Anatomical Characteristics of the Masseter Muscle in Mandibular Prognathism
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Group Classification
2.3. 3D CT and Segmentation
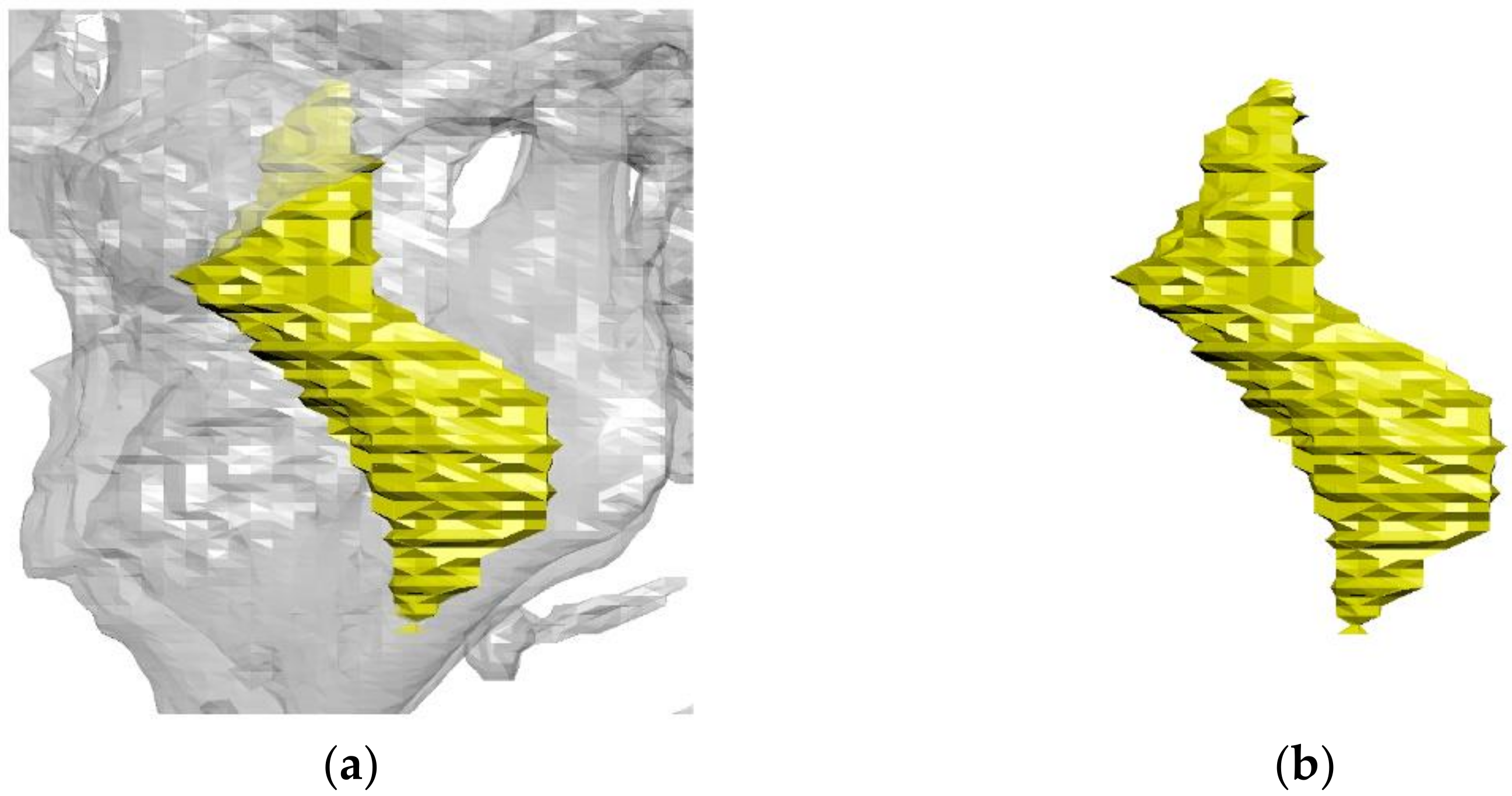
2.4. 3D Image Reconstruction and Revision
2.5. Volume and Length Measurement of the Masseter Muscle
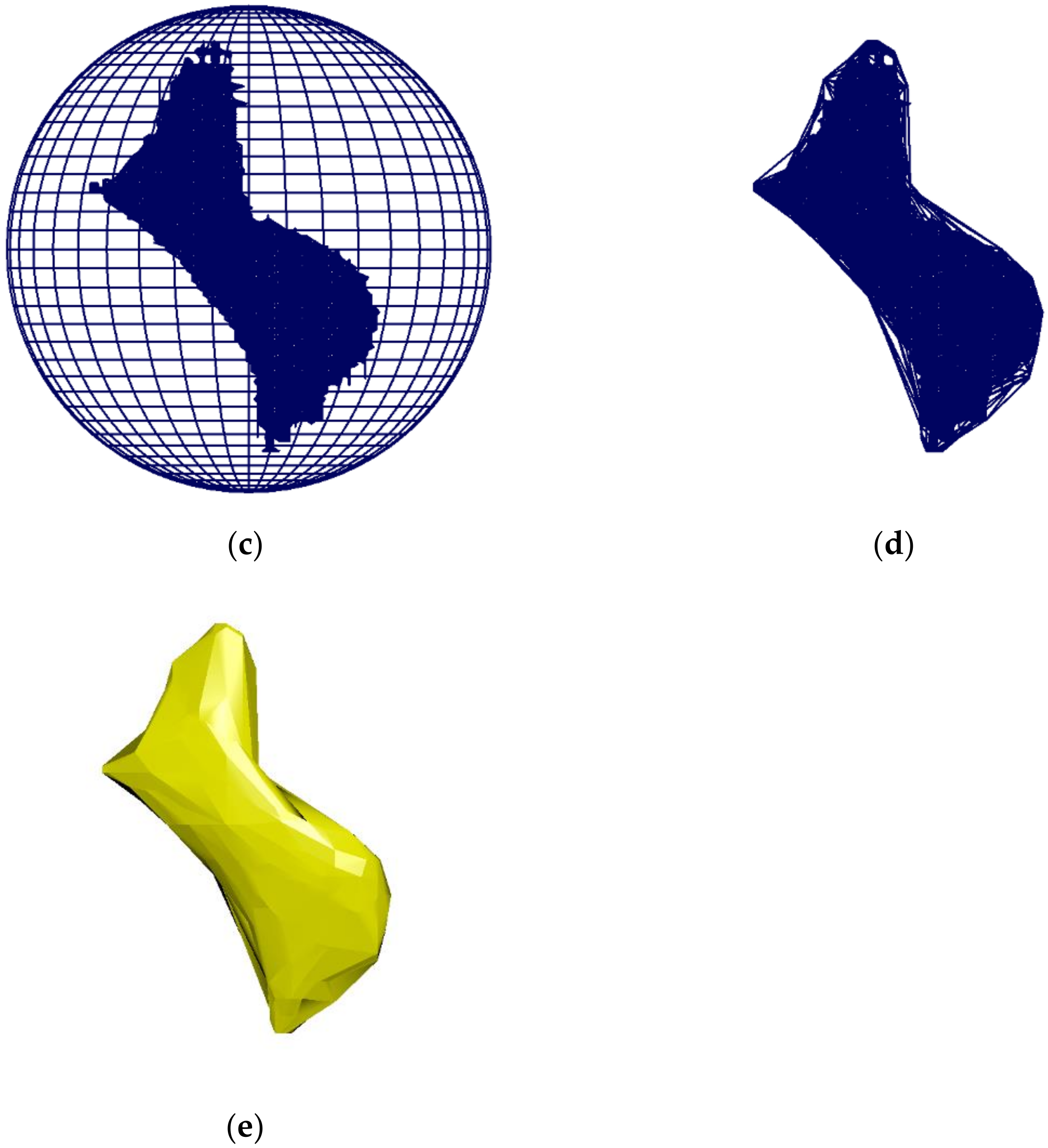
2.6. Measurement of Angles between the Masseter Muscle and the Reference Planes
- -
- Midsagittal plane: Plane through the foramen cecum, falx cerebri, and center of the foramen magnum [20].
- -
- Horizontal plane: Plane through the midpoints of the bilateral eyeball and bilateral orbital canal [21].
- -
- Palatal plane: A plane perpendicular to the midsagittal plane passing through the anterior nasal spine and posterior nasal spine [22].
- -
- Occlusal plane: Plane through half distance point between the incisal edges of the maxillary and mandibular incisors and the mesial cuspid tips of the mandibular bilateral permanent first molars [23].
- -
- Mandibular plane: A plane perpendicular to the midsagittal plane passing through Go (Gonion) and Me (Menton) [24].
