Determining Risk Factors for the Development of Temporomandibular Disorders during Orthodontic Treatment
Abstract
Featured Application
Abstract
1. Introduction
2. Materials and Methods
Evaluation for TMD
3. Results
Development of Symptoms of TMD
4. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- Ohrbach, R.; Dworkin, S.F. The Evolution of TMD Diagnosis: Past, Present, Future. J. Dent. Res. 2016, 95, 1093–1101. [Google Scholar] [CrossRef] [PubMed]
- Liu, F.; Steinkeler, A. Epidemiology, diagnosis, and treatment of temporomandibular disorders. Dent. Clin. 2013, 57, 465–479. [Google Scholar] [CrossRef] [PubMed]
- Jeon, H.M.; Ahn, Y.W.; Jeong, S.H.; Ok, S.M.; Choi, J.; Lee, J.Y.; Joo, J.Y.; Kwon, E.Y. Pattern analysis of patients with temporomandibular disorders resulting from unilateral mastication due to chronic periodontitis. J. Periodontal Implant Sci. 2017, 47, 211–218. [Google Scholar] [CrossRef] [PubMed]
- Ugolini, A.; Parodi, G.B.; Casali, C.; Silvestrini-Biavati, A.; Giacinti, F. Work-related traumatic dental injuries: Prevalence, characteristics and risk factors. Dent. Traumatol. 2018, 34, 36–40. [Google Scholar] [CrossRef]
- Lobbezoo, F.; Ahlberg, J.; Raphael, K.G.; Wetselaar, P.; Glaros, A.G.; Kato, T.; Santiago, V.; Winocur, E.; De Laat, A.; De Leeuw, R.; et al. International consensus on the assessment of bruxism: Report of a work in progress. J. Oral Rehabil. 2018, 45, 837–844. [Google Scholar] [CrossRef]
- Al-Baghdadi, M.; Durham, J.; Araujo-Soares, V.; Robalino, S.; Errington, L.; Steele, J. TMJ Disc Displacement without Reduction Management: A Systematic Review. J. Dent. Res. 2014, 93, 37S–51S. [Google Scholar] [CrossRef]
- Mongini, F.; Evangelista, A.; Rota, E.; Ferrero, L.; Ugolini, A.; Ceccarelli, M.; Ciccone, G.; Galassi, C. Long-term benefits of an educational and physical program on headache, and neck and shoulder pain, in a working community. J. Pain 2009, 10, 1138–1145. [Google Scholar] [CrossRef]
- Mongini, F.; Evangelista, A.; Rota, E.; Ferrero, L.; Ugolini, A.; Milani, C.; Ceccarelli, M.; Joffrain, L.; Ciccone, G.; Galassi, C. Further evidence of the positive effects of an educational and physical program on headache, neck and shoulder pain in a working community. J. Headache Pain 2010, 11, 409–415. [Google Scholar] [CrossRef][Green Version]
- Conti, A.C.; Oltramari, P.V.; Navarro, R.D.; Almeida, M.R. Examination of temporomandibular disorders in the orthodontic patient: A clinical guide. J. Appl. Oral Sci. 2007, 15, 77–82. [Google Scholar] [CrossRef][Green Version]
