Effects of Simulated Gastric Acid Exposure on Surface Topography, Mechanical and Optical Features of Commercial CAD/CAM Ceramic Blocks
Abstract
:Featured Application
Abstract
1. Introduction
2. Materials and Methods
2.1. Specimens Preparation
2.2. Immersion of Ceramic Disks in Simulated Gastric Acid Solution
2.3. Investigation of Optical Parameters
2.4. Evaluation of Translucency Parameters
2.5. Microhardness Measurements
2.6. Surface Roughness Measurements
2.7. Scanning Electron Microscopy (SEM) and Energy Dispersive X-ray Spectroscopy (EDX) Analysis
2.8. Statistical Analysis
3. Results
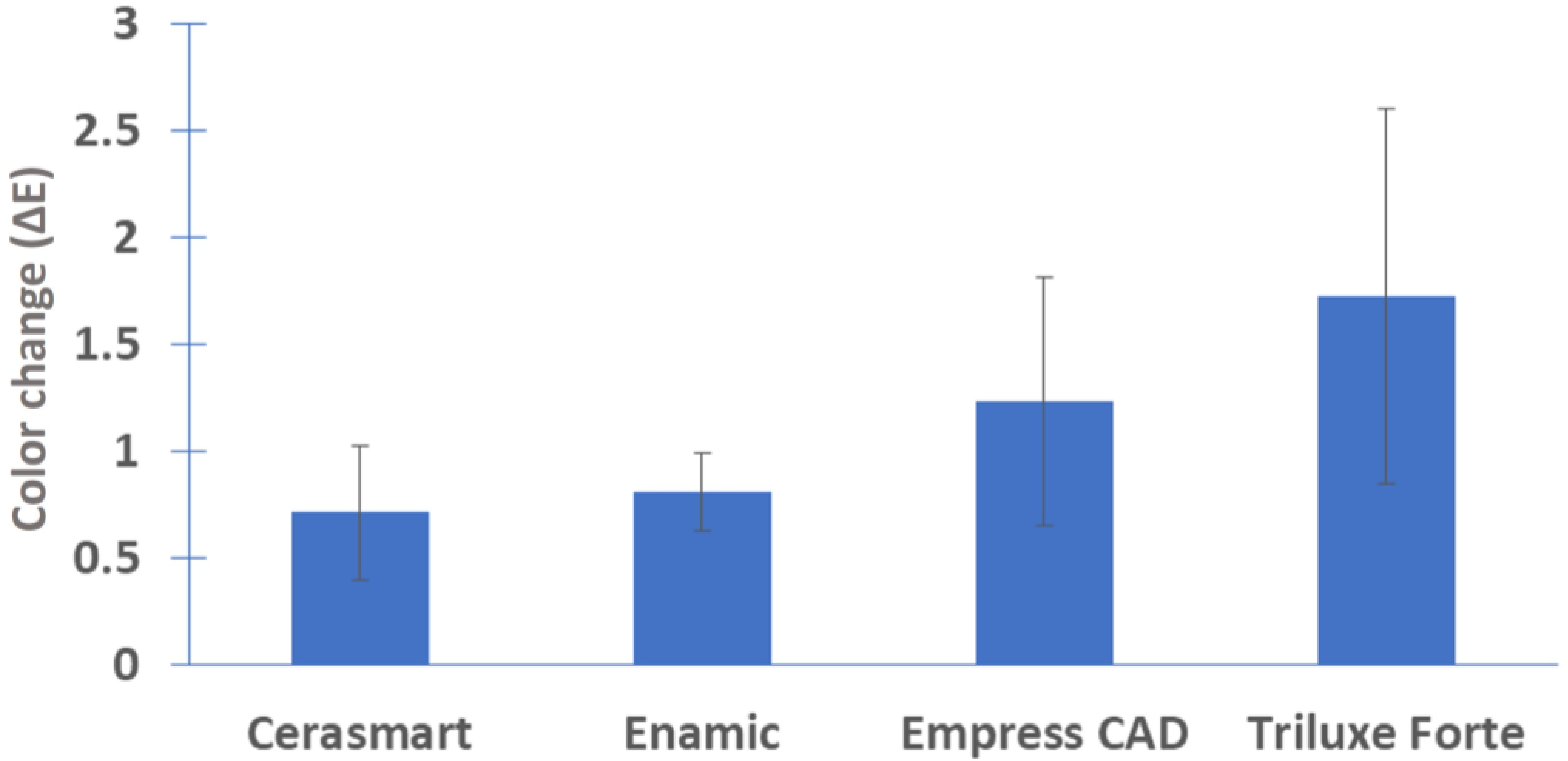
3.1. Optical Parameters
3.2. Translucency Parameters
3.3. Microhardness Test
3.4. Surface Roughness Results
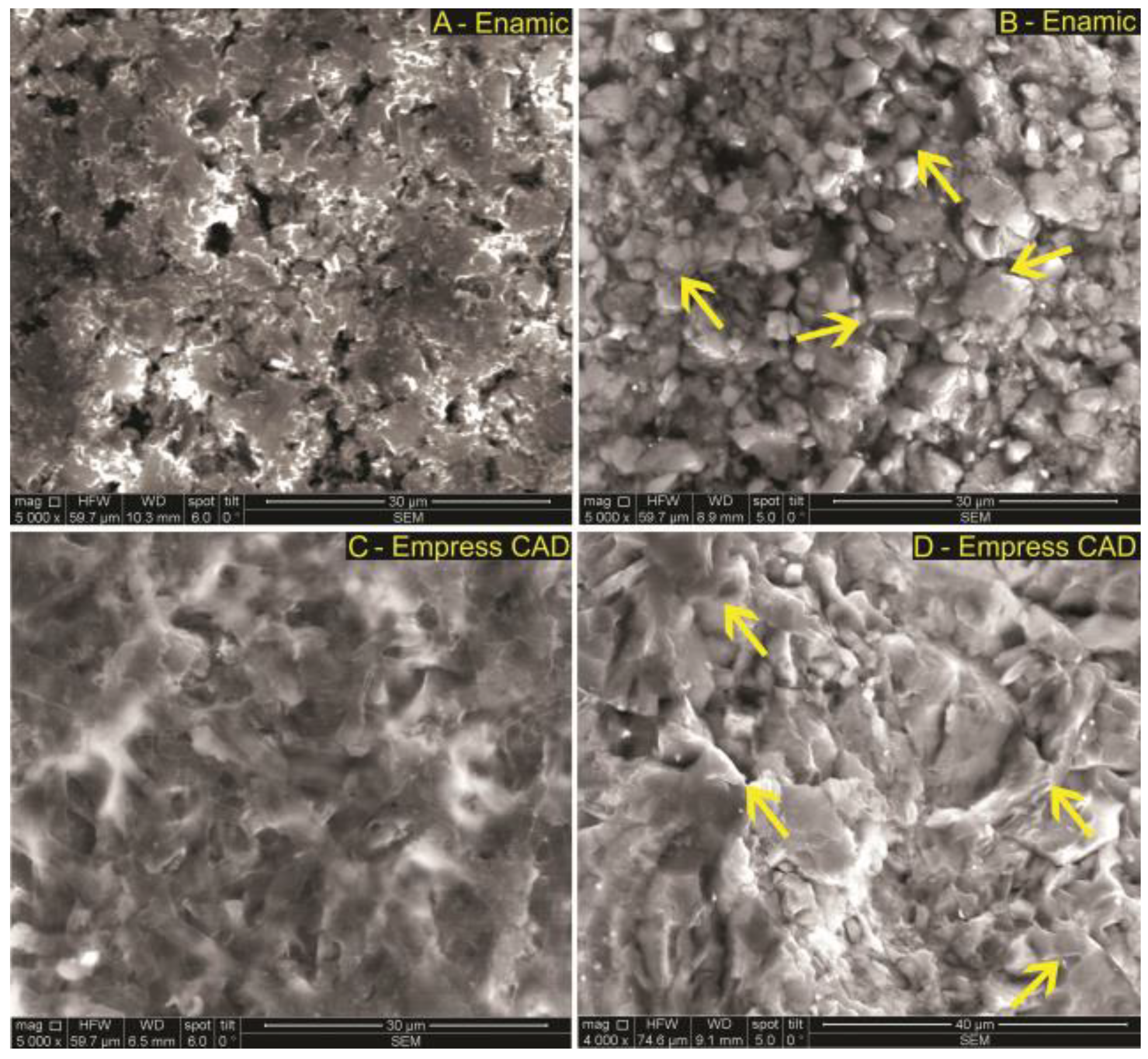
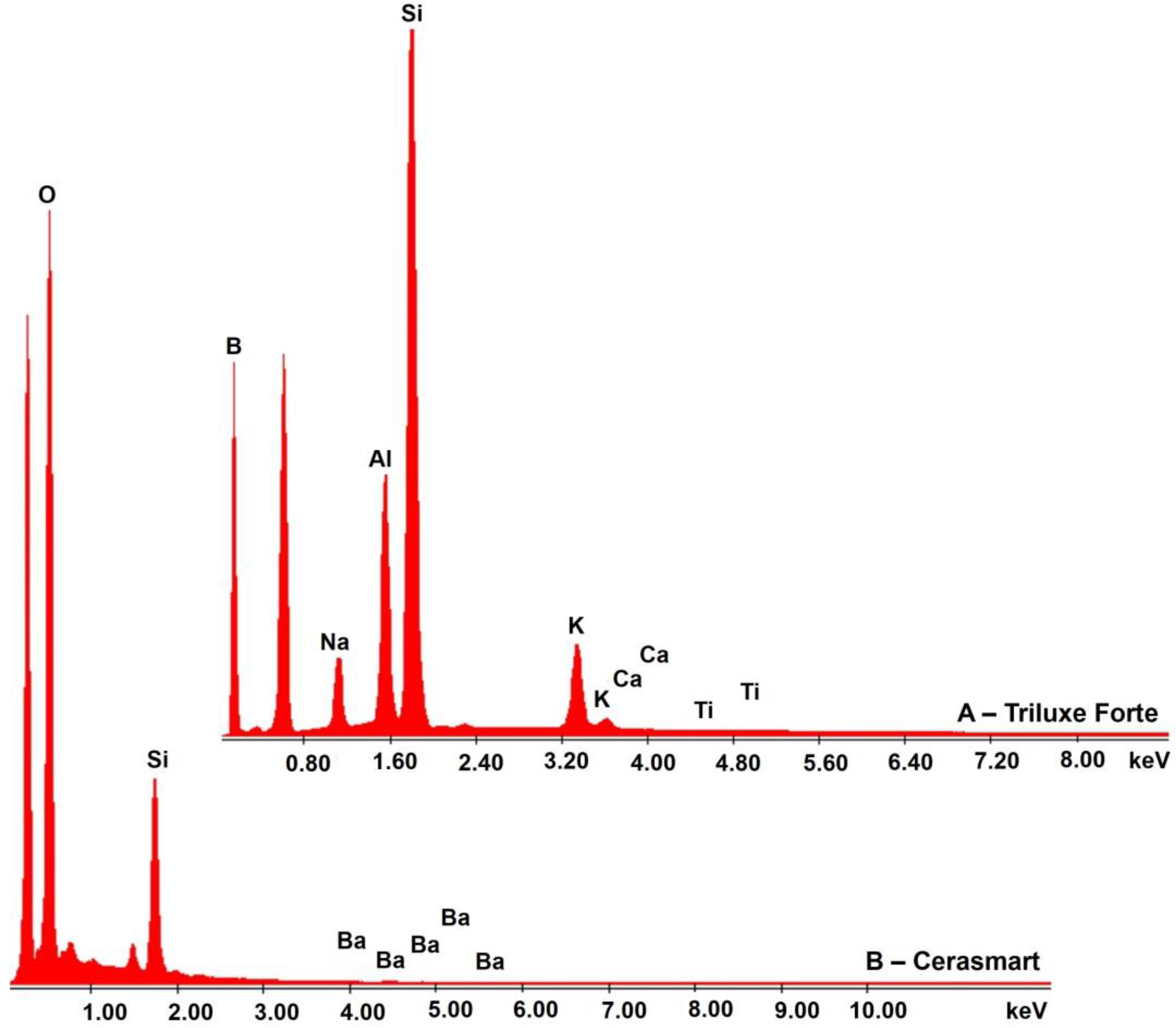
3.5. SEM-EDX Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Mörmann, W.H.; Stawarczyk, B.; Ender, A.; Sener, B.; Attin, T.; Mehl, A. Wear characteristics of current aesthetic dental restorative CAD/CAM materials: Two-body wear, gloss retention, roughness and Martens hardness. J. Mech. Behav. Biomed. Mater. 2013, 20, 113–125. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gracis, S.; Thompson, V.P.; Ferencz, J.L.; Silva, N.R.; Bonfante, E.A. A new classification system for all ceramic and ceramic-like restorative materials. Int. J. Prosthodont. 2015, 28, 227–235. [Google Scholar] [CrossRef] [Green Version]
- Traini, T.; Sinjari, B.; Pascetta, R.; Serafini, N.; Perfetti, G.; Trisi, P.; Caputi, S. The zirconia-reinforced lithium silicate ceramic: Lights and shadows of a new material. Dent. Mater. J. 2016, 35, 748–755. [Google Scholar] [CrossRef] [Green Version]
- Sato, T.P.; Anami, L.C.; Melo, R.M.; Valandro, L.F.; Bottino, M.A. Effects of Surface Treatments on the Bond Strength Between Resin Cement and a New Zirconia-reinforced Lithium Silicate Ceramic. Oper. Dent. 2016, 41, 284–292. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Elsaka, S.E.; Elnaghy, A.M. Mechanical properties of zirconia reinforced lithium silicate glass-ceramic. Dent. Mater. 2016, 32, 908–914. [Google Scholar] [CrossRef] [PubMed]
