1. Introduction
Tuberculosis (TB) as both an acute and chronic infectious disease is still unbeaten and represents an important social, medical, and biological challenge for the healthcare worldwide [
1]. The infection caused by
Mycobacterium tuberculosis strains is most often located in the respiratory tract from which it is transmitted in the population by aerosols. At the same time, mycobacteria can be disseminated also to other organs. However, it is now well acknowledged that even in its primary location, the TB pathogen is present in different microenvironments and thus in various metabolic states, which substantially complicates the treatment [
2]. According to the last Global Tuberculosis Report issued by the World Health Organization (WHO) [
3], in 2018 the death rate was estimated to be about 1.45 million people. Among the estimated 10 million new cases of TB, 3.4% had multidrug-resistant TB or rifampicin-resistant TB (MDR/RR-TB). This number increased to 18% in previously treated cases, with the highest proportions (>50% in previously treated cases) in countries of the former Soviet Union. Although efficient TB treatment is available, only 7 million new cases were treated for the disease in 2018, while an estimated 3 million patients did not have access to quality care or were not reported, and only one in three people with drug-resistant TB accessed care [
3].
In addition to interventions in the social area and point-of-care management of TB, one of the key challenges in making the fight against TB more effective is to improve treatment options. The current chemotherapy for the drug-sensitive TB takes about six months and requires administration of four different medicines (isoniazid, rifampicin, ethambutol, pyrazinamide) to avoid development of drug resistance. The length of the treatment and its adverse effects result in bad compliance and thus it is imperative to find novel drugs and regimens that would be less demanding on patients [
4].
During recent years, three novel drugs against TB were approved. These are bedaquiline [
5], delamanid [
6] and pretomanid [
7], which are currently undergoing several clinical trials aimed at treatment of the drug-resistant TB, as well as at shortening standard TB treatment [
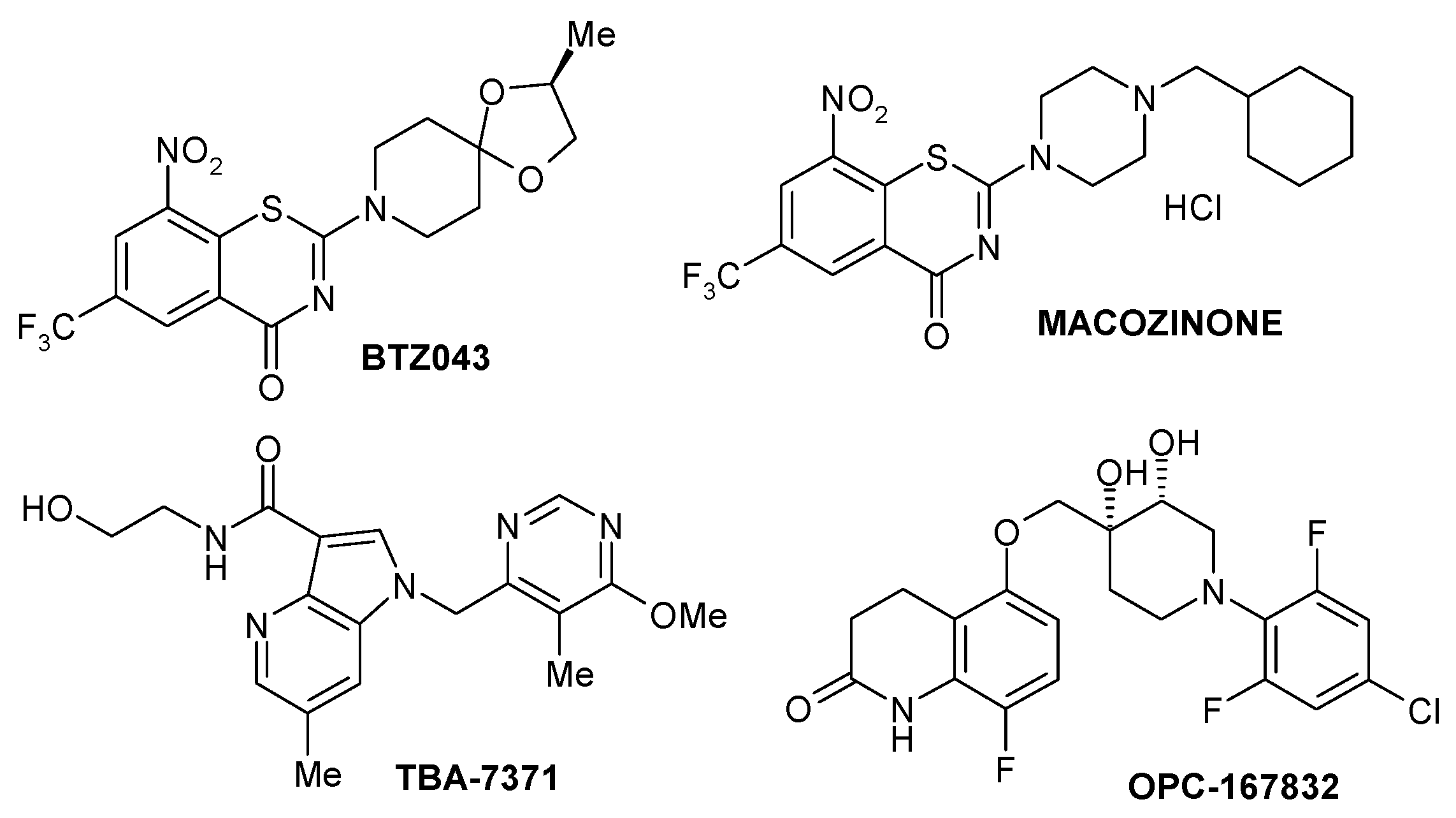
8]. The efforts and hope for better TB drugs are exemplified also by the pipeline of several new molecules, that are currently at different stages of clinical development. Among them there are inhibitors of protein synthesis from the oxazolidinone family (delpazolid, sutezolid, contezolid, TBI-223), inhibitor of leucyl-tRNA synthetase (GSK3036656), inhibitor of DNA gyrase B (SPR720), compounds interfering with the respiratory chain of a TB pathogen (telacebec, TBI-166), a cell wall inhibitor targeting MmpL3 transporter (SQ109) and four compounds targeting another cell wall target, DprE1. These are BTZ043, TBA-7371, OPC-167832, and macozinone (
Figure 1) [
4,
8]. In this review we will present the key findings towards the discovery and development of macozinone, an optimized benzothiazinone, which currently appears to be the most advanced DprE1 inhibitor.
2. Discovery of Benzothiazinones as Highly Potent Killers of Mycobacterium Tuberculosis
The very first scientific report on benzothiazinones (BTZs) with extremely high antimycobacterial activity was published in 2009 [
