Digital Procedures Compared to Conventional Gypsum Casts in the Manufacturing of CAD/CAM Adhesive Restorations: 3D Surface Trueness and Interfacial Adaptation Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample Teeth Selection and Preparation
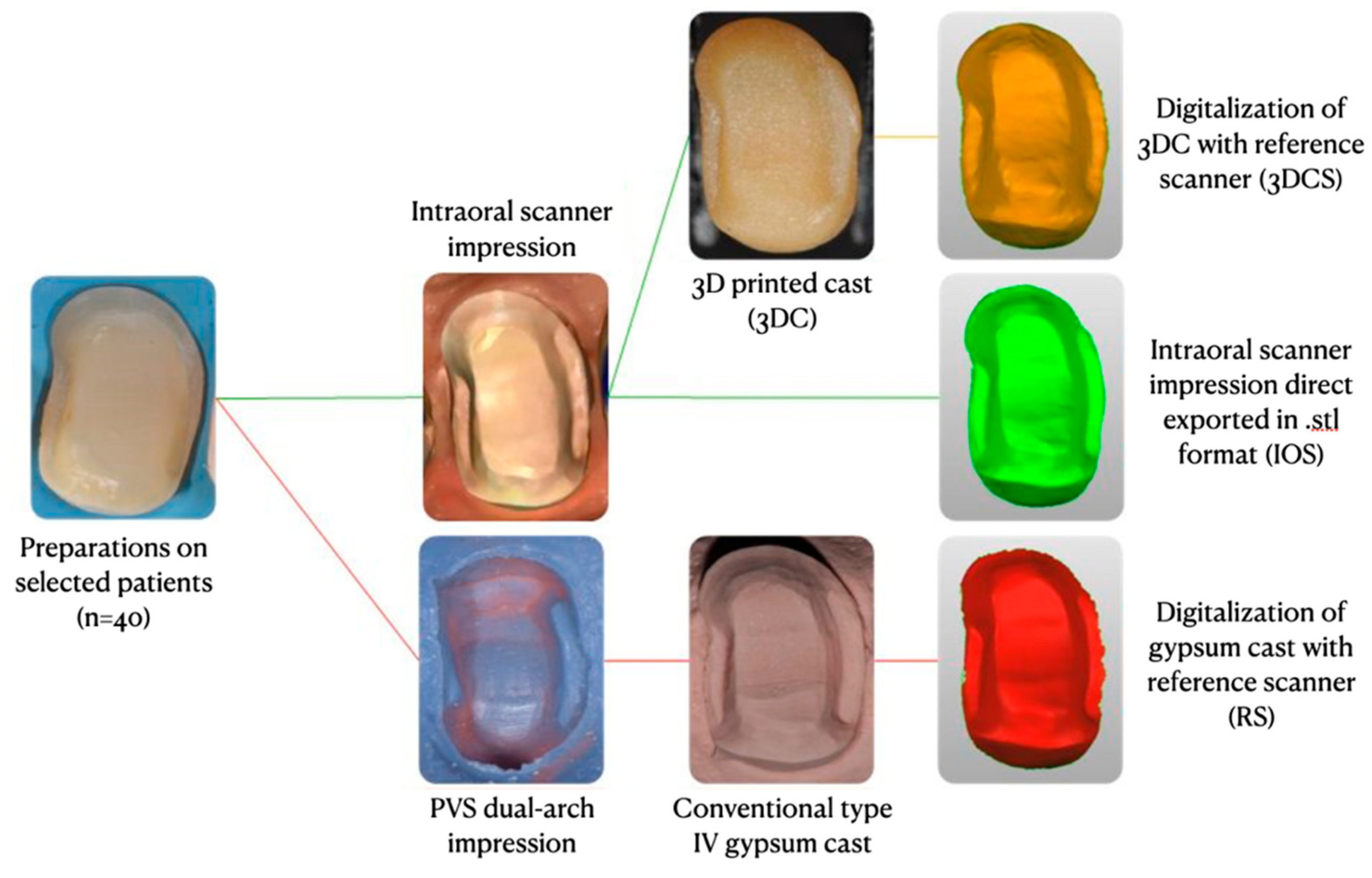
2.2. STL Files Setup
2.3. 3D Surface Trueness Analysis
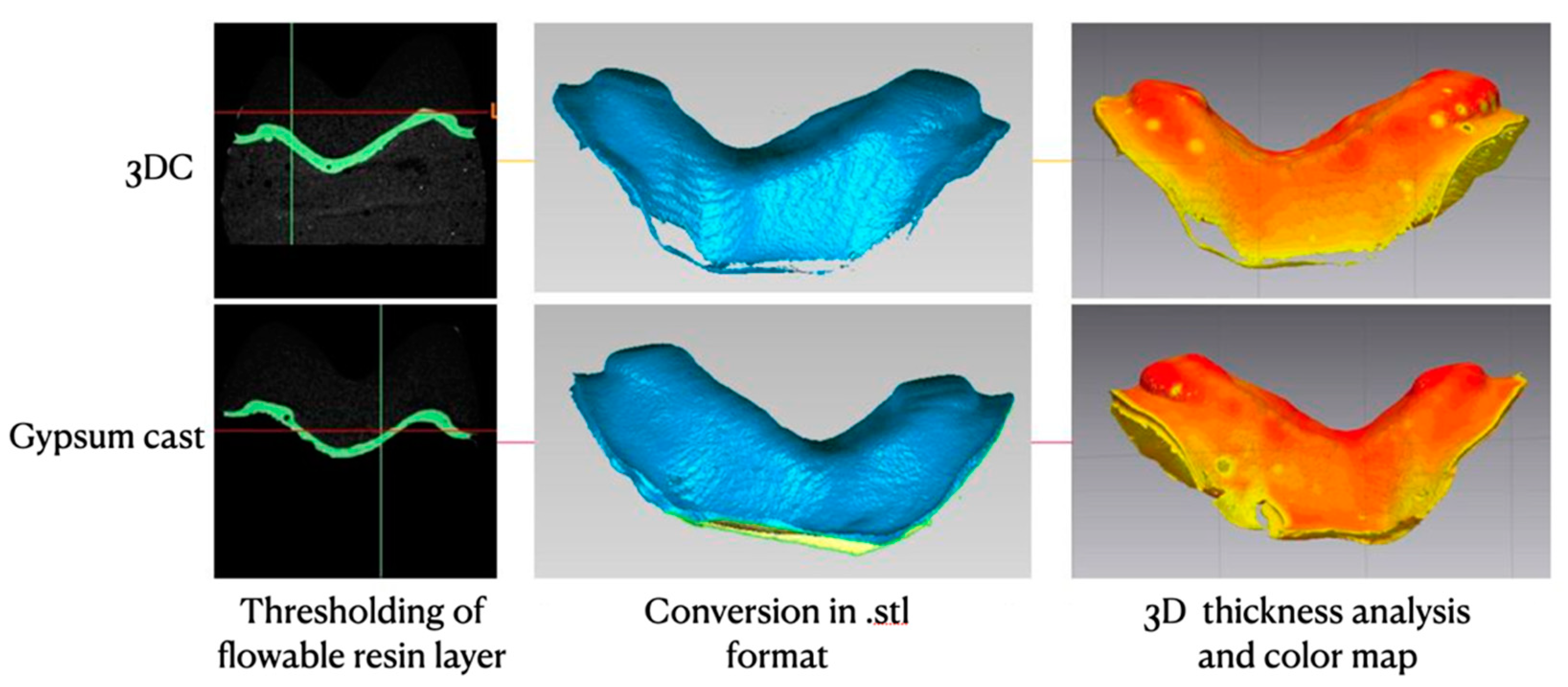
2.4. Interfacial Adaptation Evaluation
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Van Noort, R. The future of dental devices is digital. Dent. Mater. 2012, 28, 3–12. [Google Scholar] [CrossRef]
- Wittneben, J.-G.; Wright, R.F.; Weber, H.-P.; Gallucci, G.O. A systematic review of the clinical performance of CAD/CAM single-tooth restorations. Int. J. Prosthodont. 2009, 22, 466–471. [Google Scholar]
- Fasbinder, D.J. Computerized technology for restorative dentistry. Am. J. Dent. 2013, 26, 115–120. [Google Scholar]
- Revilla-León, M.; Olea-Vielba, M.; Esteso-Saiz, A.; Martínez-Klemm, I.; Özcan, M. Marginal and Internal Gap of Handmade, Milled and 3D Printed Additive Manufactured Patterns for Pressed Lithium Disilicate Onlay Restorations. Eur. J. Prosthodont. Restor. Dent. 2018, 26, 31–38. [Google Scholar] [CrossRef] [PubMed]
- Liu, Q.; Leu, M.C.; Schmitt, S.M. Rapid prototyping in dentistry: Technology and application. Int. J. Adv. Manuf. Technol. 2006, 29, 317–335. [Google Scholar] [CrossRef]
- Nedelcu, R.; Olsson, P.; Nyström, I.; Rydén, J.; Thor, A. Accuracy and precision of 3 intraoral scanners and accuracy of conventional impressions: A novel in vivo analysis method. J. Dent. 2018, 69, 110–118. [Google Scholar] [CrossRef]
- Kuhr, F.; Schmidt, A.; Rehmann, P.; Wöstmann, B. A new method for assessing the accuracy of full arch impressions in patients. J. Dent. 2016, 55, 68–74. [Google Scholar] [CrossRef]
- Hamalian, T.A.; Nasr, E.; Chidiac, J.J. Impression Materials in Fixed Prosthodontics: Influence of Choice on Clinical Procedure. J. Prosthodont. 2011, 20, 153–160. [Google Scholar] [CrossRef] [PubMed]
- Papadiochos, I.; Papadiochou, S.; Emmanouil, I. The Historical Evolution of Dental Impression Materials. J. Hist. Dent. 2017, 65, 79–89. [Google Scholar] [PubMed]
