Why Determining the Native Length Change Pattern of Medial Patellofemoral Ligament Is Still a Challenge: State-of-the-Art Review of Potential Sources of Heterogeneity within Studies Evaluating Isometry of MPFL
Abstract
1. Introduction
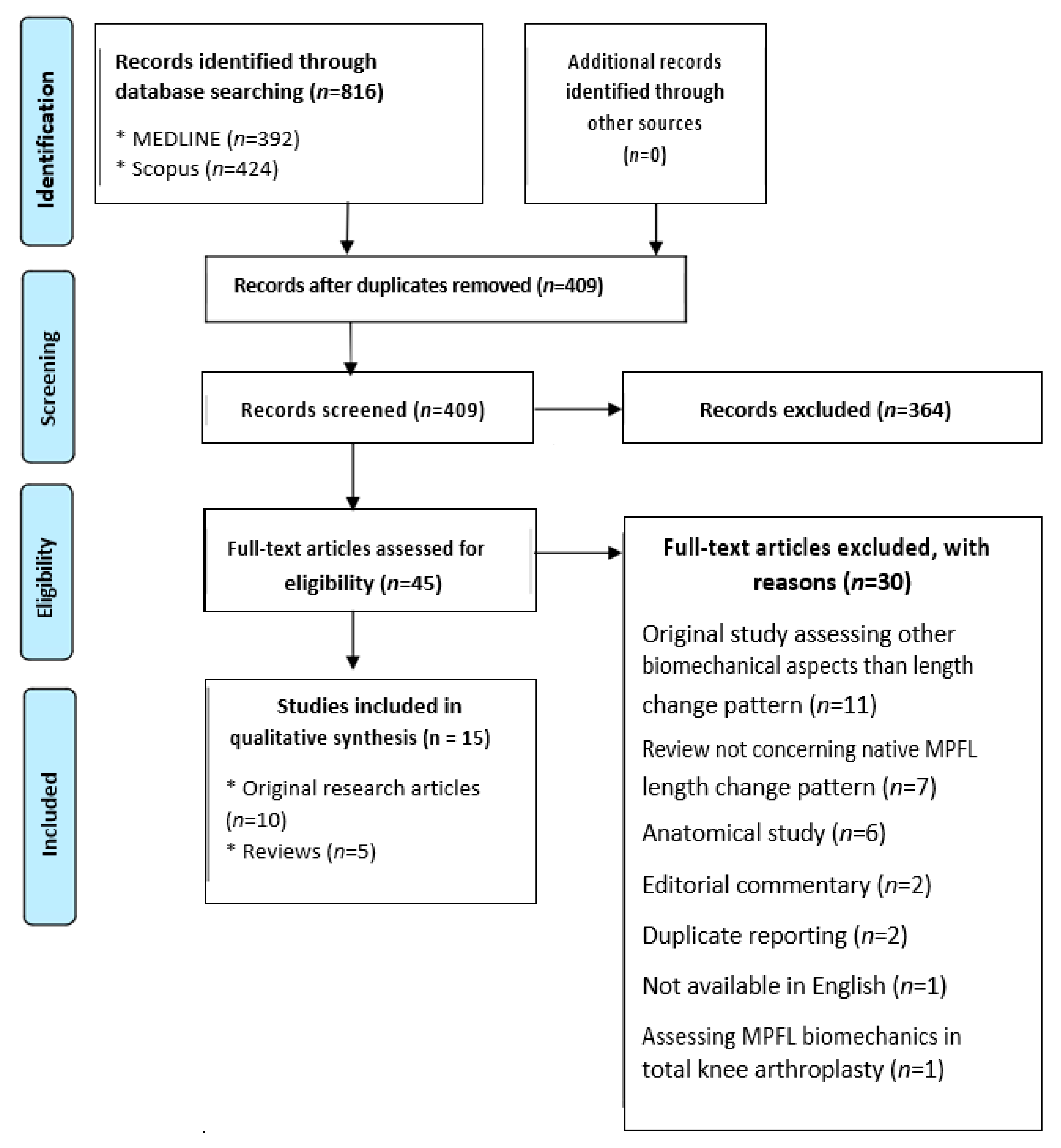
2. Materials and Methods
2.1. Search Methods and Exclusion Criteria
2.2. Results of the Query
2.3. Data Extraction Process
- (1)
- Demographics: age, number of patients/cadavers, male to female ratio.
