Abstract
Background: Dentists (Ds) and dental assistants (DAs) have a high lifetime prevalence of musculoskeletal disorders (MSDs). In this context, it is assumed that they have an increased intake of substances such as pain medication. Currently, there exist no data on the use of medication among Ds and DAs with MSDs in Germany. Methods: The online questionnaire (i.e., the Nordic Questionnaire) analysed the medical therapies used by 389 Ds (240 f/149 m) and 406 DAs (401 f/5 m) to treat their MSDs. Results: Ds (28.3–11.5%) and DAs (29.4–10.3%) with MSDs took medication depending on the affected body region. A trend between the Ds and DAs in the intake of drug therapy and the frequency was found for the neck region (Ds: 21.1%, DAs: 28.7%). A single medication was taken most frequently (Ds: 60.0–33.3%, DAs: 71.4–27.3%). The frequency of use varied greatly for both occupational groups depending on the region affected. Conclusion: Ds and DAs perceived the need for medical therapies because of their MSDs. Painkillers such as ibuprofen and systemic diclofenac were the medications most frequently taken by both occupational groups. The intake of pain killers, most notably for the neck, should prevent sick leave.
1. Introduction
Dentists (Ds) and dental assistants (DAs) are exposed to several risk factors for developing musculoskeletal disorders (MSDs) due to their occupational demands, such as prolonged static postures, repetitive movements, instrument vibration, poor lighting conditions, poor and awkward positioning of the dental health professionals (DHPs) when working on the patients or the poor positioning of the patients [1]. A high prevalence of MSDs in dental personnel has been demonstrated in several international studies over many years [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18]. The regions of the neck, shoulder and back are the most affected [3,4,19]. In previous studies with Ds and DAs in Germany [3,4], 96.1% of Ds and 98.5% of DAs reported a lifetime prevalence, 92.8% of Ds and 97.5% of DAs a 12-month prevalence and 66.8% of Ds and 86.9% of DAs a 7-day prevalence of MSDs.
DHPs, like other healthcare professionals (HCPs), play an important role in society by maintaining the health of others. The importance of this task may mean that Ds and DAs do not wish to, or cannot easily, interrupt their work. Ds, in particular, not only have a responsibility in their medical work towards the patient, but also an economic responsibility in the context of a managerial function or ownership of a practice towards the staff. This leads to the assumption that the interruption of dental work is not desirable, which may, thus, predispose Ds and DAs to increased work injuries such as MSDs [2].
In order to be able to continue working despite complaints, painkillers, among other things, are taken to alleviate or suppress illness-related complaints [2,20]. The use of alcohol and other drugs are also used in this regard [21]. It is estimated that around 10.0–15.0% of all HCPs misuse drugs or alcohol at some point in their career [20]; 6.0–8.0% of HCPs have a substance use disorder while up to 14.0% have an alcohol use disorder [20]. Overall, there are few studies, internationally, that examine substance use in HCPs. This may partly be due to the fact that it is a topic that HCPs do not wish to talk about. However, this also means that the figures from studies carried out are probably higher in reality due to underreporting.
The present study is part of a research project on the optimisation of ergonomics in dentistry (German abbrev.: SOPEZ) [22]. As part of this large study, the highest lifetime prevalence of MSDs was found at the neck (Ds: 79.4%, DAs: 90.9%), followed by the shoulder (Ds: 66.8%, DAs: 80.0%), lower back (Ds: 58.6%, DAs: 68.7%) and upper back (Ds: 42.9%, DAs: 56.9%) regions [3,4].
In this context, the question arises whether, in Germany, these complaints are treated with medication in order to continue achieving professional performance and to ensure the supply of health care. Therefore, the aim of the present study was threefold: (1) to survey the choice of drug therapy among Ds and DAs, as well as (2) the substrates and (3) the frequency of intake. The hypotheses to be tested are:
- Both dentists and dental assistants take pain medication to reduce MSD.
- There is no difference in the amount of medication intake between dentists and dental assistants.
- There is no difference in the frequency of medication intake between dentists and dental assistants.
2. Materials and Methods
2.1. Subjects
Of the 2548 people who followed the link to the online questionnaire of the present observational and cross-sectional study, 795 participants completed the questionnaire and were included in the analysis. Of these, 389 were Ds (240 f/149 m) and 406 were DAs (401 f/5 m).
