1. Introduction
The lumbar extensor muscles, specifically the lumbar paraspinal muscles, comprise two main groups: the transversospinalis group, including the multifidus muscle, and more laterally, the erector spinae muscles, which consist of the longissimus and iliocostalis muscles [
1,
2]. Trunk stability is maintained by the deep spinal (core) stabilization system, including the lumbar paraspinal muscles, diaphragm, abdominal muscles, and pelvic floor. The lumbar extensor muscular system, more precisely the lumbar multifidus muscle and the erector spinae muscle, plays an essential role in stabilizing the lumbar spine and initiating and controlling all movements in the lumbar vertebral column [
3,
4]. By controlling these movements, the lumbar extensors also stabilize and protect the underlying osteoligamentous spinal structures from potentially harmful stresses that might otherwise be experienced as a result of movements made beyond their optimal functional range and/or over protracted periods [
5]. There is evidence of an association between decreased strength, muscular endurance, atrophy, and excessive fatigability of the lumbar extensors, and chronic non-specific low back pain [
6,
7,
8,
9,
10,
11,
12]. Prospective studies also suggest lumbar extensor deconditioning may be a common risk factor predicting acute low back injury and low back pain (LBP) [
11,
12].
A gold standard for appropriate quantitative methods of evaluating trunk function (defined as trunk or core stability, including the coordination, strength, and muscular endurance of trunk muscles) has yet to be determined [
13,
14]. However, such an exhaustive assessment appears to be important not only in patients with LBP, but also in patients with certain neuromuscular diseases (NMDs) in which the axial musculature is affected (e.g., axial myopathies, amyotrophic lateral sclerosis, spinal muscular atrophy) [
15]. A comprehensive evaluation of trunk function may well be of value in following the patterns of disease progression over time, assisting in selecting appropriate rehabilitation techniques and exercises, and in monitoring the effects of treatment.
Many fields and laboratory protocols have been employed to assess trunk muscle strength and muscular endurance in sports, fitness, clinical, and research settings [
16]. Isokinetic dynamometry has been widely used to measure trunk-muscle strength in light of its high validity, reliability, and capacity to measure different muscle groups while controlling contraction type, angular velocity, range of motion, body position, and the number of repetitions and sets [
16]. However, high costs, the need for considerable user expertise, and protracted testing time together constitute drawbacks of this approach [
17]. In contrast, field tests are easy to perform, do not require extensive and expensive equipment, and allow large numbers of people to be evaluated in a short period [
16]. Recently, the use of a hand-held dynamometer (HHD) has been described in the literature for the assessment of lower back extensor strength. This alternative method appears to have great potential, and is quick, inexpensive, and reliable [
15,
17,
18]. However, using an HHD to assess isometric lower back extensor strength has not yet been standardized.
This study aimed to create a battery of simple tests that would examine trunk function (strength and muscular endurance) comprehensively, with a special focus on lumbar extensor muscles, to unify the methodology of the tests selected, to confirm the reliability and validity of dynamometric protocols, and to monitor differences in performance between sex and age subgroups in healthy volunteers without chronic LBP in current socioeconomic conditions.
4. Discussion
This study has defined a battery of simple tests that are easy to perform in everyday practice and provide a comprehensive overview of essential components of trunk function (strength and muscular endurance). Strength-testing procedures included measurement of isometric lower back extensor strength using HHD and measurement of respiratory muscle strength. Muscular endurance of the trunk muscles was evaluated by the Biering-Sørensen, prone-plank, and side-bridge tests.
Isokinetic dynamometry is often referred to as the “gold standard” for the measurement of trunk muscle strength [
12,
15,
16,
18]. A certain number of studies have already been devoted to finding an alternative, practical, cheaper, and more user-friendly clinical tool that might provide reliable information about back extensor strength using HHD. Similar to the current study, the above studies established excellent validity and reliability for the new method [
17,
18,
19]. The present study confirmed the repeatability and the short-term and long-term test-retest reliability of techniques measuring maximal isometric lower back extensor strength by HHD as excellent in all three positions. Unifying the methodology of the three existing protocols [
17,
18,
19] and proving the repeatability of measurements using one dynamometer device allows us to compare obtained data measured in different postural positions and to discuss which of the positions is the most reasonable to use in terms of the biomechanics of the motion and in terms of usefulness in everyday practice.