2.7. The Reliability of Measurements
2.8. Statistical Analysis
3. Results
3.1. Reliability of Measurements
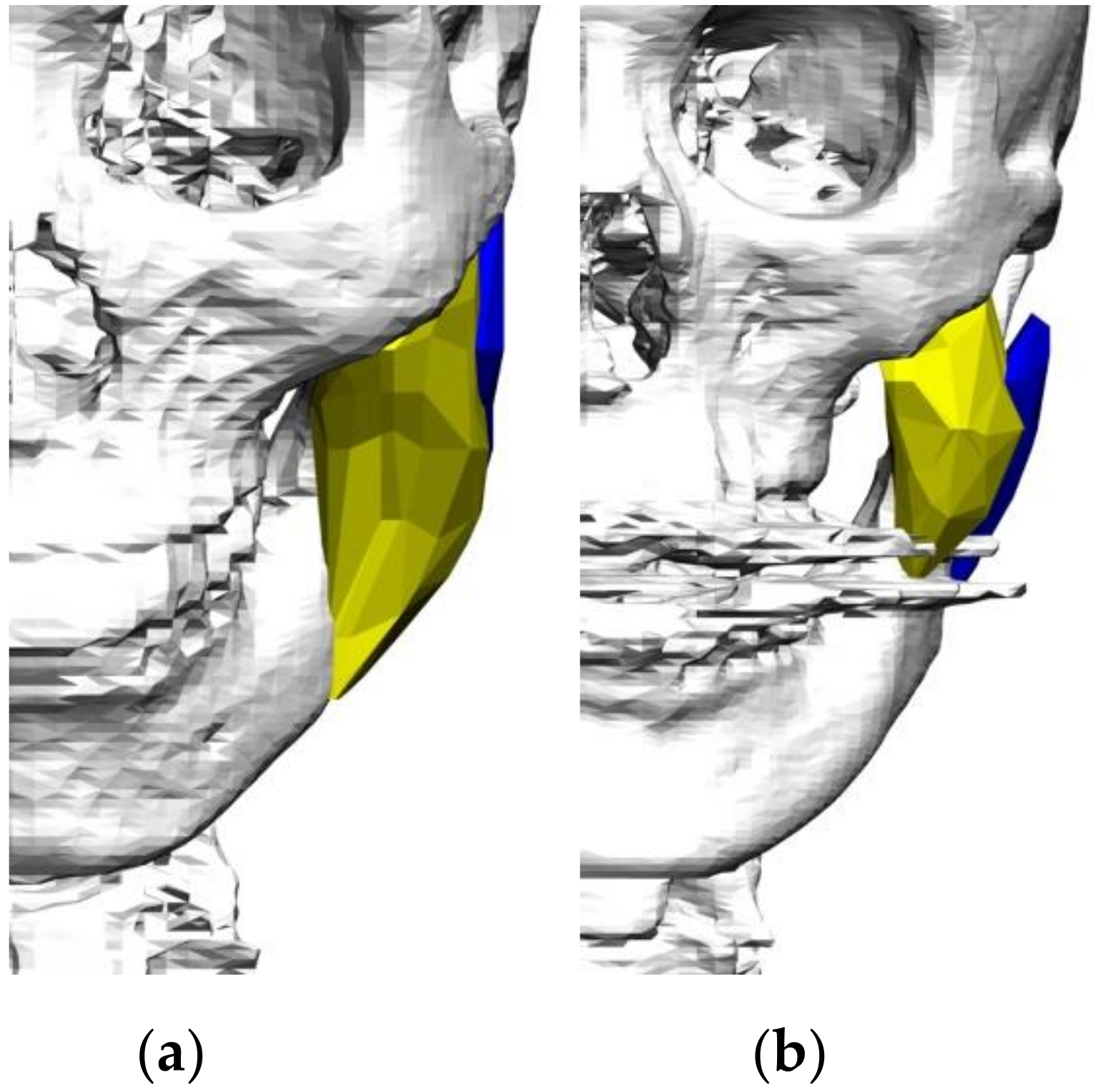
3.2. Comparison of the Masseter Muscle Ratio between