- Rudolph, H.; Graf, M.R.S.; Kuhn, K.; Rupf-Köhler, S.; Eirich, A.; Edelmann, C.; Quaas, S.; Luthardt, R.G. Performance of dental impression materials: Benchmarking of materials and techniques by three-dimensional analysis. Dent. Mater. J. 2015, 34, 572–584. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Barabanti, N.; Preti, A.; Vano, M.; Derchi, G.; Mangani, F.; Cerutti, A. Indirect composite restorations luted with two different procedures: A ten years follow up clinical trial. J. Clin. Exp. Dent. 2015, 7, e54–e59. [Google Scholar] [CrossRef] [PubMed]
- Abduo, J.; Sambrook, R.J. Longevity of ceramic onlays: A systematic review. J. Esthet. Restor. Dent. 2018, 30, 193–215. [Google Scholar] [CrossRef] [PubMed]
- Caputi, S.; Varvara, G. Dimensional accuracy of resultant casts made by a monophase, one-step and two-step, and a novel two-step putty/light-body impression technique: An in vitro study. J. Prosthet. Dent. 2008, 99, 274–281. [Google Scholar] [CrossRef]
- Christensen, G.J. The state of fixed prosthodontic impressions: Room for improvement. J. Am. Dent. Assoc. 2005, 136, 343–346. [Google Scholar] [CrossRef] [PubMed]
- Schepke, U.; Meijer, H.J.A.; Kerdijk, W.; Cune, M.S. Digital versus analog complete-arch impressions for single-unit premolar implant crowns: Operating time and patient preference. J. Prosthet. Dent. 2015, 114, 403–406.e1. [Google Scholar] [CrossRef]
- Haralur, S.B.; Toman, M.S.; Al-Shahrani, A.A.; Al-Qarni, A.A. Accuracy of Multiple Pour Cast from Various Elastomer Impression Methods. Int. J. Dent. 2016, 2016, 7414737. [Google Scholar] [CrossRef]
- Memari, Y.; Mohajerfar, M.; Armin, A.; Kamalian, F.; Rezayani, V.; Beyabanaki, E. Marginal Adaptation of CAD/CAM All-Ceramic Crowns Made by Different Impression Methods: A Literature Review. J. Prosthodont. Off. J. Am. Coll. Prosthodont. 2019, 28, e536–e544. [Google Scholar] [CrossRef]
- Patzelt, S.B.M.; Lamprinos, C.; Stampf, S.; Att, W. The time efficiency of intraoral scanners: An in vitro comparative study. J. Am. Dent. Assoc. 2014, 145, 542–551. [Google Scholar] [CrossRef]
- Abduo, J.; Elseyoufi, M. Accuracy of Intraoral Scanners: A Systematic Review of Influencing Factors. Eur. J. Prosthodont. Restor. Dent. 2018, 26, 101–121. [Google Scholar]