- (2)
- Study design:
- (a)
- How was measured fibers identified? How was MPFL length measured and what was the precision of measurements (3D vs. 2D; magnetic resonance imaging [MRI] vs. computed tomography [CT] vs. caliper vs. suture vs. other; straight line vs. convex line; precision in mm)?
- (b)
- What was the activity of quadriceps muscle, iliotibial band (ITB), and hamstrings (in study assessing patients: contracted/resting/not contracted; in study assessing cadavers: simulated/simulation of resting tension/not simulated)?
- (3)
- Morphology of patellofemoral joints:
- (a)
- What was the patellar height (reported vs. not reported; if reported, normal vs. stratified vs. abnormal)?
- (b)
- Whether there was trochlear or patellar dysplasia (as above).
- (c)
- Femoral anteversion (as above).
- (d)
- Mechanical axis of the limb (as above).
- (e)
- Tibial tubercle–trochlear groove (TT–TG) distance (as above).
- (f)
- Condylar anteroposterior dimensions (as above).
2.4. Summarizing the Extracted Data
3. Demographics as the Source of Heterogeneity
4. Study Design as the Source of Heterogeneity
4.1. Identification of Measured Fibers and Measurement Methods
4.2. Muscular Activity
5. Morphology of Participants’ Patellofemoral Joints as the Source of Heterogeneity
6. Summary of the Review
7. Limitations
8. Considerations for Future Research
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Panagiotopoulos, E.; Strzelczyk, P.; Herrmann, M.; Scuderi, G. Cadaveric study on static medial patellar stabilizers: The dynamizing role of the vastus medialis obliquus on medial patellofemoral ligament. Knee Surg. Sports Traumatol. Arthrosc. 2006, 14, 7–12. [Google Scholar] [CrossRef] [PubMed]
- Conlan, T.P.; Garth, W.; Lemons, J.E. Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J. Bone Jt. Surg. Am. 1993, 75, 682–693. [Google Scholar] [CrossRef]
- Desio, S.M.; Burks, R.T.; Bachus, K.N. Soft Tissue Restraints to Lateral Patellar Translation in the Human Knee. Am. J. Sports Med. 1998, 26, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Hautamaa, P.V.; Fithian, D.C.; Kaufman, K.R.; Daniel, D.M.; Pohlmeyer, A.M. Medial Soft Tissue Restraints in Lateral Patellar Instability and Repair. Clin. Orthop. Relat. Res. 1998, 349, 174–182. [Google Scholar] [CrossRef] [PubMed]
- Atkin, D.M.; Fithian, D.C.; Marangi, K.S.; Stone, M.L.; Dobson, B.E.; Mendelsohn, C. Characteristics of Patients with Primary Acute Lateral Patellar Dislocation and Their Recovery within the First 6 Months of Injury. Am. J. Sports Med. 2000, 28, 472–479. [Google Scholar] [CrossRef] [PubMed]
- Criscenti, G.; De Maria, C.; Sebastiani, E.; Tei, M.; Placella, G.; Speziali, A.; Vozzi, G.; Cerulli, G. Material and structural tensile properties of the human medial patello-femoral ligament. J. Mech. Behav. Biomed. Mater. 2016, 54, 141–148. [Google Scholar] [CrossRef] [PubMed]
- Higuchi, T.; Arai, Y.; Takamiya, H.; Miyamoto, T.; Tokunaga, D.; Kubo, T. An analysis of the medial patellofemoral ligament length change pattern using open-MRI. Knee Surg. Sports Traumatol. Arthrosc. 2010, 18, 1470–1475. [Google Scholar] [CrossRef]
- Mochizuki, T.; Nimura, A.; Tateishi, T.; Yamaguchi, K.; Muneta, T.; Akita, K. Anatomic study of the attachment of the medial patellofemoral ligament and its characteristic relationships to the vastus intermedius. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 305–310. [Google Scholar] [CrossRef]
- Blatter, S.C.; Fürnstahl, P.; Hirschmann, A.; Graf, M.; Fucentese, S.F. Femoral insertion site in medial patellofemoral ligament reconstruction. Knee 2016, 23, 456–459. [Google Scholar] [CrossRef]