- Alves, L.M.M.; Contreras, L.P.C.; Campos, T.M.B.; Bottino, M.A.; Valandro, L.F.; Melo, R.M. In vitro wear of a zirconium-reinforced lithium silicate ceramic against different restorative materials. J. Mech. Behav. Biomed. Mater. 2019, 100, 103403. [Google Scholar] [CrossRef] [PubMed]
- Maenosono, R.M.; Brianezzi, L.F.F.; Ishikiriama, S.K.; Furuse, A.Y. Clinical perceptions of zirconia-reinforced lithium silicate ceramic: A case report and 6-month follow-up. Gen. Dent. 2019, 67, 47–50. [Google Scholar] [PubMed]
- Curtis, A.R.; Shortall, A.C.; Marquis, P.M.; Palin, W.M. Water uptake and strength characteristics of a nanofilled resin-based composite. J. Dent. 2008, 36, 186–193. [Google Scholar] [CrossRef]
- Kim, Y.S.; Kwon, H.K.; Kim, B.I. Effect of nano-carbonate apatite to prevent restain after dental bleaching in vitro. J. Dent. 2011, 39, 636–642. [Google Scholar] [CrossRef]
- Ernst, C.P.; Brandenbusch, M.; Meyer, G.; Canbek, K.; Gottschalk, F.; Willershausen, B. Two-year clinical performance of a nanofiller vs. a fine-particle hybrid resin composite. Clin. Oral Investig. 2006, 10, 119–125. [Google Scholar] [CrossRef]
- Sauro, S.; Osorio, R.; Watson, T.F.; Toledano, M. Therapeutic effects of novel resin bonding systems containing bioactive glasses on mineral-depleted areas within the bonded-dentine interface. J. Mater. Sci. Mater. Med. 2012, 23, 1521–1532. [Google Scholar] [CrossRef]
- De Fúcio, S.B.; Bolzan de Paula, A.; Galbiatti de Carvalho, F.; Pinheiro Feitosa, V.; Ambrosano, G.M.B.; Puppin-Rontani, R.M. Biomechanical degradation of the nano-filled resin-modified glass-ionomer surface. Am. J. Dent. 2012, 25, 315–320. [Google Scholar]
- Chen, C.; Trindade, F.Z.; de Jager, N.; Kleverlaan, C.J.; Feilzer, A.J. The fracture resistance of a CAD/CAM Resin Nano Ceramic (RNC) and a CAD ceramic at different thicknesses. Dent. Mater. 2014, 30, 954–962. [Google Scholar] [CrossRef] [PubMed]
- Alves, P.B.; Brandt, W.C.; Neves, A.C.; Gonçalves Cunha, L.; Silva-Concilio, L.R. Mechanical properties of direct and indirect composites after storage for 24 h and 10 months. Eur J. Dent. 2013, 7, 117–122. [Google Scholar] [PubMed]
