Syndrome. J. Perianesth. Nurse 2020, 35, 437–438. [Google Scholar] [CrossRef] [PubMed]
- Kim, W.; Kang, B.; Chung, C.; Park, S.; Oh, J.; Park, S.; Cho, W.H.; Sim, Y.S.; Cho, Y.-J.; Park, S.; et al. Prone positioning before extracorporeal membrane oxygenation for severe acute respiratory distress syndrome: A retrospective multicenter study. Med. Intensiva 2018, 43, 402–409. [Google Scholar] [CrossRef]
- Guérin, C.; Albert, R.K.; Beitler, J.; Gattinoni, L.; Jaber, S.; Marini, J.J.; Munshi, L.; Papazian, L.; Pesenti, A.; Vieillard-Baron, A.; et al. Prone position in ARDS patients: Why, when, how and for whom. Intensive Care Med. 2020, 46, 2385–2396. [Google Scholar] [CrossRef] [PubMed]
- Weiss, T.T.; Cerda, F.; Scott, J.B.; Kaur, R.; Sungurlu, S.; Mirza, S.H.; Alolaiwat, A.A.; Kaur, R.; Augustynovich, A.E.; Li, J. Prone positioning for patients intubated for severe acute respiratory distress síndrome (ARDS) secondary to COVID-19: A retrospective observational cohort study. Br. J. Anaesth. 2020, 126, 48–55. [Google Scholar] [CrossRef]
- Peko, L.; Barakat-Johnson, M.; Gefen, A. Protenting pone positioned patients from facial pressure lceres using prophylactic dressing: A timely biomechanical análisis in the contexto of the COVID-19 pandemic. Int. Would J. 2020, 17, 1595–1606. [Google Scholar] [CrossRef]
- Ibarra, G.; Rivera, A.; Fernandez-Ibarburu, B.; Lorca-García Gacia-Ruano, A. Prone position pressure sores in the COVID-19 pandemic: The Madrid experience. J. Plast. Reconstr. Aesthetic Surg. 2020, 79, 2141–2148. [Google Scholar]
- Martel, T.; Orgill, D.P. Medical Device- Related Pressure Injuries During the COVID-19 Pandemic. J. Wound Cont. Nurse 2020, 47, 430–434. [Google Scholar] [CrossRef]
- Perrillat, A.; Foletti, J.M.; Lacagne, A.S.; Guyot, L.; Graillon, N. Facial pressure ulcers in COVID-19 patients undergoing prone positioning: How to prevent an underestimated epidemic. J. Stomatol. Oral Maxillofac. Surg. 2020, 121, 442–444. [Google Scholar] [CrossRef] [PubMed]
- Sleiwah, A.; Nair, G.; Mughal, M.; Lancaster, K.; Ahmad, I. Perioral pressure ulcers in patients with COVID-19 requiring invasive mechanical ventilation. Eur. J. Plast. Surg. 2020, 15, 1–6. [Google Scholar] [CrossRef]
- Singh, C.; Tay, J.; Shoqirat, N. Skin and Mucosal Damage in Patients Diagnosed With COVID-19. J Wound Ostomy Cont. Nurs 2020, 47, 425–438. [Google Scholar] [CrossRef]
- Carrillo, R.; Mejía, L.; Monares, E.; Chavarría, U.; Díaz, A.; Ayala, M.; Zamora, S.; Sánchez, J.S.; Lomelí, M.; Briones, J.C.; et al. Hemodynamic and mechanical ventilation approach in patients with COVID-19. Cir. y Ciruj. 2020, 88, 805–817. [Google Scholar]
