Abstract
This paper mainly examines the fixation performances of the cephalomedullary nail for the incidence of intertrochanteric (IT) fracture to guide the appropriate fixations with respect to the bone density in terms of a biomechanical perspective. It is substantially important to guide which types of fixation are applied during the operation since it tends to induce the backout or migration of the helical blade and screw according to weight and bone density. Biomedical polyurethane (PUR) foam blocks for simulating human bone are adopted with two grades of densities to simulate a normal person and an elderly person who has osteoporosis. Tensile and compression tests are conducted to analyze the tensile-compression anisotropy of PUR foams. Pull-out performances of screw and helical blades are evaluated from experimental perspectives, which are supported by comparison with the results of finite element method analysis. The clamping force of the screw is higher than the helical blade, about 177% in normal foam density and 198% in low foam density. After physical evaluation of the critical pull-out fixation force of screw and helical blade, we have suggested that stable fixation is guaranteed when the pull-out force is larger than projected force.
1. Introduction
The incidence of intertrochanteric (IT) fracture has been issued continuously with an increase of the elderly population [1,2,3,4], which tends to have a close relation to the mortality rate since it increases up to 30% within one year after IT fractures [5,6,7]. Extramedullary implant and cephalomedullary nail are commonly used for operative treatment against IT fracture [8]. Especially, cephalomedullary nail is a representative method that has been frequently utilized by surgeons in terms of biomechanical advantages [9,10,11].
Although both clinical and biomechanical studies suggested that cephalomedullary nail has a mechanical advantage over extramedullary implants, a high rate of complications or implant failure remains in elderly patients with osteoporosis [12,13,14].
There are two types of main implants, such as screw and helical blade [15,16] for adopting the cephalomedullary nail system, designed to allow sliding of a proximal fragment so that contact surface and stability of fracture site can be increased after fixation. However, it is possible for instability to occur in the cephalomedullary nail system due to excessive sliding when the gap between several fragmentations along the fracture surface is relatively large after fixation [17,18,19]. To minimize the gap at the fracture surface during the operation, intraoperative compression is additionally applied to the cephalomedullary nail by utilizing devices in the designed nail set [20]. In some clinical cases, however, a proximal fixation implant escapes out from the proximal fragment during the intraoperative compression procedure before the proper compression is achieved due to the osteoporotic bone quality.
Furthermore, even though the fixation is successfully conducted by utilizing the cephalomedullary nail system, there are several issues in nail migration with different types of loading conditions, such as walking and dynamic exercise, etc. S.Y. Lee et al. [21] reported traumatic complete back out of the helical blade of the PFNA-II in a healed IT fracture. L. Karapinar et al. [22] examined the blade migration over time, which resulted in fracture site collapse. N. Lasanianos et al. [23] emphasized that sufficient screw fixation to resist migration under dynamic loading is substantially important since it can be considered to be an evolutionary complication. Under these circumstances, it is essential to examine the pull-out performances of cephalomedullary nails with screw and helical blade types in terms of bone density.
To make a comparison of the pull-out performance of screw and helical blade in the cephalomedullary nail system, biomedical polyurethane (PUR) foam blocks to simulate the human bone with two grades of densities to represent the normal person (0.35 g/cm3) and elderly person who has osteoporosis (0.14 g/cm3) were prepared to carry out the tension, compression, and pull-out tests. Based on the biomechanical tests, material properties have been obtained to conduct FEM analysis, which demonstrates the failure mode as well as reaction force during the pull-out test, in detail.
2. Experimental Procedure
To represent human bone for comparative pull-out performances of cephalomedullary nail, biomedical PUR foam blocks produced by Synbone [24] with two grades of densities such as low density (0.14 g/cm3) and normal density (0.35 g/cm3) were prepared based on American Society for Testing and Materials (ASTM) F1938-08 [25], as shown in Figure 1, which consists of cancellous bone exhibiting closed-cell structure and cortical bone at the top of the block.
Figure 1.
Foam blocks (Synbone, Zizers) with different density of: (a) 0.14 g/cm3; (b) 0.35 g/cm3.