- Belli, R.; Geinzer, E.; Muschweck, A.; Petschelt, A.; Lohbauer, U. Mechanical fatigue degradation of ceramics versus resin composites for dental restorations. Dent. Mater. 2014, 30, 424–432. [Google Scholar] [CrossRef] [PubMed]
- Sen, N.; Us, Y.O. Mechanical and optical properties of monolithic CAD-CAM restorative materials. J. Prosthet Dent. 2018, 119, 593–599. [Google Scholar] [CrossRef] [PubMed]
- Belli, R.; Wendler, M.; de Ligny, D.; Cicconi, M.R.; Petschelt, A.; Peterlik, H.; Lohbauer, U. Chairside CAD/CAM materials. Part 1: Measurement of elastic constants and microstructural characterization. Dent. Mater. 2017, 33, 84–98. [Google Scholar] [CrossRef] [PubMed]
- Lawson, N.C.; Bansal, R.; Burgess, J.O. Wear, strength, modulus and hardness of CAD/CAM restorative materials. Dent. Mater. 2016, 32, 275–283. [Google Scholar] [CrossRef]
- Albero, A.; Pascual, A.; Camps, I.; Grau-Benitez, M. Comparative characterization of a novel cad-cam polymer-infiltrated-ceramic-network. J. Clin. Exp. Dent. 2015, 7, 495–500. [Google Scholar] [CrossRef]
- Acar, O.; Yilmaz, B.; Altintas, S.H.; Chandrasekaran, I.; Johnston, W.M. Color stainability of CAD/CAM and nanocomposite resin materials. J. Prosthet. Dent. 2016, 115, 71–75. [Google Scholar] [CrossRef]
- Stawarczyk, B.; Liebermann, A.; Eichberger, M.; Güth, J.F. Evaluation of mechanical and optical behavior of current esthetic dental restorative CAD/CAM composites. J. Mech. Behav. Biomed. Mater. 2016, 55, 1–11. [Google Scholar] [CrossRef]
- Karakaya, I.; Cengiz, E. Effect of 2 bleaching agents with a content of high concentrated hydrogen peroxide on stained 2 CAD/CAM blocks and a nanohybrid composite resin: An AFM evaluation. Biomed. Res. Int. 2017, 2017, 6347145. [Google Scholar] [CrossRef] [Green Version]
- Jones, L.; Lekkas, D.; Hunt, D.; McIntyre, J.; Rafir, W. Studies on dental erosion: An in vivo-in vitro model of endogenous dental erosion—Its application to testing protection by fluoride gel application. Aust. Dent. J. 2002, 47, 304–308. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Turssi, C.P.; Hara, A.T.; de Magalhaes, C.S.; Campos Serra, M.; Rodrigues Jr, A.L. Influence of storage regime prior to abrasion on surface topography of restorative materials. J. Biomed. Mater. Res. B Appl. Biomater. 2003, 65, 227–232. [Google Scholar] [CrossRef] [PubMed]
