Comparison of Palliative Care Models in Idiopathic Pulmonary Fibrosis
Abstract
:1. Introduction
2. Methods
Statistical Analysis
3. Results
3.1. Patient Characteristics
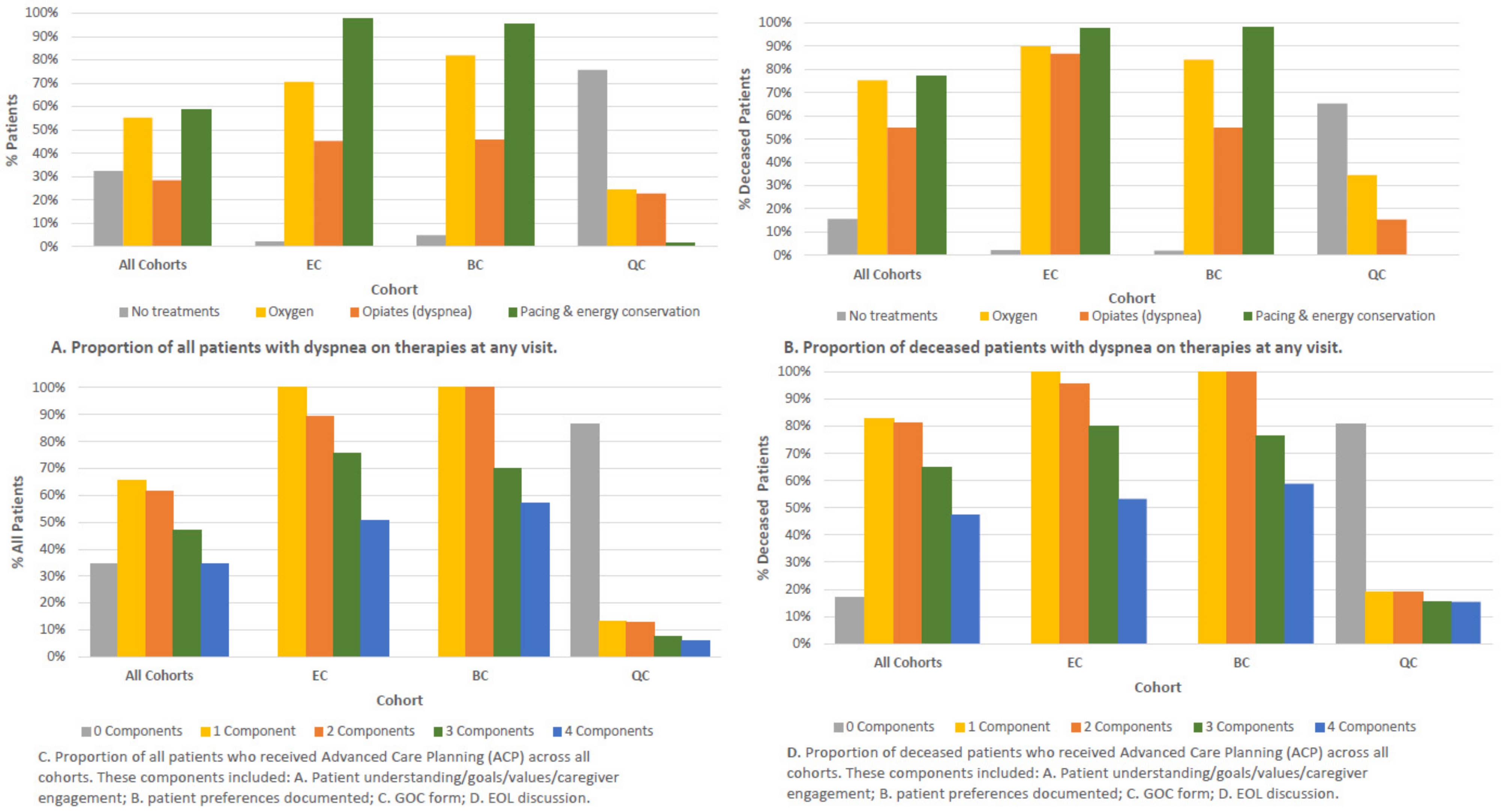
3.2. Palliative Care Delivery—Increased Symptom Management and ACP
3.3. Improved EOL Care
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Swigris, J.J.; Kuschner, W.G.; Jacobs, S.S.; Wilson, S.R.; Gould, M.K. Health-related quality of life in patients with idiopathic pulmonary fibrosis: A systematic review. Thorax 2005, 60, 588–594. [Google Scholar] [CrossRef] [Green Version]
- Lee, J.Y.; Tikellis, G.; Corte, T.J.; Goh, N.S.; Keir, G.J.; Spencer, L.; Sandford, D.; Khor, Y.H.; Glaspole, I.; Price, J.; et al. The supportive care needs of people living with pulmonary fibrosis and their caregivers: A systematic review. Eur. Respir. Rev. 2020, 29, 190125. [Google Scholar] [CrossRef]
- Glaspole, I.N.; Chapman, S.A.; Cooper, W.A.; Ellis, S.J.; Goh, N.S.; Hopkins, P.M.; Macansh, S.; Mahar, A.; Moodley, Y.P.; Paul, E.; et al. Health-related quality of life in idiopathic pulmonary fibrosis: Data from the Australian IPF Registry. Respirology 2017, 22, 950–956. [Google Scholar] [CrossRef] [PubMed]
- Rajala, K.; Lehto, J.; Sutinen, E.; Kautiainen, H.; Myllärniemi, M.; Saarto, T. Marked deterioration in the quality of life of patients with idiopathic pulmonary fibrosis during the last two years of life. BMC Pulm. Med. 2018, 18, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kreuter, M.; Bendstrup, E.; Russell, A.-M.; Bajwah, S.; Lindell, K.; Adir, Y.; Brown, C.E.; Calligaro, G.; Cassidy, N.; Corte, T.J.; et al. Palliative care in interstitial lung disease: Living well. Lancet Respir. Med. 2017, 5, 968–980. [Google Scholar] [CrossRef]
- Schroedl, C.J.; Yount, S.E.; Szmuilowicz, E.; Hutchison, P.J.; Rosenberg, S.R.; Kalhan, R. A qualitative study of unmet healthcare needs in chronic obstructive pulmonary disease: A potential role for specialist palliative care? Ann. Am. Thorac. Soc. 2014, 11, 1433–1438. [Google Scholar] [CrossRef]
- Bajwah, S.; Higginson, I.J.; Ross, J.R.; Wells, A.U.; Birring, S.S.; Riley, J.; Koffman, J. The palliative care needs for fibrotic interstitial lung disease: A qualitative study of patients, informal caregivers and health professionals. Palliat. Med. 2013, 27, 869–876. [Google Scholar] [CrossRef] [PubMed]
