Abstract
Radiation dose management of medical staff has become increasingly important. Particularly, based on the statement by the International Commission on Radiological Protection (ICRP) in 2011, a new lower equivalent dose limit for the eye lens is being established in each country. Although many reports have discussed the occupational radiation dose in interventional radiology (IR), few studies have examined the dose during computed tomography (CT) examinations. This study investigated the radiation dose exposure to medical staff present in the CT room during irradiation, with particular focus on the exposure to eye lens. The radiation dose exposure to those who assist patients during head, chest and upper abdomen CT examination was measured in a phantom study. The radiation dose exposure with scattered radiation was never negligible (i.e., high); Hp(3) was the highest in head CT examination, at 0.44 mSv per examination. Furthermore, the shielding effect of radiation protection glasses was large, and radiation protection glasses are useful tools for the medical staff who are involved in CT examinations. The justification and optimisation should be carefully considered in assistant actions.
1. Introduction
Computed tomography (CT) is an indispensable modality in modern diagnostic imaging. The use of CT is increasing owing to the technical advances in this technique. Medical staff members (e.g., physicians, nurses and radiological technologists) occasionally remain in the CT examination room during irradiation to monitor the injection of the contrast media, to restrain the patient, operate medical devices, etc. [1,2,3,4,5,6]. These actions are performed for medical safety/procedures or maintaining image quality. In particular, in Japan and United States, both, the frequency CT examination [7,8] and radiation dose exposure of the patient undergoing CT examination is high [8]. In these situations, radiation dose management for the medical staff is more meaningful. The importance of radiation protection during irradiation in CT room is presented in a guideline for radiation safety of medical staff [9].
The International Commission on Radiological Protection (ICRP) recommended the new lower equivalent dose limit for the eye lens of 20 mSv/y that is averaged over a defined period of 5 y, with no single year exceeding 50 mSv for occupational exposure [10,11].
Many studies have investigated the occupational radiation dose in interventional radiology (IR), wherein medical staff may be exposed to considerable scattered X-rays. However, few studies have discussed occupational radiation dose in CT examinations [1,2,3,4,5,6,12]. Our literature search did not reveal any report that directly investigated the radiation dose of eye lens as Hp(3). Moreover, radiation protection glasses (Pb glasses) are useful for reducing the radiation exposure to eye lens; the shielding effect of the light type of Pb glasses (0.07 mmPb) in IR is about 60% [13,14,15]. Pb glasses may also need to be worn by the medical assisting staff who are present in the room during CT examination. The tube voltage used in CT examination is generally fixed at 120 kV [16] that is typically higher than that in IR [17]. With an increase in the photon energy, the shielding effect of Pb glasses decreases [18]. Therefore, the protective effect of Pb glasses in CT needs to be determined.
This phantom study aimed to measure Hp(3) to the eye with or without Pb glasses and Hp(10) and Hp(0.07) to the trunk inside or outside the radiation protection apron for the assisting staff during CT examination.
2. Materials and Methods
In this study, radiation dose exposure of the medical staff members who assist in head, chest and upper abdomen CT scans was evaluated. The assistant actions included acts, such as monitoring injection of the contrast media (e.g., initial supervision in bolus tracking method), restraining the patient (e.g., fixation of head or arms) and operating the medical device (e.g., operating of bag valve mask).
Medical staff phantom built up has been shown in Figure 1. Medical staff phantom was constructed with anthropomorphic head phantoms (ALDERSON) and X-ray water phantom for chest and abdomen (JIS Z 4915-1974, Miwa Electric Medical Co., Ltd., Aichi, Japan). External layer of the water phantom was filled with water. The water phantom was set on a desk, and the head phantom was set on the water phantom. The height of medical staff phantom was 158 cm; it simulates the average body height of a Japanese woman. The medical staff phantom was covered with radiation protection apron of lead equivalent of 0.35 mmPb (Dream Light, Maeda & Co., Ltd., Tokyo, Japan).