9]. These compounds emerged as a result of several years of efforts focused on investigation of a family of ditiocarbamate (DTC) derivatives with antimicrobial properties, which was carried out at the Research Center for Antibiotics in Moscow and the Hans Knöll Institute in Jena [
10]. DTCs gained their fame primarily as additives in industry and pesticides, which have been in use since 1930. However, some of them were tested as pharmacological agents for treatment of alcoholism, human immunodeficiency virus (HIV) or cancer [
11]. It occurred that selected DTC derivatives had minimal inhibitory concentrations (MICs) between 3–30 μg/ml for
M. tuberculosis, but were active also on several species of fast-growing mycobacteria and multiresistant staphylococci [
10]. Thorough structure-activity studies focused on improvement of the activity and selectivity of these compounds for mycobacteria was performed. Selected compounds derived from the basic active ortho nitro-dialkyldithiocarbamate structure showed enhanced activity towards fast growing mycobacteria, with
M. vaccae being the most sensitive reaching MICs 0.4–1.56 μg/ml [
12]. In addition, 3 out of 7 tested molecules were efficient and well tolerated also in the mouse foot pad model of leprosy [
12]. Nevertheless, it was clear that reactivity of DTCs poses a significant problem in further development of these compounds despite their activity and rather unexpected low level of toxicity as exemplified by studies in mice [
12]. Consequently, a thorough investigation of the metabolic conversion of the most active DTCs containing spiroamine moiety, was undertaken. The drug was incubated with the non-pathogenic strain
M. smegmatis and all isolated metabolites were tested for antimycobacterial activity. One of these metabolites was particularly active and its structure established by nuclear magnetic resonance (NMR) revealed the principal BTZ scaffold. A set of novel BTZ derivatives was synthesized and tested against both fast-growing and pathogenic mycobacteria in collaboration with Prof. Stewart Cole at Pasteur Institute in Paris [
13]. Surprisingly, these compounds were highly active and selective against mycobacteria in vitro, with MIC values 0.195–1.56 μg/ml for
M. tuberculosis, including the resistant strains. The lowest MIC value, 0.023 pg/ml, was obtained for
M. fortuitum and 2,2-[2-methyl-1,4-dioxa-8-azaspiro[4.5]dec-8-yl]-8-nitro- 6-(trifluoromethyl)-4H-1,3-benzothiazin-4-one, later named BTZ038 [
9]. The pilot in vivo studies with this compound revealed its potency in the murine model of TB, which was comparable to isoniazid used in the same dose of 25 mg/kg [
13]. These encouraging results warranted further exploration of BTZs as perspective compounds for development of a new TB drug.
3. Mechanism of Action of Benzothiazinones
An investigation of mechanism of action of BTZ was carried out within the European Union (EU)-funded consortium New Medicines for Tuberculosis (NM4TB), which was formed in 2006 under the leadership of Prof. Stewart Cole. The compound BTZ038 was initially chosen as a lead molecule. Since it contains a chiral center, pure enantiomers BTZ043 (S) and BTZ044 (R) were prepared and subjected to MIC determination. Both forms showed comparable activities in vitro in
M. tuberculosis. Accordingly, only one of them, BTZ043, was subjected to mechanistic studies [
9].