- Kalluri, M.; Lu-Song, J.; Younus, S.; Nabipoor, M.; Richman-Eisenstat, J.; Ohinmaa, A.; Bakal, J.A. Health care costs at the end of life for patients with idiopathic pulmonary fibrosis. Evaluation of a pilot multidisciplinary collaborative interstitial lung disease clinic. Ann. Am. Thorac. Soc. 2020, 17, 706–713. [Google Scholar] [CrossRef]
- Bajwah, S.; Ross, J.R.; Wells, A.U.; Mohammed, K.; Oyebode, C.; Birring, S.S.; Patel, A.S.; Koffman, J.; Higginson, I.J.; Riley, J. Palliative care for patients with advanced fibrotic lung disease: A randomised controlled phase II and feasibility trial of a community case conference intervention. Thorax 2015, 70, 830–839. [Google Scholar] [CrossRef] [Green Version]
- Boland, J.; Martin, J.; Wells, A.U.; Ross, J.R. Palliative care for people with non-malignant lung disease: Summary of current evidence and future direction. Palliat. Med. 2013, 27, 811–816. [Google Scholar] [CrossRef]
- Lanken, P.N.; Terry, P.B.; Delisser, H.M.; Fahy, B.F.; Hansen-Flaschen, J.; Heffner, J.E.; Levy, M.; Mularski, R.A.; Osborne, M.L.; Prendergast, T.J.; et al. An official American Thoracic Society clinical policy statement: Palliative care for patients with respiratory diseases and critical illnesses. Am. J. Respir. Crit. Care Med. 2008, 177, 912–927. [Google Scholar] [CrossRef] [Green Version]
- Quill, T.E.; Abernethy, A.P. Generalist plus specialist palliative care—Creating a more sustainable model. N. Engl. J. Med. 2013, 368, 1173–1175. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barratt, S.L.; Morales, M.; Speirs, T.; Al Jboor, K.; Lamb, H.; Mulholland, S.; Edwards, A.; Gunary, R.; Meek, P.; Jordan, N.; et al. Specialist palliative care, psychology, interstitial lung disease (ILD) multidisciplinary team meeting: A novel model to address palliative care needs. BMJ Open Respir. Res. 2018, 5, e000360. [Google Scholar] [CrossRef] [PubMed]
- Wijsenbeek, M.S.; Holland, A.E.; Swigris, J.J.; Renzoni, E. Comprehensive supportive care for patients with fibrosing interstitial lung disease. Am. J. Respir. Crit. Care Med. 2019, 200, 152–159. [Google Scholar] [CrossRef]
- Graney, B.A.; He, C.; Marll, M.; Matson, S.; Bianchi, P.; Cosgrove, G.P.; Lee, J.S.; Abrencillo, R.; Bascom, R.; Scholand, M.B.; et al. Essential components of an interstitial lung disease clinic. Chest 2021, 159, 1517–1530. [Google Scholar] [CrossRef]