To obtain the tensile and compressive stress-strain curves of the PUR foams, the tensile and compression tests have been carried out three times, since they tend to show totally different material behavior in the tensile and compressive deformation modes with respect to the density of the porous material [26]. Figure 2 demonstrates the detailed dimension of test specimens for tensile, compressive, and pull-out tests based on the ASTM D 1623 and ASTM D 1621 standards, respectively. In the case of the tensile specimen, a pre-machined part from the PUR block as depicted in Figure 2a is attached to a cylindrical grip with a diameter of 34 mm by applying with the metal adhesive, which is set in the universal testing machine as shown in Figure 3a. The tensile tests are carried out with a head speed of 1mm/min to guarantee the quasi-static strain rate.
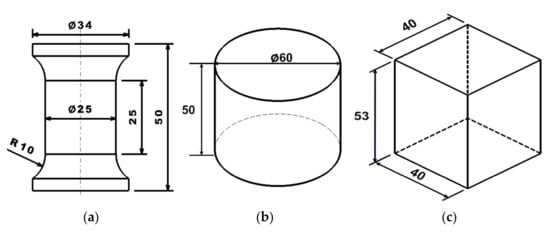
Figure 2.
Dimensions of test specimens for: (a) tensile test; (b) compressive test; (c) pull-out test.
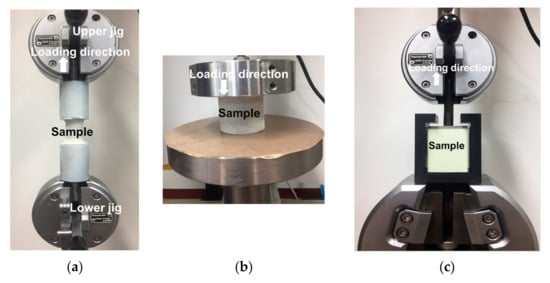
Figure 3.
Experimental set-up for: (a) tensile test; (b) compressive test; (c) pull-out test.
For the compressive test, a cylindrical specimen with a diameter of 60 mm and height of 50 mm is compressed by a flat punch with a speed of 5 mm/min, and a Teflon sheet is applied to minimize the frictional effects between the die-set and specimen.
In the pull-out test, a screw and helical blade are inserted, first, into a pre-machined parallelepiped block with dimensions of 40 × 40 × 53 (mm3), which is set in the specially designed fixture to conduct the pull-out test as shown in Figure 3c. The pre-installed screw or helical blade is pulled upward with the speed of 5 mm/min until the final failure occurs, and the pull-out load is measured to examine their pull-out performance. To visually evaluate the strain distribution of the specimen during the tensile and compression tests, the digital image correlation (DIC) technique is applied by utilizing the ARAMIS system [27].
3. Pull-Out Performance of Cephalomedullary Nail
3.1. Experimental Results
Figure 4 represents the experimental results of the tensile and compressive tests with respect to the densities of PUR foam. The compressive strength of the lower density specimen exhibits about 17% of the normal density specimen, as depicted in Figure 4b, while the tensile strength of the lower density specimen exhibits about 30%, as shown in Figure 4a.
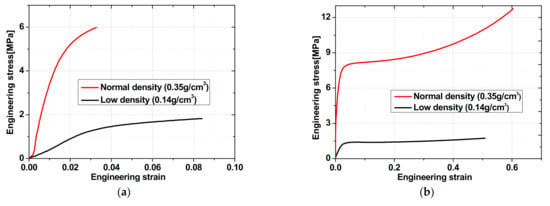
Figure 4.
Experimental stress-strain curves in: (a) tensile test; (b) compressive test.
Pull-out tests with helical blade and screw were conducted with respect to the PUR foam density for three repeated tests to guarantee reproducibility. Figure 5 compares the experimental reaction forces from the pull-out tests in which screw-type shows substantially higher reaction force than helical blade independent of the foam density. After the first peak occurs, the pull-out force rapidly decreases since the contact area between the screw or helical blade and the PUR foam decrease. Since there is a lot of debris observed in the screw thread after pull-out tests as depicted in Figure 6a,c, it is evaluated that the screw-type tends to induce severe damage to the PUR foam during the pull-out process even though it is able to guarantee sufficient clamping force. In terms of the peak loads in the pull-out test, the screw-type demonstrates higher clamping forces of 177 7% in the normal-density foam and 198 13% in the low-density foam, as seen in Figure 7.