Genetic experiments aimed at identification of the BTZ target were carried out by Prof. Giovanna Riccardi and her team at University of Pavia. The two approaches which were chosen for this purpose pointed out to the role of the gene
rv3790 in conferring resistance against the drug. In the first approach,
M. smegmatis was transformed with a cosmid library containing DNA fragments from the same organism. An ortholog of the
rv3790 gene from
M. smegmatis mc
2155,
MSMEG_6382, was identified on a cosmid, which resulted in an increase in MICs towards BTZ043. In the second approach, BTZ-resistant strains of
M. smegmatis,
M. bovis BCG and
M. tuberculosis were isolated and their resistance was traced to mutations in the same codon in
rv3790 and its orthologs. In all mutant strains codons corresponding to Cys387 in
rv3790 gene product were replaced by Ser or Gly, which increased the MICs of the resistant strains up to 10,000 times. Accordingly, the mycobacterial species
M. avium and
M. aurum, in which this position was occupied by Ala or Ser, respectively, were naturally resistant against BTZ, which supported identification of
rv3790 as a target [
9]. Coincidentally, the function of the protein encoded by this gene was described only a short while before the data on the BTZ target became available. In the course of studies focused on the metabolism of arabinose in mycobacteria carried out by Prof. Michael McNeil with collaborators at Colorado State University in Fort Collins, the
rv3790 and
rv3791 gene products were proposed to be involved in a unique epimerisation of decaprenylphosphoryl ribose (DPR) to decaprenylphosphoryl arabinose (DPA) [
14]. The latter molecule serves as a sole donor of arabinose residues for synthesis of the essential arabinan polymers of the mycobacterial cell wall [
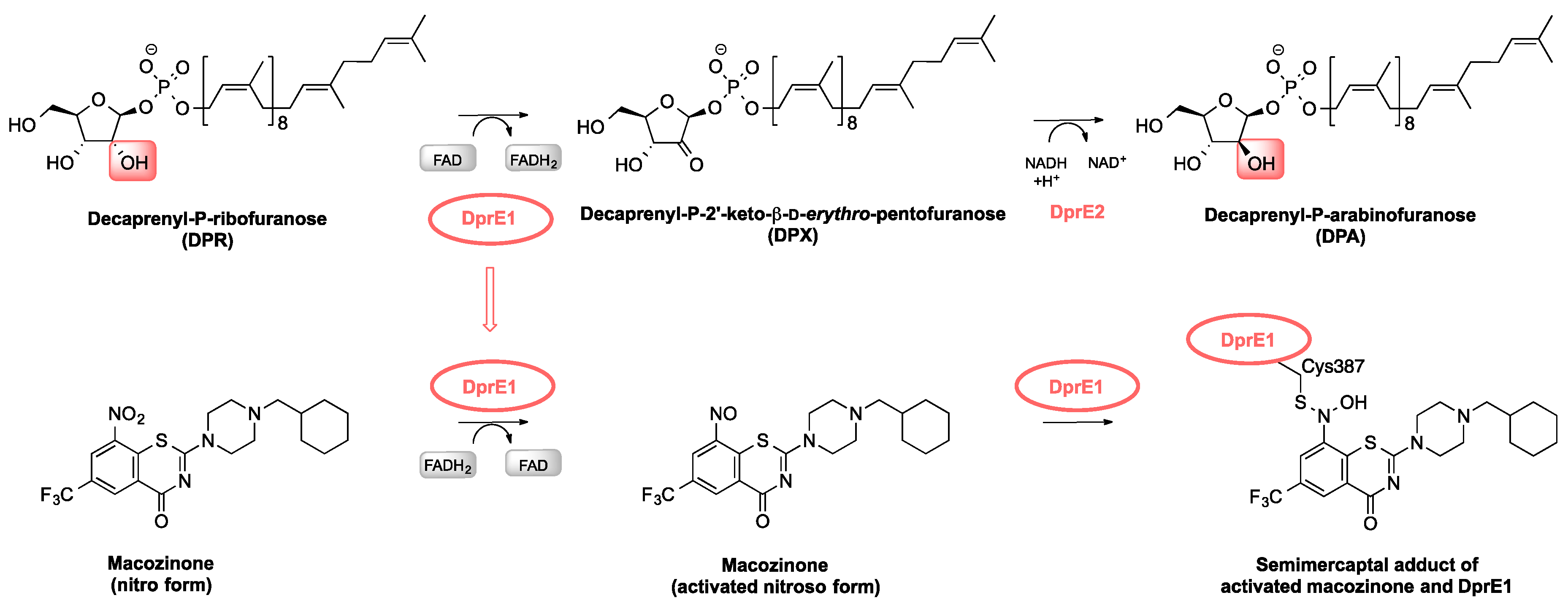
15]. It was shown that the conversion takes place via oxidation of the DPR substrate, followed by reduction of the resulting keto-intermediate and thus the two oxidoreductases,
rv3790 and
rv3791, from the so-called arabinogalactan biosynthesis cluster [
16] were ideal candidates to catalyse these reactions. However, at the time it was not possible to conclude which of the two is responsible for oxidation and which for the reduction step. Examination of the effects of BTZ043 on enzymatic conversion of DPR to DPA proved that the compound inhibited the oxidation step. Given the confirmed roles of Rv3790 and Rv3791 in epimerization of DPR, we named them DprE1 and DprE2, respectively (
Figure 2) [
9].