- Cottin, V.; Bourdin, A.; Crestani, B.; Prévot, G.; Guérin, M.; Bouquillon, B. Healthcare pathway and patients’ expectations in pulmonary fibrosis. ERJ Open Res. 2017, 3, 00134–02016. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Raghu, G.; Collard, H.R.; Egan, J.J.; Martinez, F.J.; Behr, J.; Brown, K.K.; Colby, T.V.; Cordier, J.-F.; Flaherty, K.R.; Lasky, J.A.; et al. An official ATS/ERS/JRS/ALAT statement: Idiopathic pulmonary fibrosis: Evidence-based guidelines for diagnosis and management. Am. J. Respir. Crit. Care Med. 2011, 183, 788–824. [Google Scholar] [CrossRef] [PubMed]
- Lindell, K.O.; Liang, Z.; Hoffman, L.A.; Rosenzweig, M.Q.; Saul, M.I.; Pilewski, J.M.; Gibson, K.F.; Kaminski, N. Palliative care and location of death in decedents with idiopathic pulmonary fibrosis. Chest 2015, 147, 423–429. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rajala, K.; Lehto, J.T.; Saarinen, M.; Sutinen, E.; Saarto, T.; Myllärniemi, M. End-of-life care of patients with idiopathic pulmonary fibrosis. BMC Palliat. Care 2016, 15, 85. [Google Scholar] [CrossRef] [Green Version]
- Ahmadi, Z.; Wysham, N.G.; Lundström, S.; Janson, C.; Currow, D.; Ekström, M. End-of-life care in oxygen-dependent ILD compared with lung cancer: A national population-based study. Thorax 2016, 71, 510–516. [Google Scholar] [CrossRef] [Green Version]
- Janssen, K.; Rosielle, D.; Wang, Q.; Kim, H.J. The impact of palliative care on quality of life, anxiety, and depression in idiopathic pulmonary fibrosis: A randomized controlled pilot study. Respir. Res. 2020, 21, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liang, Z.; Hoffman, L.A.; Nouraie, M.; Kass, D.J.; Donahoe, M.P.; Gibson, K.F.; Saul, M.I.; Lindell, K.O. Referral to palliative care infrequent in patients with idiopathic pulmonary fibrosis admitted to an intensive care unit. J. Palliat. Med. 2017, 20, 134–140. [Google Scholar] [CrossRef] [PubMed]
- Bischoff, K.E.; Choi, S.; Su, A.; Cohen, E.; O’Riordan, D.L.; Oettel, E.; Blachman, M.; Meister, S.; Zapata, C.; Lindenfeld, P.; et al. Better together: A mixed-methods study of palliative care co-management for patients with interstitial lung disease. J. Palliat. Med. 2021. [Google Scholar] [CrossRef]
- Tikellis, G.; Tong, A.; Lee, J.Y.T.; Corte, T.J.; Hey-Cunningham, A.J.; Bartlett, M.; Crawford, T.; Glaspole, I.; Price, J.; Maloney, J.; et al. Top 10 research priorities for people living with pulmonary fibrosis, their caregivers, healthcare professionals and researchers. Thorax 2021, 76, 575–581. [Google Scholar] [CrossRef] [PubMed]