the Normal Group and Prognathic Group
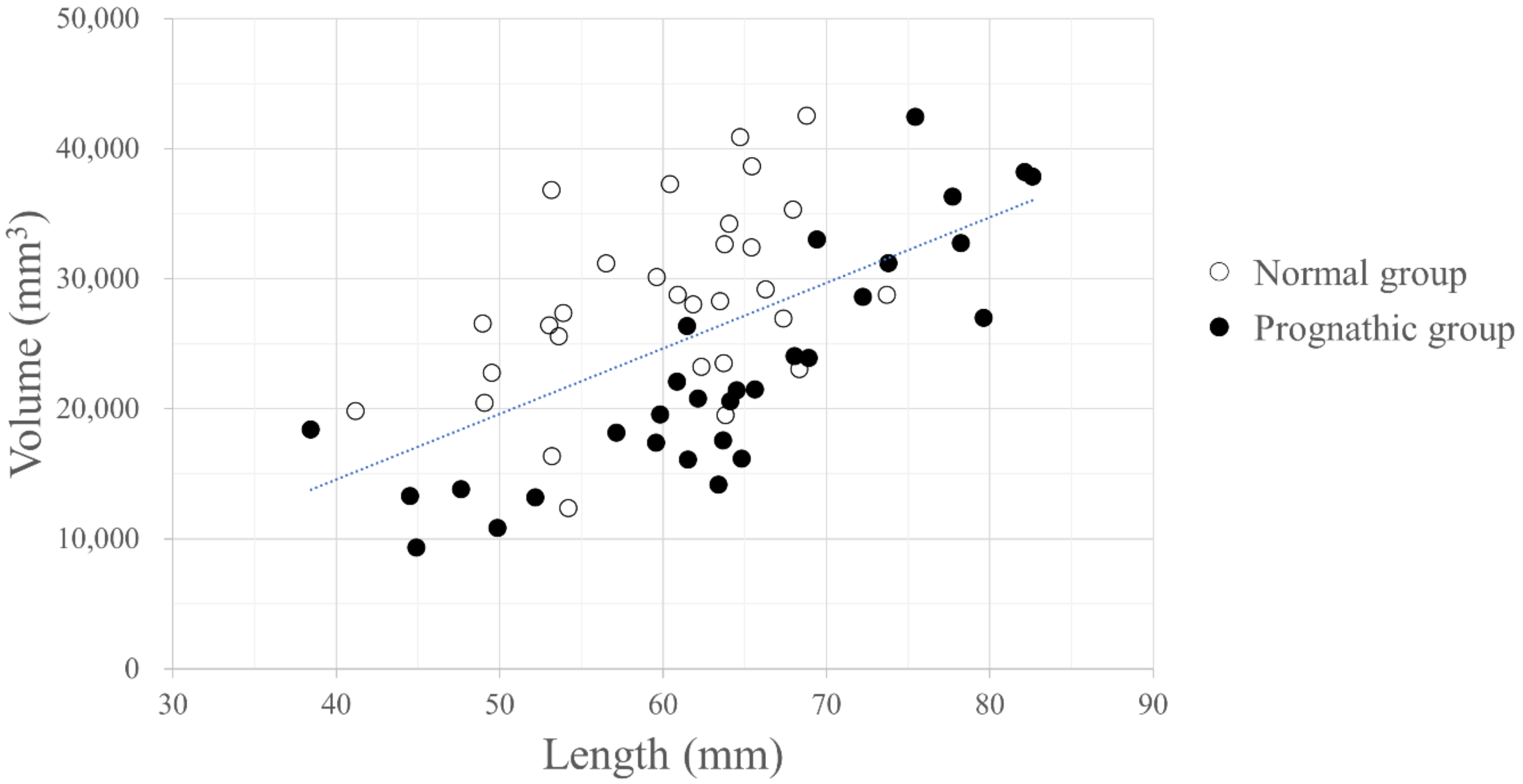
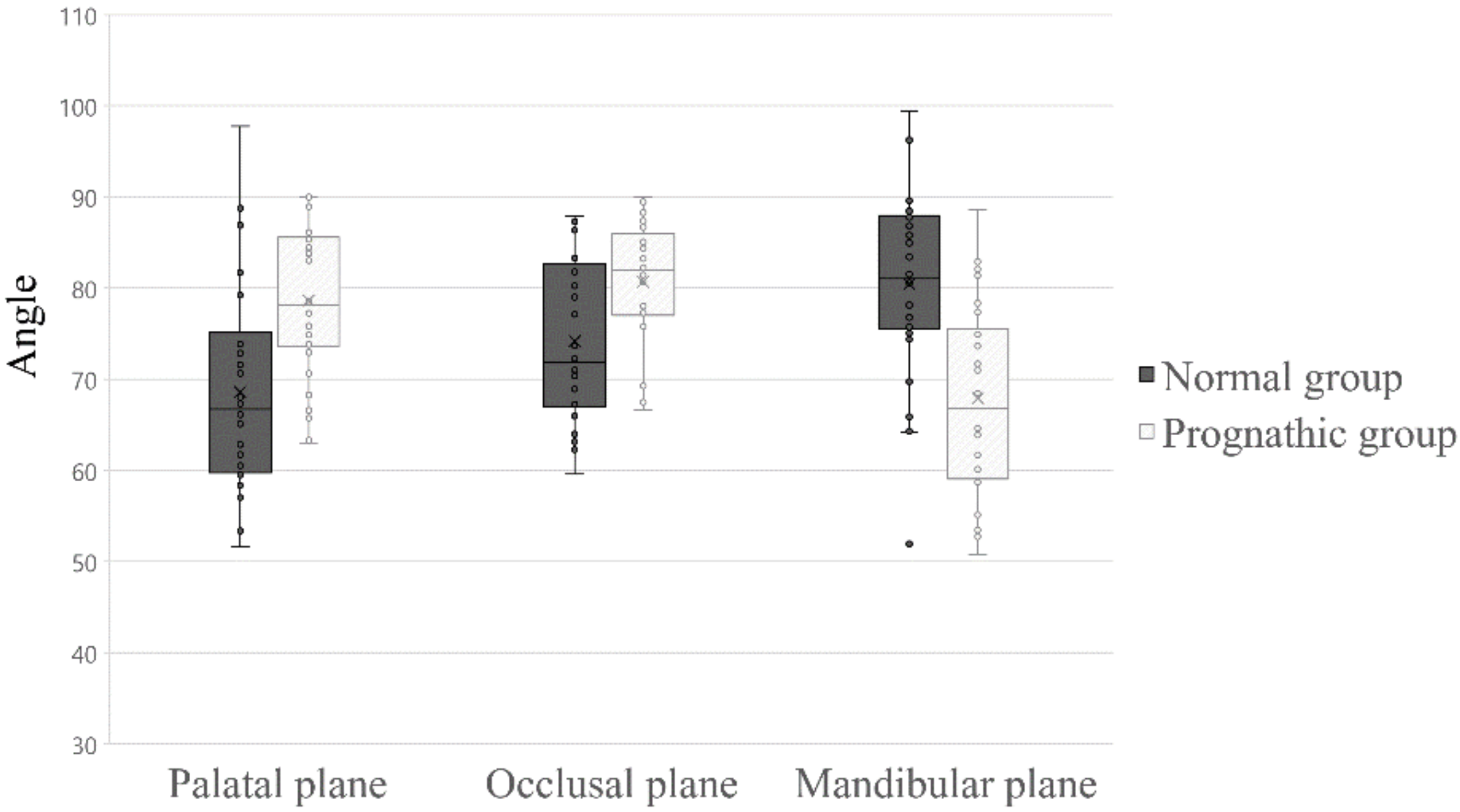
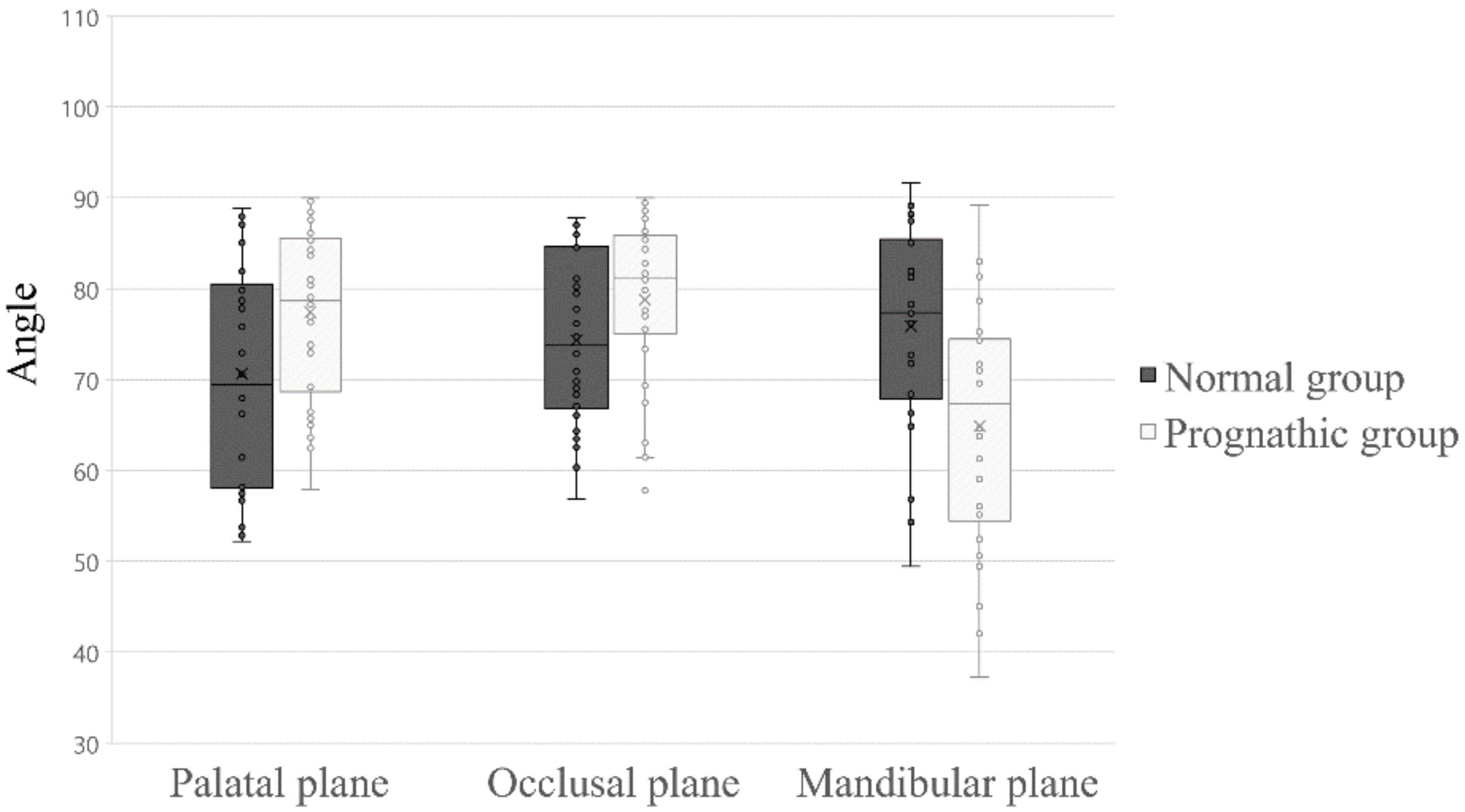
3.3. Comparison of the Angle of the Masseter Muscle Orientation to Three Reference Planes
4. Discussion
5. Conclusions
- (a)
- The volume/length ratio of the masseter of the normal group was greater than that of the prognathic group.