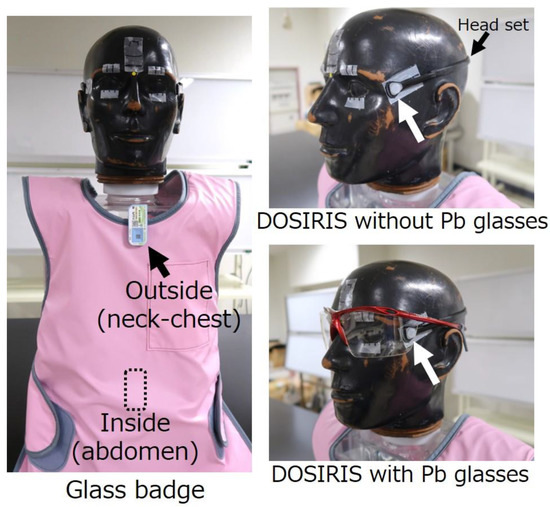
Figure 1.
Medical staff phantom and layout of personal dosimeter and Pb glasses.
DOSIRIS (Chiyoda Technol Corporation, Tokyo, Japan) for Hp(3) and glass badge (Chiyoda Technol Corporation, Tokyo, Japan) for Hp(10) and Hp(0.07) [19] were used as personal dosimeter. DOSIRIS is consist of thermoluminescent dosimeter, and glass badge is composed of radiophotoluminescence glass dosimeter. These dosimeters are of the passive type, and a radiation dose reading is performed by manufacturer. Radiation monitoring system of the manufacturer complies with ISO/IEC 17025: 2017 and traceability is ensured [20,21]. With glass badge, Hp(10) and Hp(0.07) can be measured simultaneously. DOSIRIS and glass badge were set on medical staff phantom. DOSIRIS was set near the left lateral canthus using a ready-made head set prepared by manufacturer. Glass badges were set both, outside (neck–chest position) and inside (abdomen) the radiation protection apron. It has reported that DOSIRIS and glass badge have a good angular response [19,22].
Light type of Pb glasses (Panorama Shield, Toray Medical Co. Ltd., Tokyo, Japan) whose lead equivalent was 0.07 mmPb was used. With or without Pb glasses, individual dose measurement was performed. Dose reduction effect of Pb glasses was calculated as follows:
Dose reduction effect (%) = {1 − (Hp(3) with Pb glasses)/(Hp(3) without Pb glasses)}×100.
An 8-channel multi-detector row CT scanner (LightSpeed Ultra, GE Healthcare Japan Corporation, Tokyo, Japan) was used for measuring the dose after performing the daily calibration. Anthropomorphic phantom (PBU-50, Kyoto Kagaku Co., Ltd., Kyoto, Japan) was laid down on the bed of the CT scanner as patient phantom. In head scan, the hands of patient phantom were set on the abdomen. In chest and upper abdomen scans, the arms of the patient phantom were raised and fixed. Scanning was performed using CT-auto exposure control. Detail scan parameters and dose information (CT dose index: CTDIvol, dose length product: DLP) indicated on CT scanner console are shown in Table 1. These values (CTDIvol or DLP) are reasonable setting compared to national diagnostic reference levels in Japan (Japan DRLs 2020) [23].

Table 1.
Scan parameter and dose information obtained from the CT scanner console.
Medical staff phantom was made to stand straight, facing the iso-centre of the CT scanner. The distance between the iso-centre and the nasal root was 75, 85 and 95 cm in the head, chest and upper abdomen scans, respectively. The layout in dose measurement is shown in Figure 2. Scanning was performed 10 times in the head scan, 20 times in the chest and upper abdomen scans. The scattered X-ray (mainly derived from patient phantom) was measured with a personal dosimeter (i.e., DOSIRIS and glass badge). Each personal dose equivalent per examination was calculated by dividing the accumulated dose by the number of scan times. Furthermore, effective dose of medical staff related to nonuniform exposure was also calculated using the following equation:
where Ha and Hb are Hp(10) outside and inside apron, respectively. This formula is generally used to evaluate an individual effective dose in radiation management in Japan [24,25,26,27].