- Brighton, L.J.; Tunnard, I.; Farquhar, M.; Booth, S.; Miller, S.; Yi, D.; Gao, W.; Bajwah, S.; Man, W.D.; Reilly, C.; et al. Recommendations for services for people living with chronic breathlessness in advanced disease: Results of a transparent expert consultation. Chronic Respir. Dis. 2018, 16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bausewein, C.; Schunk, M.; Schumacher, P.; Dittmer, J.; Bolzani, A.; Booth, S. Breathlessness services as a new model of support for patients with respiratory disease. Chronic Respir. Dis. 2017, 15, 48–59. [Google Scholar] [CrossRef]
- Bajwah, S.; Higginson, I.J.; Ross, J.R.; Wells, A.U.; Birring, S.S.; Patel, A.; Riley, J. Specialist palliative care is more than drugs: A retrospective study of ILD patients. Lung 2012, 190, 215–220. [Google Scholar] [CrossRef]
- Spathis, A.; Booth, S.; Moffat, C.; Hurst, R.; Ryan, R.; Chin, C.; Burkin, J. The breathing, thinking, functioning clinical model: A proposal to facilitate evidence-based breathlessness management in chronic respiratory disease. NPJ Prim. Care Respir. Med. 2017, 27, 27. [Google Scholar] [CrossRef]
- King, T.E.; Bradford, W.Z.; Castro-Bernardini, S.; Fagan, E.A.; Glaspole, I.; Glassberg, M.K.; Gorina, E.; Hopkins, P.M.; Kardatzke, D.; Lancaster, L.; et al. A phase 3 trial of pirfenidone in patients with idiopathic pulmonary fibrosis. N. Engl. J. Med. 2014, 370, 2083–2092. [Google Scholar] [CrossRef] [Green Version]
- Tran, T.; Registry, F.T.E.; Šterclová, M.; Mogulkoc, N.; Lewandowska, K.; Müller, V.; Hájková, M.; Kramer, M.R.; Jovanović, D.; Tekavec-Trkanjec, J.; et al. The European MultiPartner IPF Registry (EMPIRE): Validating long-term prognostic factors in idiopathic pulmonary fibrosis. Respir. Res. 2020, 21, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Visca, D.; Mori, L.; Tsipouri, V.; Fleming, S.; Firouzi, A.; Bonini, M.; Pavitt, M.J.; Alfieri, V.; Canu, S.; Bonifazi, M.; et al. Effect of ambulatory oxygen on quality of life for patients with fibrotic lung disease (AmbOx): A prospective, open-label, mixed-method, crossover randomised controlled trial. Lancet Respir. Med. 2018, 6, 759–770. [Google Scholar] [CrossRef] [Green Version]
- Kalluri, M.; Luppi, F.; Ferrara, G. What patients with idiopathic pulmonary fibrosis and caregivers want: Filling the gaps with patient reported outcomes and experience measures. Am. J. Med. 2020, 133, 281–289. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Archibald, N.; Bakal, J.A.; Richman-Eisenstat, J.; Kalluri, M. Early integrated palliative care bundle impacts location of death in interstitial lung disease: A pilot retrospective study. Am. J. Hosp. Palliat. Med. 2021, 38, 104–113. [Google Scholar] [CrossRef] [PubMed]