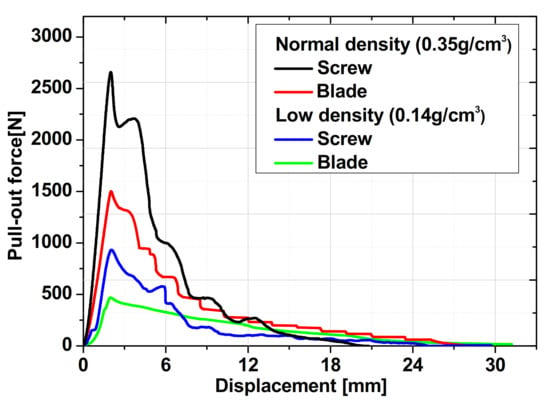
Figure 5.
Experimental results of pull-out test with screw and helical blade with respect to different foam densities.
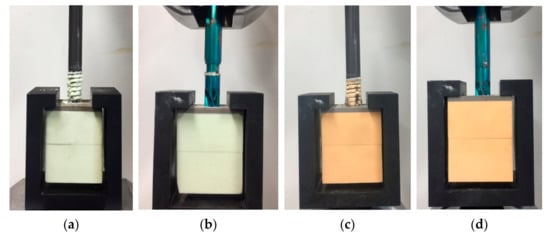
Figure 6.
Pull-out specimen at the final failure: (a) screw (0.14 g/cm3); (b) helical blade (0.14 g/cm3); (c) screw (0.35 g/cm3); (d) helical blade (0.35 g/cm3).
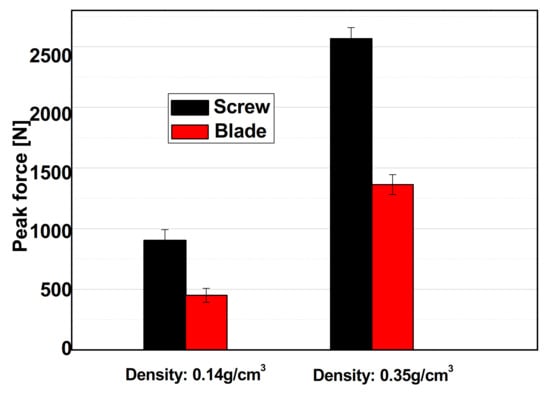
Figure 7.
Comparison of peak force in pull-out test.
3.2. Finite Element Analysis with Damage Model
In order to precisely evaluate the pull-out behavior of the synthetic bone material, commercial FEM software, ABAQUS/Explicit, has been utilized. The screw and helical blade are pre-installed in the synthetic bone material as demonstrated in Figure 8. Since the porous materials show substantially different material behaviors in tension and compression test as represented in Figure 4, it is highly required to adopt the special material model which can express tension–compression anisotropy characteristics. In this paper, the concrete damaged plasticity model [26,28,29] has been applied to numerical simulation for the pull-out test, which does not only represent tensile and compressive material behaviors, simultaneously, but also describes the degradation of material hardening for failure, successfully. The concrete damaged plasticity model assumes the non-associated potential plastic flow where the flow potential, G, used for this model is the Drucker–Prager hyperbolic function as expressed in Equation (1).
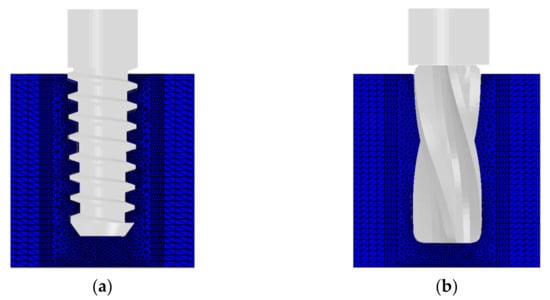
Figure 8.
Initial modeling for FEM analysis: (a) screw; (b) helical blade.
is the dilation angle measured in the p-q plane at high confining pressure, is the uniaxial tensile stress at failure, is a parameter, referred to as the eccentricity, which defines the rate at which the function approaches the asymptote, is the effective hydrostatic pressure, is the effective stress, is the von Mises equivalent stress, where is the deviator of the Cauchy stress tensor, , [30,31,32]. In terms of effective stresses, the yield function, F, takes into consideration the yield strength of tension and compression with the form as follows [31,33],
where is the equivalent plastic strain tensor, is the maximum principal effective stress, is the ratio of initial equibiaxial compressive yield stress to initial uniaxial compressive yield stress, and is the ratio of the second stress invariant on the tensile meridian, and are the effective tensile and compressive cohesion stress, respectively. In addition, and both are dimensionless material constants.
