New Training Approach for Improving the Spatial Perception and Orientation Ability of Dentistry Students
Abstract
1. Introduction
2. Materials and Methods
Study Population
3. Protocols
3.1. Grooved Pegboard Test
3.2. Innovative Portable Training Tool: PhantHome
3.3. Study Procedure
3.4. Statistics
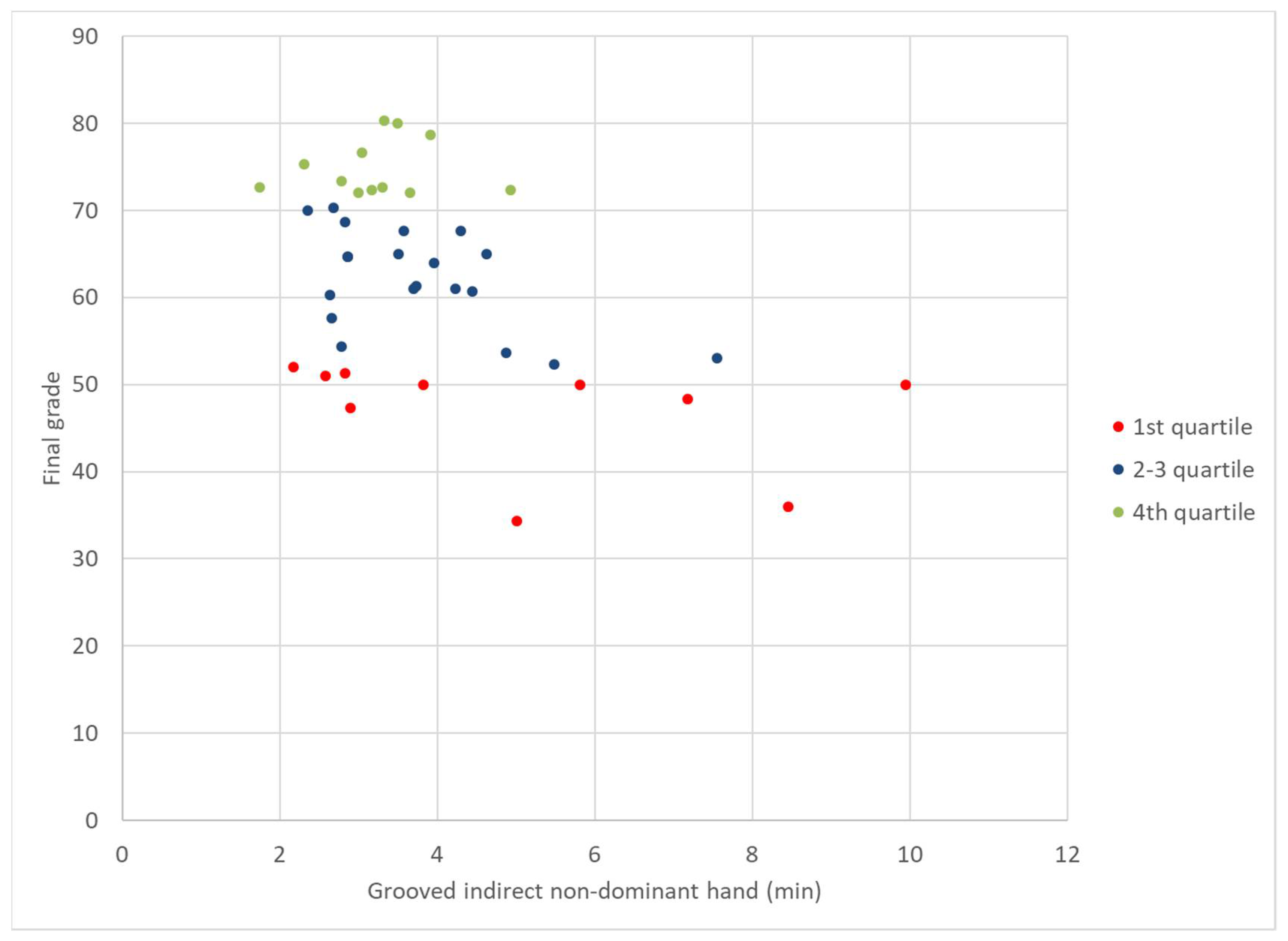
4. Results
5. Discussion
6. Conclusions
- The ability for orientation and spatial perception required in a prosthodontics course is governed by a combination of acquired ability that improves significantly after training and innate ability.
- There is a positive transfer in learning: PhantHome training led to improved performance on the Grooved tests without further training on these tests. Therefore, training in the PhantHome tool can significantly improve performance in the prosthodontics phantom course.