- Güth, J.-F.; Runkel, C.; Beuer, F.; Stimmelmayr, M.; Edelhoff, D.; Keul, C. Accuracy of five intraoral scanners compared to indirect digitalization. Clin. Oral Investig. 2017, 21, 1445–1455. [Google Scholar] [CrossRef]
- Ender, A.; Zimmermann, M.; Attin, T.; Mehl, A. In vivo precision of conventional and digital methods for obtaining quadrant dental impressions. Clin. Oral Investig. 2016, 20, 1495–1504. [Google Scholar] [CrossRef] [PubMed]
- Mangano, F.; Gandolfi, A.; Luongo, G.; Logozzo, S. Intraoral scanners in dentistry: A review of the current literature. BMC Oral Health 2017, 17, 149. [Google Scholar] [CrossRef]
- Ahlholm, P.; Sipilä, K.; Vallittu, P.; Jakonen, M.; Kotiranta, U. Digital Versus Conventional Impressions in Fixed Prosthodontics: A Review. J. Prosthodont. Off. J. Am. Coll. Prosthodont. 2018, 27, 35–41. [Google Scholar] [CrossRef] [PubMed]
- Berrendero, S.; Salido, M.P.; Ferreiroa, A.; Valverde, A.; Pradíes, G. Comparative study of all-ceramic crowns obtained from conventional and digital impressions: Clinical findings. Clin. Oral Investig. 2019, 23, 1745–1751. [Google Scholar] [CrossRef] [PubMed]
- Felton, D.A.; Kanoy, B.E.; Bayne, S.C.; Wirthman, G.P. Effect of in vivo crown margin discrepancies on periodontal health. J. Prosthet. Dent. 1991, 65, 357–364. [Google Scholar] [CrossRef]
- Lang, N.P.; Kiel, R.A.; Anderhalden, K. Clinical and microbiological effects of subgingival restorations with overhanging or clinically perfect margins. J. Clin. Periodontol. 1983, 10, 563–578. [Google Scholar] [CrossRef] [PubMed]
- Al-Imam, H.; Gram, M.; Benetti, A.R.; Gotfredsen, K. Accuracy of stereolithography additive casts used in a digital workflow. J. Prosthet. Dent. 2018, 119, 580–585. [Google Scholar] [CrossRef] [PubMed]
- Kasparova, M.; Grafova, L.; Dvorak, P.; Dostalova, T.; Prochazka, A.; Eliasova, H.; Prusa, J.; Kakawand, S. Possibility of reconstruction of dental plaster cast from 3D digital study models. Biomed. Eng. Online 2013, 12, 49. [Google Scholar] [CrossRef]
