Abstract
The purpose of this article is to evaluate the amount of the relapse of anterior crowding and the efficacy of retention appliances by reviewing the best available scientific evidence. A survey of articles published up to November 2019 about the stability of dental alignment and retention after fixed orthodontic treatment was performed using seven electronic databases. Study Selection: Only randomized clinical trials investigating patients previously treated with multi-bracket appliances with a follow-up period longer than 6 months were included. Data Extraction: Two authors independently performed the study selection, data extraction, and risk of bias assessment. All pooled data analyses were performed using a random-effects model. Statistical heterogeneity was evaluated. In total, eight randomized clinical trials (RCTs) were included, grouping data from 987 patients. The ages of the patients varied across the studies, ranging between 13 and 17 years. The observation period ranged between 6 and 24 months. The data showed no significant intercanine width modifications during the retention period with both fixed and removable retainers. A significant modification of Little’s Index was found for the mandibular removable retainers with a mean difference of 0.72 mm (95% Cl, 0.47 to 0.98) and for the maxillary removable retainers with a mean difference of 0.48 mm (95% Cl, 0.27 to 0.68). No significant changes were found by evaluating Little’s Index modification for the mandibular fixed retainers. The results of this meta-analysis showed that all the considered retainers were effective in maintaining dental alignment after fixed orthodontic treatment. However, fixed retainers showed greater efficacy compared to removable retainers.
1. Introduction
Stable tooth position after orthodontic treatment is considered a treatment goal. However, evidence shows that the majority of orthodontic treatments move teeth from a stable to an unstable position [1]. In this way, the use of a retainer is considered the only method able to maintain occlusal results [2]. Post-treatment tooth stability can be affected by several different factors, including bone and soft tissue development [3], primary crowding [4,5,6], dental eruption [7], modification of arch form [8], post-treatment occlusion [9], and the characteristics of pre-treatment malocclusion [10]. Retention can be performed by placing removable or fixed retainers. A recent Cochrane review reported a lack of evidence concerning the effectiveness different retention methods [11]. The efficacy of different retention appliances is of great interest for clinicians to support clinical retention protocols [12,13,14]. The literature does not provide meta-analytic data reporting and comparing the amount of relapse that occurs when using different retention appliances. The aim of this systematic review and meta-analysis was to evaluate the amount of relapse of anterior crowding and consequently to evaluate the efficacy of retention appliances used after fixed orthodontic treatment according to the best scientific evidence available [15].
2. Materials and Methods
The present systematic review with meta-analysis was performed according to the guidelines provided by the Cochrane Handbook for Systematic Reviews of Interventions (version 5.1.0) and was reported according to the PRISMA statement [16,17,18,19]. The protocol of this meta-analysis was preliminary registered on PROSPERO (https://www.crd.york.ac.uk/prospero/). Two authors independently carried out the selection of the studies, data collection, and the assessment of the risk of bias. Any disagreement was resolved by discussion with a third author. The level of agreement between the 2 reviewers was assessed by Cohen kappa statistics, for which a threshold value of 0.90 was preset.
2.1. Information Sources and Search
A survey of articles published up to November 2019 on stability and retention after orthodontic treatment was performed using several electronic databases (Table 1).

Table 1.
Performed electronic searches.
Previous systematic reviews and meta-analyses on this topic were also identified, and their reference lists were scanned to find additional trials. No restriction was applied to language, publication year, or status.
2.2. Selection of Studies
Duplicated reports were preliminary excluded. All retrieved records were screened on the basis of their titles and abstracts, and the full texts of the remaining articles were assessed for eligibility in the final analysis.
Studies were considered eligible if they met the following criteria (reported according to the PICO format): clinical trials on human subjects, orthodontic patients treated with multi-bracket appliances with no craniofacial deformity (population), orthodontic retention performed with fixed or removable retainers (intervention), a comparable control group (control group), results analyzed at the beginning of retention and after a follow-up period longer than 6 months (outcomes measured), and analyzed treatment effects that were not influenced by concomitant and/or additional therapeutic procedures.
2.3. Data Extraction and Management
A data extraction form was developed to collect the characteristics (study design, type of retention appliance, sample size, age, sex, orthodontic treatment characteristics, setting, observation time, type of measurements, and follow-up) and outcomes from the included studies. Relapse after orthodontic treatment was investigated by using two parameters: Little’s Irregularity Index (LII) for assessment of the degree of crowding and intercanine width for assessment of the transversal anterior dental arch width.
2.4. Assessment of Risk of Bias
The risk of bias assessment was performed using the Cochrane Collaboration’s risk of bias tool (Review Manager version 5.2; Nordic Cochrane Centre, Cochrane Collaboration, Copenhagen, Denmark, 2012). Each randomized clinical trial (RCT) was assigned an overall risk of bias rating: low risk (low for all key domains), high risk (high for ≥1 key domain), or unclear risk (unclear for ≥1 key domain).