To represent the degradation of the material, the concrete damaged plasticity model adopts the constitutive curves for uniaxial damage in tension and compression, separately, as shown in Figure 9. The evolution of the compressive damage parameter, , is linked to the corresponding plastic strain which is determined proportionally to the inelastic strain using a constant factor with [34].
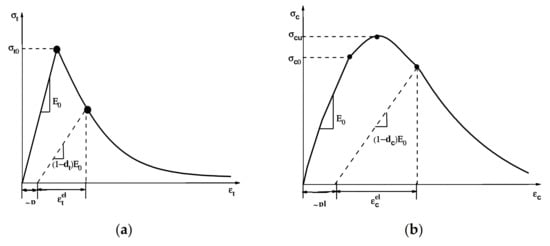
Figure 9.
Constitutive curves for uniaxial damage in: (a) tension; (b) compression.
Similar to Equation (5), the tension damage, , depends on , which is expressed in Equation (6) [34].
Based on these calibrated damage parameters from the tensile and compressive experimental results, it is possible to numerically simulate the material behaviors in tension and compression as shown in Figure 10. Figure 11 compares the pull-out forces between experiment and FEM analysis with the screw and helical blade, which tends to predict the peak pull-out forces, precisely, compared with experimental results. To investigate the failure mechanism during the pull-out test, sectional views at the pull-out stroke of 4 mm and 6 mm have been presented as shown in Figure 12, in which von Mises stress distribution around the screw is substantially larger than that of the helical blade. Furthermore, von Mises stress on the thread of the screw is concentrated severely, which results in material failure to induce pull-out behavior.
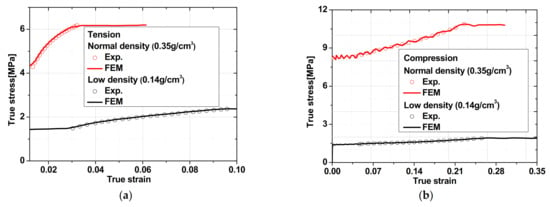
Figure 10.
Comparison of experimental and analysis results using concrete damaged plasticity model with respect to foam density in: (a) tension; (b) compression.
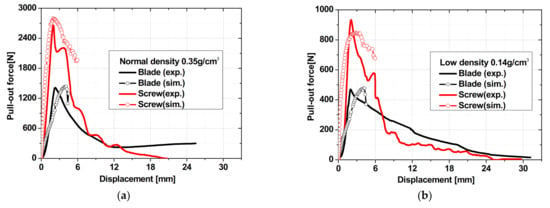
Figure 11.
Comparison of pull-out forces between experiment and FEM analysis with screw and helical blade: (a) normal density (0.35 g/cm3); (b) low density (0.14 g/cm3).
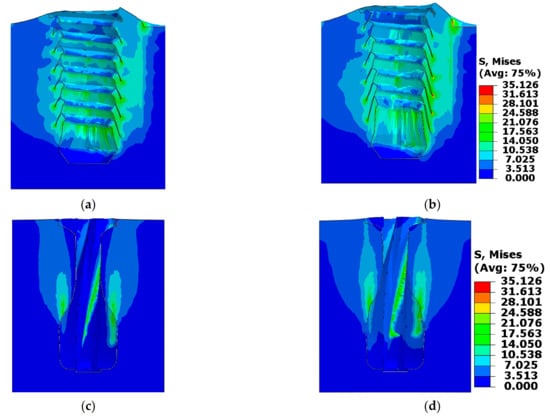
Figure 12.
Distribution of von Mises equivalent stress (MPa) with increase of pull-out stroke in normal foam density (0.35 g/cm3): (a) screw at pull-out stroke of 4 mm; (b) screw at pull-out stroke of 6 mm; (c) helical blade at pull-out stroke of 4 mm; (d) helical blade at pull-out stroke of 6 mm.