Effective dose (mSv) = 0.11 Ha + 0.89 Hb
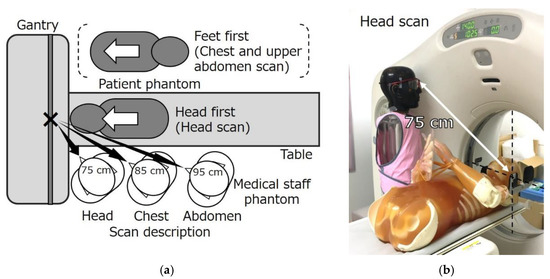
Figure 2.
Layout in dose measurement. (a) a top view and (b) an example; the layout of head scan.
Hp(3) of the medical staff per DLP in each scan was also determined. The value of Hp(3) in each scan was normalised to that in the 75 cm position based on the inverse square law. The normalised Hp(3) was divided by DLP.
In this study, uncertainty was evaluated only for the measured value of the personal dose equivalent using a personal dosimeter. The expanded uncertainty was evaluated with a coverage factor of k = 2, which indicates approximately 95% confidence level. The accuracy of the personal dosimeter has not been reported; therefore, we assumed an accuracy of 10%. The measurement result was denoted as measured value ± expanded uncertainty.
3. Results
The radiation dose exposure of the medical staff in head scans is shown in Figure 3a. Hp(3) without Pb glasses, Hp(10) and Hp(0.07) outside apron in head scans were 0.44 ± 0.05, 0.51 ± 0.06 and 0.53 ± 0.06 mSv per examination, respectively. Hp(3) with the Pb glasses, Hp(10) and Hp(0.07) inside the apron per examination were 0.14 ± 0.02, 0.035 ± 0.004 and 0.035 ± 0.004 mSv.
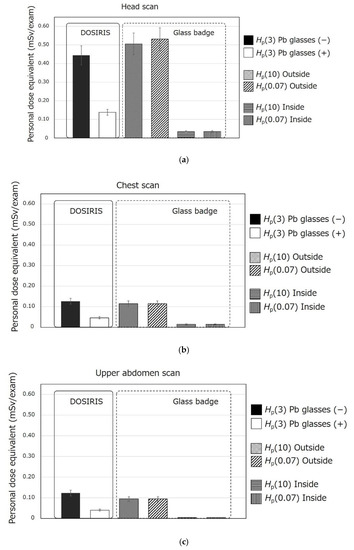
Figure 3.
Personal dose equivalent in (a) head scan, (b) chest scan and (c) upper abdomen scan. Pb glasses (−) and Pb glasses (+) denote without Pb glasses and with Pb glasses, respectively. The error bars indicate the uncertainty of the measured value.
Figure 3b shows the results in chest scan. Hp(3) without Pb glasses and Hp(10) and Hp(0.07) outside apron per examination were 0.13 ± 0.01, 0.12 ± 0.01 and 0.12 ± 0.01 mSv, respectively. Hp(3) with Pb glasses and Hp(10) and Hp(0.07) inside apron per examination were 0.047 ± 0.005, 0.015 ± 0.002 and 0.015 ± 0.002 mSv, respectively.
Figure 3c depicts the personal dose equivalent in upper abdominal scan, Hp(3) without Pb glasses and Hp(10) and Hp(0.07) outside apron per examination were 0.12 ± 0.01, 0.095 ± 0.011 and 0.095 ± 0.011 mSv, respectively. Hp(3) with Pb glasses and Hp(10) and Hp(0.07) inside the apron per examination were 0.041 ± 0.005, 0.0050 ± 0.0006 and 0.0050 ± 0.0006 mSv, respectively.
Dose reduction effect of Pb glasses was 63–69%. Determined effective doses of medical staff per examination are shown in Table 2, and determined Hp(3) (without Pb glasses) of medical staff per DLP in each scan in the normalised position of 75 cm is shown in Table 3.

Table 2.
Estimated effective dose exposure of the medical staff in each scan.

Table 3.
Hp(3) of the medical staff per DLP in normalised position of 75 cm (without Pb glasses).
4. Discussion
Research has shown that the radiation dose in patients who underwent CT was the highest in diagnostic radiography [28]. Therefore, scattered X-ray from patient in CT also seemed to be high due to the considerable radiation dose used in CT. It is imperative to identify the radiation dose exposure of the medical staff members who are present in the CT room during examination, particularly the radiation exposure dose of eye lens, whose equivalent dose limit is being reduced is important.