- (b)
- The orientation of both the superficial and deep head of the masseter of the participants in the normal group was more vertical with respect to the mandibular plane than that of the prognathic group.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chang, H.P.; Tseng, Y.C.; Chang, H.F. Treatment of mandibular prognathism. J. Formos. Med Assoc. Taiwan Yi Zhi 2006, 105, 781–790. [Google Scholar] [CrossRef]
- Kim, D.; Choi, E.; Jeong, H.G.; Chang, J.; Youm, S. Expert system for mandibular condyle detection and osteoarthritis classification in panoramic imaging using r-cnn and cnn. Appl. Sci. 2020, 10, 7464. [Google Scholar] [CrossRef]
- Woon, S.C.; Thiruvenkatachari, B. Early orthodontic treatment for class iii malocclusion: A systematic review and meta-analysis. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 28–52. [Google Scholar] [CrossRef] [PubMed]
- Ngan, P.; Moon, W. Evolution of class iii treatment in orthodontics. Am. J. Orthod. Dentofac. Orthop. 2015, 148, 22–36. [Google Scholar] [CrossRef] [PubMed]
- Moss, M.L. A theoretical analysis of the functional matrix. Acta Biotheoretica 1968, 18, 195–202. [Google Scholar] [CrossRef] [PubMed]
- Moss, M.L.; Simon, M.R. Growth of the human mandibular angular process: A functional cranial analysis. Am. J. Phys. Anthropol. 1968, 28, 127–138. [Google Scholar] [CrossRef]
- Ginszt, M.; Zieliński, G.; Berger, M.; Szkutnik, J.; Bakalczuk, M.; Majcher, P. Acute effect of the compression technique on the electromyographic activity of the masticatory muscles and mouth opening in subjects with active myofascial trigger points. Appl. Sci. 2020, 10, 7750. [Google Scholar] [CrossRef]
- Costa, Y.M.; Exposto, F.G.; Castrillon, E.E.; Conti, P.C.R.; Bonjardim, L.R.; Svensson, P. Local anaesthesia decreases nerve growth factor induced masseter hyperalgesia. Sci. Rep. 2020, 10, 15458. [Google Scholar] [CrossRef]
- Bin Heyat, M.B.; Akhtar, F.; Khan, A.; Noor, A.; Benjdira, B.; Qamar, Y.; Abbas, S.J.; Lai, D. A novel hybrid machine learning classification for the detection of bruxism patients using physiological signals. Appl. Sci. 2020, 10, 7410. [Google Scholar] [CrossRef]
- Sella-Tunis, T.; Pokhojaev, A.; Sarig, R.; O’Higgins, P.; May, H. Human mandibular shape is associated with masticatory muscle force. Sci. Rep. 2018, 8, 6042. [Google Scholar] [CrossRef] [PubMed]
- Marques, H.B.; Richter, F.F.; Heck, L.; Xavier, L.L.; de Campos, D. Biomechanical potential of the temporal muscle in brachyfacial and dolichofacial subjects: A study on dry mandibles. Orthod. Craniofac. Res. 2016, 19, 162–168. [Google Scholar] [CrossRef]
- Gionhaku, N.; Lowe, A. Relationship between jaw muscle volume and craniofacial form. J. Dent. Res. 1989, 68, 805–809. [Google Scholar] [CrossRef] [PubMed]
- Kiliaridis, S. Masticatory muscle influence on craniofacial growth. Acta Odontol. Scand. 1995, 53, 196–202. [Google Scholar] [CrossRef]
- Van Spronsen, P.H.; Koolstra, J.H.; van Ginkel, F.C.; Weijs, W.A.; Valk, J.; Prahl-Andersen, B. Relationships between the orientation and moment arms of the human jaw muscles and normal craniofacial morphology. Eur. J. Orthod. 1997, 19, 313–328. [Google Scholar] [CrossRef] [PubMed]
- Mun, S.H.; Park, M.; Lee, J.; Lim, H.J.; Kim, B.C. Volumetric characteristics of prognathic mandible revealed by skeletal unit analysis. Ann. Anat. Anatomischer Anzeiger 2019, 226, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Widmer, C.G.; English, A.W.; Morris-Wiman, J. Developmental and functional considerations of masseter muscle partitioning. Arch. Oral Biol. 2007, 52, 305–308. [Google Scholar] [CrossRef]
