Surgical Repositioning of an Inverted Developing Incisor Assisted by 3D Technology
Abstract
:1. Introduction
2. Case Report
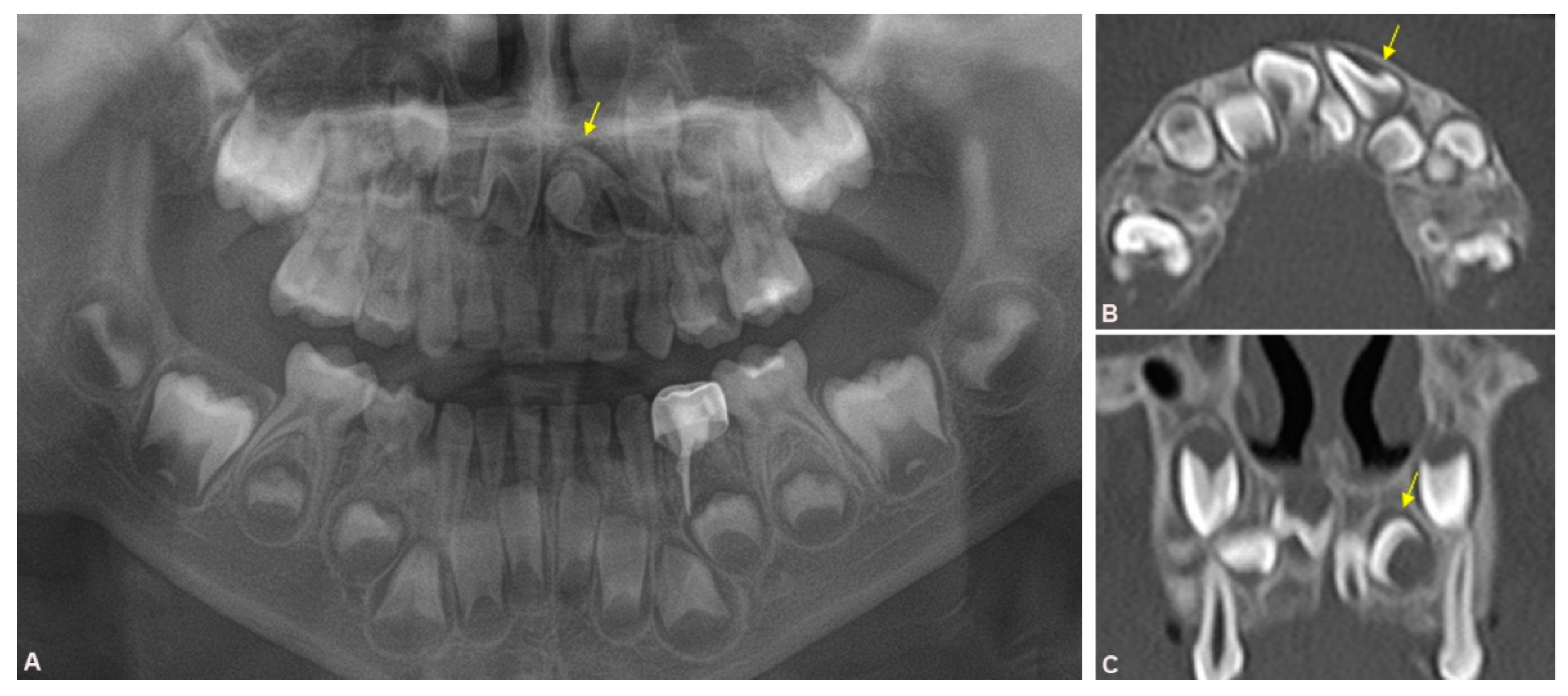
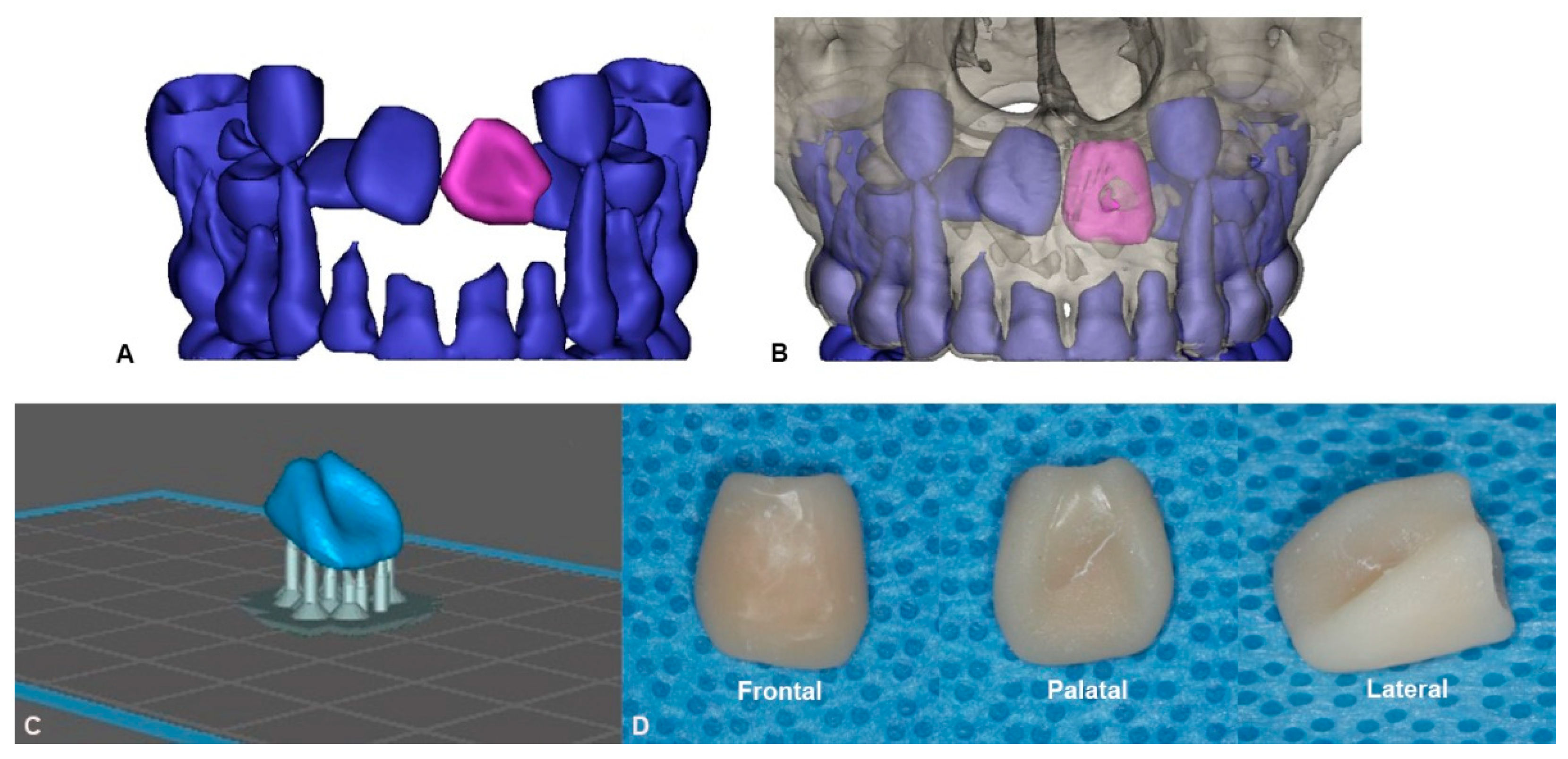
2.1. Preoperative Evaluation and Preparation
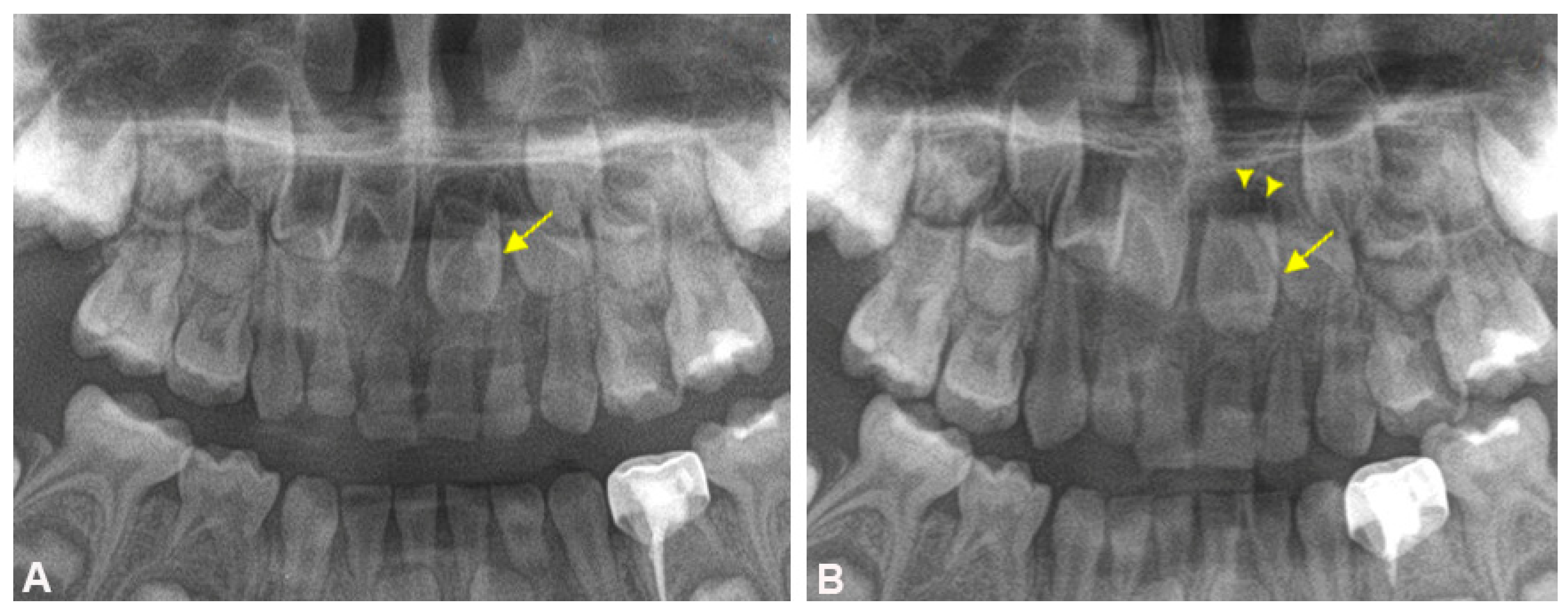
2.2. Surgical Procedure and Follow-up
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Grover, P.S.; Lorton, L. The incidence of unerupted permanent teeth and related clinical cases. Oral Surg. Oral Med. Oral Pathol. 1985, 59, 420–425. [Google Scholar] [CrossRef]
- Huber, K.L.; Suri, L.; Taneja, P. Eruption Disturbances of the Maxillary Incisors:A Literature Review. J. Clin. Pediatr. Dent. 2008, 32, 221–230. [Google Scholar] [CrossRef] [Green Version]
- Cozza, P.; Marino, A.; Ballanti, F. Orthodontic treatment of a patient with an unusual impaction of a central incisor: Case report. J. Dent. Child. 2003, 70, 174–177. [Google Scholar]
- Kuroe, K.; Tomonari, H.; Soejima, K.; Maeda, A. Surgical repositioning of a developing maxillary permanent central incisor in a horizontal position: Spontaneous eruption and root formation. Eur. J. Orthod. 2005, 28, 206–209. [Google Scholar] [CrossRef] [PubMed]
- Fllippi, A.; Pohl, Y.; Tekin, U. Transplantation of displaced and dilacerated anterior teeth. Dent. Traumatol. 1998, 14, 93–98. [Google Scholar] [CrossRef] [PubMed]