- Yu, H.; Wegehaupt, F.J.; Wiegand, A.; Roos, M.; Attin, T.; Buchalla, W. Erosion and abrasion of tooth-colored restorative materials and human enamel. J. Dent. 2009, 37, 913–922. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matsou, E.; Vouroutzis, N.; Kontonasaki, E.; Paraskevopoulos, K.M.; Koidis, P. Investigation of the influence of gastric acid on the surface roughness of ceramic materials of metal-ceramic restorations. An in vitro study. Int. J. Prosthodont. 2011, 24, 26–29. [Google Scholar] [PubMed]
- Backer, A.D.; Münchow, E.A.; Eckert, G.J.; Hara, A.T.; Platt, J.A.; Bottino, M.C. Effects of simulated gastric juice on CAD/CAM resin composites-morphological and mechanical evaluations. J. Prosthodont. 2017, 26, 424–443. [Google Scholar] [CrossRef]
- Bartlett, D.W.; Coward, P.Y. Comparison of the erosive potential of gastric juice and a carbonated drink in vitro. J. Oral Rehabil. 2001, 28, 1045–1047. [Google Scholar] [CrossRef]
- Sulaiman, T.A.; Abdulmajeed, A.A.; Shahramian, K.; Hupa, L.; Donovan, T.E.; Vallittu, P.; Närhi, T.O. Impact of gastric acidic challenge on surface topography and optical properties of monolithic zirconia. Dent. Mater. 2015, 31, 1445–1452. [Google Scholar] [CrossRef]
- Cruz, M.E.M.; Simoes, R.; Martins, S.B.; Trinidade, F.Z.; Dovigo, L.N.; Fonseca, R.G. Influence of simulated gastric juice on surface characteristics of CAD-CAM monolithic materials. J. Prosthet Dent. 2020, 123, 483–490. [Google Scholar] [CrossRef]
- Harryparsad, A.; Dullabh, H.; Sykes, L.; Herbst, D. The effects of hydrochloric acid on all-ceramic restorative materials: An in-vitro study. SADJ 2014, 69, 106–111. [Google Scholar]
- Castillo, M.; Weiselberg, E. Bulimia nervosa/purging disorder. Curr. Probl. Pediatr. Adolesc. Health Care 2017, 47, 85–94. [Google Scholar] [CrossRef]