- Ringqvist, M. Isometric bite force and its relation to dimensions of the facial skeleton. Acta Odontol. Scand. 1973, 31, 35–42. [Google Scholar] [CrossRef]
- Lee, S.H.; Kil, T.J.; Park, K.R.; Kim, B.C.; Kim, J.G.; Piao, Z.; Corre, P. Three-dimensional architectural and structural analysis—A transition in concept and design from delaire’s cephalometric analysis. Int. J. Oral Maxillofac. Surg. 2014, 43, 1154–1160. [Google Scholar] [CrossRef]
- Parker, W.S. Centric relation and centric occlusion—An orthodontic responsibility. Am. J. Orthod. 1978, 74, 481–500. [Google Scholar] [CrossRef]
- Kim, H.-J.; Kim, B.C.; Kim, J.-G.; Zhengguo, P.; Kang, S.H.; Lee, S.-H. Construction and validation of the midsagittal reference plane based on the skull base symmetry for three-dimensional cephalometric craniofacial analysis. J. Craniofacial Surg. 2014, 25, 338–342. [Google Scholar] [CrossRef]
- Kang, Y.; Kim, B.; Park, K.; Yon, J.; Kim, H.; Tak, H.; Piao, Z.; Kim, M.; Lee, S. Visual pathway-related horizontal reference plane for three-dimensional craniofacial analysis. Orthod. Craniofacial Res. 2012, 15, 245–254. [Google Scholar] [CrossRef]
- Nahoum, H.I. Vertical proportions and the palatal plane in anterior open-bite. Am. J. Orthod. 1971, 59, 273–282. [Google Scholar] [CrossRef]
- Del Santo, M., Jr. Influence of occlusal plane inclination on anb and wits assessments of anteroposterior jaw relationships. Am. J. Orthod. Dentofac. Orthop. 2006, 129, 641–648. [Google Scholar] [CrossRef]
- Nelson, C.; Harkness, M.; Herbison, P. Mandibular changes during functional appliance treatment. Am. J. Orthod. Dentofac. Orthop. 1993, 104, 153–161. [Google Scholar] [CrossRef]
- Bakke, M.; Tuxetv, A.; Vilmann, P.; Jensen, B.R.; Vilmann, A.; Toft, M. Ultrasound image of human masseter muscle related to bite force, electromyography, facial morphology, and occlusal factors. Eur. J. Oral Sci. 1992, 100, 164–171. [Google Scholar] [CrossRef] [PubMed]
- Kiliaridis, S.; Kälebo, P. Masseter muscle thickness measured by ultrasonography and its relation to facial morphology. J. Dent. Res. 1991, 70, 1262–1265. [Google Scholar] [CrossRef]
- Biondi, K.; Lorusso, P.; Fastuca, R.; Mangano, A.; Zecca, P.; Bosco, M.; Caprioglio, A.; Levrini, L. Evaluation of masseter muscle in different vertical skeletal patterns in growing patients. Eur. J. Paediatr. Dent. 2016, 17, 47–52. [Google Scholar]
- Kasai, K.; Richards, L.; Kanazawa, E.; Ozaki, T.; Iwasawa, T. Relationship between attachment of the superficial masseter muscle and craniofacial morphology in dentate and edentulous humans. J. Dent. Res. 1994, 73, 1142–1149. [Google Scholar] [CrossRef]
- Sondang, P.; Kumagai, H.; Tanaka, E.; Ozaki, H.; Nikawa, H.; Tanne, K.; Hamada, T. Correlation between maximum bite force and craniofacial morphology of young adults in indonesia. J. Oral Rehabil. 2003, 30, 1109–1117. [Google Scholar] [CrossRef]
- Iwase, M.; Ohashi, M.; Tachibana, H.; Toyoshima, T.; Nagumo, M. Bite force, occlusal contact area and masticatory efficiency before and after orthognathic surgical correction of mandibular prognathism. Int. J. Oral Maxillofac. Surg. 2006, 35, 1102–1107. [Google Scholar] [CrossRef]