- Gobbi, R.G.; Pereira, C.A.M.; Sadigursky, D.; Demange, M.K.; Tírico, L.E.P.; Pécora, J.R.; Camanho, G.L. Evaluation of the isometry of different points of the patella and femur for medial patellofemoral ligament reconstruction. Clin. Biomech. 2016, 38, 8–12. [Google Scholar] [CrossRef]
- Sanchis-Alfonso, V.; Ramirez-Fuentes, C.; Montesinos-Berry, E.; Domenech, J.; Martí-Bonmatí, L. Femoral insertion site of the graft used to replace the medial patellofemoral ligament influences the ligament dynamic changes during knee flexion and the clinical outcome. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 2433–2441. [Google Scholar] [CrossRef]
- Farr, J.; Schepsis, A.A. Reconstruction of the medial patellofemoral ligament for recurrent patellar instability. J. Knee Surg. 2006, 19, 307–316. [Google Scholar] [CrossRef] [PubMed]
- Redler, L.H.; Meyers, K.N.; Brady, J.M.; Dennis, E.R.; Nguyen, J.T.; Stein, B.E.S. Anisometry of Medial Patellofemoral Ligament Reconstruction in the Setting of Increased Tibial Tubercle–Trochlear Groove Distance and Patella Alta. Arthrosc. J. Arthrosc. Relat. Surg. 2018, 34, 502–510. [Google Scholar] [CrossRef]
- Kernkamp, W.A.; Wang, C.; Li, C.; Hu, H.; van Arkel, E.R.; Nelissen, R.; LaPrade, R.F.; van de Velde, S.K.; Tsai, T.-Y. The Medial Patellofemoral Ligament Is a Dynamic and Anisometric Structure: An In Vivo Study on Length Changes and Isometry. Am. J. Sports Med. 2019, 47, 1645–1653. [Google Scholar] [CrossRef]
- Chahla, J.; Smigielski, R.; Laprade, R.F.; Fulkerson, J.P. An Updated Overview of the Anatomy and Function of the Proximal Medial Patellar Restraints (Medial Patellofemoral Ligament and the Medial Quadriceps Tendon Femoral Ligament). Sports Med. Arthrosc. Rev. 2019, 27, 136–142. [Google Scholar] [CrossRef] [PubMed]
- Huber, C.; Zhang, Q.; Taylor, W.R.; Amis, A.A.; Smith, C.; Nasab, S.H.H. Properties and Function of the Medial Patellofemoral Ligament: A Systematic Review. Am. J. Sports Med. 2020, 48, 754–766. [Google Scholar] [CrossRef]
- Amis, A.A.; Firer, P.; Mountney, J.; Senavongse, W.; Thomas, N.P. Anatomy and biomechanics of the medial patellofemoral ligament. Knee 2003, 10, 215–220. [Google Scholar] [CrossRef]
- Bicos, J.; Fulkerson, J.P.; Amis, A. Current Concepts Review: The Medial Patellofemoral Ligament. Am. J. Sports Med. 2007, 35, 484–492. [Google Scholar] [CrossRef] [PubMed]
- Grant, M.J.; Booth, A. A typology of reviews: An analysis of 14 review types and associated methodologies. Health Inf. Libr. J. 2009, 26, 91–108. [Google Scholar] [CrossRef] [PubMed]
- Woo, S.L.-Y.; Hollis, J.M.; Adams, D.J.; Lyon, R.M.; Takai, S. Tensile properties of the human femur-anterior cruciate ligament-tibia complex. The effects of specimen age and orientation. Am. J. Sports Med. 1991, 19, 217–225. [Google Scholar] [CrossRef] [PubMed]
- Steensen, R.N.; Dopirak, R.M.; McDonald, W.G. The Anatomy and Isometry of Themedial Patellofemoral Ligament. Am. J. Sports Med. 2004, 32, 1509–1513. [Google Scholar] [CrossRef] [PubMed]
- Victor, J.; Wong, P.; Witvrouw, E.; Sloten, J.V.; Bellemans, J. How Isometric Are the Medial Patellofemoral, Superficial Medial Collateral, and Lateral Collateral Ligaments of the Knee? Am. J. Sports Med. 2009, 37, 2028–2036. [Google Scholar] [CrossRef]
- Stephen, J.M.; Kader, D.; Lumpaopong, P.; Deehan, D.J.; Amis, A.A. Sectioning the medial patellofemoral ligament alters patellofemoral joint kinematics and contact mechanics. J. Orthop. Res. 2013, 31, 1423–1429. [Google Scholar] [CrossRef] [PubMed]
- Graf, M.; Diether, S.; Vlachopoulos, L.; Fucentese, S.; Fürnstahl, P. Automatic string generation for estimating in vivo length changes of the medial patellofemoral ligament during knee flexion. Med. Biol. Eng. Comput. 2014, 52, 511–520. [Google Scholar] [CrossRef] [PubMed]