An important step towards understanding the mechanism of action of BTZs was isolation of a covalent adduct of BTZ043 and DprE1 by Trefzer et al. in 2010 [
17]. The authors concluded that reduction of the nitro-group to nitroso derivative is critical for formation of the semimercaptal adduct of BTZ043 and DprE1 through the Cys387, which was verified by mass spectrometry. The following study proved that DprE1 itself is responsible for the reductive activation of DprE1. The electrons needed for the reaction are provided by the enzyme’s prosthetic group, FAD, which gets reduced during the catalysis of DPR oxidation (
Figure 2) [
18]. Accordingly, BTZ represents a typical example of a suicide inhibitor. The proposed mechanism of action was confirmed by crystallographic studies in which structures of DprE1 from
M. smegmatis were obtained in native and BTZ043-bound forms. As expected, the semimercaptal adduct was formed only in the presence of the substrate analog, farnesylphosphoryl ribose, which provided electrons for reduction of the FAD cofactor necessary for BTZ activation [
19].
4. From BTZ043 to PBTZ169
At the time of its discovery, BTZ043 was the most efficient inhibitor of in vitro mycobacterial growth ever described. While MICs for first line drugs isoniazid or ethambutol for
M. tuberculosis were 0.02–0.2 μg/ml or 1–5 μg/ml, respectively, the value for BTZ043 was just 1 ng/ml. The compound proved to be active also in intracellular
M. tuberculosis infection in Raw 264.7 macrophages and in a mouse model of chronic tuberculosis and it did not show any signs of toxicity or mutagenicity in concentrations well above the amounts used for the experiments. Nevertheless, the extremely low MIC did not translate to comparably high efficiencies in animal studies [
9].
In the effort to improve pharmacological properties of benzothiazinone series, structure-activity relationship (SAR) analysis was performed, with main focus on position 2 of BTZ scaffold [
20]. It was previously shown that the rest of the positions harbor substituents critical for the antimycobacterial activity, e.g., replacement of 8-nitro-group with any other group, including hydroxylamino-, amino- and nitryl-, led to at least a 500-fold increase in the MIC against
M. tuberculosis [
9]. The new series contained a piperazine at the position 2 of the BTZ structure, which allowed extensive modifications of the N-4 position of this substituent. Evaluation of the 60 prepared piperazine-benzothiazinones (PBTZ) for in vitro activity on
M. tuberculosis pointed to a strong correlation between the MICs and lipophilicity. The alkyl-PBTZ derivatives were most active and some of them reached the MICs between 0.19–0.75 ng/ml for
M. tuberculosis. Five of these derivatives were tested in the chronic TB mouse model, which allowed for selection of PBTZ169 as the most promising candidate [
20].
Comparison of BTZ043 with PBTZ169 confirmed superior properties of the latter in all tested parameters. It was three to seven times more active in vitro against
M. tuberculosis,
M. bovis BCG,
M. marinum,
M. smegmatis,
Corynebacterium diphtheriae and
C. glutamicum as established by resazurin microtiter assay (REMA). The molecule was also highly active against a panel of 9 MDR- and XDR-clinical isolates of
M. tuberculosis [
20]. Cross-resistance between BTZ043 and PBTZ169 was confirmed for BTZ-resistant strains of
M. tuberculosis,
M. bovis BCG and
M. smegmatis, indicating the common mechanism of action. Interestingly, PBTZ169 was less susceptible to inactivation by nitro-reduction by the nitroreductase NfnB from
M. smegmatis compared to BTZ043, as confirmed by the liquid chromatography-mass spectrometry analyses. This property could be critical for in vivo activity, due to inevitable actions of host nitroreductases or microbial nitroreductases in the digestive tract of the patients, which would potentially reduce the amount of the available active drug. Enzymologic studies confirmed that PBTZ169 is more efficient inhibitor of its DprE1 target than BTZ043; the enzyme was completely inactivated after 5 min of incubation with 5 μM PBTZ169, while four times higher concentration was needed to achieve the same result with BTZ043. The crystal structure of
M. tuberculosis DprE1 with covalently bound PBTZ169 showed similarities with the BTZ043-bound structure of the
M. smegmatis enzyme. However, higher flexibility of the methyl-cyclohexyl group on piperazine, could account for better affinity of this drug for its target and explain its higher capacity to inactivate the enzyme [
20].