Inclusion criteria were that the participants should be Ds or DAs, as well as DAs in training (with a minimum age of 18 years and a job or training position as a DA) in Germany. Occupational groups that were not regarded as Ds or DAs (e.g., dental hygienists, employees in administration, industry and the dental laboratory) and also dental students, as they have little or no practical experience depending on the year of study (in contrast to DAs in training, who already have a permanent dental job at the beginning of their training), were excluded. Additionally, discontinued questionnaires and participants with missing important information (e.g., gender) were excluded.
Table 1 shows individual data of the interviewed Ds and DAs. In addition to the number (n) and the corresponding percentage (%) of the study population, the median ( and the interquartile range (I50) were calculated.

Table 1.
Individual data of the study population: Ds and DAs.
Overall, 96.1% of Ds and 98.5% of DAs reported a lifetime prevalence of MSDs [3,4]. Figure 1 shows the lifetime prevalence of the respective body regions.
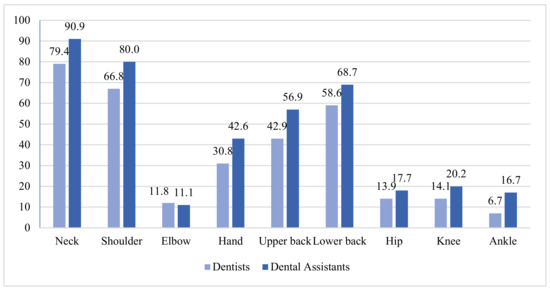
Figure 1.
Lifetime prevalence of MSDs among Ds and DAs expressed as a %.
The study was approved by the local medical ethics committee of the medical faculty (Goethe University Frankfurt; No. 356/17 [7 February 2018]).
2.2. Questionnaire
The questionnaire was part of the SOPEZ project on the optimisation of ergonomics in dentistry, regarding among other things MSDs among Ds and DAs [22]. Results of the prevalence of MSDs, socio-demographic and workplace information among Ds and DAs in Germany have already been published [3,4,23].
At the beginning of the online survey, a declaration of informed consent had to be accepted. The personal data have been anonymized so that the subject cannot be identified. The present questionnaire consisted of questions concerning the medical therapies used to treat MSDs. If drug treatment was indicated, the questionnaire also asked about the substance, the number of drugs and the frequency with which they were taken. These questions were asked for each body region affected by MSDs according to the Nordic Questionnaire scheme by Kuorinka et al. [24,25].
The Nordic Questionnaire according to Kuorinka et al. [25] examines musculoskeletal complaints using 28 multiple choice questions for the nine body regions of the neck, shoulder, elbow, wrist, thoracic spine, lumbar spine, hip, knee and ankle. The questions ask about the 7-day prevalence and 12-month prevalence. In addition, the Nordic Questionnaire asks about the lifetime prevalence of MSDs, professional and private consequences of MSDs, the duration of the problems, possible accidents and therapies in the three areas: the neck, shoulder and lower back. The validated questionnaire is used for various studies worldwide to describe MSDs in different work settings.
The questionnaire was subjected to a pretest with n = 13 participants and thus checked for comprehensibility and functionality. This was followed by a re-evaluation and adjustment.
2.3. Recruitment
Participants were recruited through several channels. The project presentation and distribution of flyers took place at the German Dentists’ Day in Frankfurt am Main (Germany) on 9–11 October 2018 and at the International Dental Show (IDS) in Cologne (Germany) on 15 March 2019 and 16 March 2019 (which are both considered as the largest events for Ds and DAs in Germany). Furthermore, articles were published in the dental journals “Die Zahnärzte Woche (DZW)” and “Zahnärztliche Mitteilungen (ZM)” to inform about the study. In addition, the dental chambers nationwide were made aware of the study. Subsequently, the information was shared via various internal networks of dental employees. Furthermore, various German social networks of Ds, DAs and DAs in training were used to further disseminate the project.
These data were collected via the online platform SoSci Survey [26] between May 2018 and May 2019.
2.4. Data Editing and Analysis
The data were collected via the SoSci Survey [26] and afterwards exported to “Microsoft Excel 16.5” [27], where data checking, editing and coding took place. Improvements were made with regard to the logic of the answers, e.g., in the case of incorrect occupational classifications.