- Song, S.Y.; Pang, C.-H.; Kim, C.H.; Kim, J.; Choi, M.L.; Seo, Y.-J. Length Change Behavior of Virtual Medial Patellofemoral Ligament Fibers During In Vivo Knee Flexion. Am. J. Sports Med. 2015, 43, 1165–1171. [Google Scholar] [CrossRef]
- Decante, C.; Geffroy, L.; Salaud, C.; Chalopin, A.; Ploteau, S.; Hamel, A. Descriptive and dynamic study of the medial patellofemoral ligament (MPFL). Surg. Radiol. Anat. 2019, 41, 763–774. [Google Scholar] [CrossRef] [PubMed]
- Huddleston, H.P.; Campbell, K.J.; Madden, B.T.; Christian, D.R.; Chahla, J.; Farr, J.; Cole, B.J.; Yanke, A.B. The quadriceps insertion of the medial patellofemoral complex demonstrates the greatest anisometry through flexion. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 757–763. [Google Scholar] [CrossRef]
- Yanke, A.B.; Huddleston, H.P.; Campbell, K.; Redondo, M.L.; Espinoza, A.; Chahla, J.; Cole, B.J.; Farr, J. Effect of Patella Alta on the Native Anatomometricity of the Medial Patellofemoral Complex: A Cadaveric Study. Am. J. Sports Med. 2020, 48, 1398–1405. [Google Scholar] [CrossRef]
- Zaffagnini, S.; DeJour, D.; Grassi, A.; Bonanzinga, T.; Muccioli, G.M.M.; Colle, F.; Raggi, F.; Benzi, A.; Marcacci, M. Patellofemoral anatomy and biomechanics: Current concepts. Joints 2013, 1, 15–20. [Google Scholar] [CrossRef]
- Kaiser, J.M.; Vignos, M.F.; Kijowski, R.; Baer, G.; Thelen, D.G. Effect of Loading on In Vivo Tibiofemoral and Patellofemoral Kinematics of Healthy and ACL-Reconstructed Knees. Am. J. Sports Med. 2017, 45, 3272–3279. [Google Scholar] [CrossRef]
- Edmonds, E.W.; Glaser, D.A. Adolescent Patella Instability Extensor Mechanics. J. Pediatr. Orthop. 2015, 36, 262–267. [Google Scholar] [CrossRef]
- Flandry, F.; Hommel, G. Normal Anatomy and Biomechanics of the Knee. Sports Med. Arthrosc. Rev. 2011, 19, 82–92. [Google Scholar] [CrossRef] [PubMed]
- Fairclough, J.; Hayashi, K.; Toumi, H.; Lyons, K.; Bydder, G.; Phillips, N.; Best, T.M.; Benjamin, M. The functional anatomy of the iliotibial band during flexion and extension of the knee: Implications for understanding iliotibial band syndrome. J. Anat. 2006, 208, 309–316. [Google Scholar] [CrossRef] [PubMed]
- Arai, Y.; Nakagawa, S.; Higuchi, T.; Inoue, A.; Honjo, K.; Inoue, H.; Ikoma, K.; Ueshima, K.; Ikeda, T.; Fujiwara, H.; et al. Comparative analysis of medial patellofemoral ligament length change pattern in patients with patellar dislocation using open-MRI. Knee Surg. Sports Traumatol. Arthrosc. 2015, 25, 2330–2336. [Google Scholar] [CrossRef]
- Ghosh, K.M.; Merican, A.M.; Deehan, D.J.; Amis, A.A.; Iranpour-Boroujeni, F. Length change patterns of the extensor retinaculum and the effect of total knee replacement. J. Orthop. Res. 2009, 27, 865–870. [Google Scholar] [CrossRef] [PubMed]
- Stephen, J.M.; Lumpaopong, P.; Deehan, D.J.; Kader, D.; Amis, A.A. The Medial Patellofemoral Ligament: Location of femoral attachment and length change patterns resulting from anatomic and nonanatomic attachments. Am. J. Sports Med. 2012, 40, 1871–1879. [Google Scholar] [CrossRef] [PubMed]
- Gobbi, A.; Espregueira-Mendes, J.; Nakamura, N. The Patellofemoral Joint: State of the Art in Evaluation and Management; Springer: Berlin, Germany, 2014; pp. 1–287. [Google Scholar]
- Belkin, N.S.; Meyers, K.N.; Redler, L.H.; Maher, S.; Nguyen, J.T.; Stein, B.E.S. Medial Patellofemoral Ligament Isometry in the Setting of Patella Alta. Arthrosc. J. Arthrosc. Relat. Surg. 2020, 36, 3031–3036. [Google Scholar] [CrossRef]
- Krebs, C.; Tranovich, M.; Andrews, K.; Ebraheim, N. The medial patellofemoral ligament: Review of the literature. J. Orthop. 2018, 15, 596–599. [Google Scholar] [CrossRef]