2.5. Summary Measures and Data Analysis
Two outcomes were considered for the meta-analytic analysis: Little’s Irregularity Index and Intercanine width. The published clinical trials evaluating retention protocols do not have a control group with un-retained patients for ethical reasons. As a consequence, all the published trials compare two or more treatment protocols. In order to obtain a quantitative estimation of occlusal changes occurred with different retention protocols, we considered the single-arm data of clinical trials as the data obtained from case-series studies, and we performed a meta-analysis extrapolating and combining these data. In terms of data characteristics, the single-arm data from the RCTs and case series studies data are equivalent, as both studies report data with a mean value and standard deviation. However, the data extrapolated from the single-arm RCTs present less bias compared to the data from the case series studies. Finally, our strategy was supported by the literature. Indeed, when clinical trials with untreated control groups are not available, case-series studies without a control group can be used to perform a meta-analysis [20,21,22].
The considered effects size used for the meta-analysis was the difference between the outcome values at the end of treatment with fixed appliances and the outcome values after the retention period. Some studies reported the interquartile range rather than standard deviation, and the data extracted from those studies were properly adjusted [23]. The mean differences (MDs) and their corresponding 95% confidence intervals (95% Cls) were used to summarize and combine the data. A random-effects model was applied to estimate all the pooled data. This analysis was performed by means of the OpenMeta [Analyst] computer program (http://www.cebm.brown.edu/openmeta/) [24]. A third outcome (i.e., the fixed retainer failure rate) was considered only for qualitative evaluation.
2.6. Assessment of Heterogeneity
Clinical heterogeneity was evaluated by examining the types of participants and the interventions for the outcome in each included study. For all analyses, heterogeneity was assessed with the I2 index, which is an indicator of true heterogeneity in percentages [14,15,16,17,18,19].
2.7. Assessment of Quality of Evidence
The quality of evidence was assessed using the Grades of Recommendation, Assessment, Development, and Evaluation Pro software (GRADEPro) [25]. The strength of the recommendation for each outcome investigated was assessed using the Strength of Recommendation Taxonomy (SORT) Grading system [26], which addresses the issue of patient-oriented (effectiveness) versus disease-oriented evidence (efficacy). POEMs (patient oriented evidence that matters) allows clinicians to filter information from the medical literature and focus only on what is in fact important for the patient [26].
2.8. Sensitivity Analysis
A sensitivity analysis was conducted to evaluate the LII modification in the lower arch with the mandibular removable retention appliances, excluding the RCT with the highest risk of bias (Figure S1).
3. Results
3.1. This Study Selection
Figure 1 shows the flow diagram for the selection of studies. Supplementary Table S1 reports the number of excluded studies and the reasons for exclusion. Eleven studies [21,22,23,24,25,26,27,28,29,30,31] were selected for the qualitative analysis and eight studies for the final quantitative synthesis [21,22,23,24,25,26,27,28] (Table 1). The inter-reviewer agreements for study selection were suitable, with a kappa value of 0.987.
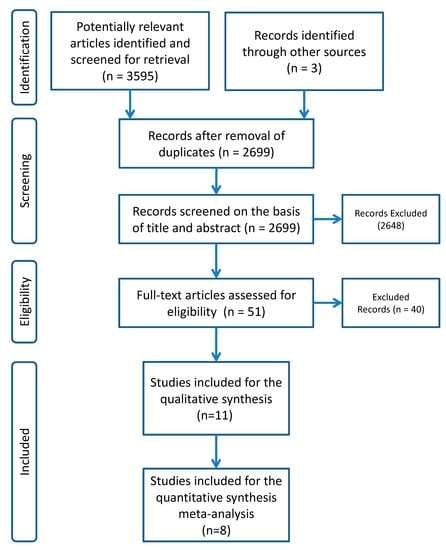
Figure 1.
Flow Chart.
3.2. Study Characteristics
The characteristics of the 11 RCTs included for the qualitative synthesis are summarized in Table 2. All eight RCTs selected for the meta-analysis evaluated the efficacy of different type of retention appliances (both removable and fixed) after orthodontic treatment with a multi-bracket appliance; the majority of trials took place in university settings. The total number of pooled observed patients was 987. Six studies [27,30,31,32,33,34] included both male and female participants, while in two studies [28,31], the authors did not specify the numbers of male and female participants. Five studies [27,29,30,33,34] reported the patients’ ages, with an age range between 13 and 17 years. The appliance features were heterogeneous among the selected studies: Six trials evaluated the effects of vacuum-formed retainers [27,30,31,32,33,34], four trials evaluated the effects of bonded fixed retainers [27,28,29,30,31], two trials evaluated the effects of a Hawley retainer [33,34], one trial evaluated the effects of a Begg retainer [31], and one trial evaluated the effects of a positioner [27].

Table 2.
Study characteristics.
Seven studies [27,29,30,32,33,34] reported the percentage of patients treated with or without extraction, as shown in Table 2. The times of daily wear for the removable appliances (vacuum-formed retainers, Hawley retainers, Begg retainers, and positioners) varied between full-time and night-time among the RCTs, and the observation time varied from 6 to 24 months. The inter-reviewer agreements for study selection were suitable, with a kappa value of 0.968.
3.3. Risk of Bias Assessment
Although we took only single arm data from the selected studies to perform the meta-analysis, all the pooled data come from RCTs. Therefore, in order to assess the risk of bias, we had to assess the methodological quality of the RCTs; we used the Cochrane Collaboration tool, which is considered the gold standard for this purpose (Table S1). Among the eight studies included for the quantitative synthesis and meta-analysis, only 1 RCT was evaluated to have a high risk of bias [34]. In two RCTs, the risk of bias was unclear [31,33], and five RCTs had a low risk of bias [26,27,28,29,30,32] (Table 3). Consequently, the summary assessments of risk of bias across the studies were considered to be low. The inter-reviewer agreements for risk of bias assessment were suitable, with kappa values of 0.925. Publication bias was not assessed as there were inadequate numbers of included trials to properly develop a funnel plot or more advanced regression-based assessments.