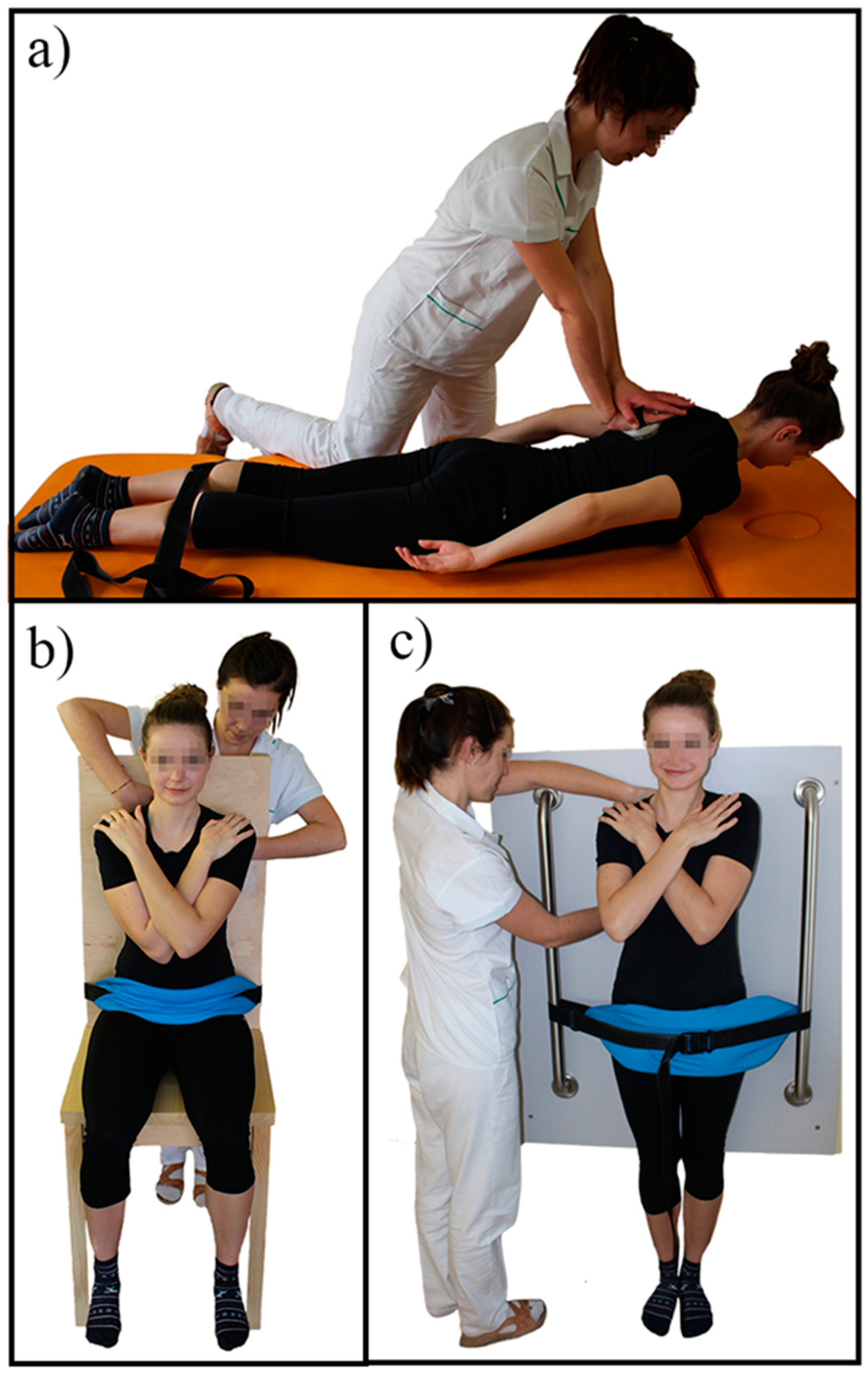
The highest values of isometric lower back extensor strength were measured in the sitting position, followed by those measured standing, while the lowest values were measured in the prone position. No other studies have compared lower back extensor strength in different postural positions. Some studies have suggested that it is reasonable to use pelvic fixation [
12] and, at the same time, a semi-sitting position with a hip flexion angle of 40–60°, since this position appears to increase the specificity of back extensor action (contraction) and reduce hip extensor activity [
12,
23]. In sitting and standing positions, this study employed pelvic fixation to specify the movement of the back extensor muscles, as suggested above [
17,
18,
23]. However, the current study did not reach the semi-sitting position (40–60°); it prioritized simplicity, requiring less time- and space-consuming procedures; creating a chair that could achieve the necessary angles for every subject would have added to study difficulty.