Named drugs were grouped into categories. While the pain medications were divided into their active ingredients (arcoxia, ASS 500, systemic diclofenac, local diclofenac, ibuprofen, metamizol, naproxen, paracetamol, tapendadol, tilidin, tramadol), other medications were grouped under “further”. “Further” includes immunosuppressants (further subdivided into systemic cortisone, cortisone injections, MTX and other individual treatments), muscle relaxants (further subdivided into ortoton, tizinidine, tolperisone and others with individual mentions), other injections (except cortisone injections) as well as other medication (adjuvants, antidepressants, antihypertensives, anticoagulation, hormones, minerals, vitamins and others).
If the recorded number of medicines taken did not correspond to the single mention of medicines, the number was corrected. The answers to the option of an open statement regarding the frequency of taking medication (in addition to monthly, weekly and daily) were divided into categories. The answers were subsequently allocated under “as needed”, “rarely” and “others” (information that could not be clearly classified).
After the improvements, the data were transferred and analysed descriptively in IBM Statistics SPSS 26 [28]. The median and the interquartile range were calculated for the non-normally distributed data which were evaluated using the Kologorov–Smirnov test. Significant differences were determined by using the Chi2 test. The significances in the results section were marked, for example, as: * at p = 0.02. The individual therapies with their subcategories were not tested for significance due to their low frequency (≤9) in the present paper. The p-values were subjected to a Bonferroni–Holm correction. The significance level was set at 5%.
Research manuscripts reporting large datasets that are deposited in a publicly available database should specify where the data have been deposited and provide the relevant accession numbers. If the accession numbers have not yet been obtained at the time of submission, please state that they will be provided during review. They must be provided prior to publication.
Interventionary studies involving animals or humans, and other studies that require ethical approval, must list the authority that provided approval and the corresponding ethical approval code.
3. Results
Table 2 shows that, depending on the region affected by MSDs, 28.3–11.5% of Ds and 29.4–10.3% of DAs were aware of suitable medical therapies for the MSDs. The difference between the occupational groups regarding the use of medicines for treating MSDs was significant for the neck (p = 0.02); however, after a Bonferroni–Holm correction, this significance did not hold.

Table 2.
Medical therapy of MSDs among Ds and DAs in Germany in n (%).
The Intake of Medication against MSDs
Table 3 shows that Ds (60.0–33.3%) and DAs (71.4–27.3%) were most likely to take one single medication to treat MSDs. This was true for all body regions with MSDs except for the elbow region (45.5% of DAs most often used two medications), the knee region (50.0% of Ds most often used no medication) and the hip regions (30.0% of DAs used either no, one or two medication/s most often, while 33.3% of Ds used either no or one medication most often).

Table 3.
Current number of medications used for MSD treatment among Ds and DAs in Germany in n (%).
The difference between the occupational groups with regard to the number of medications taken to treat MSDs was significant only for the neck region (p = 0.05). After a Bonferroni–Holm correction, this significance did not hold.
Table 4 shows that the most commonly chosen frequency of medication intake among Ds was “as needed” for MSDs of the neck (20.7%). Medications for MSDs of the shoulder (28.6%) and the upper back (31.6%) were most frequently taken monthly, while MSDs of the elbow were most often treated weekly (25.0%) and of the hand, daily (30.8%). The lower back (23.9%) and hip (33.3%) regions were most commonly treated “as needed” and daily.

Table 4.
Frequency of medication use for MSDs among Ds and DAs in Germany in n (%).
In the case of the DAs, medication was most frequently taken on a weekly basis (between 50.0% and 28.6%) for MSDs of the shoulder, hand, upper back, lower back and hip. For MSDs of the neck, medication was most frequently taken on a monthly or weekly basis (29.6% each). The most frequent treatment for the elbow (36.4%) and ankle (40.0%) was “as needed” and for the knee, daily (41.7%).
The difference between the occupational groups with regard to the frequency of taking medication for MSDs was significant only for the neck (p = 0.01). After a Bonferroni–Holm correction, this significance did not hold.
Table 5 and Table 6 summarize the most frequent pain medication choices taken by the Ds and DAs. The most common choice of pain medication against all MSDs listed was ibuprofen for both Ds and DAs (44.0–17.6% versus 100.0–37.9%, respectively), as seen in Table 4. Systemic diclofenac was the second most common treatment for Ds and DAs (20.0–5.9% versus 20.2–7.2%, respectively), except for MSDs of DAs at the elbow and hand, whose second most common treatment was topical diclofenac (16.7% and 13.8%, respectively).