- Hwang, S.H.; Park, S.G. Experience of Orthodontic Treatment and Symptoms of Temporomandibular Joint in South Korean Adults. Iran J. Public Health 2018, 47, 13–17. [Google Scholar]
- Michelotti, A.; Iodice, G. The role of orthodontics in temporomandibular disorders. J. Oral Rehabil. 2010, 37, 411–429. [Google Scholar] [CrossRef] [PubMed]
- Mohlin, B.; Axelsson, S.; Paulin, G.; Pietilä, T.; Bondemark, L.; Brattström, V.; Hansen, K.; Holm, A.K. TMD in relation to malocclusion and orthodontic treatment: A systematic review. Angle Orthod. 2007, 77, 542–548. [Google Scholar] [CrossRef]
- Fernández-González, F.J.; Cañigral, A.; López-Caballo, J.L.; Brizuela, A.; Moreno-Hay, I.; del Río-Highsmith, J.; Vega, J.A. Influence of orthodontic treatment on temporomandibular disorders. A systematic review. J. Clin. Exp. Dent. 2015, 7, e320. [Google Scholar] [CrossRef] [PubMed]
- Minghelli, B.; Cardoso, I.; Porfírio, M.; Gonçalves, R.; Cascalheiro, S.; Barreto, V.; Soeiro, A.; Almeida, L. Prevalence of temporomandibular disorder in children and adolescents from public schools in Southern Portugal. N. Am. J. Med. Sci. 2014, 6, 126–132. [Google Scholar] [CrossRef]
- Fischman, S.L. Current status of indices of plaque. J. Clin. Periodontol. 1986, 13, 371–374. [Google Scholar] [CrossRef]
- Schiffman, E.; Ohrbach, R.; Truelove, E.; Look, J.; Anderson, G.; Goulet, J.P.; List, T.; Svensson, P.; Gonzalez, Y.; Lobbezoo, F.; et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: Recommendations of the International RDC/TMD Consortium Network and Orofacial Pain Special Interest Group. J. Oral Facial Pain Headache 2014, 28, 6–27. [Google Scholar] [CrossRef] [PubMed]
- Aaseth, K.; Grande, R.B.; Lundqvist, C.; Russell, M.B. Pericranial tenderness in chronic tension-type headache: The Akershus population-based study of chronic headache. J. Headache Pain 2014, 15, 58. [Google Scholar] [CrossRef]
- Mongini, F.; Ciccone, G.; Ceccarelli, M.; Baldi, I.; Ferrero, L. Muscle tenderness in different types of facial pain and its relation to anxiety and depression: A cross-sectional study on 649 patients. Pain 2007, 131, 106–111. [Google Scholar] [CrossRef]
- Jensen, R.; Rasmussen, B.K. Muscular disorders in tension-type headache. Cephalalgia 1996, 16, 97–103. [Google Scholar] [CrossRef]
- Hatch, J.P.; Rugh, J.D.; Sakai, S.; Prihoda, T.J. Reliability of the craniomandibular index. J. Orofac. Pain 2002, 16, 284–295. [Google Scholar]