On the other hand, the chair deployed herein provided similar circumstances for all patients and measurements. The contraction of lumbar extensors in this position still appeared to be the strongest out of all three positions. The anchor rails required for measurements in the standing position are even cheaper than the specially designed chair and less space-consuming. However, they are not easy to move, so the measures always need to be taken in the same room. The technique for the prone position requires no special equipment (except the HHD itself).
While using an HHD, it may be difficult for the assessor to provide a counter-pressure that corresponds to the effort exerted by the patient, especially when measuring larger muscle groups [
24]. This raises a question regarding the assessment of isometric lower back extensor strength using an HHD in the prone position, as the maximal strength of the examiner may limit it, and a ceiling effect may occur when testing strong individuals [
15,
19,
20]. Valentine et al. suggest an alternative technique for prone position measurement, using a tripod fixed by a non-elastic belt to the table and the patient. The portable dynamometer is held between these [
19]. External fixation can reduce measurement errors compared to assessments in which the assessor fixes the HHD manually. The Valentine et al. study results showed that, when using an HHD to assess lower back extensor strength, an HHD fixed with a tripod was superior to one that was manually set [
19].
On the other hand, an ICC of ≥0.90 is required for clinical application to ensure valid interpretation of any findings [
25]; this study achieved this figure from the prone position without using tripod fixation. However, it must be borne in mind that movement in the prone position alone does not comply with the biomechanics of everyday life for most people. It may be anticipated that this movement could lead to discomfort in patients with low back pain and older people. Some of the studies even point out that several of their patients, those with hyperkyphosis due to osteoporotic fractures, were unable to perform the task [
19].
The outcomes herein indicated that isometric lower back extensor strength in the prone position was mainly dependent on age (decreasing with advancing age). However, the isometric back extensor strength in sitting and standing positions seemed to be dependent not only on age, but predominantly on sex and weight; in the study population, weight was related to sex (data are not displayed); however, it can be assumed that the same pattern may also be seen in other populations of volunteers/patients. This finding accords with observations made by other authors [
16], in which males exhibited higher extensor strength than females. Some authors explain this finding in terms of more excellent anthropometric dimensions and more elevated experience of maximum effort in men, which may allow them to achieve higher forces [
16,
26]. Mannion et al. posit that absolute muscle strength is determined by the quantity of force-generating elements and their geometry, so the strength of a muscle is mainly determined by its overall cross-sectional area [
4]. The difference in maximum strength between the sexes may thus be simply associated with the gross muscle-size differences between men and women, a factor present in almost all skeletal muscles.
The current study disclosed a robust and significant correlation between strength-testing results using HHD from the sitting and standing positions. Respiratory muscle strength proved a significant moderate correlation with isometric back extensor strength in sitting and standing positions, which could confirm validity for the technique measuring the lower back extensor muscle strength in sitting and standing positions using HHD. However, outcomes obtained from the prone position did not correlate strongly with those obtained from the other two positions. This did not hold for the technique performed in the prone position since the results did not correlate with respiratory muscle strength at all. These findings suggest to other working groups, who aim to assess lower back extensor strength using HHD in their practice, that one of the positions may be chosen to assess lower back extensor strength, preferably in a sitting or standing position, depending on the availability of equipment. In further works, the authors aim to use all these tests to observe the performance of patients with LBP and NMD; how do these results correlate and how do they differ from healthy volunteers. Only then will it be possible to exclude tests that seem to be redundant for clinical practice.