Table 5.
Pain medication agents used to treat the MSDs of Ds and DAs, according to body region of Ds and DAs in n (%).

Table 6.
Use of co-analgesics in treating MSDs of Ds and DAs, according to body region in n (%).
Table 6 lists other co-analgesics that are also used for analgesia but primarily are used for treating other conditions [29]. Table 6 shows that the most commonly used immunosuppressant was MTX (up to 20.0% of Ds; up to 16.7% of DAs) followed by systemic cortisone (up to 11.8% of Ds; up to 13.8% of DAs). The most commonly used muscle relaxant was ortoton (up to 12.0% of Ds; up to 6.4% of DAs). Other injections were reported by up to 20.0% of Ds and up to 16.7% of DAs.
4. Discussion
The present study shows that both Ds and DAs perceived the need for drug therapies for MSDs; accordingly, the majority of MSD complaints were deemed sufficiently severe to require therapy. Those affected by MSDs sought medical therapy and, thus, accepted possible consequences such as costs, time or side effects. Drug therapy was carried out by 28.3–11.5% of Ds with MSDs and by 29.4–10.3% DAs with MSDs. Therefore, hypothesis 1 can be verified. One possible explanation is that drug therapy can, presumably, be started more quickly and easily and that taking it involves less effort than other therapy concepts like physiotherapy or osteopathy.
The comparison between Ds and DAs showed a great similarity in the use of medication. All subjects seem to take medications according to their efficacy, regardless of their occupational belonging. In each case, a similar number took a medical therapy; only the medication use for MSDs of the neck was used more by DAs. Thus, the most frequently taken medications in both occupational groups were represented by pain medication. It could be shown that especially the non-opioid analgesics, in particular, ibuprofen and diclofenac, were taken, regardless of the two occupational groups; low-potency opioid analgesics were rarely taken and high-potency opioid analgesics not at all. This means that the pain therapy chosen by the Ds and DAs was mainly in the range of the first stage of the WHO-stage scheme and only very rarely in the range of the second stage [30]. Co-analgesics were also reported to treat the symptoms, such as immunosuppressants, muscle relaxants and other injections. However, compared to the use of pain medication, the numbers were very low. One possible explanation for the choice of medication could be the effect of the active ingredients. Both ibuprofen and diclofenac belong to the group of non-steroidal anti-inflammatory drugs (NSAIDs) and are, therefore, not only effective against pain, but also have a fever-reducing musculoskeletal pain caused by an anti-inflammatory effect [31]. Furthermore, both these medicines are available over-the-counter and so do not require a prescription.
The number of medications taken was similar for Ds and DAs with MSDs and, with a few exceptions, was a single product. It can be assumed that the respective medications taken have a symptom-reducing effect. In addition, a combination of two NSAIDs, which were taken most frequently by the respondents, is not recommended due to a small increase in analgesic effect but a notable increase in side effects [32]. The knowledge of Ds and DAs on this subject could explain why in most cases only one agent was taken. Therefore, hypothesis 2 can be verified.
The frequency of medication intake showed that Ds took their medication more irregularly but also more frequently as needed, depending on the region, while the DAs took their medication more frequently on a weekly basis. One reason for this is that the most commonly taken drugs from the NSAID class are not taken regularly over a long period of time because of the possible adverse effects; these include asthma attacks, increased risk of cardiovascular events or the loss of cytoprotective prostaglandins and the associated damage to the gastric and intestinal mucosa [33]. Since DAs took their medication more frequently on a weekly basis and Ds more frequently as needed, hypothesis 3 has to be rejected.
Compared to a previous study [20] on substance use in HCPs, little to no regular use of opioids was found in the present study. At this point it should be mentioned that in the present study the focus was on the use of medication for complaints caused by MSDs and not on the use of substances due to various other causes [20]. Since the aim of the present analysis was to investigate the use of drugs for pain relief from MSDs no statement can be made of the use of other drugs, such as alcohol or other substances due to other complaints. In addition, another study could investigate other causes or variables besides MSDs for taking medication, such as other illnesses of a DHP or the psychological and psychosocial components at the workplace of Ds or DAs. These facts would be another interesting topic for a future study among DHPs in Germany.