- A Prediction model was found using the scores of the various motor tests at T0, which predicted success in a prosthodontics course with 86% accuracy.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Abbreviations | Meaning |
| Pegboard_Direct_Dominant Hand | Performing the Grooved Pegboard test by direct vision using dominant hand |
| Grooved Pegboard | Performing the Grooved Pegboard test by direct vision using non-dominant hand |
| _Direct_Non Dominant Hand | |
| Grooved Pegboard | Performing the Grooved Pegboard test by indirect vision using dominant hand |
| indirect dominant hand | |
| Grooved Pegboard | Performing the Grooved Pegboard test by indirect vision using non-dominant hand |
| indirect Non dominant hand | |
| FPD | Fixed partial denture |
| Final.Phantom | The final phantom grade |
| PhantHome_Direct | Performing the PhantHome test in direct vision |
| PhantHome_Indirect | Performing the PhantHome test in indirect vision |
References
- Luck, O.; Reitemeier, B.; Scheuch, K. Testing of fine motor skills in dental students. Eur. J. Dental Educ. 2000, 4, 10–14. [Google Scholar] [CrossRef]
- Suddick, R.P.; Yancey, J.M.; Wilson, S. Mirror-tracing and Embedded Figures tests as predictors of dental students’ performance. J. Dental Educ. 1983, 47, 149–154. [Google Scholar] [CrossRef] [PubMed]
- Shillingburg, H.T. Fundamentals of Fixed Prosthodontics, Textbook, 4th ed.; Quintessence Publishing: Berlin, Germany, 2012; p. 131. [Google Scholar]
- Potts, R.G.; Shililingburg, H.T.; Ducanson, M.G. Retention and resistance of preparation for cast restoration. J. Prosthet. Dent. 1980, 43, 303–308. [Google Scholar] [CrossRef]
- Schwartz, I.S. A review of methods and techniques to improve the fit of cast restorations. J. Prosthet. Dent. 1986, 56, 279–283. [Google Scholar] [CrossRef]
- Kaufman, E.G.; Coelho, D.H.; Colin, L. Factors influencing the retention of cemented gold casting. J. Prosthet. Dent. 1961, 11, 487. [Google Scholar] [CrossRef]
- Jorgensen, K.D. The relationship between retention and convergence angle in cemented veneer crowns. Acta Odontol. Scand. 1955, 13, 35–40. [Google Scholar]
- Weed, R.M.; Suddick, R.P.; Kleffner, J.H. Taper of clinical and typodonts crown prepared by dental students. J. Dental Res. 1984, 63, 286. [Google Scholar]
- Noonan, J.E., Jr.; Goldfogel, M.H. Converge of the axial walls of full veneer crown preparation in dental school environment. J. Prosthet. Dent. 1991, 66, 706–708. [Google Scholar] [CrossRef]
- Callan, R.S.; Palladino, C.L.; Furness, A.R.; Bundy, E.L.; Ange, B.L. Effectiveness and feasibility of utilizing E4D technology as a teaching tool in a preclinical dental education environment. J. Dental Educ. 2014, 78, 1416–1423. [Google Scholar] [CrossRef]
- Callan, R.S.; Blalock, J.S.; Cooper, J.R.; Coleman, J.F.; Looney, S.W. Reliability of CAD/CAM technology in assessing crown preparations in a preclinical dental school environment. J. Dental Educ. 2014, 78, 40–50. [Google Scholar] [CrossRef]
- Carly, F.; Justin, M.; Yasushi, T.; Raina, C.; Lisa, L.; Cliff, L.; John, D.; Shigemi, I.N. Dental Students’ perceptions of digital assessment software for preclinical tooth preparation exercises. J. Dental Educ. 2016, 81, 597–603. [Google Scholar]
- Ben Gal, G.; Weiss, E.I.; Gafni, N.; Ziv, A. Preliminary assessment of faculty and student perception of a haptic virtual reality simulator for training dental manual dexterity. J. Dental Educ. 2011, 75, 496–504. [Google Scholar]
- Jasinevicius, T.R.; Landers, M.; Nelson, S.; Urbankova, A. An evaluation of two dental simulation systems: Virtual reality versus contemporary non-computer assisted. J. Dental Educ. 2004, 68, 1151–1162. [Google Scholar] [CrossRef]
- Gottlieb, R.; Lanning, S.K.; Gunsolley, J.C.; Buchanan, J.A. Faculty impressions of dental students’ performance with and without virtual reality simulation. J. Dental Educ. 2011, 75, 1443–1451. [Google Scholar] [CrossRef]