- Sengupta, A. Dental Erosion: Etiology, Diagnosis and Management. Acta Sci. Dent. Sci. 2018, 2, 43–48. [Google Scholar]
- Haq, M.W.; Batool, M.; Ahsan, S.H.; Lone, M.A.; Islam, T. Dental erosion: Influencing factors & pH analysis. Can. J. Appl. Sci. 2012, 2, 222–232. [Google Scholar]
- Zhang, J.; Du, Y.; Wei, Z.; Tai, B.; Jiang, H.; Du, M. The prevalence and risk indicators of tooth wear in 12- and 15-year-old adolescents in Central China. BMC Oral Health. 2015, 15, 120. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Theocharidou, A.; Kontonasaki, E.; Koukousaki, I.; Koumpouli, A.; Betsani, I.; Koidis, P. Effect of in vitro aging and acidic storage on color, translucency, and contrast ratio of monolithic zirconia and lithium disilicate ceramics. J. Prosthet. Dent. 2021, 3913, 30805–30815. [Google Scholar]
- Kulkarni, A.; Rothrock, J.; Thompson, J. Impact of Gastric Acid Induced Surface Changes on Mechanical Behavior and Optical Characteristics of Dental Ceramics. J. Prosthodont. 2020, 29, 207–218. [Google Scholar] [CrossRef] [PubMed]
- Egilmez, F.; Ergun, G.; Cekic-Nagas, I.; Vallittu, P.K.; Lassila, L.V.J. Does artificial aging affect mechanical properties of CAD/CAM composite materials. J. Prosthodont. Res. 2018, 62, 65–74. [Google Scholar] [CrossRef]
- Kaur, S.; Makkar, S.; Kumar, R.; Pasricha, S.; Gupta, P. Comparative evaluation of surface properties of enamel and different esthetic restorative materials under erosive and abrasive challenges: An in vitro study. Indian J. Dent. 2015, 6, 172–180. [Google Scholar]
- Zaki, D.Y.I.; Hamzawy, E.M.A.; El Halim, S.A.; Amer, M.A. Effect of simulated gastric juice on surface characteristics of direct esthetic restorations. Aust. J. Basic Appl. Sci. 2012, 6, 686–694. [Google Scholar]
- Cengiz, S.; Sarac, S.; Özcan, M. Effects of simulated gastric juice on color stability, surface roughness and microhardness of laboratory-processed composites. Dent. Mater. J. 2014, 33, 343–348. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bakar, W.Z.W.; McIntyre, J. Susceptibility of selected tooth-coloured dental materials to damage by common erosive acids. Aust. Dent. J. 2008, 53, 226–234. [Google Scholar] [CrossRef] [PubMed]