- Pooler, C.; Richman-Eisenstat, J.; Kalluri, M. Early integrated palliative approach for idiopathic pulmonary fi-brosis: A narrative study of bereaved caregivers’ experiences. Palliat. Med. 2018, 32, 1455–1464. [Google Scholar] [CrossRef]
- Kalluri, M.; Orenstein, S.; Archibald, N.; Pooler, C. Advance Care Planning Needs in Idiopathic Pulmonary Fi-brosis: A Qualitative Study. Am. J. Hosp. Palliat. Med. 2021. [Google Scholar] [CrossRef]
- Akiyama, N.; Fujisawa, T.; Morita, T.; Mori, K.; Yasui, H.; Hozumi, H.; Suzuki, Y.; Karayama, M.; Furuhashi, K.; Enomoto, N.; et al. Palliative care for idiopathic pulmonary fibrosis patients: Pulmonary physicians’ view. J. Pain Symptom Manag. 2020, 60, 933–940. [Google Scholar] [CrossRef]
- Saeed, F.; Hoerger, M.; Norton, S.A.; Guancial, E.; Epstein, R.M.; Duberstein, P.R. Preference for palliative care in cancer patients: Are men and women alike? J. Pain Symptom Manag. 2018, 56, 1–6. [Google Scholar] [CrossRef] [Green Version]
- Kalafatis, D.; Gao, J.; Pesonen, I.; Carlson, L.; Sköld, C.M.; Ferrara, G. Gender differences at presentation of idiopathic pulmonary fibrosis in Sweden. BMC Pulm. Med. 2019, 19, 222. [Google Scholar] [CrossRef]
| Patient Profile at Baseline | All Cohorts (n = 298) | EC (n = 95) | BC (n = 84) | QC (n = 119) |
|---|---|---|---|---|
| Age, years (median, IQR) | Median: 71 (IQR 67–78) | Median: 71 (IQR 65–76) | Median: 74 (IQR: 68–78) | Median: 74 (IQR 68–79) |
| Gender (%) | M: 73.8% (220), F: 26.1% (78) | 65.3% m (62), 34.7% f (33) | 85.7% m (72), 14.3% f (12) | 72.3% M (86), 27.7% F (33) |
| BMI (median, IQR) | 28.3, 25.5–32.0 | 29.0, 26.0–33.3 | 26.4, 24.6–28.7 | 29.9, 26.5–32.2 |
| CCI (median, IQR) | 4, 3–5 | 3, 3–4 | 4, 3–5 | 4, 3–5 |
| Ever smoker (%) | 78.1% (225/288) | 82.0% (73/89) | 77.1% (64/83) | 75.9% (88/116) |
| Dyspnea (Y/N %) | 97.0% (289/298) | 95.8% (91/95) | 96.4% (81/84) | 98.3% (117/119) |
| MRC score (median, IQR) | 3, 2–4 | 3, 2–4 | 3, 2–4 | 2, 2–4 |
| Cough (Y/N %) | 81.6% (239/293) | 79.8% (75/94) | 75.9% (63/83) | 87.1% (101/116) |
| Fatigue (Y/N %) | 32.1% (86/268) | 52.9% (37/70) | 27.2% (22/81) | 23.1% (27/117) |
| % pred FVC (median, IQR) | 73%, 61–85% | 73%, 63–83% | 69%, 57–80% | 81%, 70–92% |
| FVC ≤ 50% | 10.1% (28/278) | 9.20% (8/87) | 13.1% (11/84) | 8.41% (9/107) |
| % pred DLCO adj for Hg FVC (median, IQR) | 48%, 39–61% | 47%, 38–59% | 38%, 30–46% | 54%, 45–67% |