All data, including those on the prevalence of the disease or on therapy, were self-reported by the respondents and not verified by HCPs. This may have led to conscious or unconscious errors when filling out the questionnaire. It was also not possible to subdivide the active substance according to dose although it was explicitly asked for. Participants were rarely able to answer the question of dosage, which may mean that painkillers are taken automatically regardless of the dose and possible negative physiological side effects. This lack of information also occurred in Ds who had taken pharmacological courses in their studies, which shows the importance of continuing to work regardless of possible health consequences. Furthermore, for Ds, possible revenue-sharing in the practice may lead to increased medication use in order to continue working and earning money. This possible influence could not be investigated in the present analysis, since no data on the earnings structure were collected. Continuing to work despite musculoskeletal complaints, and thus earning enough money, might also be associated with concerns about early retirement in both Ds and DAs. Furthermore, we did not ask women of childbearing age if they were pregnant. Pregnancy could increase the possible use of painkillers in case of discomfort or decrease it in case of contraindication. Comorbidities, e.g., rheumatic diseases were also not considered. Since we focused on the use of pain medication, this aspect should be analysed in future studies. In addition, people suffering from MSDs may be more interested in participating in the questionnaire than people without symptoms, which may have led to a biased prevalence and limited the external validity of the study. In addition, the group studied was only a random sample of the population of dentists or dental assistants; this, together with the fact that younger people feel more familiar with the medium of an online questionnaire than older people, may have led to a rather skewed sample with more younger DHPs being represented (Table 1).
Based on the finding that DHPs are aware of drug therapies against MSDs, a comparative study between Ds and DAs on other therapies, such as physiotherapy, ergo therapy, heat or cold therapy, chiropractic or osteopathy would be interesting. A comparison between the present results of medication use against MSDs in the DHPs and other non-medical professions could not be performed because of missing detailed medication information in other occupational groups worldwide. The investigation of medication use against MSDs in other occupational groups could be part of exciting studies. Furthermore, it would also be interesting to conduct research on the work culture of HCPs with regard to the tolerance of absenteeism due to the illness of an employee or employer and the possible physical and psychological effects. Last, but not least, with regard to the MSDs in dental staff that have been described for a long time, it seems essential to continue to improve the prevention of these diseases and, thereby, also minimize the use of medication in the long term.
5. Conclusions
In summary, both Ds and DAs used medical therapy against MSDs. Ibuprofen and systemic diclofenac were the drugs most frequently taken by both occupational groups. Both Ds and DAs took a single medical product most frequently. The frequency of use varied between occupations and body regions, but without causality.
Author Contributions
Conceptualization: Y.H., A.N. (Antonia Naser), J.H., C.E., W.B., D.A.G. and D.O.; methodology: Y.H., A.N. (Antonia Naser), J.H., L.F., F.H., E.M.W., D.B., A.N. (Albert Nienhaus), D.O.; Software: Y.H., A.N. (Antonia Naser), J.H.; validation: Y.H., A.N. (Antonia Naser), J.H. and D.O.; formal analysis: D.O., Y.H., A.N. (Antonia Naser) and J.H.; investigation: Y.H., A.N. (Antonia Naser), J.H., L.F., F.H., C.E., W.B.; writing—original draft preparation: Y.H., A.N. (Antonia Naser), J.H., L.F., F.H., and D.O.; writing—review and editing: C.E., W.B., E.M.W., D.B., A.N. (Albert Nienhaus) and D.A.G.; supervision: D.O.; project administration: Y.H., D.A.G. and D.O. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was approved by the local medical ethics committee of the medical faculty (Goethe University Frankfurt; No. 356/17).
Informed Consent Statement
Informed consent to participate in this study was obtained from all participants.
Data Availability Statement
The data presented in this study are included in this published article but are also available on request from the corresponding author.