- de Carvalho Panzeri Pires-de-Souza, F.; Assirati Casemiro, L.; da Fonseca Roberti Garcia, L.; Rodrigues Cruvinel, D. Color stability of dental ceramics submitted to artificial accelerated aging after repeated firings. J. Prosthet. Dent. 2009, 101, 13–18. [Google Scholar] [CrossRef]
- Pires, L.A.; Novais, P.M.; Araújo, V.D.; Pegoraro, L.F. Effects of the type and thickness of ceramic, substrate, and cement on the optical color of a lithium disilicate ceramic. J. Prosthet Dent. 2017, 117, 144–149. [Google Scholar] [CrossRef] [PubMed]
- Salas, M.; Lucena, C.; Javier Herrera, L.; Yebra, A.; Della Bona, A.; Pérez, M.M. Translucency thresholds for dental materials. Dent. Mater. 2018, 34, 1168–1174. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Kelly, J.R. Dental Ceramics for Restoration and Metal Veneering. Dent. Clin. N. Am. 2017, 61, 797–819. [Google Scholar] [CrossRef]
- Choi, B.J.; Yoon, S.; Im, I.W.; Lee, J.H.; Jung, H.J.; Lee, H.H. Uniaxial/biaxial flexure strengths and elastic properties of resin-composite block materials for CAD/CAM. Dent. Mater. 2019, 35, 389–401. [Google Scholar] [CrossRef]
- Aldamaty, M.F.; Haggag, K.M.; Othman, H.I. Effect of simulated gastric acid on surface roughness of different monolithic ceramics. Al-Azhar J. Dent. Sci. 2020, 23, 327–334. [Google Scholar] [CrossRef]
- El-Serag, H.B.; Sweet, S.; Winchester, C.C.; Dent, J. Update on the epidemiology of gastro-oesophageal reflux disease: A systematic review. Gut 2014, 63, 871–880. [Google Scholar] [CrossRef]
- International Organization for Standardization. International Standards for Dental Ceramics; ISO 6872; International Organization for Standardization: Geneva, Switzerland, 1995. [Google Scholar]
- Carvalho Ramos, N.; Campos, T.M.; Paz, I.S.; Machado, J.P.; Bottino, M.A.; Cesar, P.F.; de Melo, R.M. Microstructure characterization and SCG of newly engineered dental ceramics. Dent. Mater. 2016, 32, 870–878. [Google Scholar] [CrossRef] [Green Version]