3.3. Discussion
From the experimental results of the tension and compression test as represented in Figure 4, the strengths of tension and compression dramatically increase more than three and six times when the density of the PUR foam increases twice, which indicates that the bone density can be the main standard to decide the type of fixation. For these reasons, pull-out performances of the lower density of PUR foam representing osteoporosis are significantly aggravated regardless of types of fixation, as shown in Figure 7. From the results of numerical simulation, the thread of the screw makes it possible to increase the resistance of the pull-out by biting the threads and pre-machined bone, but their resistance dramatically reduced when bone near the thread reaches the onset of fracture during fracture. In the case of the helical blade type, it withstands the pull-out by inducing local plastic deformation near the blade, and the resistance load gradually decreases with the inducing of local plastic deformation without failure when it reaches the peak force as shown in Figure 5. This is why the screw-type exhibits lots of debris near the thread, but it is clean in the helical blade type after the pull-out test, as shown in Figure 6a.
Bergmann et al. [35] have directly measured the contact force on the femoral head according to various types of activity such as walking, stance, and jogging, etc., which were expressed in terms of x, y, z coordinates. To evaluate the critical pull-out force physically, it is necessary to project the contact force (Fres) along the insertion direction as shown in Figure 13. Using Equation (7), projected force, Fproj, is calculated along the insertion direction. Then, stable fixation against screw or helical blade migration is guaranteed when the pull-out force, Fpull-out, from Figure 5 is larger than Fproj.
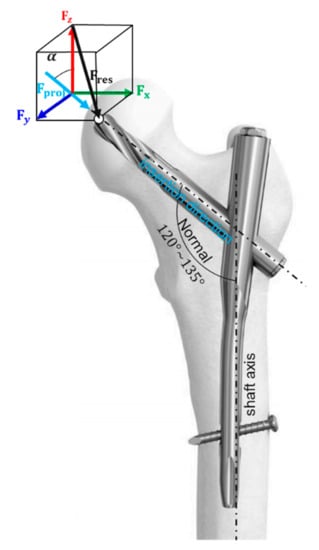
Figure 13.
Relation between contact force on femoral head and pull-out force along insertion direction.
When assuming the walking activity for a person weighing 100 kg, Fproj ranges from 1323.8 N to 629.36 N, when α is 45° and 60° based on the HIGH100 data [36]. By applying the conversion factor, [35], to the previous data for a 100 kg person, Fproj for a person weighing 75 kg is calculated from 406.2 N to 854.1 N. Figure 14 represents the comparison of projected force and pull-out force from the experiment where the orange and blue band highlights the range of Fproj for a 100 kg and 75 kg person, respectively. For a 100 kg person having a normal bone density, both types of fixation are available since the projected force during the walking activity is lower than the pull-out force from the fixations. To minimize the loss of a bone during the surgery, a helical blade type is recommended, because its insertion method could achieve retention and compaction of cancellous bone compared with that of a screw-type implant [16]. However, for a 100 kg person with low bone density, a screw type is recommended to guarantee high clamping force against migration or loosening during the walking activity, as depicted in Figure 14. For an ordinary person (≈75 kg) with normal bone density, both types of fixations are available, since the projected force during the walking activity is lower than the pull-out force from fixation. However, for an ordinary person (≈75 kg) who has low bone density, a screw type is recommended, since the helical blade type shows a lower pull-out force than the projected force induced by walking activity, as represented in Figure 14. Concerning the weight and bone density of an elderly woman who is prone to having osteoporosis, a screw type is also recommended rather than blade types, but it should be considered in terms of the aggravation effect of pre-drilling on the neighbor bone, since the drill bit of pre-drilling for the screw type is larger than the helical blade type.
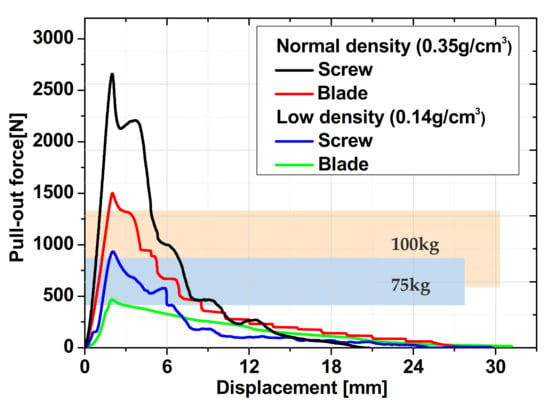
Figure 14.