Acknowledgments
We thank Lukasz Hasske from Morita for the possibility of flyer distribution at IDS in Cologne.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Lietz, J.; Kozak, A.; Nienhaus, A. Prevalence and occupational risk factors of musculoskeletal diseases and pain among dental professionals in Western countries: A systematic literature review and meta-analysis. PLoS ONE 2018, 13, e0208628. [Google Scholar] [CrossRef] [Green Version]
- Ayers, K.M.S.; Thomson, W.M.; Newton, J.T.; Morgaine, K.C.; Rich, A.M. Self-reported occupational health of general dental practitioners. Occup. Med. 2009, 59, 142–148. [Google Scholar] [CrossRef] [Green Version]
- Ohlendorf, D.; Haas, Y.; Naser, A.; Haenel, J.; Maltry, L.; Holzgreve, F.; Erbe, C.; Betz, W.; Wanke, E.M.; Brüggmann, D.; et al. Prevalence of Muscular Skeletal Disorders among Qualified Dental Assistants. Int. J. Environ. Res. Public Health 2020, 17, 3490. [Google Scholar] [CrossRef]
- Ohlendorf, D.; Naser, A.; Haas, Y.; Haenel, J.; Fraeulin, L.; Holzgreve, F.; Erbe, C.; Betz, W.; Wanke, E.M.; Brueggmann, D.; et al. Prevalence of Musculoskeletal Disorders among Dentists and Dental Students in Germany. Int. J. Environ. Res. Public Health 2020, 17, 8740. [Google Scholar] [CrossRef]
- Ratzon, N.; Yaros, T.; Mizlik, A.; Kanner, T. Musculoskeletal symptoms among dentists in relation to work posture. Work 2000, 15, 153–158. [Google Scholar] [PubMed]
- Feng, B.; Liang, Q.; Wang, Y.; Andersen, L.L.; Szeto, G. Prevalence of work-related musculoskeletal symptoms of the neck and upper extremity among dentists in China. BMJ Open 2014, 4, e006451. [Google Scholar] [CrossRef] [Green Version]
- Meyer, V.P.; Brehler, R.; Castro, W.H.M.; Nentwig, C.G. Arbeitsbelastungen bei Zahnärzten in Niedergelassener Praxis: Eine Arbeitsmedizinische Bestandsaufnahme zu Wirbelsäulenbelastungen, Berufsdermatosen und Stressfaktoren; Deutscher Zahnärzte Verl. DÄV-Hanser: München, Germany, 2001; p. 167. [Google Scholar]
- Zafarmand, A.H.; Nokhostin, M.R. “Musculoskeletal problem”: Its prevalence among Iranian dentists. J. Int. Soc. Prev. Community Dent. 2016, 6, S41–S46. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Proteau, R.-A. Prevention of work-related musculoskeletal disorders (MSDs) in dental clinics. Asstsas Montréal QC Can. 2009, 1–104. [Google Scholar]
- Harutunian, K.; Gargallo-Albiol, J.; Figueiredo, R.; Escoda, C.G. Ergonomics and musculoskeletal pain among postgraduate students and faculty members of the School of Dentistry of the University of Barcelona (Spain). A cross-sectional study. Med. Oral Patol. Oral Y Cir. Bucal 2011, 16, e425–e429. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hodacova, L.; Sustova, Z.; Čermáková, E.; Kapitán, M.; Šmejkalová, J. Self-reported risk factors related to the most frequent musculoskeletal complaints among Czech dentists. Ind. Health 2015, 53, 48–55. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lindfors, P.; Von Thiele, U.; Lundberg, U. Work Characteristics and Upper Extremity Disorders in Female Dental Health Workers. J. Occup. Health 2006, 48, 192–197. [Google Scholar] [CrossRef] [Green Version]
- Alghadir, A.; Zafar, H.; Iqbal, Z.A. Work-related musculoskeletal disorders among dental professionals in Saudi Arabia. J. Phys. Ther. Sci. 2015, 27, 1107–1112. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dajpratham, P.; Ploypetch, T.; Kiattavorncharoen, S.; Boonsiriseth, K. Prevalence and associated factors of musculoskeletal pain among the dental personnel in a dental school. J. Med Assoc. Thai. 2010, 93, 714–721. [Google Scholar] [PubMed]
- Finsen, L.; Christensen, H.; Bakke, M. Musculoskeletal disorders among dentists and variation in dental work. Appl. Ergon. 1998, 29, 119–125. [Google Scholar] [CrossRef]