- Thorndike, E.L. The effect of practice in the case of purely intellectual function. Am. J. Psychiatr. 1908, 19, 374–384. [Google Scholar] [CrossRef]
- Neuman, L.M. A simple exercise for teaching mirror vision skills. J. Dental Educ. 1988, 52, 170–172. [Google Scholar] [CrossRef]
- Gunter, M.R.; Anne, K. Training device for dental students to practice mirror- inverted movement. J. Dental Educ. 2011, 75, 1280–1284. [Google Scholar]
- Bohnen, N.I.; Kuwabara, H.; Constantine, G.M.; Mathis, C.A.; Moore, R.Y. Grooved Pegboard Test as a biomarker of nigrostriatal denervation in Parkinson’s disease. Neurosci. Lett. 2007, 424, 185–189. [Google Scholar] [CrossRef]
- Bryden, P.J.; Roy, E.A. A new method of administering the Grooved Pegboard Test: Performance as a function of handedness and sex. Brain Cogn. 2005, 58, 258–268. [Google Scholar] [CrossRef] [PubMed]
- Strenge, H.; Niederberger, U. Unidirectional interference in use of nondominant hand during concurrent Grooved Pegboard and random number genera-tion tasks. Percept. Mot. Skills 2008, 106, 763–774. [Google Scholar] [CrossRef] [PubMed]
- Kao, E.; Ngan, P.; Wilson, S.; Kunovich, R. Wire-bending test as a predictor of preclinical performance by dental students. Percept. Mot. Skills 1990, 71, 667–673. [Google Scholar] [CrossRef]
- Kothe, C.; Hissbach, J.; Hampe, W. Prediction of practical performance in preclinical laboratory courses: The return of wire bending for admission of dental students in Hamburg. GMS Z. Med. Ausbild. 2014, 31, 22. [Google Scholar]
- Lugassy, D.; Levanon, Y.; Shpack, N.; Levartovsky, S.; Pilo, R.; Brosh, T. An interventional study for improving the manual dexterity of dentistry students. PLoS ONE 2019, 14, e0211639. [Google Scholar] [CrossRef] [PubMed]
- Osgood, C.E. The similarity paradox in human learning: A resolution. Psychol. Rev. 1949, 56, 132–143. [Google Scholar] [CrossRef] [PubMed]
- Muscio, B. Motor capacity with special reference to vocational guidance. Br. J. Psychol. Gen. Sect. 1922, 13, 157–184. [Google Scholar] [CrossRef]
- Oliver, E.C. A sensorimotor program for improving writing readiness skills in elementary age children. Am. J. Occup. Ther. 1989, 44, 111–115. [Google Scholar] [CrossRef][Green Version]
- Smith, J.C. Effects of occupational therapy services on fine motor and functional performance in preschool children. Am. J. Occup. Ther. 2000, 54, 372–380. [Google Scholar] [CrossRef][Green Version]
- Lugassy, D.; Levanon, Y.; Pilo, R.; Shely, A.; Rosen, G.; Meirowitch, A.; Brosh, T. Predicting the clinical performance of dental students with a manual dexterity test. PLoS ONE 2018, 13, e0193980. [Google Scholar] [CrossRef]
- Schwibbe, A.; Kothe, C.; Hampe, W.; Konradt, U. Acquisition of dental skills in preclinical technique course: Influence of spatial and manual abilities. Adv. Health Sci. Educ. 2016, 21, 841–857. [Google Scholar] [CrossRef]
- Willis, D.O.; Kincheloe, J.E. Teaching dental students mirror vision skills. J. Dental Educ. 1983, 47, 311–316. [Google Scholar] [CrossRef]
- Boyd, M.A.; Rucker, L.M. Effects of immediate introduction of indirect vision on performance and posture. J. Dental Educ. 1987, 51, 98–101. [Google Scholar] [CrossRef]
- McClure, A.R.; Roomian, T.C.; Eisen, S.E.; Kugel, G.; Amato, R.B. Jumpstart Mirror Trainer: A New Device for Teaching Mirror Skills to First-Year Dental Students. J. Dental Educ. 2019, 83, 1199–1204. [Google Scholar] [CrossRef]
- Gagne, R.M.; Foster, H. Transfer of training from practice on components in a motor skill. J. Exp. Psychol. 1949, 39, 47–68. [Google Scholar] [CrossRef]
- Bezdicek, O.; Nikolai, T.; Hoskovcova, M.; Stochl, J.; Brožová, H.; Dušek, P.; Zárubová, K.; Jech, R.; Růžička, E. Grooved pegboard predicates more of cognitive than motor involvement in parkinson’s disease. Assessment 2014, 21, 723–730. [Google Scholar] [CrossRef]