| DLCO ≤ 35% | 16.5% (40/243) | 20.5% (15/73) | 30.4% (21/69) | 3.96% (4/101) |
| 6MWD, m (median, IQR) | 330, 240–424 | 328, 210–445 | 260, 200–340 | 384, 314–456 |
| Nadir % SpO2 (median, IQR) | 87%, 82–91% | 84%, 80–88% | 85%, 82–89% | 91%, 85–95% |
| GAP Stage I | 36.8% (102/277) | 36.8% (32/87) | 23.8% (20/84) | 47.2% (50/106) |
| GAP Stage II | 43.3% (120/277) | 41.4% (36/87) | 45.2% (38/84) | 43.4% (46/106) |
| GAP Stage III | 19.9% (55/277) | 21.8% (19/87) | 30.9% (26/84) | 9.43% (10/106) |
| Antifibrotics (%) | 39.5% (110/298) | 24.2% (23/95) | 31.0% (26/84) | 58.0% (69/119) |
| Anti-acid medications (PPI) (%) | 58.8% (174/296) | 66.3% (63/95) | 47.6% (40/84) | 60.7% (71/117) |
| NAC (%) | 9.06% (27/296) | 3.16% (3/95) | 4.76% (4/84) | 17.1% (20/117) |
| NIV (CPAP/Bipap) | 4.62% (12/260) | 19.3% (11/57) | 1.19% (1/84) | 0 |
| Transplant | 1 tx, 9 listed | 0 tx, 6 listed | 1 tx, 1 listed | 0 tx, 2 listed |
| V1 and Any Visit | All Cohorts (n = 298) | EC (n = 95) | BC (n = 84) | QC (n = 119) | p Value | ||||
|---|---|---|---|---|---|---|---|---|---|
| V1 | Any visit | V1 | Any visit | V1 | Any visit | V1 | Any visit | ||
| Palliative care (%) | 54% (161/298) | 63% (188/298) | 91.6% (87/95) | 98% (93/95) | 86.9% (73/84) | 94% (79/84) | 0.84% (1/119) * | 13.4% (16/119) * | <0.001/<0.001 |
| I. Symptom Assessment/Documentation (%Y, tool) | |||||||||
| MRC | 97% (289/298) | 97.7% (291/298) | 95.8% (91/95) | 96.8% (92/95) | 96.4% (81/84) | 97.6% (82/84) | 97.5% (116/119) | 99.2% (118/119) | 0.8/0.4 |
| Other | 64.8% (193/298) | 93.9% (201/214) | 91.6% (87/95) MDDS | 93.7% (89/95) MDDS | ILD tool # NR | UCSD: 89.1% (106/119) | UCSD: 94.1% (112/119) | 0.6/ 0.05 | |
| II. Symptom Management (%Y) | |||||||||
| Pacing or energy conservation | 53.7% (160/298) | 58.4% (174/298) | 91.6% (87/95) | 97.9% (93/95) | 86.9% (73/84) | 94.0% (79/84) | 0% (0/119) * | 1.68% (2/119) * | <0.001/<0.001 |
| Oxygen | 33.2% (99/298) | 55.7% (166/298) | 48.4% (46/95) | 70.5% (67/95) | 52.4% (44/84) | 86.9% (70/84) | 7.56% (9/119) | 24.4% (29/119) | <0.001/<0.001 |
| Opiates (for dyspnea) | 7.71% (23/298) | 28.2% (84/298) | 14.7% (14/95) | 45.2% (43/95) | 10.7% (9/84) | 45.2% (38/84) | 0.840% (1/119) | 22.7% (27/119) | <0.001/<0.001 |
| III. ACP (A–D) | |||||||||
| A. Patient understanding Goals/values/caregiver engagement (any 1) | 58.4% (174/298) | 66.1% (197/298) | 93.7% (89/95) | 97.9% (93/95) | 100% (84/84) | 100% (84/84) | 5% (1/119) | 13.4% (16/119) | <0.001/<0.001 |