Efficacies of PBTZ169 and BTZ043 were also evaluated against
M. marinum in a zebrafish embryo model. Although after 5 days of treatment both drugs efficiently decreased the bacterial burden at concentrations of 25 nM and 50 nM, examination of BTZ043-treated embryos pointed to developmental defects. By contrast, application of PBTZ169 up to 10 μM did not cause any pathological changes. In vivo studies in the mouse chronic model of TB proved the superiority of PBTZ169 over BTZ043 in lowering colony forming unit counts in the spleen and lungs, which, however, could not be attributed to better pharmacokinetics, since the two compounds had similar properties except for faster uptake of PBTZ169 [
20]. Aiming at the use of the novel PBTZ derivative in designing a new regimen for TB, combination studies with selection of approved and experimental drugs were performed. The combination of PBTZ169 and bedaquiline, which proved to be synergistic in the in vitro REMA assay, was tested in the mouse chronic model of TB. Simultaneous administration of PBTZ, bedaquiline and pyrazinamide was more efficient in reducing the mycobacterial counts both in the lungs and spleen compared to the standard mixture of isoniazid, rifampicin and pyrazinamide [
20].
Among favorable properties of PBTZ169 over BTZ043 is the lack of the chiral center, which simplified the production of the drug and significantly decreased its price. This is critical for developing treatment for a disease greatly affecting low-income and middle-income countries in particular. Taken together, PBTZ169 was identified as a promising candidate for development as a novel TB medicine [
20].
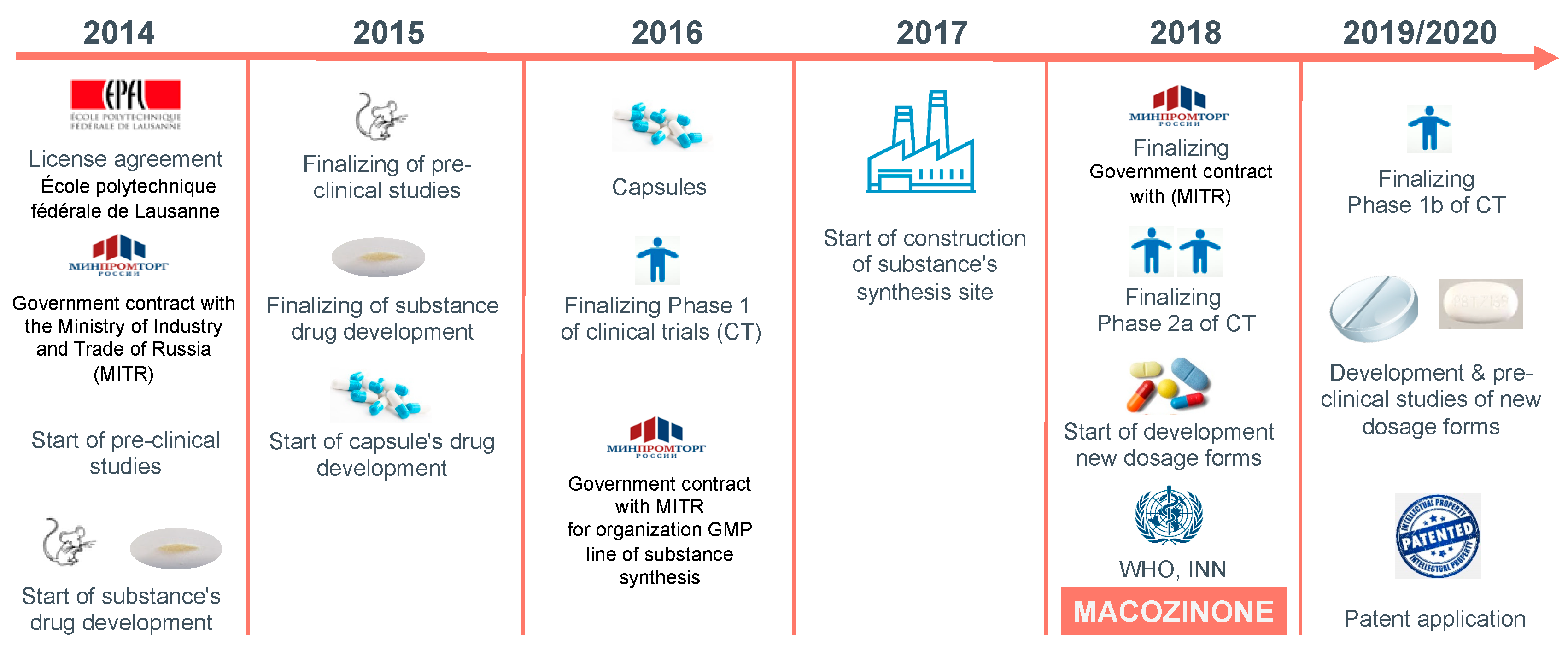
5. From PBTZ169 to Macozinone: First Results of the Clinical Studies
Establishment of a non-profit Innovative Medicines for Tuberculosis Foundation (iM4TB Foundation) at Ecole Polytechnique Fédérale de Lausanne (EPFL) in March 2014 was a principal milestone for the further development of PBTZ169 and its transformation from a valuable TB drug candidate to the compound reaching promising results in the pilot clinical studies (
Figure 3) [
21]. This approach was necessary to overcome the lack of interest from pharmaceutical companies to address the disease primarily affecting low-income countries. The mission of the foundation is “to develop better and faster-acting medicines to fight tuberculosis and bridge the gap between scientific discovery and the market in order to provide affordable TB treatment to anyone in the world”. In July 2014 the foundation joined in this effort with the Russian pharmaceutical company Nearmedic Plus LLC, which bought a license covering the use of PBTZ169 in most countries of the former Soviet Union, while iM4TB retained the rights for the rest of the world. Investments of Nearmedic, along with funds raised by iM4TB, including the generous support of the Bill and Melinda Gates foundation, enabled performing all necessary pre-clinical trials with PBTZ169, such as ADME (absorption, distribution, metabolism, excretion) profiling, toxicology studies, as well as production of clinical supplies of the drug, and preparation of regulatory documents necessary for entering the first clinical trials [
21,
22].