Table 3.
Risk of bias assessment.
3.4. Quantitative Data Synthesis
The data showed that the mean difference of intercanine width during the retention period was 0.05 mm (95% Cl, −0.41 to 0.51; P = 0.84; I2 = 99%) for the mandibular fixed retainers (Figure 2a), 0.01 mm (95% Cl, −0.26 to 0.28; P = 0.95; I2 = 100%) for the mandibular removable retainers (Figure 2b), and −0.13 mm (95% Cl, −0.52 to 0.27; P = 0.53; I2 = 99%) for the maxillary removable retainers (Figure 2c). The mean difference of Little’s Index during the retention period was 0.48 mm (95% Cl, −0.04 to 1.01; P = 0.07; I2 = 98%) for the mandibular fixed retainers (Figure 2d), 0.73 mm (95% Cl, 0.47 to 0.98; P = 0.00001; I2 = 100%) for the mandibular removable retainers (Figure 2e), and 0.48 mm (95% Cl, 0.27 to 0.68; P = 0.00001; I2 = 91%) for the maxillary removable retainers (Figure 2f).
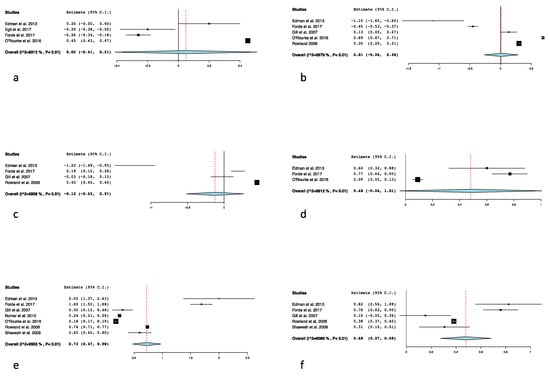
Figure 2.
(a) Forest plot of the intercanine width modification: mandibular fixed retainers; (b) mandibular removable retainers; (c) maxillary removable retainers; (d) forest plot of the Little’s Index modification: mandibular fixed retainers; (e) mandibular removable retainers; (f) maxillary removable retainers.
3.5. Fixed Retainer Failure Rate
Among the 11 studies included for qualitative synthesis, four RCTs [28,35,36,37] reported the failure rate of the fixed retainers during the observation period. The summarized failure rate was 41.3% (72/174) for the maxillary arch and 36.7% (115/313) for the mandibular arch (Table 4). Among the four studies, only one RCT had a high risk of bias [35]. For two RCTs, the risk of bias was unclear [36,37], and one RCT had a low risk of bias [28] (Table 3).

Table 4.
Fixed retainer failure rate.
3.6. Assessment of Quality of Evidence
According to the GRADE [25], there was low level of evidence for all the LII outcomes (Table 5) and for the mandibular and maxillary intercanine width outcomes with both fixed and removable retainers (Table 6). According to the SORT approach [26], the strength of the recommendations was classified as A for LII and C for intercanine width (Table 7).

Table 5.
Should fixed retainers or removable retainers be used for maintaining the alignment of anterior teeth?

Table 6.
Should fixed retainers or removable retainers be used for maintaining intercanine width?

Table 7.
Strength of recommendations for each outcome investigated in the present study.
4. Discussion
To the best of our knowledge, this is the first review with meta-analysis that investigates the current literature with the best evidence (RCTs) on the efficacy of orthodontic retainers to maintain the occlusal results after fixed orthodontic treatment. The results of this meta-analysis will provide clinicians a quantitative evaluation of the efficacy of fixed and removable retainers and consequently a quantitative evaluation of orthodontic relapse during the retention period.
The pooled data show that the intercanine width does not change significantly during retention with all evaluated retention appliances [37,38,39,40,41,42,43,44].
The data show that the fixed retainers are also able to avoid significant modifications of LII (p = 0.07). However, this datum should be interpreted with caution because of the fewer number of considered trials. Conversely, the use of removable retainers showed a significant increase of LII. This datum was obtained by pooling the data from five trials for the maxillary arch (Figure 2f) and from seven trials for the mandibular arch (Figure 2e); it can be considered a consistent meta-analytic datum. The amount of variation for LII is 0.48 and 0.72 mm, respectively, for the maxillary and mandibular arch. This result clearly shows that, despite the use of a removable retainer appliance, the teeth of both arches present a small statistically significant (but clinically insignificant) alignment alteration. These results, especially for intercanine width, must be interpreted with caution due to the young age of the sample participants, as this type of alteration can influence the outcome due to residual growth and patient compliance.
Interestingly, our data show a significant alteration of LII in the absence of modification of the intercanine width. These results could be explained by interpreting the alteration of LII as a consequence of a single tooth rotational relapse, rather than a transversal inter-canine diameter relapse. The reported modifications of LII could be related to specific factors associated with the use of removable retainers, such as patient compliance and the limitations of using retainers nocturnally. This last hypothesis, however, does not seem to be supported by the evidence. Indeed, one of the considered RCTs compared removable retainers used full time and removable retainers used part-time [45,46,47,48,49,50,51,52,53,54,55]. The authors did not find significant differences in terms of relapse after 12 months of retention.