- Strenge, H.; Niederberger, U.; Seelhorst, U. Correlation between tests of attention and performance on grooved and Purdue pegboard in normal subjects. Percept. Mot. Skills 2002, 95, 507–514. [Google Scholar] [CrossRef]
- Spratley, M.H. Regression analysis of dexterity tests and dental students’ practical examination results. Aust. Dental J. 1992, 37, 461–466. [Google Scholar] [CrossRef] [PubMed]
- Stacey, D.G.; Whittaker, J.M. Predicting academic performance and clinical competency for international dental students: Seeking the most effective measures. J. Dental Educ. 2005, 69, 270–280. [Google Scholar] [CrossRef] [PubMed]
- Spratley, M.H. Aptitude testing and the selection of dental students. Aust. Dental J. 1990, 35, 159–168. [Google Scholar] [CrossRef]
- Kunovich, R.; Rachid, R.G. Mirror training in three dimensions for dental students. Percept. Mot. Skills 1992, 75, 923–928. [Google Scholar] [CrossRef] [PubMed]
- Nishida, M.; Sohmura, T.; Takahashi, J. Training in tooth preparation utilizing a support system. J. Oral Rehabil. 2004, 31, 149–154. [Google Scholar] [CrossRef] [PubMed]

| Motor Task | T0 | T1 | ||
|---|---|---|---|---|
| Mean (±SD) | [Range] (min) | Mean (±SD) | [Range] (min) | |
| Grooved Pegboard_Direct_Dominant Hand | 1 (±0.16) | [0.43–1.36] | 0.9 (±0.1) | [0.53–1.25] |
| Grooved Pegboard_Direct_Non Dominant Hand | 1.1 (±0.17) | [0.8–1.65] | 1 (0.18) | [0.75–1.6] |
| Grooved Pegboard_Indirect_Dominant Hand | 3.6 (±1.6) | [1.83–7.6] | 2.4 (±0.9) | [1.45–5.46] |
| Grooved Pegboard_Indirect_Non Dominant Hand | 3.9 (±1.7) | [1.7–9.9] | 2.9 (±1.1) | [1.46–7.18] |
| PhantHome_Direct | 2.6 (±2.3) | [0.6–13.8] | 1.6 (±0.88) | [0.68–5] |
| PhantHome_Indirect | 3.9 (±3) | [0.7–12.7] | 2.4 (±1.3) | [0.76–8.33] |
| Motor Task | Final Grade in Prosthodontics Course |
|---|---|
| Grooved Pegboard_Direct_Dominant hand | −0.290 p = 0.012 |
| Grooved Pegboard_Direct_Non-Dominant hand | −0.288 p = 0.013 |
| Grooved Pegboard t_Indirect_Dominant hand | −0.124 p = 0.274 |
| Grooved Pegboard t_Indirect_Non Dominanat hand | −0.316 p = 0.005 |
| PhantHome_Direct | −0.379 p = 0.019 |
| PhantHome_Indirect | −0.183 p = 0.107 |
| Observed | Predicted | ||
|---|---|---|---|
| Failed | Passed | Percentage of Predictability | |
| Failed | 10 | 4 | 71.4% |
| Passed | 1 | 23 | 95.8% |
| Overall percentage of prediction model readiness | 86.8% | ||
| Motor Task | B | Sig | Exp(B) | 95% C.I. for Exp(B) | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Grooved Pegboard Test_Direct_Dominant | −4.473 | 0.125 | 0.011 | 0.005 | 3.461 |
| Grooved Pegboard Test_Direct_Non-Dominant hand | −2.257 | 0.455 | 0.105 | 0.005 | 39.154 |
| Grooved Pegboard Test_Indirect_Non Dominanat | −0.652 | 0.044 | 0.521 | 0.267 | 0.983 |
| PhantHome_Direct hand | −0.515 | 0.05 | 0.598 | 0.357 | 1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shely, A.; Ben-Izhack, G.; Lugassy, D.; Matalon, S.; Pilo, R.; Brosh, T.; Dolev, E. New Training Approach for Improving the Spatial Perception and Orientation Ability of Dentistry Students. Appl. Sci. 2021, 11, 9387. https://doi.org/10.3390/app11209387
Shely A, Ben-Izhack G, Lugassy D, Matalon S, Pilo R, Brosh T, Dolev E. New Training Approach for Improving the Spatial Perception and Orientation Ability of Dentistry Students. Applied Sciences. 2021; 11(20):9387. https://doi.org/10.3390/app11209387
Chicago/Turabian StyleShely, Asaf, Gil Ben-Izhack, Diva Lugassy, Shlomo Matalon, Raphael Pilo, Tamar Brosh, and Eran Dolev. 2021. "New Training Approach for Improving the Spatial Perception and Orientation Ability of Dentistry Students" Applied Sciences 11, no. 20: 9387. https://doi.org/10.3390/app11209387
APA StyleShely, A., Ben-Izhack, G., Lugassy, D., Matalon, S., Pilo, R., Brosh, T., & Dolev, E. (2021). New Training Approach for Improving the Spatial Perception and Orientation Ability of Dentistry Students. Applied Sciences, 11(20), 9387. https://doi.org/10.3390/app11209387