- Della Bona, A.; Nogueira, A.D.; Pecho, O.E. Optical properties of CAD-CAM ceramic systems. J. Dent. 2014, 42, 1202–1209. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sarac, D.; Sarac, Y.S.; Yuzbasioglu, E.; Bal, S. The effects of porcelain polishing systems on the color and surface texture of feldspathic porcelain. J. Prosthet. Dent. 2006, 96, 122–128. [Google Scholar] [CrossRef] [PubMed]
- Kukiattrakoon, B.; Hengtrakool, C.; Kedjarune-Leggat, U. Chemical durability and microhardness of dental ceramics immersed in acidic agents. Acta Odontol. Scand. 2010, 68, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Zakir, T.; Dandekeri, S.; Suhaim, K.S.; Shetty, N.H.G.; Ragher, M.; Shetty, S.K. Influence of aerated drink, mouthwash, and simulated gastric acid on the surface roughness of dental ceramics: A comparative in Vitro study. J. Pharm. Bioallied. Sci. 2020, 12, S480–S4871. [Google Scholar]




| Material | Classification | Composition | Manufacturer |
|---|---|---|---|
| Triluxe Forte | feldspathic ceramics | SiO2 56–64%; Al2O3 20–23%; Na2O 6–9%; K2O 6–8%; CaO 0.3–0.6%; TiO2 0.0–0.1% | VITA Zahnfabrik (Bad Säckingen, Germany) |
| Cerasmart | nanoceramic resin | 71% Silica and barium glass nanoparticles | GC Europe (Tokyo, Japan) |
| Enamic | hybrid ceramic with a dual network structure | SiO2 5–63%; Al2O3 20–23%; Na2O 6–11%; K2O 4–6%; B2O3 0.5–2%; CaO < 1%; TiO2 < 1% | VITA Zahnfabrik (Bad Säckingen, Germany) |
| Empress CAD | leucite-reinforced glass-ceramic | SiO2 60–65%; Al2O3 16–20%; K2O 10–14%; Na2O 3.5–6.5% | Ivoclar Vivadent (Zurich, Schwitzerland) |
| Cerasmart | Enamic | Empress CAD | Triluxe Forte | |
|---|---|---|---|---|
| After 18 h of exposure | 0.71 ± 0.3 | 0.81 ± 0.18 | 1.23 ± 0.58 | 1.72 ± 0.87 |
| Monolithic Material | Mean | Standard Deviation | ||
|---|---|---|---|---|
| Before | After | Before | After | |
| Cerasmart | 24.03 | 24.36 | 0.98 | 1.25 |
| Enamic | 21.26 | 21.76 | 3.06 | 2.72 |
| Empress CAD | 19.56 | 20.74 | 3.87 | 3.42 |
| Triluxe Forte | 19.51 | 18.43 | 2.19 | 2.11 |
| Material | Ra1 | Ra2 |
|---|---|---|
| Triluxe Forte | 0.81 ± 0.15 | 1.3 ± 0.08 |
| Cerasmart | 0.89 ± 0.06 | 0.92 ± 0.06 |
| Enamic | 0.92 ± 0.07 | 0.98 ± 0.08 |
| Empress CAD | 0.63 ± 0.07 | 0.72 ± 0.06 |