Respiratory muscles are an essential component of the core system. The strong correlation between maximal inspiratory pressure and maximal expiratory pressure that appeared in the results herein may support the validity of the techniques chosen for measuring respiratory muscle strength. In this study group, even though the volunteers tested were healthy, the overall strength of respiratory muscles in different subgroups did not exceed 100% of the predicted value. This may arise from the strict norms chosen, as they respect sex and age and find widespread application in this specialty [
27]. In light of the fact that even asymptomatic people fail to reach predicted values, Caruso et al. presented a study that employed lower limits for the norms of respiratory muscle-strength tests: MIP 60 cmH
2O in women and 80 cmH
2O in men and MEP 120 cmH
2O and 150 cmH
2O in women and men, respectively [
28]. All the study subgroups herein achieved their mean value for the lower limit of normal strength, except the subgroup of the youngest women, who achieved MEP values closely under this limit. It appears necessary to evaluate respiratory muscle strength since few studies point out possible discrepancies between the strength of the respiratory muscles and lumbar extensor muscles in patients with chronic LBP and patients with neuromuscular diseases [
6,
29,
30,
31].
The muscular endurance of the back extensor muscles was assessed herein by including the Biering-Sørensen test into the battery. This examination is widely accepted as a good assessment tool and predictor of non-specific low back pain [
32,
33]. The validity and repeatability of the test have been demonstrated in many studies [
33,
34,
35]. The test examines the muscular endurance of all muscles involved in trunk extension, thus the paraspinal muscles (most notably the multifidus muscles) but also the hip extensors [
33]. However, in the study baseline examination, the neurologist performed a manual muscle test of the lower extremities in all participants to ensure that no weakness was present and that the testing results would not be affected by potential weakness of the hip extensors.
In the group observed herein, a significant difference between the time of effort in men and women appeared in the Biering-Sørensen test. Women were able to hold the position for a longer time than men, which confirms the findings of other authors [
32,
33]. Mannion et al. explain the difference between the performances of the sexes in terms of the pronounced differences in the size ratios of the fiber types in the thoracic and lumbar regions of the erector spinae between them [
4]. A significantly more extensive area of the muscle occupied by type 1 fibers (slow twitch) is found in the erector spinae of women. It seems that the greater the relative area of the muscles occupied by type 1 fibers, the longer the contraction can be sustained. In the groups observed herein, time of effort was lowest in volunteers under 30 years of age. The potential influence of age is not evident [
33]. Some studies have taken the role of age into account, suggesting that back muscular endurance capacity may increase slightly with age [
36,
37]; others have contradicted this [
32]. However, the study group herein was too small to conclude the matter.
Other trunk muscular endurance tests, the prone-plank test and side-bridge tests on both sides, were included in the study herein because the endurance imbalances between trunk muscle groups may also be related to low back disorders [
38]. The prone-plank test has frequently been used in clinical settings to evaluate core stability, specifically abdominal core muscular endurance [
14,
39,
40,
41]. It is often regarded as the trunk flexor endurance test since the internal oblique, external oblique, and transverse abdominis muscles are largely activated during the procedure [
13,
42]. The side-bridge test is also an assessment that challenges core muscles, especially the lateral stabilizers [
14,
43]. These positions are also widely used as core stabilization exercise tools [
38,
42,
44,
45]. All the muscular endurance tests above have confirmed their validity and reliability in populations of athletes and healthy volunteers in previous studies [
41,
43,
46]. They have been used in patients with LBP to assess trunk function [
40,
42,
47].
In contrast to the results of the Biering-Sørensen test, the prone-plank test in this study revealed no significant differences in time of effort among either age groups or the sexes. However, more effort was observed in men than in women, although they did not achieve statistical significance. Comparing the results herein with those of a study targeted on norms for the prone plank-test [
48]. The study data were more similar to the athletic part of the previously studied population. This fact might well be explained by the high familiarity of the exercise position (prone-plank position) in socioeconomic relationships. In contrast to the Biering-Sørensen test, where none of the volunteers had ever seen or tried the position, the prone-plank exercise was widely known, and only two of the volunteers had never seen or tried it before.