- Golchha, V.; Sharma, P.; Wadhwa, J.; Yadav, D.; Paul, R. Ergonomic risk factors and their association with musculoskeletal disorders among Indian dentist: A preliminary study using Rapid Upper Limb Assessment. Indian J. Dent. Res. 2014, 25, 767–771. [Google Scholar] [CrossRef] [PubMed]
- Hayes, M.; Smith, D.R.; Cockrell, D. Prevalence and correlates of musculoskeletal disorders among Australian dental hygiene students. Int. J. Dent. Hyg. 2009, 7, 176–181. [Google Scholar] [CrossRef]
- Morse, T.; Bruneau, H.; Dussetschleger, J. Musculoskeletal disorders of the neck and shoulder in the dental professions. Work 2010, 35, 419–429. [Google Scholar] [CrossRef]
- Rafie, F.; Jam, A.Z.; Shahravan, A.; Raoof, M.; Eskandarizadeh, A. Prevalence of Upper Extremity Musculoskeletal Disorders in Dentists: Symptoms and Risk Factors. J. Environ. Public Health 2015, 2015, 1–6. [Google Scholar] [CrossRef]
- Baldisseri, M.R. Impaired healthcare professional. Crit. Care Med. 2007, 35, S106–S116. [Google Scholar] [CrossRef]
- Kenna, G.A.; Wood, M.D. The prevalence of alcohol, cigarette and illicit drug use and problems among dentists. J. Am. Dent. Assoc. 2005, 136, 1023–1032. [Google Scholar] [CrossRef] [PubMed]
- Ohlendorf, D.; Maltry, L.; Hänel, J.; Betz, W.; Erbe, C.; Maurer-Grubinger, C.; Holzgreve, F.; Wanke, E.M.; Brüggmann, D.; Nienhaus, A.; et al. SOPEZ: Study for the optimization of ergonomics in the dental practice—Musculoskeletal disorders in dentists and dental assistants: A study protocol. J. Occup. Med. Toxicol. 2020, 15, 1–9. [Google Scholar] [CrossRef]
- Haas, Y.; Naser, A.; Haenel, J.; Fraeulin, L.; Holzgreve, F.; Erbe, C.; Betz, W.; Wanke, E.M.; Brueggmann, D.; Nienhaus, A.; et al. Prevalence of self-reported musculoskeletal disorders of the hand and associated conducted therapy approaches among dentists and dental assistants in Germany. PLoS ONE 2020, 15, e0241564. [Google Scholar] [CrossRef]
- Caffier, G.; Steinberg, U.; Liebers, F. Praxisorientiertes Methodeninventar zur Belastungs-und Beanspruchungsbeurteilung im Zusammenhang mit Arbeitsbedingten Muskel-Skelett-Erkrankungen; Wirtschaftsverl: Frankfurt am Main, Germany, 1999. [Google Scholar]
- Kuorinka, I.; Jonsson, B.; Kilbom, A.; Vinterberg, H.; Biering-Sørensen, F.; Andersson, G.; Jørgensen, K. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl. Ergon. 1987, 18, 233–237. [Google Scholar] [CrossRef]
- Leiner, D.J. SoSci Survey (Version 3.1.06). München SoSci Surv. GmbH. 2019. Available online: https://www.soscisurvey.de (accessed on 28 July 2021).
- Corp, M. Microsoft Excel for Mac, Version 16. Redmond; Washington Microsoft Corp: Washington, DC, USA, 2019. [Google Scholar]
- Corp, I. IBM SPSS Statistics for Mac, Version 26; IBM Corp: Armonk, NY, USA, 2019. [Google Scholar]
- Artner, J.; Hofbauer, H.; Steffen, P.R.P. Zuordnung der Medikamente zu Substanzklassen. In Medikamente in der Schmerztherapie; Springer Science and Business Media LLC: Berlin/Heidelberg, Germany, 2020; pp. 49–51. [Google Scholar]
- Systemische Therapie (Stufenplan der WHO). Band 4: Schmerztherapie; Thieme: New York, NY, USA, 2002. [Google Scholar]
- Waldvogel, H.H. Analgetika, Antinozizeptiva, Adjuvantien. Handbuch für die Schmerzpraxis, 2nd ed.; Springer: Berlin/Heidelberg, Germany, 2001. [Google Scholar]
- Artner, J.; Hofbauer, H.; Steffen, P.R.P. Grundlagen der Pharmakotherapie. In Medikamente in der Schmerztherapie; Springer Science and Business Media LLC: Berlin/Heidelberg, Germany, 2020; pp. 41–47. [Google Scholar]
- Artner, J.; Hofbauer, H.; Steffen, P.R.P. Wirkmechanismen von Pharmaka. In Medikamente in der Schmerztherapie; Springer Science and Business Media LLC: Berlin/Heidelberg, Germany, 2020; pp. 17–40. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).