| Material | Element | At [%] | Wt [%] | K-Ratio |
|---|---|---|---|---|
| Triluxe Forte | B | 97.68 | 94.03 | 0.4133 |
| Na | 0.19 | 0.38 | 0.0021 | |
| Al | 0.46 | 1.11 | 0.0104 | |
| Si | 1.38 | 3.45 | 0.0360 | |
| K | 0.29 | 1.00 | 0.0107 | |
| Ca | 0.00 | 0.02 | 0.0002 | |
| Ti | 0.00 | 0.01 | 0.0001 | |
| Cerasmart | O | 91.01 | 85.22 | 0.4745 |
| Si | 8.99 | 14.77 | 0.0780 | |
| Ba | 0.00 | 0.01 | 0.0001 | |
| Enamic | B | 0.00 | 0.02 | 0.0001 |
| O | 55.27 | 41.53 | 0.1011 | |
| Na | 5.61 | 6.06 | 0.0168 | |
| Al | 9.91 | 12.57 | 0.0595 | |
| Si | 26.78 | 35.35 | 0.1612 | |
| K | 2.34 | 4.30 | 0.0288 | |
| Ca | 0.07 | 0.14 | 0.0010 | |
| Ti | 0.02 | 0.03 | 0.0003 | |
| Empress CAD | O | 60.52 | 46.55 | 0.1152 |
| Na | 4.40 | 4.86 | 0.0125 | |
| Al | 7.86 | 10.20 | 0.0469 | |
| Si | 24.11 | 32.56 | 0.1541 | |
| K | 3.11 | 5.84 | 0.0403 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pîrvulescu, I.L.; Pop, D.; Moacă, E.-A.; Mihali, C.-V.; Ille, C.; Jivănescu, A. Effects of Simulated Gastric Acid Exposure on Surface Topography, Mechanical and Optical Features of Commercial CAD/CAM Ceramic Blocks. Appl. Sci. 2021, 11, 8703. https://doi.org/10.3390/app11188703
Pîrvulescu IL, Pop D, Moacă E-A, Mihali C-V, Ille C, Jivănescu A. Effects of Simulated Gastric Acid Exposure on Surface Topography, Mechanical and Optical Features of Commercial CAD/CAM Ceramic Blocks. Applied Sciences. 2021; 11(18):8703. https://doi.org/10.3390/app11188703
Chicago/Turabian StylePîrvulescu, Ioana Ligia, Daniel Pop, Elena-Alina Moacă, Ciprian-Valentin Mihali, Codruța Ille, and Anca Jivănescu. 2021. "Effects of Simulated Gastric Acid Exposure on Surface Topography, Mechanical and Optical Features of Commercial CAD/CAM Ceramic Blocks" Applied Sciences 11, no. 18: 8703. https://doi.org/10.3390/app11188703
APA StylePîrvulescu, I. L., Pop, D., Moacă, E.-A., Mihali, C.-V., Ille, C., & Jivănescu, A. (2021). Effects of Simulated Gastric Acid Exposure on Surface Topography, Mechanical and Optical Features of Commercial CAD/CAM Ceramic Blocks. Applied Sciences, 11(18), 8703. https://doi.org/10.3390/app11188703