- Loeb, A.; Tanaka, M.J. The medial patellofemoral complex. Curr. Rev. Musculoskelet. Med. 2018, 11, 201–208. [Google Scholar] [CrossRef]
- Roger, J.; Lustig, S.; Cerciello, S.; Bruno, C.F.; Neyret, P.; Servien, E.; Lustig, S. Short lateral posterior condyle is associated with trochlea dysplasia and patellar dislocation. Knee Surg. Sports Traumatol. Arthrosc. 2018, 27, 731–739. [Google Scholar] [CrossRef]
- Pfeiffer, T.R.; Burnham, J.M.; Hughes, J.D.; Kanakamedala, A.C.; Herbst, E.; Popchak, A.; Shafizadeh, S.; Irrgang, J.J.; Debski, R.E.; Musahl, V. An Increased Lateral Femoral Condyle Ratio Is a Risk Factor for Anterior Cruciate Ligament Injury. J. Bone Jt. Surg. Am. Vol. 2018, 100, 857–864. [Google Scholar] [CrossRef] [PubMed]
- Li, K.; Zheng, X.; Li, J.; Seeley, R.A.; Marot, V.; Murgier, J.; Liang, X.; Huang, W.; Cavaignac, E. Increased lateral femoral condyle ratio is associated with greater risk of ALC injury in non-contact anterior cruciate ligament injury. Knee Surg. Sports Traumatol. Arthrosc. 2020. [Google Scholar] [CrossRef] [PubMed]
- Li, R.; Yuan, X.; Fang, Z.; Liu, Y.; Chen, X.; Zhang, J. A decreased ratio of height of lateral femoral condyle to anteroposterior diameter is a risk factor for anterior cruciate ligament rupture. BMC Musculoskelet. Disord. 2020, 21, 1–6. [Google Scholar] [CrossRef] [PubMed]
| Authors | Year | Patients/Cadavers | n of Subjects | Age, Years | Sex | |
|---|---|---|---|---|---|---|
| Original articles | Steensen et al. | 2004 | Cadavers | 11 | “Elderly” | 7M; 4F |
| Victor et al. | 2009 | Cadavers | 12 | 78–87 at the time of death | 8M; 4F | |
| Higuchi et al. | 2010 | Patients | 20 | Mean 32 (range, 26–38) | 10M; 10F | |
| Stephen et al. | 2013 | Cadavers | 8 | Mean 73.5 (range, 46–88) | 5M; 3F | |
| Graf et al. | 2014 | Patients | 10 | Mean 35 (range, 25–42) | 10M; 0F | |
| Song et al. | 2015 | Patients | 11 | Mean 32.0 ± 3.9 (range, 27–39) | 11M; 0F | |
| Decante at al. | 2019 | Cadavers | 8 | Mean 85.25 | Not reported | |
| Kernkamp et al. | 2019 | Patients | 15 | Mean 25.1 ± 5.2 | 9M; 6F | |
| Huddleston et al. | 2020 | Cadavers | 8 | Below 65 | Not reported | |
| Yanke et al. | 2020 | Cadavers | 8 | Below 65 | Not reported | |
| Reviews | Amis et al. | 2003 | - | Not investigated | Not investigated | Not investigated |
| Bicos et al. | 2006 | - | Not investigated | Not investigated | Not investigated | |
| Zaffagnini et al. | 2013 | - | Not investigated | Not investigated | Not investigated | |
| Chahla et al. | 2019 | - | Not investigated | Not investigated | Not investigated | |
| Huber et al. | 2020 | - | Investigated | Investigated | Not investigated |
| Authors | Year | Patients/Cadavers | Identification of Measured Fibers | Measurement Method | Measurement Precision | |
|---|---|---|---|---|---|---|
| Original articles | Steensen et al. | 2004 | C | Multiple fibers, connecting most superior edge, midpoint, and inferior edge of the ligament at its patellar and femoral insertions. | 3D caliper straight line | Rounded to the nearest mm |
| Victor et al. | 2009 | C | Multiple fibers, connecting single femoral attachment (“bony depression proximal/posterior to the medial epicondyle and anterior/distal to the adductor tubercle”) with three patellar attachments (“at 20%, 40%, and 60% of the patellar length from the proximal tip”). | 3D CT straight line | Not reported | |
| Higuchi et al. | 2010 | P | Two fibers, measured on the most proximal and distal slice among slices in which “the entire length of the fiber bundle connecting the patella and the adductor tubercle could be observed in one cross-section”. Their values were averaged, resulting in combined single fiber value. | 2D MRI convex line | Not reported | |