Compliance is certainly an issue related to removable retainers. However, the results of this review clearly show that fixed retainers are not free of issues. In fact, the failure rate of fixed retainers (caused by wire breakage or bonding failure) is, on average, 41% and 36% for maxillary and mandibular retainers, respectively (Table 4). These data are in accordance with previously published data [14,56,57,58,59,60,61].
One limitation of this meta-analysis is the small number of included trials; this aspect affected the I2 index, undervaluing the extent of between-study heterogeneity [62,63]. The I2 values reported a high total variation across the studies, with a mean value and a standard deviation equal to 97.8% and 2.2%, respectively. This variation was assumed to be due to the clinical heterogeneity of the different appliances used in the considered RCTs. Moreover, the source of heterogeneity could be related to other factors such as patient compliance, final occlusal results, orthodontist expertise, type of malocclusion, and type of treatment (with or without extractions) [13,64,65,66,67,68,69,70,71,72,73,74,75,76,77].
The I2 values potentially affected the level of evidence of our findings, which ranged from very low to low, according to the GRADE approach. Although we selected only published trials offering the highest level of evidence (RCTs), the GRADE score showed that the included studies provided, in most cases, a very low quality of evidence (Table 5 and Table 6). This result should be assessed while considering the difficulties in conducting RCTs for orthodontics [46].
All these aspects increased the heterogeneity of the different clinical trials and, consequently, contributed to limiting the methodological GRADE score of the orthodontic trials.
The SORT approach (Table 7) revealed a high strength of recommendations for the LII outcome and a poor strength of recommendations for the intercanine width outcome, likely because the LII represents a clinical outcome that directly affect smile aesthetics and appearance (i.e., a patient-oriented outcome).
The sensitivity analysis showed a similar outcome compared with the results of this meta-analysis for the same parameter (0.74) (95% Cl, 0.47 to 1.01; P = 0.00001; I2 = 100%), confirming the validity of the performed meta-analysis.
5. Conclusions
The results of this meta-analysis show that all the considered retainers are effective in maintaining dental alignment after fixed orthodontic treatment. However, the fixed retainers showed greater efficacy than the removable retainers.
The most important issues for fixed and removable retainers are, respectively, the risk of failure and patient compliance. Further RCT studies with longer observation periods are needed in order to assess the long-term efficacy of orthodontic retainers.
Supplementary Materials
The following are available online at https://www.mdpi.com/2076-3417/10/9/3107/s1, Table S1: Excluded articles with reason for exclusion. Figure S1: Sensitivity analysis.
Author Contributions
Conceptualization, A.L.G. and L.R.; methodology, M.P., G.I.; software, V.R.; writing—original draft preparation, writing—review and editing R.N. and G.I. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Little, R.M.; Wallen, T.R.; Riedel, R.A. Stability and relapse of mandibular anterior alignment—First premolar extraction cases treated by traditional edgewise orthodontics. Am. J. Orthod. 1981, 80, 349–365. [Google Scholar] [CrossRef]
- Blake, M.; Bibby, K. Retention and stability: A review of the literature. Am. J. Orthod. Dentofac. Orthop. 1998, 114, 299–306. [Google Scholar] [CrossRef]
- Nucera, R.; Lo Giudice, A.; Bellocchio, M.; Spinuzza, P.; Caprioglio, A.; Cordasco, G. Diagnostic concordance between skeletal cephalometrics, radiographbased soft-tissue cephalometrics, and photograph-based soft-tissue cephalometrics. Eur. J. Orthod. 2017, 39, 352–357. [Google Scholar] [PubMed]
- Lo Giudice, A.; Nucera, R.; Leonardi, R.; Paiusco, A.; Baldoni, M.; Caccianiga, G. A Comparative Assessment of the Efficiency of Orthodontic Treatment with and without Photobiomodulation during Mandibular Decrowding in Young Subjects: A Single-Center, Single-Blind Randomized Controlled Trial. Photobiomodul Photomed. Laser Surg. 2020. [Google Scholar] [CrossRef] [PubMed]
- Richardson, M.E. Late lower arch crowding in relation to primary crowding. Angle Orthod. 1982, 44, 56–61. [Google Scholar]