- Pezzoli, M.; Ugolini, A.; Rota, E.; Ferrero, L.; Milani, C.; Pezzoli, L.; Pecorari, G.; Mongini, F. Tinnitus and its relationship with muscle tenderness in patients with headache and facial pain. J. Laryngol. Otol. 2015, 129, 638–643. [Google Scholar] [CrossRef]
- Mazzi, F.; Morosini, P.; De Girolamo, G.; Lussetti, M.; Guaraldi, G.P. SCID-I-Structured Clinical Interview for DSM-IV Axis I Disorders, Italian Edition; OS Organizzazioni Speciali: Firenze, Italy, 2000. [Google Scholar]
- Bendtsen, L.; Jensen, R.; Jensen, N.K.; Olesen, J. Pressure-controlled palpation: A new technique which increases the reliability of manual palpation. Cephalalgia 1995, 15, 205–210. [Google Scholar] [CrossRef]
- Chisnoiu, A.M.; Picos, A.M.; Popa, S.; Chisnoiu, P.D.; Lascu, L.; Picos, A.; Chisnoiu, R. Factors involved in the etiology of temporomandibular disorders—A literature review. Clujul Med. 2015, 88, 473–478. [Google Scholar] [CrossRef] [PubMed]
- Tecco, S.; Marzo, G.; Crincoli, V.; Di Bisceglie, B.; Tetè, S.; Festa, F. The prognosis of myofascial pain syndrome (MPS) during a fixed orthodontic treatment. Cranio 2012, 30, 52–71. [Google Scholar] [CrossRef] [PubMed]
- Almoznino, G.; Zini, A.; Zakuto, A.; Zlutsky, H.; Bekker, S.; Shay, B.; Haviv, Y.; Sharav, Y.; Benoliel, R. Cervical muscle tenderness in temporomandibular disorders and its association with diagnosis, disease related outcomes, and comorbid pain conditions. J. Oral Facial Pain Headache. 2020, 34, 67–76. [Google Scholar] [CrossRef] [PubMed]
- MacFarlane, T.V.; Kenealy, P.; Kingdon, H.A.; Mohlin, B.O.; Pilley, J.R.; Richmond, S.; Shaw, W.C. Twenty-year cohort study of health gain from orthodontic treatment: Temporomandibular disorders. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 692.e1–692.e8. [Google Scholar] [CrossRef]
- Keeling, S.D.; McGorray, S.; Wheeler, T.T.; King, G.J. Risk factors associated with temporomandibular joint sounds in children 6 to 12 years of age. Am. J. Orthod. Dentofac. Orthop. 1994, 105, 279–287. [Google Scholar] [CrossRef]
- Kindler, S.; Samietz, S.; Houshmand, M.; Grabe, H.J.; Bernhardt, O.; Biffar, R.; Kocher, T.; Meyer, G.; Völzke, H.; Metelmann, H.R.; et al. Depressive and anxiety symptoms as risk factors for temporomandibular joint pain: A prospective cohort study in the general population. J. Pain 2012, 13, 1188–1197. [Google Scholar] [CrossRef]
- Mongini, F.; Rota, E.; Evangelista, A.; Ciccone, G.; Milani, C.; Ugolini, A.; Ferrero, L.; Mongini, T.; Rosato, R. Personality profiles and subjective perception of pain in head pain patients. Pain 2009, 144, 125–129. [Google Scholar] [CrossRef] [PubMed]