Comparison of projected force and pull-out force.
4. Conclusions
This paper mainly compares the fixation performances of cephalomedullary nail in terms of the pull-out force when applying screw and helical blade types with respect to femur bone densities. It is substantially important to guide which types of fixation are applied during the operation, since it tends to induce the backout or migration of helical blade and screw depending on the weight and bone density under the fully tightened condition. To compare the pull-out forces between the normal person and an elderly person who has osteoporosis, two different densities of biomedical PUR foam blocks are utilized. The pre-installed screw or helical blade is pulled out while tracking the pull-out load until the final failure occurs. To make a physical comparison of the critical fixation force of screw and helical blade, we have suggested that stable fixation is guaranteed when the pull-out force, Fpull-out, is larger than Fproj. Based on these close examinations, the following conclusions can be drawn:
- (1)
- The clamping force of the screw is about 177% higher than the helical blade in the normal foam density (0.35 g/cm3) and 198% in the low foam density (0.14 g/cm3).
- (2)
- Based on the previous experimental data [35], for a 100 kg person with normal bone density, both types of fixation such as screw and helical blade are available considering walking activity, since the pull-out force, Fpull-out, is greater than the projected force, Fproj. However, the helical blade type is evaluated as more favorable, since the screw-type tends to require predrilling for lateral cortex opening, inducing inevitable loss of cancellous bone.
- (3)
- For a 100 kg person with low bone density, the screw type is recommended to guarantee high clamping force against migration or loosening during walking activity.
Author Contributions
Conceptualization, J.Y. and Y.-C.P.; Data curation, D.-S.C., K.-Y.K., and Y.D.; Formal analysis, K.-Y.K. and Y.D.; Writing—original draft, S.-J.P. and J.Y.; Writing—review & editing, J.Y. All authors have read and agreed to the published version of the manuscript.
Funding
The author Prof. Dong-Sik Chae received research funding from the National Research Foundation of Korea (NRF-2020R1C1C1013166), and the author Prof. Jonghun Yoon received research funding from the National Research Foundation of Korea (NRF) grant funded by the Korea Government (MSIT) (No. 2019R1A2C4070160).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Banan, H.; Al-Sabti, A.; Jimulia, T.; Hart, A.J. The treatment of unstable, extracapsular hip fractures with the AO/ASIF proximal femoral nail (PFN)—Our first 60 cases. Injury 2002, 33, 401–405. [Google Scholar] [CrossRef]
- Hu, S.J.; Yu, G.R.; Zhang, S.M. Surgical treatment of basicervical intertrochanteric fractures of the proximal femur with cephalomeduallary hip nails. Orthop. Surg. 2013, 5, 124–129. [Google Scholar] [CrossRef] [PubMed]
- Holt, G.; Smith, R.; Duncan, K.; Hutchison, J.; Gregori, A. Outcome Afer Surgery for the Treatment of Hip Fracture in the Extremely Elderly. J. Bone Jt. Surg. Vol. 2008, 90, 1899–1905. [Google Scholar] [CrossRef] [PubMed]
- Saarenpää, I.; Partanen, J.; Jalovaara, P. Basicervical fracture-A rare type of hip fracture. Arch. Orthop. Trauma Surg. 2002, 122, 69–72. [Google Scholar]
- Ozdemir, H.; Dabak, T.K.; Urgüden, M.; Gür, S. A different treatment modality fortrochanteric fractures of the femur in surgical high-risk patients: A clinical studyof 44 patients with 21-month follow-up. Arch. Orthop Trauma Surg. 2003, 213, 538–543. [Google Scholar] [CrossRef] [PubMed]