| Stephen et al. | 2013 | C | Single fiber, connecting single femoral attachment (midway between the adductor tubercle and the medial epicondyle) with singe patellar attachment (“on the superomedial border of the patella, halfway between the uppermost medial border and the mid patellar body”). | 3D suture | Between 0 ± 0 mm and 1.4 ± 0.5 mm | |
| Graf et al. | 2014 | P | Two fibers, connecting “one femoral (i.e., at the adductor tubercle) and two patellar insertion points lying on the medial patellar border (i.e., the most proximal point and a distal point in the proximal third)”. | 3D CT convex line | 0.01 mm | |
| Song et al. | 2015 | P | Multiple fibers, connecting single femoral attachment (Schöttle) and five patellar attachments: “20% (point 20), 30% (point 30), 40% (point 40), 50% (point 50), and 60% (point 60) from the superior pole of the patella”. | 3D CT convex line | Not reported | |
| Decante et al. | 2019 | C | Multiple fibers, connecting single femoral attachment (“on the medial femoral epicondyle, immediately behind the femoral insertion of the MCL in 80% of the cases, remaining below and in front, at a distance from the adductor tubercle; […] on the femoral insertion of the MCL in 14% of cases, in front of the femoral insertion of the MCL in 6% of cases”) and two patellar attachments (upper and lower border of dissected MPFL). | 3D, probably straight line, no convexity reported | Not reported | |
| Kernkamp et al. | 2019 | P | Multiple fibers, connecting 185 points on the medial femoral epicondyle, including five “anatomic” attachments of MPFL (proximal, central, distal, posterior, and anterior within the dimple between the adductor tubercle and the medial femoral epicondyle) and three patellar attachments (proximal, central, and distal). | 3D CT convex line | 0.3 ± 0.1 mm | |
| Huddleston et al. | 2020 | C | Multiple fibers, connecting single femoral attachment (identified “visually”) and four patellar attachments of MPFC: midpoint patella, MPFC osseous footprint center, superior medial pole of the patella at the level of the quadriceps insertion, and “the proximal extent of the MPFC along the quadriceps tendon”. | 3D caliper straight line | 0.051 mm | |
| Yanke et al. | 2020 | C | Multiple fibers, connecting single femoral attachment (established by means of palpating “the sulcus between the medial epicondyle and abductor tubercle”) and four patellar attachments the same as in the study of Huddleston et al. | 3D straight line | Not reported | |
| Reviews | Amis et al. | 2003 | - | Mentioned: “it often seems to have two functional bands of fibers, that run along the proximal and distal edges”. | not investigated | Not investigated |
| Bicos et al. | 2006 | - | Not investigated | not investigated | Not investigated | |
| Zaffagnini et al. | 2013 | - | Investigated | not investigated | Not investigated | |
| Chahla et al. | 2019 | - | Not investigated | not investigated | Not investigated | |
| Huber et al. | 2020 | - | Mentioned: “investigations into the influence of the patellar attachment sites on the elongation behavior of the ligament have suggested that the superior fibers are strained differently from the inferior fibers, hence plausibly indicating that 2 functionally independent regions of the structure exist”. | investigated | Not investigated |
| Authors | Year | Patients/Cadavers | Quadriceps Muscle | Iliotibal Band | Hamstrings | |
|---|---|---|---|---|---|---|
| Original articles | Steensen et al. | 2004 | Cadavers | Simulated, load not reported | Not simulated | Not simulated |
| Victor et al. | 2009 | Cadavers | Simulated, high load | Not simulated | Simulated, high load | |