- Cho, S.-H.; Schaefer, O.; Thompson, G.A.; Guentsch, A. Comparison of accuracy and reproducibility of casts made by digital and conventional methods. J. Prosthet. Dent. 2015, 113, 310–315. [Google Scholar] [CrossRef] [PubMed]
- Kurz, M.; Attin, T.; Mehl, A. Influence of material surface on the scanning error of a powder-free 3D measuring system. Clin. Oral Investig. 2015, 19, 2035–2043. [Google Scholar] [CrossRef]
- Heshmati, R.H.; Nagy, W.W.; Wirth, C.G.; Dhuru, V.B. Delayed linear expansion of improved dental stone. J. Prosthet. Dent. 2002, 88, 26–31. [Google Scholar] [CrossRef] [PubMed]
- Gan, N.; Xiong, Y.; Jiao, T. Accuracy of Intraoral Digital Impressions for Whole Upper Jaws, Including Full Dentitions and Palatal Soft Tissues. PLoS ONE 2016, 11, e0158800. [Google Scholar] [CrossRef] [PubMed]
- Malik, J.; Rodriguez, J.; Weisbloom, M.; Petridis, H. Comparison of Accuracy Between a Conventional and Two Digital Intraoral Impression Techniques. Int. J. Prosthodont. 2018, 31, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Ender, A.; Attin, T.; Mehl, A. In vivo precision of conventional and digital methods of obtaining complete-arch dental impressions. J. Prosthet Dent. 2016, 115, 313–320. [Google Scholar] [CrossRef] [PubMed]
- Joda, T.; Zarone, F.; Ferrari, M. The complete digital workflow in fixed prosthodontics: A systematic review. BMC Oral Health 2017, 17, 124. [Google Scholar] [CrossRef]
- Pesce, P.; Pera, F.; Setti, P.; Menini, M. Precision and Accuracy of a Digital Impression Scanner in Full-Arch Implant Rehabilitation. Int. J. Prosthodont. 2018, 31, 171–175. [Google Scholar] [CrossRef]
- Rhee, Y.-K.; Huh, Y.-H.; Cho, L.-R.; Park, C.-J. Comparison of intraoral scanning and conventional impression techniques using 3-dimensional superimposition. J. Adv. Prosthodont. 2015, 7, 460–467. [Google Scholar] [CrossRef]
- Giachetti, L.; Sarti, C.; Cinelli, F.; Russo, D.S. Accuracy of Digital Impressions in Fixed Prosthodontics: A Systematic Review of Clinical Studies. Int. J. Prosthodont. 2020, 33, 192–201. [Google Scholar] [CrossRef]
- Contrepois, M.; Soenen, A.; Bartala, M.; Laviole, O. Marginal adaptation of ceramic crowns: A systematic review. J. Prosthet. Dent. 2013, 110, 447–454.e10. [Google Scholar] [CrossRef]