- McNamara, T.; Woolfe, S.N.; McNamara, C.M. Orthodontic management of a dilacerated maxillary central incisor with an unusual sequela. J. Clin. Orthod 1998, 32, 293–297. [Google Scholar] [PubMed]
- Tsai, T.P. Surgical repositioning of an impacted dilacerated incisor in mixed dentition. J. Am. Dent. Assoc. 2002, 133, 61–66. [Google Scholar] [CrossRef] [PubMed]
- Saad, A.Y.; Abdellatief, E.-S.M. Surgical repositioning of unerupted anterior teeth. J. Endod. 1996, 22, 376–379. [Google Scholar] [CrossRef]
- Dawood, A.; Marti Marti, B.; Sauret-Jackson, V.; Darwood, A. 3D printing in dentistry. Br. Dent. J. 2015, 219, 521–529. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Xu, C.; Zhang, Z. Flexible film separation analysis of LCD based mask stereolithography. J. Mater. Process. Technol. 2021, 288, 116916. [Google Scholar] [CrossRef]
- Quan, H.; Zhang, T.; Xu, H.; Luo, S.; Nie, J.; Zhu, X. Photo-curing 3D printing technique and its challenges. Bioact. Mater. 2020, 5, 110–115. [Google Scholar] [CrossRef]
- Chaushu, S.; Dykstein, N.; Ben-Bassat, Y.; Becker, A. Periodontal Status of Impacted Maxillary Incisors Uncovered by 2 Different Surgical Techniques. J. Oral Maxillofac. Surg. 2009, 67, 120–124. [Google Scholar] [CrossRef]
- Alberto, P.L. Surgical Exposure of Impacted Teeth. Oral Maxillofac. Surg. Clin. N. Am. 2020, 32, 561–570. [Google Scholar] [CrossRef]