The highest personal dose equivalent of the medical staff was observed in head scan. This is firstly owing to the small distance between the iso-centre and eye. Second, it assumed to be attributed to the higher radiation dose in the scan protocol (i.e., high DLP). Hp(3) without Pb glasses in head scan was 0.44 ± 0.05 mSv per examination. If a medical staff member engages in assistant action of head CT scan 46 times without Pb glasses, the radiation dose of the eye lens reaches a new dose limit of 20 mSv/y. A medical staff member frequently assists patient during radiation exposure from necessity; therefore, it is important for the staff member to wear Pb glasses. In the meantime, in the first place, it should be considered whether the assistant action is necessary in the clinical situation based on the concept of ‘justification of practices’. The assistant action should be kept to the minimum.
In this study, Hp(3) in the chest and upper abdomen scan were relatively low. Furthermore, when an injection of contrast media is monitored as assistant action at only an early timing (e.g., in bolus tracking method), radiation dose exposure of medical staff would be smaller due to the short time of assistant action and less amount of X-ray used in the method. However, it is never negligible; if examination is repeated in dynamic scan, etc. in the case of holding patient body, the radiation dose is simply added. Furthermore, if an examination is performed with higher radiation dose (i.e., high DLP), the amount of scattered X-ray radiation increases.
Additionally, as described above, since the radiation dose exposure of medical staff with scattered X-ray in CT examination is high, the use of mobile radiation shielding screen should be also considered depending on the situation in the case of observation/supervision of patient, to reduce radiation dose of the whole body.
The use of a dosimeter for eye lens is not widespread; therefore, it is challenging to evaluate Hp(3) in the current clinical situation. Personal dose equivalent (i.e., Hp(3), Hp(10) and Hp(0.07)) per air-absorbed dose depends on the photon energy [29]. Within this study, there was no distinguished difference between the measured value of Hp(3) without Pb glasses and Hp(10), Hp(0.07) outside a protective apron in assistant action during CT examination that is generally performed with a tube voltage of 120 kV; the difference was within 25%. Therefore, it may be possible to estimate the radiation dose of eye lens of medical staff using popular personal dosimeter for Hp(10) or Hp(0.07) measurement in CT examination, when the medical staff does not wear Pb glasses owing to the small amount of scattered X-ray or infrequent assistance.
Although X-ray energy used in CT examination is relatively high, the dose reduction effect of Pb glasses was 63–69%, similar to that in IR reported previously [13,14,15]. Air dose distribution and energy distribution of scattered X-ray in CT examination is expected to be very complicated owing to the rotation of the X-ray tube. Thus, it was believed that the dose reduction effect was not lower than that in IR.
The effective doses per examination of the medical staff member associated with assistance actions in CT with protective apron were 0.087, 0.026 and 0.015 mSv in the head, chest and upper abdomen, respectively. Hp(10) inside the protective apron was about 1/10th of Hp(10) outside the protective apron. The trunk of the body was adequately protected by the apron. Therefore, the effective dose was much smaller than Hp(10) without the apron. Thus, the use of a radiation protective apron is essential while performing assistive actions during X-ray irradiation.