- List, T.; Jensen, R.H. Temporomandibular disorders: Old ideas and new concepts. Cephalalgia 2017, 37, 692–704. [Google Scholar] [CrossRef]
- Rota, E.; Evangelista, A.; Ciccone, G.; Ferrero, L.; Ugolini, A.; Milani, C.; Ceccarelli, M.; Galassi, C.; Mongini, F. Effectiveness of an educational and physical program in reducing accompanying symptoms in subjects with head and neck pain: A workplace controlled trial. J. Headache Pain 2011, 12, 339–345. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Scrivani, S.J.; Keith, D.A.; Kaban, L.B. Temporomandibular disorders. N. Engl. J. Med. 2008, 359, 2693–2705. [Google Scholar] [CrossRef] [PubMed]
- Apkarian, A.V.; Baliki, M.N.; Geha, P.Y. Towards a theory of chronic pain. Prog. Neurobiol. 2009, 87, 81–97. [Google Scholar] [CrossRef] [PubMed]
- Slade, G.D.; Ohrbach, R.; Greenspan, J.D.; Fillingim, R.B.; Bair, E.; Sanders, A.E.; Dubner, R.; Diatchenko, L.; Meloto, C.B.; Smith, S.; et al. Painful Temporomandibular Disorder: Decade of Discovery from OPPERA Studies. J. Dent. Res. 2016, 95, 1084–1092. [Google Scholar] [CrossRef]
- Schwahn, C.; Grabe, H.J.; Meyer zu Schwabedissen, H.; Teumer, A.; Schmidt, C.O.; Brinkman, C.; Kocher, T.; Nauck, M.; Volzke, H.; Biffar, R.; et al. The effect of catechol-O-methyltransferase polymorphisms on pain is modified by depressive symptoms. Eur. J. Pain 2012, 16, 878–889. [Google Scholar] [CrossRef]
- Michelotti, A.; Liguori, R.; Toriello, M.; D’Antò, V.; Vitale, D.; Castaldo, G.; Sacchetti, L. Catechol-O-methyltransferase (COMT) gene polymorphisms as risk factor in temporomandibular disorders patients from Southern Italy. Clin. J. Pain 2014, 30, 129–133. [Google Scholar] [CrossRef]
| Sample n° = 224 | Subjects | |||
|---|---|---|---|---|
| Males | Females | Total | % | |
| Gender | 105 | 119 | 224 | |
| Age at T0 (mean ± SD in years) | 28 ± 8.3 | |||
| Anxiety or depression at T0 | 18 | 39 | 57 | 25.4 |
| Somatic symptoms > 4 | 31 | 55 | 86 | 38.3 |
| Class I malocclusion at T0 | 55 | 61 | 116 | 51.9 |
| Class II malocclusion at T0 | 37 | 50 | 87 | 38.6 |
| Class III malocclusion at T0 | 14 | 7 | 21 | 9.5 |
| Extraction of premolars during treatment | 17 | 23 | 40 | 17.7 |
| Duration of orthodontic treatment (T1 − T0 in months) | 21 ± 3.5 | |||
| Overjet (mm) at T0 | 5 ± 4.1 | |||
| Overbite (mm) at T0 | 4 ± 3.9 | |||
| Tongue thrust at T0 | 49 | 45 | 94 | 42.1 |
| Oral hygiene status during treatment (plaque index Silness/Loe > 2) [15] | 64 | 54 | 118 | 52.5 |
| Crossbite at T0 | 20 | 24 | 44 | |
| TMD evaluation | ||||
| Males | Females | Total | % | |