| B. Patient preferences documented | 31.2% (93/298) | 52.3% (156/298) | 67% (64/95) | 83.1% (79/95) | 33.3% (28/84) | 71.4% (60/84) | 5.88% (1/119) | 14.2% (17/119) | <0.001/<0.001 |
| DNI/DNR/non-ICU (medical care) only | 19.1% (57/298) | 43.6% (130/298) | 48.4% (46/95) | 62.1% (59/95) | 11.9% (10/84) | 67.8% (57/84) | 0.84% (1/119) | 11.8% (14/119) | <0.001/<0.001 |
| C. GOC form | 41.6% (124/298) | 49.3% (147/298) | 43.2% (41/95) | 58.9% (56/95) | 97.6% (82/84) | 97.6% (82/84) | 0.84% (1/119) * | 7.56% (9/119) * | <0.001/<0.001 |
| D. EOL discussion | 29.9% (89/298) | 47.7% (142/298) | 71.6% (68/95) | 84.2% (80/95) | 22.6% (19/84) | 63.1% (53/84) | 1.68% (2/119) * | 7.56% (9/119) * | <0.001/<0.001 |
| IV. Palliative assessments (%Y) | |||||||||
| PC Specialist consultation | 1.68% (5/298) | 19.5% (58/298) | 0% (0/95) | 3.16% (3/95) | 2.38% (2/84) | 20.2% (17/84) | 2.52% (3/119) | 21% (25/119) | 0.7 |
| Palliative multidisciplinary discussion | N/A | N/A | N/A | N/A | 11.9% (10/84) | 54% (45/84) | N/A | N/A | N/A |
| All Cohorts | EC | BC | QC | p-Value | |
|---|---|---|---|---|---|
| Deceased of total | 40.9% (122/298) | 47.4% (45/95) | 60.7% (51/84) | 21.8% (26/119) | <0.001 |
| Palliative care (%) | 76.2% (93/122) | 91.1% (41/45) | 92.1% (47/51) | 19.2% (5/26) | <0.001 |
| Interval between last visit and death (median months, IQR) | 3, IQR 1–6 | 2, IQR 1–5 | 3, IQR 1–5 | 3.5 *, IQR 1.25–15.5 | 0.01 |
| Median #EOL visits (last 6 months), IQR | 1, 0–2 | 1, 1–2 | 1, 1–2 | 0 *, 0–2 | 0.3 |
| Symptom Management | |||||
| Pacing or Energy conservation | 72.1% (88/122) | 91.1% (41/45) | 92.2% (47/51) | 0% (0/26) * | <0.001 |
| Oxygen (%) | 66.4% (81/122) | 82.2% (37/45) | 76.5% (39/51) | 19.2% (5/26) * | 0.04 |
| Initiated (median months, IQR) | 15, IQR 6–27 | 21, IQR 9–31 | 10, IQR 5–21 | NR | <0.001 |
| Opiates for dyspnea (%) | 35.2% (43/122) | 51.1% (23/45) | 39.2% (20/51) | 15.4% (4/26) * | 0.01 |
| Initiated (median months, IQR) | 5, IQR 2–9 | 5, IQR 2–12 | 4, IQR 2–8 | N/A | 0.1 |
| ACP (A-D) | |||||
| A. Documentation of patient understanding/goals/values/CG (any) | 80.3% (98/122) | 93.3% (42/45) | 100% (51/51) | 19.2% (5/26) * | <0.001 |
| B. Patient preferences documented | 68.8% (84/122) | 93.3% (42/45) | 72.5% (37/51) | 19.2% (5/26) * | 0.001 |
| Preferred type of Care (DNR/DNI/Others) | 63.9% (78/122) | 80% (36/45) | 72.5% (37/51) | 19.2% (5/26) * | <0.001 |