Hp(3) of the medical staff per DLP was determined as 3.6 × 10−4, 7.4 × 10−4 and 7.3 × 10−4 mSv/DLP in head, chest and upper abdomen scans, respectively. In spite of the largest Hp(3) of 0.44 mSv/exam in the head scan, Hp(3) per DLP was the smallest among the 3 kinds of scans. This may be owing to the size difference of CTDI phantom used in CTDI measurement. DLP indicated on the console of the CT scanner is the product of CTDIvol and scan range (cm). This CTDIvol was a value measured by the manufacturer in advance. In the measurement of CTDIvol, small size phantom (diameter of 16 cm) for head and large size phantom (diameter of 32 cm) for trunk of the body are used. If the output of X-ray from X-ray tube is same, CTDIvol obtained by small size CTDI phantom is larger than that obtained with large CTDI phantom. Therefore, output of X-ray from X-ray tube per CTDIvol in head scan is smaller than that in chest and upper abdomen scans. Consequently, scattered X-ray per CTDIvol in head scan is also smaller than that in chest and upper abdomen scan. Moreover, the amount of scattered X-ray depends on the size of the scanning subject; therefore, the scattered X-ray from the anthropomorphic head phantom was smaller than that from the chest or abdomen phantom. Thus, it was thought that Hp(3) per DLP in head scan was the smallest. We believe that Hp(3) per DLP shown in Table 3 can be universally used as a crude indicator (i.e., conversion factor) to estimate the Hp(3) of the medical staff in any CT examination, multiplying the value of Hp(3)/DLP and DLP indicated on the console, unless there are significant differences in the patient physique or scan range. In this case, it needs to be distinguished from the head and trunk of the body as the body site of the scan (i.e., it needs to be distinguished whether the DLP indicated on the console obtained from 16 cm or 32 cm CTDI phantom). Furthermore, the estimated radiation dose needs to be corrected by distance based on the inverse square law. This indicator may need to be additionally reviewed for use in several situations. For example, the difference in the filter used for the X-ray tube may need consideration because it influences the effective energy of X-ray that affects the amount of scattered X-ray radiation.
This study has certain limitations. First, only female medical staff members with standard height of 158 cm were enrolled. This height is not representative of all medical staff members because the average height of male medical staff members would be more. This would affect the results because the eye lens of shorter subjects is located in a position that is closer to the iso-centre than those of taller staff members. Therefore, we believe that the radiation dose was conservatively estimated in this study. Taller medical staff members would be exposed to less radiation. Second, the CT scanner used in this study was not the most advanced model. However, the amount of scattered X-ray radiation depends on DLP; therefore, we believe that the result of this study can be applied to the current clinical situation used by advanced CT scanner. Next, although the typical tube voltage of 120 kV was used in this study, CT examination with low tube voltage (i.e., 80 or 100 kV) is sometimes performed [16]. Since the amount of scattered X-ray depends on tube voltage [30], the radiation dose of medical staff would be evaluated on the safe side in this study. Finally, the personal dosimeter was set not on the eye position but on the side of the eye. The radiation dose of the eye lens may be slightly different in the present results.
5. Conclusions
This study evaluated the radiation dose exposure of medical staff who occasionally stay in CT room during irradiation focusing on the eye lens. Hp(3) of the medical staff in head CT examination was the highest, at 0.44 mSv per procedure. The new lower limit of exposure for eye lens (20 mSv/y) may be exceeded without the use of Pb glasses, depending on the assistance situation. Pb glasses are important protection tools in CT examination as well. The justification of practice and optimisation of protection should be carefully considered for medical staff members providing assistance in CT examinations.
Author Contributions
Conceptualization, M.O. and K.K.; methodology, M.O., K.K., M.H., M.K., M.T. and A.F.; data analysis, M.O., H.S. and K.S.; validation, K.K. and S.H.; formal analysis, M.O., H.S. and K.S.; writing—original draft preparation, M.O.; writing—review and editing, M.O., K.K. and M.H.; supervision, Y.H. and Y.S.; funding acquisition, M.O., K.K. and M.K. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by JSPS KAKENHI Grant Number JP19K10705, JP19K10763.
Institutional Review Board Statement
Not applicable. This study did not involve humans or animals.
Informed Consent Statement
Not applicable. This study did not involve humans.
Data Availability Statement
Not applicable
Conflicts of Interest
The authors declare no conflict of interest.