- Lo Giudice, A.; Nucera, R.; Perillo, L.; Paiusco, A.; Caccianiga, G. Is low-level laser therapy an effective method to alleviate pain induced by active orthodontic alignment archwire? A randomized clinical trial. J. Evid. Based Dent. Prac. 2019, 19, 71–78. [Google Scholar] [CrossRef]
- Richardson, M.E. Late lower arch crowding in relation to the direction of eruption. Eur. J. Orthod. 1996, 18, 341–347. [Google Scholar] [CrossRef]
- Bondemark, L.; Holm, A.K.; Hansen, K.; Axelsson, S.; Mohlin, B.; Brattstrom, V.; Paulin, G.; Pietila, T. Long term stability of orthodontic treatment and patient satisfaction: A systematic review. Angle Orthod. 2007, 77, 181–191. [Google Scholar] [CrossRef]
- Weiland, F. The role of occlusal discrepancies in the long-term stability of the mandibular arch. Eur. J. Orthod. 1994, 16, 521–529. [Google Scholar] [CrossRef]
- Little, R.M.; Riedel, R.A. Postretention evaluation of stability and relapse—Mandibular arches with generalized spacing. Am. J. Orthod. Dentofac. Orthop. 1989, 95, 37–41. [Google Scholar] [CrossRef]
- Littlewood, S.J.; Millett, D.T.; Doubleday, B.; Bearn, D.R.; Worthington, H.V. Retention procedures for stabilising tooth position after treatment with orthodontic braces. Cochrane Database Syst. Rev. 2016. [Google Scholar] [CrossRef]
- Al-Moghrabi, D.; Pandis, N.; Fleming, P.S. The effects of fixed and removable orthodontic retainers: A systematic review. Prog. Orthod. 2016, 17, 24. [Google Scholar] [CrossRef] [PubMed]
- Nucera, R.; Gatto, E.; Borsellino, C.; Aceto, P.; Fabiano, F.; Matarese, G.; Perillo, L.; Cordasco, G. Influence of bracket-slot design on the forces released by superelastic nickel-titanium alignment wires in different deflection configurations. Angle Orthod. 2014, 84, 541–547. [Google Scholar] [CrossRef] [PubMed]
- Lo Giudice, G.; Lo Giudice, A.; Isola, G.; Fabiano, F.; Artemisia, A.; Fabiano, V.; Nucera, R.; Matarese, G. Evaluation of bond strength and detachment interface distribution of different bracket base designs. Acta Med. Mediterr. 2015, 31, 585–590. [Google Scholar]
- Papadopoulos, M.A. Meta-analysis in evidence-based orthodontics. Orthod. Craniofac. Res 2003, 6, 112–126. [Google Scholar] [CrossRef]
- Nucera, R.; Militi, A.; Lo Giudice, A.; Longo, V.; Fastuca, R.; Caprioglio, A.; Cordasco, G.; Papadopoulos, M.A. Skeletal and Dental Effectiveness of Treatment of Class II Malocclusion with Headgear: A Systematic Review and Meta-analysis. J. Evid. Based Dent. Prac. 2018, 18, 41–58. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Green, S. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions, (version 5.1.0, updated March 2016); The Cochrane Collaboration: London, UK, 2016. [Google Scholar]
- Nucera, R.; Lo Giudice, A.; Rustico, L.; Matarese, G.; Papadopoulos, M.A.; Cordasco, G. Effectiveness of orthodontic treatment with functional appliances on maxillary growth in the short term: A systematic review and meta-analysis. Am. J. Orthod. Dentofac. Orthop. 2016, 149, 600–611.e3. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gotzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J. Clin. Epidemiol. 2009, 62, e1–e34. [Google Scholar] [CrossRef]
- Fitzpatrick-Lewis, D.; Ciliska, D.; Thomas, H. The Methods for the Synthesis of Studies without Control Groups; National Collaborating Centre for Methods and Tools: Hamilton, ON, Canada, 2009. [Google Scholar]
- Chambers, D.; Rodgers, M.; Woolacott, N. Not only randomized controlled trials, but also case series should be considered in systematic reviews of rapidly developing technologies. J. Clin. Epidemiol. 2009, 62, 1253–1260.e4. [Google Scholar] [CrossRef]
- Dalziel, K.; Round, A.; Stein, K.; Garside, R.; Castelnuovo, E.; Payne, L. Do the findings of case series studies vary significantly according to methodological characteristics? Health Technol Assess. 2005, 9, 1–148. [Google Scholar] [CrossRef]
- Hozo, S.L.; Djulbegovic, B.; Hozo, I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med. Res. Methodol. 2005, 5, 13. [Google Scholar] [CrossRef] [PubMed]
- Wallace, B.C.; Dahabreh, I.J.; Trikalinos, T.A.; Lau, J.; Trow, P.; Schmid, C.H. Closing the Gap between Methodologists and End-Users: R as a Computational Back-End. J. Stat. Softw. 2012, 49, 1–15. [Google Scholar] [CrossRef]
- Falck-Ytter, Y.; Guyatt, G.H.; Vist, G.; Kunz, R. Rating quality of evidence and strength of recommendations GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008, 336, 924–926. [Google Scholar]