| Clicking of the TMJ at T0 | Symptom free at T0 (selection criteria) | |||
| Clicking of the TMJ at T1 | 9 | 18 | 27 | 12.0 |
| Clicking of the TMJ at T2 | 3 | 7 | 10 | 4.4 |
| MTS score ≥ 2 at T0 | 45 | 70 | 115 | 51.3 |
| MTS score ≥ 2 at T1 | 55 | 89 | 145 | 64.6 |
| MTS score ≥ 2 at T2 | 41 | 60 | 101 | 44.9 |
| CTS score ≥ 2 at T0 | 62 | 78 | 141 | 62.7 |
| CTS score ≥ 2 at T1 | 67 | 88 | 155 | 69.0 |
| CTS score ≥ 2 at T2 | 55 | 72 | 127 | 56.9 |
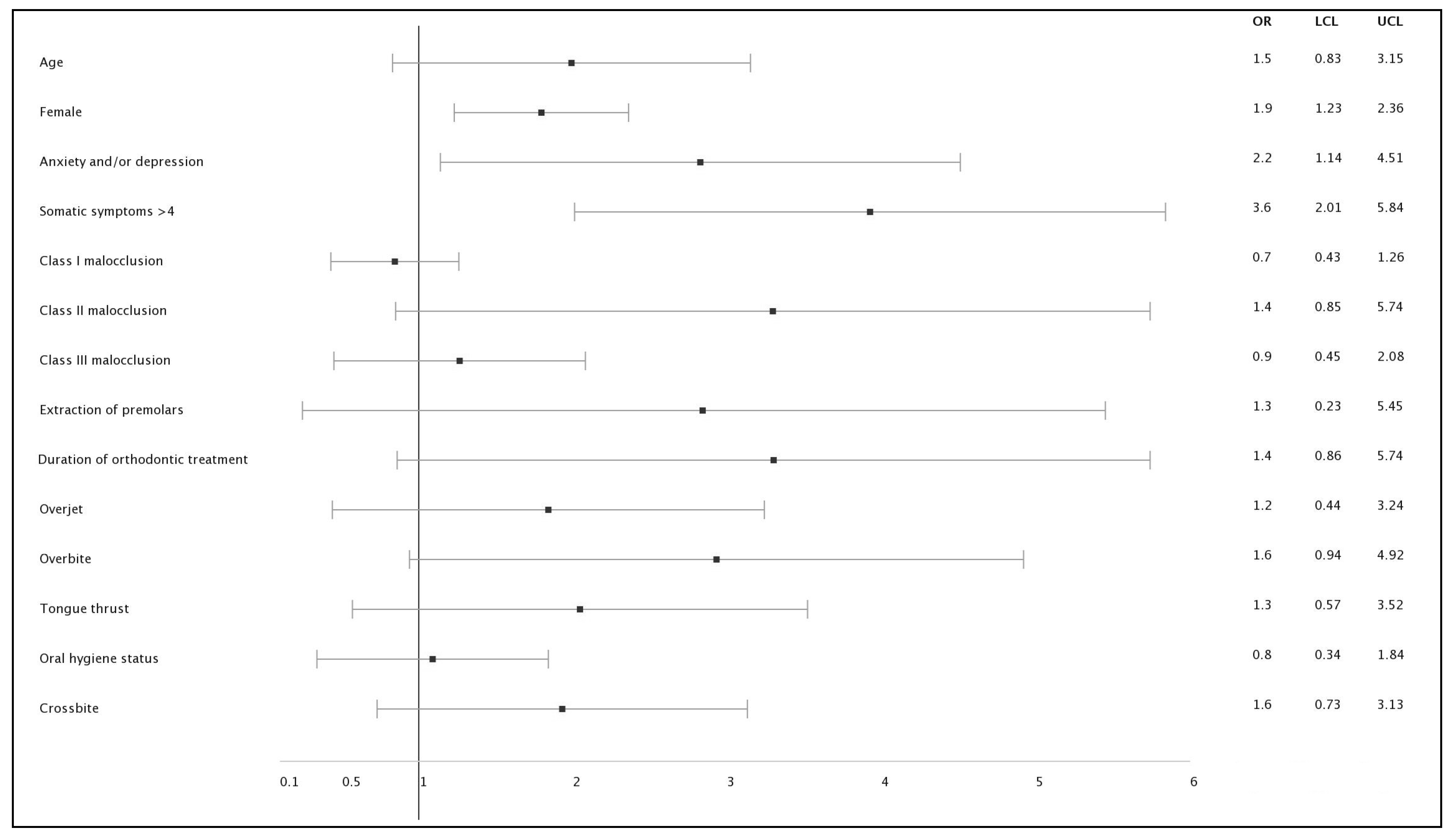
| Variable | β (Regression Coefficient) | Odds Ratio | 95% CI | p Value | |
|---|---|---|---|---|---|
| Age | 0.581 | 1.5 | 0.83 | 3.15 | 0.28 |
| Female | 1243 | 1.9 | 1.23 | 2.36 | <0.01 * |
| Anxiety or depression | 1.398 | 2.2 | 1.14 | 4.51 | <0.01 * |
| Somatic symptoms >4 | 2048 | 3.6 | 2.01 | 5.84 | <0.01 * |
| Class I malocclusion | −0.326 | 0.7 | 0.43 | 1.26 | 0.76 |
| Class II malocclusion | −0.277 | 1.4 | 0.85 | 5.74 | 0.14 |
| Class III malocclusion | 0.438 | 0.9 | 0.45 | 2.08 | 0.86 |
| Extraction of premolars | 0.627 | 1.3 | 0.23 | 5.45 | 0.74 |
| Duration of orthodontic treatment | −0.562 | 1.4 | 0.86 | 5.74 | 0.14 |
| Overjet | 0.273 | 1.2 | 0.44 | 3.24 | 0.31 |
| Overbite | −0.364 | 1.6 | 0.94 | 4.92 | 0.14 |
| Tongue thrust | 0.442 | 1.3 | 0.57 | 3.52 | 0.32 |
| Oral hygiene status | −0.383 | 0.8 | 0.34 | 1.84 | 0.42 |
| Crossbite | 0.397 | 1.6 | 0.73 | 3.13 | 0.31 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ugolini, A.; Garbarino, F.; Di Vece, L.; Silvestrini-Biavati, F.; Lanteri, V. Determining Risk Factors for the Development of Temporomandibular Disorders during Orthodontic Treatment. Appl. Sci. 2020, 10, 8216. https://doi.org/10.3390/app10228216
Ugolini A, Garbarino F, Di Vece L, Silvestrini-Biavati F, Lanteri V. Determining Risk Factors for the Development of Temporomandibular Disorders during Orthodontic Treatment. Applied Sciences. 2020; 10(22):8216. https://doi.org/10.3390/app10228216
Chicago/Turabian StyleUgolini, Alessandro, Federico Garbarino, Luca Di Vece, Francesca Silvestrini-Biavati, and Valentina Lanteri. 2020. "Determining Risk Factors for the Development of Temporomandibular Disorders during Orthodontic Treatment" Applied Sciences 10, no. 22: 8216. https://doi.org/10.3390/app10228216
APA StyleUgolini, A., Garbarino, F., Di Vece, L., Silvestrini-Biavati, F., & Lanteri, V. (2020). Determining Risk Factors for the Development of Temporomandibular Disorders during Orthodontic Treatment. Applied Sciences, 10(22), 8216. https://doi.org/10.3390/app10228216