References
- Theumann, N.H.; Verdun, F.R.; Valley, J.F.; Capasso, P.; Schnyder, P.; Meuli, R.A. Radiation doses delivered to radiologists during contrast-enhanced helical-CT examinations. Eur. Radiol. 1999, 9, 1919–1922. [Google Scholar] [CrossRef] [PubMed]
- Al-Haj, A.N.; Lobriguito, A.M.; Lagarde, C.S. Occupational doses during the injection of contrast media in paediatric CT procedures. Radiat. Prot. Dosim. 2003, 103, 169–172. [Google Scholar] [CrossRef] [PubMed]
- Mori, H.; Koshida, K.; Ishigamori, O.; Matsubara, K. Investigation of qualitative and quantitative factors related to radiological exposure to nursing staff during computed tomography examinations. Health Phys. 2014, 107, S202–S210. [Google Scholar] [CrossRef] [PubMed]
- Heilmaier, C.; Mayor, A.; Zuber, N.; Fodor, P.; Weishaupt, D. Improving radiation awareness and feeling of personal security of non-radiological medical staff by implementing a traffic light system in computed tomography. Rofo 2016, 188, 280–287. [Google Scholar] [CrossRef] [PubMed]
- Miyajima, R.; Fujibuchi, T.; Miyachi, Y.; Tateishi, S.; Uno, Y.; Amakawa, K.; Ohura, H.; Orita, S. Effective techniques to reduce radiation exposure to medical staff during assist of X-ray computed tomography examination. Nihon Hoshasen Gijutsu Gakkai Zasshi 2018, 74, 326–334. (In Japanese) [Google Scholar] [CrossRef] [PubMed]
- Radiation Council. Secretariat of Nuclear Regulation Authority of Japan. 2017. Available online: https://www.nsr.go.jp/data/000209654.pdf (accessed on 19 March 2021).
- Ono, K.; Yoshitake, T.; Hasegawa, T.; Ban, N.; Kai, M. Estimation of the number of CT procedures based on a nationwide survey in Japan. Health Phys. 2011, 100, 491–496. [Google Scholar] [CrossRef] [PubMed]
- Rehani, M.M.; Hauptmann, M. Estimates of the number of patients with high cumulative doses through recurrent CT exams in 35 OECD countries. Phys. Med. 2020, 76, 173–176. [Google Scholar] [CrossRef] [PubMed]
- 2-3 Patient Assistance in X-ray Examination Room. Guideline for Radiation Safety of Medical Staff (Provisional Translation). 2020. Available online: https://www.jsrt.or.jp/data/wp-content/uploads/2020/10/suisyoutai_pdf2020.10.1.pdf (accessed on 19 March 2021).
- International Commission on Radiological Protection. Statement on Tissue Reactions. 2011; ICRP Ref 4825-3093-1464. [Google Scholar]
- International Commission on Radiological Protection. Publication 118: ICRP Statement on Tissue Reactions/Early and Late Effects of Radiation in Normal Tissues and Organs-Threshold Doses for Tissue Reactions in a RADIATION Protection Context; Annual of ICRP; Elsevier Ltd: Amsterdam, 2012. [Google Scholar]
- Kobayashi, M.; Koshida, K.; Suzuki, S.; Katada, K. Evaluation of patient dose and operator dose in swallowing CT studies performed with a 320-detector-row multislice CT scanner. Radiol. Phys. Technol. 2012, 5, 148–155. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Haga, Y.; Chida, K.; Kaga, Y.; Sota, M.; Meguro, T.; Zuguchi, M. Occupational eye dose in interventional cardiology procedures. Sci. Rep. 2017, 7, 569. [Google Scholar] [CrossRef] [PubMed]
- Kato, M.; Chida, K.; Ishida, T.; Toyoshima, H.; Yoshida, Y.; Yoshioka, S.; Moroi, J.; Kinoshita, T. Occupational radiation exposure of the eye in neurovascular interventional physician. Radiat. Prot. Dosim. 2019, 185, 151–156. [Google Scholar] [CrossRef] [PubMed]
- Yokoyama, S.; Suzuki, S.; Toyama, H.; Arakawa, S.; Inoue, S.; Kinomura, Y.; Kobayashi, I. Evaluation of eye lens doses of interventional cardiologists. Radiat. Prot. Dosim. 2017, 173, 218–222. [Google Scholar] [CrossRef] [PubMed]