- Mostafa, N.Z.; Ruse, N.D.; Ford, N.L.; Carvalho, R.M.; Wyatt, C.C.L. Marginal Fit of Lithium Disilicate Crowns Fabricated Using Conventional and Digital Methodology: A Three-Dimensional Analysis. J. Prosthodont. 2018, 27, 145–152. [Google Scholar] [CrossRef] [PubMed]
- Seelbach, P.; Brueckel, C.; Wöstmann, B. Accuracy of digital and conventional impression techniques and workflow. Clin. Oral Investig. 2013, 17, 1759–1764. [Google Scholar] [CrossRef] [PubMed]
- Renne, W.; Wolf, B.; Kessler, R.; McPherson, K.; Mennito, A.S. Evaluation of the Marginal Fit of CAD/CAM Crowns Fabricated Using Two Different Chairside CAD/CAM Systems on Preparations of Varying Quality. J. Esthet. Restor. Dent. 2015, 27, 194–202. [Google Scholar] [CrossRef]
- Neves, F.D.; Prado, C.J.; Prudente, M.S.; Carneiro, T.A.; Zancopé, K.; Davi, L.R.; Mendonca, G.; Cooper, L.F.; Soares, C. Micro-computed tomography evaluation of marginal fit of lithium disilicate crowns fabricated by using chairside CAD/CAM systems or the heat-pressing technique. J. Prosthet. Dent. 2014, 112, 1134–1140. [Google Scholar] [CrossRef] [PubMed]
- Tsirogiannis, P.; Reissmann, D.R.; Heydecke, G. Evaluation of the marginal fit of single-unit, complete-coverage ceramic restorations fabricated after digital and conventional impressions: A systematic review and meta-analysis. J. Prosthet. Dent. 2016, 116, 328–335.e2. [Google Scholar] [CrossRef] [PubMed]
- Syrek, A.; Reich, G.; Ranftl, D.; Klein, C.; Cerny, B.; Brodesser, J. Clinical evaluation of all-ceramic crowns fabricated from intraoral digital impressions based on the principle of active wavefront sampling. J. Dent. 2010, 38, 553–559. [Google Scholar] [CrossRef]
- Koch, G.K.; Gallucci, G.O.; Lee, S.J. Accuracy in the digital workflow: From data acquisition to the digitally milled cast. J. Prosthet. Dent. 2016, 115, 749–754. [Google Scholar] [CrossRef]
- Flügge, T.V.; Schlager, S.; Nelson, K.; Nahles, S.; Metzger, M.C. Precision of intraoral digital dental impressions with iTero and extraoral digitization with the iTero and a model scanner. Am. J. Orthod. Dentofac. Orthop. 2013, 144, 471–478. [Google Scholar] [CrossRef]