- Newman, M.G.; Weyant, R.; Hujoel, P. JEBDP improves grading system and adopts strength of recommendation taxonomy grading (SORT) for guidelines and systematic reviews. J. Evid. Based Dent. Prac. 2007, 7, 147–150. [Google Scholar] [CrossRef] [PubMed]
- Edman Tynelius, G.; Bondemark, L.; Lilja-Karlander, E. A randomized controlled trial of three orthodontic retention methods in Class I four premolar extraction cases—Stability after 2 years in retention. Orthod. Craniofac. Res. 2013, 16, 105–115. [Google Scholar] [CrossRef] [PubMed]
- Egli, F.; Bovali, E.; Kiliaridis, S.; Cornelis, M.A. Indirect vs direct bonding of mandibular fixed retainers in orthodontic patients: Comparison of retainer failures and posttreatment stability. A 2-year follow-up of a single-center randomized controlled trial. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 15–27. [Google Scholar] [CrossRef]
- Forde, K.; Storey, M.; Littlewood, S.J.; Paul Scott, P.; Luther, F.; Kang, J. Bonded versus vacuum-formed retainers: A randomized controlled trial. Part 1: Stability, retainer survival, and patient satisfaction outcomes after 12 months. Eur. J. Orthod. 2018, 40, 387–398. [Google Scholar] [CrossRef]
- Gill, D.S.; Naini, F.B.; Jones, A.; Tredwin, C.J. Part-time versus full-time retainer wear following fixed appliance therapy: A randomized prospective controlled trial. World J. Orthod. 2007, 8, 300–306. [Google Scholar]
- Kumar, A.G.; Bansal, A. Effectiveness and acceptability of Essix and Begg retainers: A prospective study. Aust. Orthod. J. 2011, 27, 52–56. [Google Scholar]
- O’Rourke, N.; Albeedh, H.; Sharma, P.; Johal, A. Effectiveness of bonded and vacuum-formed retainers: A prospective randomized controlled clinical trial. Am. J. Orthod. Dentofac. Orthop. 2016, 150, 406–415. [Google Scholar] [CrossRef]
- Rowland, H.; Hichens, L.; Williams, A.; Hills, D.; Killingback, N. The effectiveness of Hawley and vacuum-formed retainers: A single-center randomized controlled trial. Am. J. Orthod. Dentofac. Orthop. 2007, 132, 730–737. [Google Scholar] [CrossRef]
- Shawesh, M.; Bhatti, B.; Usmani, T.; Mandall, N. Hawley retainers full- or part-time? A randomized clinical trial. Eur. J. Orthod. 2010, 32, 165–170. [Google Scholar] [CrossRef]
- Bolla, E.; Cozzani, M.; Doldo, T.; Fontana, M. Failure evaluation after a 6-year retention period: A comparison between glass fiber-reinforced (GFR) and multistranded bonded retainers. Int. Orthod. 2012, 10, 16–28. [Google Scholar] [CrossRef] [PubMed]
- Salehi, P.; Zarif Najafi, H.; Roeinpeikar, S.M. Comparison of survival time between two types of orthodontic fixed retainer: A prospective randomized clinical trial. Prog. Orthod. 2013, 14, 25. [Google Scholar] [CrossRef] [PubMed]
- Störmann, I.; Ehmer, U. A prospective randomized study of different retainer types. J. Orofac. Orthop. 2002, 63, 42–50. [Google Scholar] [CrossRef] [PubMed]
- Isola, G.; Anastasi, G.P.; Matarese, G.; Williams, R.C.; Cutroneo, G.; Bracco, P.; Piancino, M.G. Functional and molecular outcomes of the human masticatory muscles. Oral Dis. 2018, 24, 1428–1441. [Google Scholar] [CrossRef]
- Isola, G.; Polizzi, A.; Santonocito, S.; Alibrandi, A.; Ferlito, S. Expression of Salivary and Serum Malondialdehyde and Lipid Profile of Patients with Periodontitis and Coronary Heart Disease. Int. J. Mol. Sci. 2019, 20, 6061. [Google Scholar] [CrossRef]
- Isola, G.; Perillo, L.; Migliorati, M.; Matarese, M.; Dalessandri, D.; Grassia, V.; Alibrandi, A.; Matarese, G. The impact of temporomandibular joint arthritis on functional disability and global health in patients with juvenile idiopathic arthritis. Eur. J. Orthod. 2019, 41, 117–124. [Google Scholar] [CrossRef]
- Mev, J. Are random controlled trials appropriate for orthodontics? Evid. Based Dent. 2002, 3, 35–36. [Google Scholar]
- Leonardi, R.; Lo Giudice, A.; Rugeri, M.; Muraglie, S.; Cordasco, G.; Barbato, E. Three-dimensional evaluation on digital casts of maxillary palatal size and morphology in patients with functional posterior crossbite. Eur. J. Orthod. 2018, 40, 556–562. [Google Scholar] [CrossRef]
- Leonardi, R. Cone-beam computed tomography and three-dimensional orthodontics. Where we are and future perspectives. J. Orthod. 2019, 46 (Suppl. 1), 45–48. [Google Scholar] [CrossRef] [PubMed]
- Caccianiga, G.; Crestale, C.; Cozzani, M.; Piras, A.; Mutinelli, S.; Lo Giudice, A.; Cordasco, G. Low-level laser therapy and invisible removal aligners. J. Biol. Regul. Homeost. Agents 2016, 30 (Suppl. 1), 107–113. [Google Scholar] [PubMed]