Clinical studies were initiated by both iM4TB and Nearmedic. In the randomized, double-blind, placebo-controlled Phase 1a study performed in Switzerland (NCT03423030) [
23] the aim was to assess safety, tolerability and pharmacokinetic profile of PBTZ169 formulated as a spray-dried dispersion versus a native crystal powder. In addition, antitubercular activity of single escalating doses of PBTZ169 ex vivo was evaluated. The study included 32 healthy male volunteers, grouped to 4 panels of 8 subjects, each undergoing 2 investigation periods, during which they received either single doses of PBTZ169 at increasing dose levels up to 320 mg or a matching placebo. Promising results of this study encouraged the iM4TB team to design of the Phase 1b trial (NCT03776500) [
24] aimed at evaluation of the safety, tolerability and pharmacokinetics of PBTZ169 in multiple dosing up to 1200 mg/day in healthy volunteers (32 subjects grouped in 4 consecutive panels) receiving PBTZ169 for 14 consecutive days. An additional goal is to evaluate interactions of PBTZ16 with the human cytochrome P-450 enzyme family [
24].
The first Phase 1 clinical trial in Russia (Nearmedic Plus LLC) (NCT03036163, PBTZ169-Z00-C01-1) [
25] with an official title “Open-label Prospective Non-comparative Study of Safety, Tolerability and Pharmacokinetics of PBTZ169 after Single and Multiple Fasting Oral Administration in Increasing Doses in Healthy Volunteers” was carried out between January and November 2016. The drug was administered in the form of capsules containing 40 mg of the drug. The study included single escalating doses (40, 80, 160, 320, and 640 mg) in fasting conditions, as well as multiple fasting doses (320 and 640 mg) for 14 days. Overall the study included 40 participants [
22].
A completed open-label prospective Phase 1b study initiated by Nearmedic Plus LLC (NCT04150224, PBTZ169-Z00-C01-3) [
26] was designed to assess the safety, tolerability, pharmacokinetics, and food effects on single, double, and multiple escalating doses in healthy volunteers. During the first part of the study, safety, tolerability, and pharmacokinetics of PBTZ169 in 80 mg capsules were studied in healthy volunteers who received single or double (twice daily) fasting doses, which increased sequentially (640, 960, and 1280 mg once a day and 640 mg twice a day). The food effects were studied for a single 640 mg dose. The second part of the study involved the safety, tolerability, and pharmacokinetics of PBTZ169 in 80 mg capsules in healthy volunteers who received 1280 mg daily in fed conditions, for 14 days. In total, 60 healthy volunteers (10 in each cohort) received the investigational drug and completed the study according to the protocol [
22].
During these clinical trials, safety and tolerability of PBTZ169 in capsules were studied, including assessment of adverse effects, vital signs (blood pressure, heart rate, body temperature, respiratory rate), laboratory and instrumental parameters (hematology, blood chemistry, coagulation parameters, urinalysis, electrocardiography) and physical examination. In these studies (NCT03036163 and NCT04150224), good tolerability and favorable safety profile were demonstrated for PBTZ169 in the studied dose range. One event of dose-limiting toxicity (increase in the glucose level 2 hours after the drug administration) was documented after a single 80 mg dose of PBTZ169 in 40 mg capsules (NCT03036163). There were no other cases of dose-limiting toxicity in healthy volunteers in these studies. There were no serious adverse effects. There was no increase in the frequency of adverse effects associated with increased dose or with the administration regimen (fasting or in fed conditions), for single or multiple doses. Changes in some mean vital signs, laboratory, instrumental parameters, or physical examination data were not associated with a trend to increase with a growing dose [
22].