- Tavarez, R.R.D.J.; Carvalhal, S.T.; Gomes, M.G.; Malheiros, A.S.; Gonçalves, L.M.; Filho, E.M.; Bandeca, M.C.; Patil, S. Assessment of a Synthetic Type IV Cast and a Resin Polyol Used in the Fabrication of Dental Models. J. Contemp Dent. Pr. 2016, 17, 160–164. [Google Scholar] [CrossRef]

| Cast | 3D Surface Trueness (µm) |
|---|---|
| IOS | 11.56 ± 8.13 |
| 3DCS | 17.01 ± 9.73 |
| Type of Cast | Marginal Adaptation (µm) | Internal Adaptation (µm) |
|---|---|---|
| Gypsum | 135.78 ± 30.85 | 212.31 ± 28.35 |
| 3DC | 57.63 ± 22.24 | 144.55 ± 24.95 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baldi, A.; Comba, A.; Vergano, E.A.; Vakalis, M.L.; Alovisi, M.; Pasqualini, D.; Ferrero, G.; Italia, E.; Tempesta, R.M.; Baldi, D.; et al. Digital Procedures Compared to Conventional Gypsum Casts in the Manufacturing of CAD/CAM Adhesive Restorations: 3D Surface Trueness and Interfacial Adaptation Analysis. Appl. Sci. 2021, 11, 5060. https://doi.org/10.3390/app11115060
Baldi A, Comba A, Vergano EA, Vakalis ML, Alovisi M, Pasqualini D, Ferrero G, Italia E, Tempesta RM, Baldi D, et al. Digital Procedures Compared to Conventional Gypsum Casts in the Manufacturing of CAD/CAM Adhesive Restorations: 3D Surface Trueness and Interfacial Adaptation Analysis. Applied Sciences. 2021; 11(11):5060. https://doi.org/10.3390/app11115060
Chicago/Turabian StyleBaldi, Andrea, Allegra Comba, Edoardo Alberto Vergano, Michail L. Vakalis, Mario Alovisi, Damiano Pasqualini, Giorgio Ferrero, Edoardo Italia, Riccardo Michelotto Tempesta, Domenico Baldi, and et al. 2021. "Digital Procedures Compared to Conventional Gypsum Casts in the Manufacturing of CAD/CAM Adhesive Restorations: 3D Surface Trueness and Interfacial Adaptation Analysis" Applied Sciences 11, no. 11: 5060. https://doi.org/10.3390/app11115060
APA StyleBaldi, A., Comba, A., Vergano, E. A., Vakalis, M. L., Alovisi, M., Pasqualini, D., Ferrero, G., Italia, E., Tempesta, R. M., Baldi, D., & Scotti, N. (2021). Digital Procedures Compared to Conventional Gypsum Casts in the Manufacturing of CAD/CAM Adhesive Restorations: 3D Surface Trueness and Interfacial Adaptation Analysis. Applied Sciences, 11(11), 5060. https://doi.org/10.3390/app11115060