| Higuchi et al. | 2010 | Patients | Resting | Resting | Resting | |
| Stephen et al. | 2013 | Cadavers | Simulated, high load | Simulated, high load | Not simulated | |
| Graf et al. | 2014 | Patients | Contracted | Contracted | Contracted | |
| Song et al. | 2015 | Patients | Resting | Resting | Resting | |
| Decante at al. | 2019 | Cadavers | Not simulated | Not simulated | Not simulated | |
| Kernkamp et al. | 2019 | Patients | Contracted | Contracted | Contracted | |
| Huddleston et al. | 2020 | Cadavers | Resting tension simulated | Not simulated | Not simulated | |
| Yanke et al. | 2020 | Cadavers | Resting tension simulated | Not simulated | Not simulated | |
| Reviews | Amis et al. | 2003 | - | Mentioned | Not investigated | Not investigated |
| Bicos et al. | 2006 | - | Not investigated | Not investigated | Not investigated | |
| Zaffagnini et al. | 2013 | - | Not investigated | Not investigated | Not investigated | |
| Chahla et al. | 2019 | - | Mentioned | Not investigated | Not investigated | |
| Huber et al. | 2020 | - | Investigated | Not investigated | Not investigated |
| Authors | Year | Patients/Cadavers | Patellar Height | Trochlear or Patellar Dysplasia | TT-TG Distance | Mechanical Axis of the Limb | Femoral Anteversion | Femoral Condylar Dimensions | |
|---|---|---|---|---|---|---|---|---|---|
| Original articles | Steensen et al. | 2004 | Cadavers | Not reported | Not reported | Not reported | Not reported | Not reported | Not reported |
| Victor et al. | 2009 | Cadavers | Not reported | Not reported | Not reported | Not reported | Not reported | Not reported | |
| Higuchi et al. | 2010 | Patients | Reported, normal | Reported, normal | Not reported | Mean Q-angle 14° | Not reported | Not reported | |
| Stephen et al. | 2013 | Cadavers | Reported, normal | Reported, normal | Not reported | Not reported | Not reported | Not reported | |
| Graf et al. | 2014 | Patients | Not reported | Not reported | Not reported | Not reported | Not reported | Not reported | |
| Song et al. | 2015 | Patients | Reported, normal | Reported, normal | Reported, normal | Reported, normal | Not reported | Not reported | |
| Decante at al. | 2019 | Cadavers | Not reported | Not reported | Not reported | Severe def. excluded | Not reported | Not reported | |
| Kernkamp et al. | 2019 | Patients | Implicitly reported to be normal | Implicitly reported to be normal | Reported, normal | Not reported | Not reported | Implicitly reported to be normal | |
| Huddleston et al. | 2020 | Cadavers | Reported, normal | Reported, normal | Not reported | Not reported | Not reported | Not reported | |
| Yanke et al. | 2020 | Cadavers | Tested variable | Reported, normal | Reported, normal | Not reported | Not reported | Not reported | |
| Reviews | Amis et al. | 2003 | - | Not investigated | Not investigated | Not investigated | Not investigated | Not investigated | Not investigated |
| Bicos et al. | 2006 | - | Not investigated | Mentioned | Mentioned | Mentioned | Mentioned | Not investigated | |
| Zaffagnini et al. | 2013 | - | Not investigated | Not investigated | Not investigated | Mentioned | Mentioned | Not investigated | |
| Chahla et al. | 2019 | - | Not investigated | Not investigated | Not investigated | Not investigated | Not investigated | Not investigated | |
| Huber et al. | 2020 | - | Not investigated | Mentioned | Not investigated | Not investigated | Not investigated | Not investigated |
| Original Articles | Reviews | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Authors | Steensen et al. | Victor et al. | Higuchi et al. | Stephen et al. | Graf et al. | Song et al. | Decante at al. | Kernkamp et al. | Huddleston et al. | Yanke et al. | Amis et al. | Bicos et al. | Zaffagnini et al. | Chahla et al. | Huber et al. |