Efficacy of PBTZ169 based on the early bactericidal activity (EBA), was studied in a Phase 2a clinical trial (PBTZ169-A15-C2A-1, NCT03334734) [
27] by Nearmedic Plus LLC in patients with newly diagnosed smear-positive tuberculosis of the respiratory tract, with preserved sensitivity to isoniazid and rifampicin. Although the trial was terminated early because of slow enrollment, relevant information was obtained from 16 patients who participated in the study. The drug was administered in 80 mg capsules, orally as a monotherapy for 14 days, as follows: 160 mg/day dose—4 patients; 320 mg/day dose—4 patients; 640 mg/day dose—7 patients. Isoniazid tablets were used as a control treatment at 600 mg/day dose in one patient.
The primary efficacy of the treatment was evaluated by two methods:
(i) According to quantification of colony forming units in sputum by its inoculation on agar plates, in the group of patients receiving PBTZ169 in the 640 mg dose, EBA 0–14 (mean of the two measurements) and EBA 0–14 (the higher of the two measurements) were 0.071 log10 cells/ml/day [95% confidence interval (CI) 0; 0.143] and 0.080 log10 cells/ml/day [95% CI 0.002; 0.158], respectively.
(ii) According to quantitative polymerase chain reaction, in the same group of patients, EBA 0–14 (mean of the two measurements) and EBA 0–14 (the higher of the two measurements) were 0.098 log10 cells/ml/day [95% CI 0.021; 0.175] and 0.100 log10 cells/ml/day[95% CI 0.021; 0.180], respectively.
Thus, the analysis of efficacy based on the data obtained in a pilot Phase 2a clinical study revealed statistically significant early bactericidal activity of PBTZ169 14 days after the start of monotherapy (EBA0-14) in the group of PBTZ169 with the 640 mg dose. During this clinical study, there were no cases of death or severe adverse effects related to the PBTZ169. No adverse effects were considered as definitely related to the drug and, at the study completion, all adverse effects were resolved. There was no increase in adverse effects frequency with growing dose [
22].
During the clinical studies it was confirmed that PBTZ169 after single, double, or multiple doses was detectable in the blood plasma of all volunteers and patients who had received the drug. However, it should be noted that pharmacokinetic studies in animals and in healthy volunteers (in Phase 1 clinical studies) demonstrated that PBTZ169, being more soluble in an acidic environment, is absorbed primarily in the stomach. These data agree with the results of in vitro studies, which were conducted by Nearmedic Plus LLC, assessing cellular permeability and solubility in biorelevant media, which mimicked native gastric and intestinal juices. They confirmed that the highest solubility of PBTZ169 is observed at the pH range of 1 to 2, which coincides with the pH in the lower part of the stomach, and its solubility gradually decreases with the growing pH. In the media with pH higher than 5, PBTZ169 was virtually insoluble. According to the test of solubility in biorelevant media, the drug level in the gastric juice was much higher than in the intestinal juice. So, one of the possible methods to increase bioavailability and exposure of PBTZ169 is to prolong its presence in the stomach.
After a single fasting dose, PBTZ169 absorbed rapidly, and the speed of absorption was independent of the administered dose (median T
max was 1.5–2.5 hours for the dose range 40–640 mg (NCT03036163), and 1.5–1.75 hours for the dose range 640–1280 mg (NCT04150224). Meantime of retention of the drug in the body was 13.02–19.30 hours and was independent of the administered dose (NCT03036163) [
22].
According to the obtained pharmacokinetic data, dose proportionality of Cmax and AUC0-t was demonstrated for single, as well as for multiple administrations of the investigational drug in the dose range 40–640 mg (NCT03036163, NCT03334734). After single fasting escalating doses (640, 960, and 1280 mg), Cmax, AUC0-24, AUC0-∞ were less than dose proportional. Thus, it can be concluded that there is a trend for linear pharmacokinetics for single and multiple doses up to 640 mg.
When pharmacokinetics of different administration regimens for 1280 mg daily dose was studied (640 mg twice daily or 1280 mg once in fasting conditions), the pharmacokinetic parameters AUC0-∞ and AUC0-t increased 1.5–1.6-fold (NCT04150224). The relation of mean AUC0-∞ and AUC0-t in cohorts receiving the investigational drug as 640 mg twice a day and 1280 mg once a day, was 153.68% and 160.32%. For Cmax, a slight decrease (1.1-fold) was observed for the 640 mg twice a day (the relation of means was 90.84%). All observed differences were statistically significant.
According to the results of analysis of relative bioavailability and relative degree of absorption, the main pharmacokinetic parameters of PBTZ169 substantially and statistically significantly increased when 640 mg dose was administered in fed conditions: AUC
0-∞increased 3.45-fold, AUC
0-t (f’) increased 3.50-fold, C
max increased 2.29-fold. The drug absorbed and cleared from the body significantly more slowly, when it was administered in fed conditions compared to the fasting conditions (median T
max increased 2-fold, mean T
1/2 increased 1.44-fold). These data allow to conclude that it is preferable to administer PBTZ169 in fed conditions [
22].