Outcomes obtained in the side-bridge test showed a robust correlation between right and left sides, so it might be suggested that the test be performed on only one side. No difference in outcomes of this test appeared between the sexes in the current study. However, significant differences between age groups were observed for the right side only, a trend that may arise out of the cohort being relatively small. Evans et al., who tested a group of young athletes using the side-bridge test, found performances differed between the sexes on both sides [
46]. However, a significant difference in muscular endurance performance between sex and age groups in some muscle groups but not others implies that trunk muscular endurance should be tested comprehensively. The side-bridge test should be performed on both sides [
46].
The outcomes of the two trunk muscular endurance tests, the Biering-Sørensen and prone-plank tests, correlated, albeit only moderately. Most importantly, this study revealed a different distribution model of outcomes between age groups and the sexes in these two tests. The correlation between the side-bridge test and the prone-plank test was again moderate. It appears that all of these tests are predictive of core muscular endurance, but it is apparent that each test examines different muscle co-activations, determined by the postural situation. It therefore appears reasonable to include all three trunk muscular endurance examinations in the final test battery.
The correlation between strength-testing procedures and trunk muscular endurance tests was weak or absent. This finding suggests that there might be discrepancies between absolute strength and muscular endurance of trunk muscles even in asymptomatic people; both of these aspects should therefore be observed. Both isometric lower back extensor strength and trunk muscular endurance tests should be included in the final test battery.
In the study group herein, outcomes for strength and muscular endurance tests were not dependent on participants’ general physical activity levels. The findings of specific authors suggest that the level of general physical activity does not predict or initiate LBP; however, well-chosen measures may reveal deconditioning of certain muscle groups associated with LBP [
12]. It remains crucial to monitor the activeness of patients, as specialists in the field constantly address this issue.
In further studies, the authors of the current contribution intend to deploy this battery of tests as a whole in patients with low back pain and neuromuscular diseases to verify whether any of these outcome measures are able to recognize altered trunk muscle function and trunk muscle imbalance in such disorders. However, while using these tests in different groups of patients, the possibility of pain elicited throughout the testing procedures must be recorded and taken into account while interpreting the results. We anticipate that these tests will be helpful in clinical practice. They have the potential to capture changes in outcomes concerning disease progression or interventions, such as rehabilitation programs aiming for improvement in the strength and muscular endurance of the lumbar extensor muscles and/or core muscles. However, as mentioned above, further studies need to be conducted to prove these assumptions.
Limitations of the Study
The current study has its limitations. Firstly, only 60 volunteers were enrolled, so individual age sub-groups could not consist of more than 15 people. Normative data for each test were therefore impossible to achieve. However, the study provides an overview of the trunk muscle strengths and muscular endurance performances that might be expected in the healthy population’s various age and sex groups in the socioeconomic background. Secondly, all participants were hospital employees, so this was not a heterogeneous group of people according to education, as 80% of volunteers had graduated from university.
On the other hand, heterogeneity existed in terms of the nature of their work (sedentary/manual). Thirdly, only intra-rater reliability of strength testing procedures using HHD was established, as there was only one experienced examiner available for this study. Therefore, one should be aware of the possibility of a “ceiling effect” that may occur in powerful individuals when isometric lower back extensor strength is measured using an HHD in the prone position. Another limitation of the study is that we did not record pain throughout the assessment. This might be because exclusion criteria were defined as existing acute and chronic low back pain. It needs to be pointed out that all volunteers were highly motivated to participate in the study and did not complain concerning any pain throughout the assessments. While there is a possibility that pain elicited during the test may interfere with measurements, especially in patients with low back pain, this needs to be recorded, taken into account, and considered in the interpretation of the results. Further studies could include pain-detecting protocols and questionnaires at the enrollment and during the procedures to record whether any tests trigger pain.