| Year | 2004 | 2009 | 2010 | 2013 | 2014 | 2015 | 2019 | 2019 | 2020 | 2020 | 2003 | 2006 | 2013 | 2019 | 2020 |
| Patients/cadavers | C | C | P | C | P | P | C | P | C | C | - | - | - | - | - |
| Number | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | x | x | x | x | ✓ |
| Age | ~ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ~ | ~ | x | x | x | x | x |
| M:F ratio | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | x | ✓ | x | x | x | x | x | x | x |
| Demographics (max 3) | 2 | 3 | 3 | 3 | 3 | 3 | 2 | 3 | 1 | 1 | 0 | 0 | 0 | 0 | 1 |
| Identification of measured fibers | ✓ MF | ✓ MF | ✓ MF | ✓ SF | ~ MF | ✓ MF | ✓ MF | ✓ MF | ✓ MF | ✓ MF | ~ | x | ✓ | x | ~ |
| Measurement method | ~ 3DSL | ~ 3DSL | ~ 2D CL | ✓ 3DCL | ✓ 3DCL | ✓ 3DCL | ~ 3DSL | ✓ 3DCL | ~ 3DSL | ~ 3DSL | x | x | x | x | ✓ |
| Measurement precision | ✓ | x | x | ✓ | ✓ | x | x | ✓ | ✓ | x | x | x | x | x | x |
| Quadriceps | ~ | ✓ Co | ~ R | ✓ Co | ✓ Co | ~ R | x | ✓ Co | ~ R | ~ R | ~ | x | x | ~ | ✓ |
| ITB | x | x | ~ R | ✓ Co | ✓ Co | ~ R | x | ✓ | x | x | x | x | x | x | x |
| Hamstrings | x | ✓ Co | ~ R | x | ✓ Co | ~ R | x | ✓ Co | x | x | x | x | x | x | x |
| Study design (max 6) | 2 | 3 | 1 | 5 | 5 | 5 | 1 | 6 | 2 | 1 | 0 | 0 | 1 | 0 | 2 |
| Patellar height | x | x | ✓ | ✓ | x | ✓ | x | ~ | ✓ | ✓ | x | x | x | x | x |
| Trochlear or patellar dysplasia | x | x | ✓ | ✓ | x | ✓ | x | ~ | ✓ | ✓ | x | ~ | x | x | ~ |
| TT-TG distance | x | x | x | x | x | ✓ | x | ✓ | x | ✓ | x | ~ | x | x | x |
| Mechanical axis of the limb | x | x | ✓ | x | x | ✓ | ~ | x | x | x | x | ~ | ~ | x | x |
| Femoral anteversion | x | x | x | x | x | x | x | x | x | x | x | ~ | ~ | x | x |
| Femoral condylar dimensions | x | x | x | x | x | x | x | ~ | x | x | x | x | x | x | x |
| Morphology (max 6) | 0 | 0 | 3 | 2 | 0 | 4 | 0 | 1 | 2 | 3 | 0 | 0 | 0 | 0 | 0 |
| Total (max 15) | 4 | 6 | 7 | 10 | 8 | 9 | 3 | 10 | 5 | 5 | 0 | 0 | 1 | 0 | 3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mostowy, M.; Kwas, K.; Ruzik, K.; Koźlak, M.; Kwapisz, A.; Brzezinska, E.; Malinowski, K.; Domżalski, M.E. Why Determining the Native Length Change Pattern of Medial Patellofemoral Ligament Is Still a Challenge: State-of-the-Art Review of Potential Sources of Heterogeneity within Studies Evaluating Isometry of MPFL. Appl. Sci. 2021, 11, 4771. https://doi.org/10.3390/app11114771
Mostowy M, Kwas K, Ruzik K, Koźlak M, Kwapisz A, Brzezinska E, Malinowski K, Domżalski ME. Why Determining the Native Length Change Pattern of Medial Patellofemoral Ligament Is Still a Challenge: State-of-the-Art Review of Potential Sources of Heterogeneity within Studies Evaluating Isometry of MPFL. Applied Sciences. 2021; 11(11):4771. https://doi.org/10.3390/app11114771
Chicago/Turabian StyleMostowy, Marcin, Katarzyna Kwas, Kacper Ruzik, Magdalena Koźlak, Adam Kwapisz, Eva Brzezinska, Konrad Malinowski, and Marcin E. Domżalski. 2021. "Why Determining the Native Length Change Pattern of Medial Patellofemoral Ligament Is Still a Challenge: State-of-the-Art Review of Potential Sources of Heterogeneity within Studies Evaluating Isometry of MPFL" Applied Sciences 11, no. 11: 4771. https://doi.org/10.3390/app11114771
APA StyleMostowy, M., Kwas, K., Ruzik, K., Koźlak, M., Kwapisz, A., Brzezinska, E., Malinowski, K., & Domżalski, M. E. (2021). Why Determining the Native Length Change Pattern of Medial Patellofemoral Ligament Is Still a Challenge: State-of-the-Art Review of Potential Sources of Heterogeneity within Studies Evaluating Isometry of MPFL. Applied Sciences, 11(11), 4771. https://doi.org/10.3390/app11114771