- Leibson, C.L.; Tosteson, A.N.; Gabriel, S.E.; Ransom, J.E.; Melton, L.J. Mortality, disability, and nursing home use for persons with and without hip fracture: A population-based study. J. Am. Geriatr. Soc. 2002, 50, 644–1650. [Google Scholar] [CrossRef]
- Schnell, S.; Friedman, S.M.; Mendelson, D.A.; Bingham, K.W.; Kates, S.L. The 1-Year Mortality of Patients Treated in a Hip Fracture Program for Elders. Geriatr. Orthop. Surg. Rehabil. 2010, 1, 6–14. [Google Scholar] [CrossRef]
- Yu, X.; Wang, H.; Duan, X.; Liu, M.; Xiang, Z. Intramedullary versus extramedullary internal fixation for unstable intertrochanteric fracture, a meta-analysis. Acta Orthop. Traumatol. Turc. 2018, 52, 298–307. [Google Scholar] [CrossRef]
- Bhandari, M.; Guyatt, G.H.; Khera, V.; Kulkarni, A.V.; Sprague, S.; Schemitsch, E.H. Operative management of lower extremity fractures in patients with head injuries. Clin. Orthop. 2003, 407, 187–198. [Google Scholar] [CrossRef]
- Nowotarski, P.J.; Turen, C.H.; Brumback, R.J.; Scarboro, J.M. Conversion of external fixation to intramedullary nailing for fractures of the shaft of the femur in multiply injured patients. J. Bone Jt. Surg. Am. 2000, 82, 781–788. [Google Scholar] [CrossRef]
- Kubiak, E.N.; Bong, M.; Park, S.S.; Kummer, F.; Egol, K.; Koval, K.J. Intramedullary fixation of unstable intertrochanteric hip fractures: One or two lag screws. J. Orthop. Trauma 2004, 18, 12–17. [Google Scholar] [CrossRef] [PubMed]
- Rikli, D.; Goldhahn, J.; Käch, K.; Voigt, C.; Platz, A.; Hanson, B. The effect of local bone mineral density on the rate of mechanical failure after surgical treatment of distal radius fractures: A prospective multicentre cohort study including 249 patients. Arch. Orthop. Trauma Surg. 2015, 135, 201–207. [Google Scholar] [CrossRef]
- Boudard, G.; Pomares, G.; Milin, L.; Lemonnier, I.; Coudane, H.; Mainard, D.; Delagoutte, J.P. Locking plate fixation versus antegrade nailing of 3-and 4-part proximal humerus fractures in patients without osteoporosis. Comparative retrospective study of 63 cases. Orthop. Traumatol. Surg. Res. 2014, 100, 917–924. [Google Scholar] [CrossRef] [PubMed]
- Shin, Y.S.; Chae, J.E.; Kang, T.W.; Han, S.B. Prospective randomized study comparing two cephalomedullary nails for elderly intertrochanteric fractures: Zimmer natural nail versus proximal femoral nail antirotation II. Injury 2017, 48, 1550–1557. [Google Scholar] [CrossRef] [PubMed]
- Okano, I.; Sawada, T.; Kushima, N.; Tachibana, T.; Inagaki, K. Treatment with helical blade Cephalomedullary nail for two-part Basicervical proximal femoral fracture in elderly patients: A retrospective observational study. Geriatr. Orthop. Surg. Rehabil. 2017, 8, 244–251. [Google Scholar] [CrossRef]
- Strauss, E.; Frank, J.; Lee, J.; Kummer, F.J.; Tejwani, N. Helical blade versus sliding hip screw for treatment of unstable intertrochanteric hip fractures: A biomechanical evaluation. Injury 2006, 37, 984–989. [Google Scholar] [CrossRef]
- Massoud, E.I.E. Fixation of subtrochanteric fractures: Does a technical optimization of the dynamic hip screw application improve the results? Strateg. Trauma Limb. Reconstr. 2009, 4, 65–71. [Google Scholar] [CrossRef][Green Version]
- Tornetta, P. Subtrochanteric femur fracture. J. Orthop. Trauma 2002, 16, 280–283. [Google Scholar] [CrossRef]
- Blatter, G.; Janssen, M. Treatment of subtrochanteric fractures of the femur: Reduction on the traction table and fixation with dynamic condylar screw. Arch. Orthop. Trauma Surg. 1994, 113, 138–141. [Google Scholar] [CrossRef]