- Isola, G.; Alibrandi, A.; Rapisarda, E.; Matarese, G.; Williams, R.C.; Leonardi, R. Association of vitamin d in patients with periodontal and cardiovascular disease: A cross-sectional study. J. Periodontal. Res. 2020. [Google Scholar] [CrossRef]
- Isola, G.; Alibrandi, A.; Currò, M.; Matarese, M.; Ricca, S.; Matarese, G.; Ientile, R.; Kocher, T. Evaluation of salivary and serum ADMA levels in patients with periodontal and cardiovascular disease as subclinical marker of cardiovascular risk. J. Periodontol. 2020. [Google Scholar] [CrossRef]
- Isola, G.; Polizzi, A.; Alibrandi, A.; Indelicato, F.; Ferlito, S. Analysis of Endothelin-1 concentrations in individuals with periodontitis. Sci. Rep. 2020. [Google Scholar] [CrossRef] [PubMed]
- Isola, G.; Matarese, G.; Ramaglia, L.; Pedullà, E.; Rapisarda, E.; Iorio-Siciliano, V. Association between periodontitis and glycosylated haemoglobin before diabetes onset: A cross-sectional study. Clin. Oral Investig. 2019. [CrossRef]
- Cutroneo, G.; Piancino, M.G.; Ramieri, G.; Bracco, P.; Vita, G.; Isola, G.; Vermiglio, G.; Favaloro, A.; Anastasi, G.; Trimarchi, F. Expression of muscle-specific integrins in masseter muscle fibers during malocclusion disease. Int. J. Mol. Med. 2012, 30, 235–242. [Google Scholar] [CrossRef]
- Isola, G.; Matarese, M.; Ramaglia, L.; Cicciù, M.; Matarese, G. Evaluation of the efficacy of celecoxib and ibuprofen on postoperative pain, swelling, and mouth opening after surgical removal of impacted third molars: A randomized, controlled clinical trial. Int. J. Oral Maxillofac. Surg. 2019, 48, 1348–1354. [Google Scholar] [CrossRef]
- Isola, G.; Alibrandi, A.; Pedullà, E.; Grassia, V.; Ferlito, S.; Perillo, L.; Rapisarda, E. Analysis of the Effectiveness of Lornoxicam and Flurbiprofen on Management of Pain and Sequelae Following Third Molar Surgery: A Randomized, Controlled, Clinical Trial. J. Clin. Med. 2019, 8, 325. [Google Scholar] [CrossRef]
- Isola, G.; Matarese, G.; Alibrandi, A.; Dalessandri, D.; Migliorati, M.; Pedullà, E.; Rapisarda, E. Comparison of Effectiveness of Etoricoxib and Diclofenac on Pain and Perioperative Sequelae After Surgical Avulsion of Mandibular Third Molars: A Randomized, Controlled, Clinical Trial. Clin. J. Pain 2019, 35, 908–915. [Google Scholar] [CrossRef]
- Lo Giudice, A.; Brewer, I.; Leonardi, R.; Roberts, N.; Bagnato, G.5. Pain threshold and temporomandibular function in systemic sclerosis: Comparison with psoriatic arthritis. Clin. Rheumatol. 2018, 37, 1861–1867. [Google Scholar] [CrossRef] [PubMed]
- Lo Giudice, A.; Nucera, R.; Matarese, G.; Portelli, M.; Cervino, G.; Lo Giudice, G.; Militi, A.; Caccianiga, G.; Cicciù, M.; Cordasco, G. Analysis of resistance to sliding expressed during first order correction with conventional and self-ligating brackets: An in-vitro study. Int. J. Clin. Exp. Med. 2016, 9, 15575–15581. [Google Scholar]
- Piancino, M.G.; Isola, G.; Cannavale, R.; Cutroneo, G.; Vermiglio, G.; Bracco, P.; Anastasi, G.P. From periodontal mechanoreceptors to chewing motor control: A systematic review. Arch. Oral Biol. 2017, 78, 109–121. [Google Scholar] [CrossRef] [PubMed]
- Perillo, L.; Padricelli, G.; Isola, G.; Femiano, F.; Chiodini, P.; Matarese, G. Class II malocclusion division 1:.A new classification method by cephalometric analysis. Eur. J. Paediatr. Dent. 2012, 13, 192–196. [Google Scholar]
- Isola, G.; Giudice, A.L.; Polizzi, A.; Alibrandi, A.; Patini, R.; Ferlito, S. Periodontitis and Tooth Loss Have Negative Systemic Impact on Circulating Progenitor Cell Levels: A Clinical Study. Genes 2019, 10, 1022. [Google Scholar] [CrossRef]
- Isola, G.; Polizzi, A.; Muraglie, S.; Leonardi, R.M.; Lo Giudice, A. Assessment Of vitamin C And Antioxidants Profiles In Saliva And Serum In Patients With Periodontitis And Ischemic Heart Disease. Nutrients 2019, 11, 2956. [Google Scholar] [CrossRef]
- Cannavale, R.; Matarese, G.; Isola, G.; Grassia, V.; Perillo, L. Early treatment of an ectopic premolar to prevent molar-premolar transposition. Am. J. Orthod. Dentofac. Orthop. 2013, 143, 559–569. [Google Scholar] [CrossRef]
- Lo Giudice, A.; Barbato, E.; Cosentino, L.; Ferraro, C.M.; Leonardi, R. Alveolar bone changes after rapid maxillary expansion with tooth-born appliances: A systematic review. Eur J Orthod. 2018, 40, 296–303. [Google Scholar] [CrossRef]
- Isola, G.; Matarese, M.; Briguglio, F.; Grassia, V.; Picciolo, G.; Fiorillo, L.; Matarese, G. Effectiveness of Low-Level Laser Therapy during Tooth Movement: A Randomized Clinical Trial. Materials 2019, 12, 2187. [Google Scholar] [CrossRef]