- Osanai, M.; Saito, Y.; Oyu, K.; Ishida, J.; Sato, M.; Sasaki, T. Image quality and radiation dose with low tube voltage in coronary CT angiography: An experimental study with normal type and soft plaque phantom. Hirosaki Med. J. 2013, 64, 15–28. [Google Scholar]
- Ishii, H.; Chida, K.; Satsurai, K.; Haga, Y.; Kaga, Y.; Abe, M.; Inaba, Y.; Zuguchi, M. A phantom study to determine the optimal placement of eye dosemeters on interventional cardiology staff. Radiat. Prot. Dosim. 2019, 185, 409–413. [Google Scholar] [CrossRef] [PubMed]
- Osanai, M.; Kudo, K.; Hosoda, M.; Tazoe, H.; Akata, N.; Kitajima, M.; Tsushima, M.; Komiya, N.; Kudo, M.; Tsujiguchi, T.; et al. The impact on the eye lens of radiation emitted by natural radionuclides (lead-210) present in radiation protection glasses. Radiat. Prot. Dosim. 2020, 188, 13–21. [Google Scholar] [CrossRef] [PubMed]
- Maki, D.; Ube, M.; Nagashima, Y.; Shinozaki, W.; Ueno, S.; Koguchi, Y.; Takeuchi, N. Development of the new glass badge. Radiat. Prot. Dosim. 2016, 171, 337–345. [Google Scholar] [CrossRef] [PubMed]
- Japan Accreditation Board. Available online: https://www.jab.or.jp/system/service/upload/RTL04590/RTL04590-en.pdf (accessed on 30 April 2021).
- Chiyoda Technol Corporation. Available online: https://www.c-technol.co.jp/eng/e-reason (accessed on 9 April 2021).
- Ishii, H.; Haga, Y.; Sota, M.; Inaba, Y.; Chida, K. Performance of the DOSIRIS™ eye lens dosimeter. J. Radiol. Prot. 2019, 39, N19–N26. [Google Scholar] [CrossRef] [PubMed]
- Japan Network for Research and Information on Medical Exposure. National Diagnostic Reference Levels in Japan (2020)—Japan DRLs 2020. 2020. Available online: http://www.radher.jp/J-RIME/report/DRL2020_Engver.pdf (accessed on 19 March 2021).
- Ministry of Health, Labour and Welfare. Notice No 254. 2001. Available online: https://www.mhlw.go.jp/content/11300000/000689300.pdf (accessed on 19 March 2021).
- Funao, H.; Ishii, K.; Momoshima, S.; Iwanami, A.; Hosogane, N.; Watanabe, K.; Nakamura, M.; Toyama, Y.; Matsumoto, M. Surgeons’ exposure to radiation in single-and multi-level minimally invasive transforaminal lumbar interbody fusion; a prospective study. PLoS ONE 2014, 9, e95233. [Google Scholar] [CrossRef] [PubMed]
- Komemushi, A.; Suzuki, S.; Sano, A.; Kanno, S.; Kariya, S.; Nakatani, M.; Yoshida, R.; Kono, Y.; Ikeda, K.; Utsunomiya, K.; et al. Radiation dose of nurses during IR procedures: A controlled trial evaluating operator alerts before nursing tasks. J. Vasc. Interv. Radiol. 2014, 25, 1195–1199. [Google Scholar] [CrossRef] [PubMed]
- Inoue, T.; Komemushi, A.; Murota, T.; Yoshida, T.; Taguchi, M.; Kinoshita, H.; Matsuda, T. Effect of protective lead curtains on scattered radiation exposure to the operator during ureteroscopy for stone disease: A controlled trial. Urology 2017, 109, 60–66. [Google Scholar] [CrossRef] [PubMed]
- International Commission on Radiological Protection. ICRP Publication 87: Managing Patient Dose in Computed Tomography; Annual of ICRP; Pergamon Press: Oxford, UK, 2000. [Google Scholar]
- International Commission on Radiological Protection. ICRP Publication 51: Data for Use in Protection against External Radiation; Annual of ICRP; Pergamon Press: Oxford, UK, 1987. [Google Scholar]
- Vlachos, I.; Tsantilas, X.; Kalyvas, N.; Delis, H.; Kandarakis, I.; Panayiotakis, G. Measuring scatter radiation in diagnostic X rays for radiation protection purposes. Radiat. Prot. Dosim. 2015, 165, 382–385. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).