- Plakwicz, P.; Kapuścińska, A.; Kukuła, K.; Czochrowska, E.M. Pulp Revascularization after Repositioning of Impacted Incisor with a Dilacerated Root and a Detached Apex. J. Endod. 2015, 41, 974–979. [Google Scholar] [CrossRef] [PubMed]
- Topouzelis, N.; Tsaousoglou, P.; Gofa, A. Management of root dilaceration of an impacted maxillary central incisor following orthodontic treatment: An unusual therapeutic outcome. Dent. Traumatol. 2010, 26, 521–526. [Google Scholar] [CrossRef] [PubMed]
- Sun, H.; Hu, R.; Ren, M.; Lin, Y.; Wang, X.; Sun, C.; Wang, Y. The treatment timing of labial inversely impacted maxillary central incisors: A prospective study. Angle Orthod. 2016, 86, 768–774. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, S.; Kim, J.; Song, J.S.; Choi, H.-J.; Choi, B.-J.; Kim, S.-O. Continued root development of a surgically repositioned human incisor tooth germ. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2013, 115, e11–e15. [Google Scholar] [CrossRef] [PubMed]
- Khorsandi, D.; Fahimipour, A.; Abasian, P.; Saber, S.S.; Seyedi, M.; Ghanavati, S.; Ahmad, A.; De Stephanis, A.A.; Taghavinezhaddilami, F.; Leonova, A.; et al. 3D and 4D printing in dentistry and maxillofacial surgery: Printing techniques, materials, and applications. Acta Biomater. 2021, 122, 26–49. [Google Scholar] [CrossRef] [PubMed]