- Yu, W.; Zhang, X.; Zhu, X.; Hu, J.; Liu, Y. A retrospective analysis of the InterTan nail and proximal femoral nail anti-rotation-Asia in the treatment of unstable intertrochanteric femur fractures in the elderly. J. Orthop. Surg. Res. 2016, 11, 1–7. [Google Scholar] [CrossRef]
- Lee, S.Y.; Niikura, T.; Iwakura, T.; Sakai, Y.; Kuroda, R.; Kurosaka, M. Complete traumatic backout of the blade of proximal femoral nail antirotation: A case report. Orthop. Traumatol. Surg. Res. 2014, 100, 41–443. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Karapinar, L.; Kumbaraci, M.; Kaya, A.; Imerci, A.; Incesu, M. Proximal femoral nail anti-rotation (PFNA) to treat peritrochanteric fractures in elderly patients. Eur. J. Orthop. Surg. Traumatol. 2012, 22, 237–243. [Google Scholar] [CrossRef]
- Lasanianos, N.; Mouzopoulos, G.; Georgilas, I. Hip screw lateral migration with no cut-out or non-union implication: A case report. Cases J. 2009, 2, 1–4. [Google Scholar] [CrossRef]
- Zderic, I.; Willhuber, G.C.; Ahrend, M.D.; Gras, F.; Barla, J.; Sancineto, C.; Windolf, M.; Richards, G.; Gueorguiev, B. Biomechanical comparison between standard and inclined screw orientation in dynamic hip screw side-plate fixation: The lift-off phenomenon. J. Orthop. Transl. 2019, 18, 92–99. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.S.; Goh, T.S.; Heo, J.Y.; Kim, Y.J.; Lee, S.E.; Kim, Y.H.; Lee, C.S. Experimental Evaluation of Screw Pullout Force and Adjacent Bone Damage According to Pedicle Screw Design Parameters in Normal and Osteoporotic Bones. Appl. Sci. 2019, 9, 586. [Google Scholar] [CrossRef]
- Wu, Z.; Nassar, S.A.; Yang, X. Pullout performance of self-tapping medical screws. J. Biomech. Eng. 2011, 133, 1–9. [Google Scholar] [CrossRef]
- Helfrick, M.N.; Niezrecki, C.; Avitabile, P.; Schmidt, T. 3D digital image correlation methods for full-field vibration measurement. Mech. Syst. Signal. Process. 2011, 25, 917–927. [Google Scholar] [CrossRef]
- Demin, W.; Fukang, H. Investigation for plastic damage constitutive models of the concrete material. Procedia Eng. 2017, 210, 71–78. [Google Scholar] [CrossRef]
- Xiao, Y.; Chen, Z.; Zhou, J.; Leng, Y.; Xia, R. Concrete plastic-damage factor for finite element analysis: Concept, simulation, and experiment. Adv. Mech. Eng. 2017, 9, 1–10. [Google Scholar] [CrossRef]
- Cosgun, S.I.; Sesli, H.; Husem, M. Finite Element Model of RC Columns Subjected to Projectile Impact with Different Velocities. Int. J. Struct. Civil. Eng. Res. 2018, 7, 8–14. [Google Scholar] [CrossRef]
- Lubliner, J.; Oliver, J.; Oller, S.; Oñate, E. A plastic-damage model for concrete. Int. J. Solids Struct. 1989, 25, 299–326. [Google Scholar] [CrossRef]
- Zappitelli, M.P.; Villa, E.I.; Sáez, J.F.; Rocco, C.G. Cracking development prediction in concrete gravity dams using concrete damaged plasticity model. Mecánica Comput. 2014, 33, 909–921. [Google Scholar]
- Lee, J.; Fenves, G.L. Plastic-damage model for cyclic loading of concrete structures. J. Eng. Mech. 1998, 124, 892–900. [Google Scholar] [CrossRef]
- Birtel, V.; Mark, P. Parameterised finite element modelling of RC beam shear failure. In Proceedings of the 2006 ABAQUS Users’ Conference, Boston, MA, USA, 23–25 May 2006; pp. 95–108. [Google Scholar]
- Bergmann, G.; Bender, A.; Dymke, J.; Duda, G.; Damm, P. Standardized loads acting in hip implants. PLoS ONE 2016, 15, e0155612. [Google Scholar] [CrossRef]
- Schaeffer, E.K.; Mulpuri, K. Anatomy and Physiology of the Pediatric Hip. Pediatric Adolesc. Hip. 2019, 29–51. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).