| Preferred location of death | Home 50% (61/122) Hospice 0.001% (4/122) Hospital 5.7% (7/122) | Home 60% (27/45) Hospice 8.8% (4/45) Hospital 13.3% (6/45) | Home 66.6% (34/51) Hospice 0 Hospital 2% (1/51) | NR | |
| C. GOC form | 61.4% (75/122) | 60% (27/45) | 86% (44/51) | 15.4% (4/26) * | <0.001<0.001 |
| D. EOL disc | 54.1% (66/122) | 73.3% (33/45) | 62.7% (32/51) | 3.8% (1/26) * | 0.001 |
| Palliative assessments (%Y) | |||||
| PC Specialist Consultation | 13.9% (17/122) | 6.6% (3/45) | 17.6% (9/51) | 19.2% (5/26) * | 0.2 |
| Palliative Multidisciplinary Discussion | N/A | N/A | 49.0% (25/51) | N/A | |
| Location of Death | All Cohorts | EC | BC | p-Value |
|---|---|---|---|---|
| Home Hospice | 47.9% (46/96) 11.5% (11/96) | 42.2% (19/45) 20% (9/45) | 52.9% (27/51) 3.92% (2/51) | 0.05 |
| Home & Hospice concordance rate (actual: preferred) | 57:98 | 28:48 | 29:50 | |
| Hospital ICU | 37.5% (36/96) 1.04% (1/96) | 37.8% (17/45) 2.22% (1/45) | 37.3% (19/51) 0% (0/51) | 0.82 |
| Hospital concordance rate (actual/preferred) | 36:10 | 17:7 | 19:3 | |
| Location of Death Concordance Kappa (95% CI) | 0.002 (−0.146–0.170) | 0.29 (−0.02–0.51) | −0.11 (−0.20–0.15) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Younus, S.; Bakal, J.A.; Richman-Eisenstat, J.; Alrehaili, G.; Aldhaheri, S.; Morales, M.; Rippon, N.; Bendstrup, E.; Harle, I.; Moran-Mendoza, O.; et al. Comparison of Palliative Care Models in Idiopathic Pulmonary Fibrosis. Appl. Sci. 2021, 11, 9028. https://doi.org/10.3390/app11199028
Younus S, Bakal JA, Richman-Eisenstat J, Alrehaili G, Aldhaheri S, Morales M, Rippon N, Bendstrup E, Harle I, Moran-Mendoza O, et al. Comparison of Palliative Care Models in Idiopathic Pulmonary Fibrosis. Applied Sciences. 2021; 11(19):9028. https://doi.org/10.3390/app11199028
Chicago/Turabian StyleYounus, Sarah, Jeffrey A. Bakal, Janice Richman-Eisenstat, Ghadah Alrehaili, Sharina Aldhaheri, Michelle Morales, Naomi Rippon, Elisabeth Bendstrup, Ingrid Harle, Onofre Moran-Mendoza, and et al. 2021. "Comparison of Palliative Care Models in Idiopathic Pulmonary Fibrosis" Applied Sciences 11, no. 19: 9028. https://doi.org/10.3390/app11199028
APA StyleYounus, S., Bakal, J. A., Richman-Eisenstat, J., Alrehaili, G., Aldhaheri, S., Morales, M., Rippon, N., Bendstrup, E., Harle, I., Moran-Mendoza, O., Barratt, S. L., Adamali, H., & Kalluri, M. (2021). Comparison of Palliative Care Models in Idiopathic Pulmonary Fibrosis. Applied Sciences, 11(19), 9028. https://doi.org/10.3390/app11199028