In October 2018, the international non-proprietary name “macozinone” was given to PBTZ169 by WHO [
28]. In addition to the clinical studies, macozinone is undergoing further in vitro and in vivo testing focused on improvement of its pharmacological properties by structure-based design [
29], or on the interactions with anti-TB drugs [
30]. Importantly, an efficient method for monitoring metabolism of macozinone in human plasma was recently developed. It enables simultaneous measurement of concentrations of macozinone and its five active metabolites in the clinical samples, which is important for comprehensive pharmacokinetic/pharmacodynamic analyses [
31].
6. Other DprE1 Inhibitors under Active Clinical Development
Following the discovery of DprE1 as a target of BTZ043, numerous molecules acting on this enzyme emerged, particularly from the whole-cell based phenotypic screening campaigns (for a recent review see [
32]). As a result, DprE1 was given an unflattering attribute—a promiscuous target [
33]. Nevertheless, DprE1 remains to be one of the best understood and the most vulnerable novel targets. One of the reasons for its high sensitivity against a number of different pharmacophores could be its periplasmic localization, which makes it easily accessible for the drugs [
34]. Consequently, in addition to macozinone, there are currently three other DprE1 inhibitors progressing down the clinical studies pipeline. BTZ043, sponsored by the University of Munich; the Hans Knöll Institute, Jena; and the German Center for Infection Research, successfully completed a single dose escalation Phase 1 study (NCT03590600) [
35] and is currently recruiting for a combined Phase 1 and 2 study, which will evaluate safety, tolerability, pharmacokinetics and early bactericidal activity of the multiple ascending doses (NCT04044001) [
36]. A non-covalent DprE1 inhibitor, TBA-7371 [
37] developed by TB Alliance, Bill and Melinda Gates Medical Research Institute and Foundation for Neglected Disease Research, completed a Phase 1 study (NCT03199339) [
38]—a partially blind, placebo-controlled study of (i) a combined single ascending dose with a food effect cohort, (ii) multiple ascending dose group, and (iii) a cohort to investigate interactions between TBA-7371 with midazolam and bupropion. Currently, recruitment of adult patients with rifampicin-sensitive pulmonary tuberculosis is taking place for the participation in a Phase 2 study (NCT04176250) [
39] to assess safety, early bactericidal activity, and pharmacokinetics of escalating doses of TBA-7371. A combined Phase 1 and 2 study of OPC-167832 by Otsuka is in progress (NCT03678688) [
40], aimed at evaluation of the safety, tolerability, pharmacokinetics, and efficacy of multiple oral doses of the drug in patients with uncomplicated drug-sensitive pulmonary tuberculosis with a positive smear. In a parallel group, low dose or high dose OPC-167832 will be combined with delamanid and compared to delamanid only, or standard treatment with isoniazid, rifampin, pyrazinamide, and ethambutol.
7. Conclusions
The ultimate goal of the TB drug-development efforts is a design of new, more effective regimen, which could replace the current combination therapy. One of the most promising DprE1 inhibitors is macozinone. Its safety and tolerability profiles, pharmacokinetics, and efficacy in terms of early bactericidal activity were evaluated in the course of three clinical trials conducted by Nearmedic Plus LLC in the Russian Federation, two clinical trials by iM4TB foundation are in progress. High tolerability and a favorable safety profile of the drug in the studied dose range were demonstrated both in healthy volunteers and in patients with newly diagnosed pulmonary tuberculosis with bacterial excretion and preserved sensitivity to isoniazid and rifampicin. The main pharmacokinetics parameters of macozinone after single and multiple administration in the dosage range up to 1280 mg were studied, and a statistically significant efficacy of the drug after monotherapy at a dose of 640 mg a day was established, which allowed the preferred regimen of its intake to be determined.
A thorough study aimed at interactions of macozinone with a spectrum of clinically used and experimental TB drugs was recently performed [
30]. It revealed that macozinone does not have synergistic or antagonistic interactions with the tested first-line (rifampin, isoniazid, ethambutol) or second-line (amikacin, levofloxacin, moxifloxacin, D-cycloserin, ethionamide,
para-aminosalicyc acid) drugs. Among the tested re-purposed or new drugs, clarithromycin, delamanid, lansoprazole sulfide, linezolid, meropenem or sutezolid did not show synergistic effects, when tested individually with macozinone by the checkerboard assay. Synergism was observed for macozinone and clofazimine or bedaquiline, confirming previous findings [
20,
41]. At the same time, enumeration of colony forming units after drug exposure revealed the next two potentially synergistic candidates—delamanid and sutezolid. In the mouse model of TB, the combination of macozinone-delamanid-sutezolid was more active in the lungs of
M. tuberculosis-infected animals compared to the regimen of rifampin-isoniazid-pyrazinamide, while the bacterial burden in spleen remained comparable. However, increased toxicity of the combination for HepG2 cells was observed, so further studies are needed to evaluate the potential of this drug combination [
30]. Nevertheless, neither antagonism nor increased toxicity was found for most combinations, which paves the way for using macozinone in the development of more efficient TB regimens [
30].