- Concha, P.; Treso-Geira, M.; Esteve-Sala, C. Invasive mechanical ventilation and prolonged prone position during the COVID-19 pandemic. Med. Int. 2020, 65, 221–226. [Google Scholar]
- Chen, Y.; Zhang, J.; Feng, H.; Wan, F.; Zhang, Y.; Tan, L. Prone positioning in intubated and mechanically ventilated patients with SARS-CoV-2. J. Clin. Anest. 2021, 10, 1–9. [Google Scholar]
- Coppo, A.; Bellani, G.; Winterton, D.; Di Pierro, M.; Soria, A.; Faverio, P.; Cairo, M.; Mori, S.; Messinesi, G.; Contro, E.; et al. Feasibility and physiological effects of prone positioning in non-intubated patients with acute respiratory failure due to COVID-19 (PRON-COVID): A prospective cohort study. Lancet Respir. Med. 2020, 8, 765–774. [Google Scholar] [CrossRef]
- Pierucci, P.; Ambrosino, N.; Di Lecce, V.; Dimitri, M.; Battaglia, S.; Boniello, E.; Portacci, A.; Resta, O.; Carpagnano, G.E. Prolonged Active Prone Positioning in Spontaneously Breathing Non-intubated Patients With COVID-19-Associated Hypoxemic Acute Respiratory Failure With PaO2/FiO2 >150. Front. Med. 2021, 8, 626321. [Google Scholar] [CrossRef] [PubMed]
- Bastoni, D.; Poggiali, E.; Vercelli, A.; Demichele, E.; Tinelli, V.; Iannicelli, T.; Magnacavallo, A. Prone positioning in patients treated with non-invasive ventilation for COVID-19 pneumonia in an Italian emergency department. Emerg. Med. J. 2020, 37, 565–566. [Google Scholar] [CrossRef]
- Qadri, S.K.; Ng, P.; Toh, T.S.W.; Loh, S.W.; Tan, H.L.; Lin, C.B.; Fan, E.; Lee, J.H. Critically Ill Patients with COVID-19: A Narrative Review on Prone Position. Pulm. Ther. 2020, 6, 233–246. [Google Scholar] [CrossRef]
- Langer, T.; Brioni, M.; Guzzardella, A.; Carlesso, E.; Cabrini, L.; Castelli, G.; Dalla Corte, F.; De Robertis, E.; Favarato, M.; Forastieri, A.; et al. Prone position in intubated, mechanically ventilated patients with COVID-19: A multi-centric study of more than 1000 patients. Crit. Care 2021, 25, 128. [Google Scholar] [CrossRef]
- Vollenberg, R.; Matern, P.; Nowacki, T.; Fuhrmann, V.; Padberg, J.S.; Ochs, K.; Schütte-Nütgen, K.; Strauß, M.; Schmidt, H.; Tepasse, P.R. Prone Position in Mechanically Ventilated COVID-19 Patients: A Multicenter Study. J. Clin. Med. 2021, 10, 1046. [Google Scholar] [CrossRef]
- Lucchini, A.; Bambi, S.; Mattiussi, E.; Elli, S.; Villa, L.; Bondi, H.; Rona, R.; Fumagalli, R.; Foti, G. Prone Position in Acute Respiratory Distress Syndrome Patients: A Retrospective Analysis of Complications. Dimens. Crit. Care Nurs. 2020, 39, 39–46. [Google Scholar] [CrossRef]
- Gleissman, H.; Forsgren, A.; Andersson, E.; Lindqvist, E.; Lipka Falck, A.; Cronhjort, M.; Dahlberg, M.; Günther, M. Prone positioning in mechanically ventilated patients with severe acute respiratory distress syndrome and coronavirus disease 2019. Acta Anaesthesiol. Scand. 2021, 65, 360–363. [Google Scholar] [CrossRef]