- Lo Giudice, A.; Rustico, L.; Caprioglio, A.; Migliorati, M.; Nucera, R. Evaluation of condylar cortical bone thickness in patient groups with different vertical facial dimensions using cone-beam computed tomography. Odontology 2020, in press. [Google Scholar] [CrossRef]
- Lo Giudice, A.; Fastuca, R.; Portelli, M.; Militi, A.; Bellocchio, M.; Spinuzza, P.; Briguglio, F.; Caprioglio, A.; Nucera, R. Effects of rapid vs slow maxillary expansion on nasal cavity dimensions in growing subjects: A methodological and reproducibility study. Eur. J. Paediatr. Dent. 2017, 18, 299–304. [Google Scholar] [PubMed]
- Caccianiga, G.; Paiusco, A.; Perillo, L.; Nucera, R.; Pinsino, A.; Maddalone, M.; Cordasco, G.; Lo Giudice, A. Does Low-Level Laser Therapy Enhance the Efficiency of Orthodontic Dental Alignment? Results from a Randomized Pilot Study. Photomed Laser Surg. 2017, 35, 421–426. [Google Scholar] [CrossRef] [PubMed]
- Matarese, G.; Portelli, M.; Mazza, M.; Militi, A.; Nucera, R.; Gatto, E.; Cordasco, G. Evaluation of skin dose in a low dose spiral CT protocol. Eur. J. Paediatr. Dent. 2006, 7, 77–80. [Google Scholar]
- Caprioglio, A.; Bergamini, C.; Franchi, L.; Vercellini, N.; Zecca, P.A.; Nucera, R. Fastuca R Prediction of Class II improvement after rapid maxillary expansion in early mixed dentition. Prog. Orthod. 2017, 18, 9. [Google Scholar] [CrossRef] [PubMed]
- Nucera, R.; Lo Giudice, A.; Matarese, G.; Artemisia, A.; Cordasco, G.; Bramanti, E. Analysis of the characteristics of slot design affecting resistance to sliding during active archwire configurations. Prog Orthod. 2013, 14, 35. [Google Scholar] [CrossRef] [PubMed]
- Isola, G.; Matarese, G.; Cordasco, G.; Rotondo, F.; Crupi, A.; Ramaglia, L. Anticoagulant therapy in patients undergoing dental interventions: A critical review of the literature and current perspectives. Minerva Stomatol. 2015, 64, 21–46. [Google Scholar]
- Matarese, G.; Isola, G.; Anastasi, G.P.; Cutroneo, G.; Favaloro, A.; Vita, G.; Cordasco, G.; Milardi, D.; Zizzari, V.L.; Tetè, S.; et al. Transforming Growth Factor Beta 1 and Vascular Endothelial Growth Factor levels in the pathogenesis of periodontal disease. Eur. J. Inflamm. 2013, 11, 479–488. [Google Scholar] [CrossRef]
- Isola, G.; Williams, R.C.; Lo Gullo, A.; Ramaglia, L.; Matarese, M.; Iorio-Siciliano, V.; Cosio, C.; Matarese, G. Risk association between scleroderma disease characteristics, periodontitis, and tooth loss. Clin. Rheumatol. 2017, 36, 2733–2741. [Google Scholar] [CrossRef]
- Matarese, G.; Isola, G.; Alibrandi, A.; Lo Gullo, A.; Bagnato, G.; Cordasco, G.; Perillo, L. Occlusal and MRI characterizations in systemic sclerosis patients: A prospective study from Southern Italian cohort. Joint. Bone. Spine. 2016, 83, 57–62. [Google Scholar] [CrossRef]
- Ametrano, G.; D'Antò, V.; Di Caprio, M.P.; Simeone, M.; Rengo, S.; Spagnuolo, G. Effects of sodium hypochlorite and ethylenediaminetetraacetic acid on rotary nickel-titanium instruments evaluated using atomic force microscopy. Int. Endod. J. 2011, 44, 203–209. [Google Scholar] [CrossRef]
- Spagnuolo, G.; Ametrano, G.; D’Antò, V.; Formisano, A.; Simeone, M.; Riccitiello, F.; Amato, M.; Rengo, S. Microcomputed tomography analysis of mesiobuccal orifices and major apical foramen in first maxillary molars. Open. Dent. J. 2012, 6, 118–125. [Google Scholar] [CrossRef] [PubMed]
- Krifka, S.; Petzel, C.; Bolay, C.; Hiller, K.A.; Spagnuolo, G.; Schmalz, G.; Schweikl, H. Activation of stress-regulated transcription factors by triethylene glycol dimethacrylate monomer. Biomaterials 2011, 32, 1787–1795. [Google Scholar] [CrossRef] [PubMed]
- Pelo, S.; Saponaro, G.; Patini, R.; Staderini, E.; Giordano, A.; Gasparini, G.; Garagiola, U.; Azzuni, C.; Cordaro, M.; Foresta, E.; et al. Risks in surgery-first orthognathic approach: Complications of segmental osteotomies of the jaws. A systematic review. Eur. Rev. Med. Pharmacol. Sci. 2017, 21, 4–12. [Google Scholar] [PubMed]
- Facciolo, M.T.; Riva, F.; Gallenzi, P.; Patini, R.; Gaglioti, D. A rare case of oral multisystem Langerhans cell histiocytosis. J. Clin. Expd. Dent. 2017, 9, e820–e824. [Google Scholar] [CrossRef][Green Version]
- Cordasco, G.; Lo Giudice, A.; Militi, A.; Nucera, R.; Triolo, G.; Matarese, G. In vitro evaluation of resistance to sliding in self-ligating and conventional bracket systems during dental alignment. Korean J. Orthod. 2012, 42, 218–224. [Google Scholar] [CrossRef]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).