| Pre-op | Post-op | |
|---|---|---|
| Location of tooth | Inverted (malpositioned) | Forward (normal position) |
| Expectation for self eruption | Impossible | Possible |
| Related pathology | Possible | Expected not to occur during eruption |
| Root development | May be disturbed | Showed normal development |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seo, M.-H.; Yang, H.-J.; Han, J.-J.; Kwon, I.-J.; Myoung, H.; Kim, S.-M. Surgical Repositioning of an Inverted Developing Incisor Assisted by 3D Technology. Appl. Sci. 2021, 11, 4827. https://doi.org/10.3390/app11114827
Seo M-H, Yang H-J, Han J-J, Kwon I-J, Myoung H, Kim S-M. Surgical Repositioning of an Inverted Developing Incisor Assisted by 3D Technology. Applied Sciences. 2021; 11(11):4827. https://doi.org/10.3390/app11114827
Chicago/Turabian StyleSeo, Mi-Hyun, Hoon-Joo Yang, Jeong-Joon Han, Ik-Jae Kwon, Hoon Myoung, and Soung-Min Kim. 2021. "Surgical Repositioning of an Inverted Developing Incisor Assisted by 3D Technology" Applied Sciences 11, no. 11: 4827. https://doi.org/10.3390/app11114827
APA StyleSeo, M.-H., Yang, H.-J., Han, J.-J., Kwon, I.-J., Myoung, H., & Kim, S.-M. (2021). Surgical Repositioning of an Inverted Developing Incisor Assisted by 3D Technology. Applied Sciences, 11(11), 4827. https://doi.org/10.3390/app11114827