- Shelhamer, M.C.; Wesson, P.D.; Solari, I.L.; Jensen, D.L.; Steele, W.A.; Dimitrov, V.G.; Kelly, J.D.; Aziz, S.; Gutierrez, V.P.; Vittinghoff, E.; et al. Prone Positioning in Moderate to Severe Acute Respiratory Distress Syndrome Due to COVID-19: A Cohort Study and Analysis of Physiology. J. Intensive Care Med. 2021, 36, 241–252. [Google Scholar] [CrossRef] [PubMed]
- Binda, F.; Marelli, F.; Galazzi, A.; Pascuzzo, R.; Adamini, I.; Laquintana, D. Nursing Management of Prone Positioning in Patients With COVID-19. Crit. Care Nurse 2021, 41, 27–35. [Google Scholar] [CrossRef] [PubMed]
- Ng, J.A.; Miccile, L.A.; Iracheta, C.; Berndt, C.; Detwiller, M.; Yuse, C.; Tolland, J. Prone Positioning of Patients With Acute Respiratory Distress Syndrome Related to COVID-19: A Rehabilitation-Based Prone Team. Phys. Ther. 2020, 100, 1737–1745. [Google Scholar] [CrossRef] [PubMed]
- Araújo, M.S.; Santos, M.M.P.D.; Silva, C.J.A.; Menezes, R.M.P.; Feijão, A.R.; Medeiros, S.M. Prone positioning as an emerging tool in the care provided to patients infected with COVID-19: A scoping review. Rev. Lat. Am. Enfermagem. 2021, 29, e3397. [Google Scholar] [CrossRef] [PubMed]
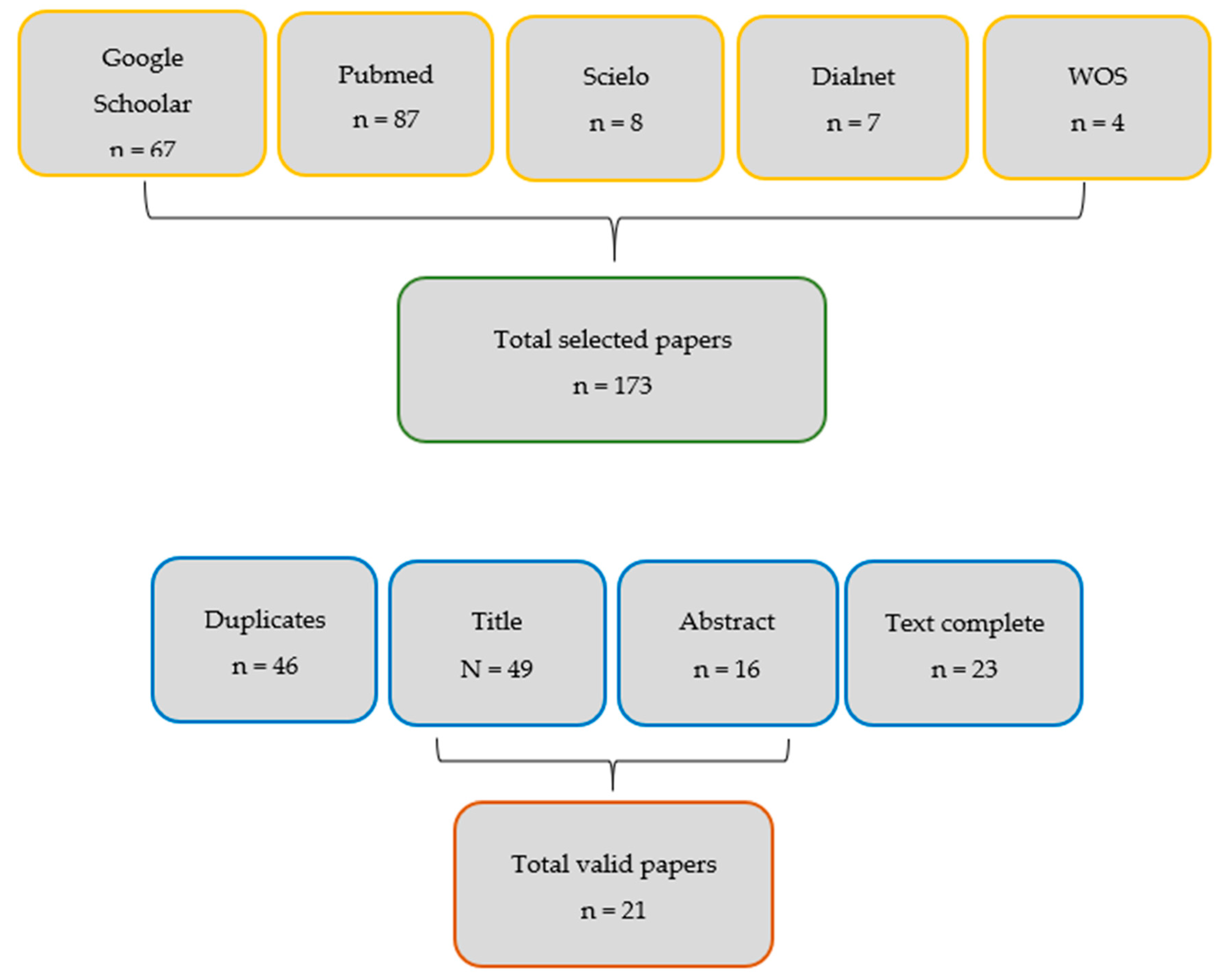
| Item Criteria | Google Scholar | Medline/ Pubmed | Scielo | Dialnet | WOS | Total |
| Identified | 67 | 87 | 8 | 7 | 4 | 173 |
| Duplicates | 17 | 23 | 4 | 4 | 1 | 46 |
| Title | 19 | 22 | 5 | 2 | 1 | 49 |
| Abstract | 4 | 9 | 1 | 1 | 1 | 16 |
| Text complete | 6 | 12 | 3 | 1 | 1 | 23 |
| Valid | 6 | 12 | 2 | 1 | 1 | 21 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Astasio-Picado, Á.; Sánchez-Sánchez, M.d.R. Effectiveness of Prone Positioning in Patients with COVID-19-Related Acute Respiratory Distress Syndrome Undergoing Invasive Mechanical Ventilation. Appl. Sci. 2021, 11, 10263. https://doi.org/10.3390/app112110263
Astasio-Picado Á, Sánchez-Sánchez MdR. Effectiveness of Prone Positioning in Patients with COVID-19-Related Acute Respiratory Distress Syndrome Undergoing Invasive Mechanical Ventilation. Applied Sciences. 2021; 11(21):10263. https://doi.org/10.3390/app112110263
Chicago/Turabian StyleAstasio-Picado, Álvaro, and María del Rocío Sánchez-Sánchez. 2021. "Effectiveness of Prone Positioning in Patients with COVID-19-Related Acute Respiratory Distress Syndrome Undergoing Invasive Mechanical Ventilation" Applied Sciences 11, no. 21: 10263. https://doi.org/10.3390/app112110263
APA StyleAstasio-Picado, Á., & Sánchez-Sánchez, M. d. R. (2021). Effectiveness of Prone Positioning in Patients with COVID-19-Related Acute Respiratory Distress Syndrome Undergoing Invasive Mechanical Ventilation. Applied Sciences, 11(21), 10263. https://doi.org/10.3390/app112110263