- Kitai, N.; Fujii, Y.; Murakami, S.; Furukawa, S.; Kreiborg, S.; Takada, K. Human masticatory muscle volume and zygomatico-mandibular form in adults with mandibular prognathism. J. Dent. Res. 2002, 81, 752–756. [Google Scholar] [CrossRef]
- Park, J.C.; Lee, J.; Lim, H.J.; Kim, B.C. Rotation tendency of the posteriorly displaced proximal segment after vertical ramus osteotomy. J. Cranio-Maxillo-Facial Surg. 2018, 46, 2096–2102. [Google Scholar] [CrossRef] [PubMed]
- Katsaros, S.K.C. The effects of myotonic dystrophy and duchenne muscular dystrophy on the orofacial muscles and dentofacial morphology. Acta Odontol. Scand. 1998, 56, 369–374. [Google Scholar] [CrossRef]
- Hong, S.W.; Kang, J.H. Decreased mandibular cortical bone quality after botulinum toxin injections in masticatory muscles in female adults. Sci. Rep. 2020, 10, 3623. [Google Scholar] [CrossRef] [PubMed]
- Inman, K.E.; Purcell, P.; Kume, T.; Trainor, P.A. Interaction between foxc1 and fgf8 during mammalian jaw patterning and in the pathogenesis of syngnathia. PLoS Genet. 2013, 9, e1003949. [Google Scholar] [CrossRef]
- Kim, T.H.; Kim, C.H. Correlation between mandibular morphology and masticatory muscle thickness in normal occlusion and mandibular prognathism. J. Korean Assoc. Oral Maxillofac. Surg. 2020, 46, 313–320. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.H.; Lee, H.; Hwang, J.J.; Jung, H.D.; Hwang, C.J.; Cha, J.Y. Differences in soft-tissue thickness changes after bimaxillary surgery between patients with vertically high angle and normal angle. Am. J. Orthod. Dentofac. Orthop. 2021, 159, 30–40. [Google Scholar] [CrossRef]
- Lee, Y.S.; Kim, Y.K.; Yun, P.Y.; Larson, B.E.; Lee, N.K. Comparison of the stability after mandibular setback with minimal orthodontics of class iii patients with different facial types. J. Oral Maxillofac. Surg. 2016, 74, e1461–e1464. [Google Scholar] [CrossRef]

| Normal Group (n = 30) | Prognathic Group (n = 30) | p Value | |
|---|---|---|---|
| Ratio | 472.6 ± 105.6 | 350.0 ± 90.0 | 0.000 * |
| Normal Group (n = 30) | Prognathic Group (n = 30) | p Value | ||
|---|---|---|---|---|
| Masseter (Superficial) | Palatal plane | 68.6 ± 11.7 | 78.7 ± 8.2 | 0.000 * |
| Occlusal plane | 74.2 ± 8.6 | 80.7 ± 7.0 | 0.002 * | |
| Mandibular Plane | 80.4 ± 10.2 | 68.0 ± 10.1 | 0.000 * | |
| Masseter (Deep) | Palatal plane | 70.7 ± 12.0 | 77.4 ± 9.3 | 0.018 * |
| Occlusal plane | 74.3 ± 9.3 | 78.8 ± 9.1 | 0.066 | |
| Mandibular plane | 75.9 ± 11.0 | 64.9 ± 13.1 | 0.001 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, J.H.; Shin, D.S.; Yoo, J.-H.; Lim, H.J.; Lee, J.; Kim, B.C. Anatomical Characteristics of the Masseter Muscle in Mandibular Prognathism. Appl. Sci. 2021, 11, 4444. https://doi.org/10.3390/app11104444
Yang JH, Shin DS, Yoo J-H, Lim HJ, Lee J, Kim BC. Anatomical Characteristics of the Masseter Muscle in Mandibular Prognathism. Applied Sciences. 2021; 11(10):4444. https://doi.org/10.3390/app11104444
Chicago/Turabian StyleYang, Ji Ho, Dong Sun Shin, Jeong-Hun Yoo, Hun Jun Lim, Jun Lee, and Bong Chul Kim. 2021. "Anatomical Characteristics of the Masseter Muscle in Mandibular Prognathism" Applied Sciences 11, no. 10: 4444. https://doi.org/10.3390/app11104444
APA StyleYang, J. H., Shin, D. S., Yoo, J.-H., Lim, H. J., Lee, J., & Kim, B. C. (2021). Anatomical Characteristics of the Masseter Muscle in Mandibular Prognathism. Applied Sciences, 11(10), 4444. https://doi.org/10.3390/app11104444






