In Vitro Comparison of Surgical Implant Placement Accuracy Using Guides Fabricated by Three Different Additive Technologies
Abstract
1. Introduction
2. Materials and Methods
2.1. Model Preparation
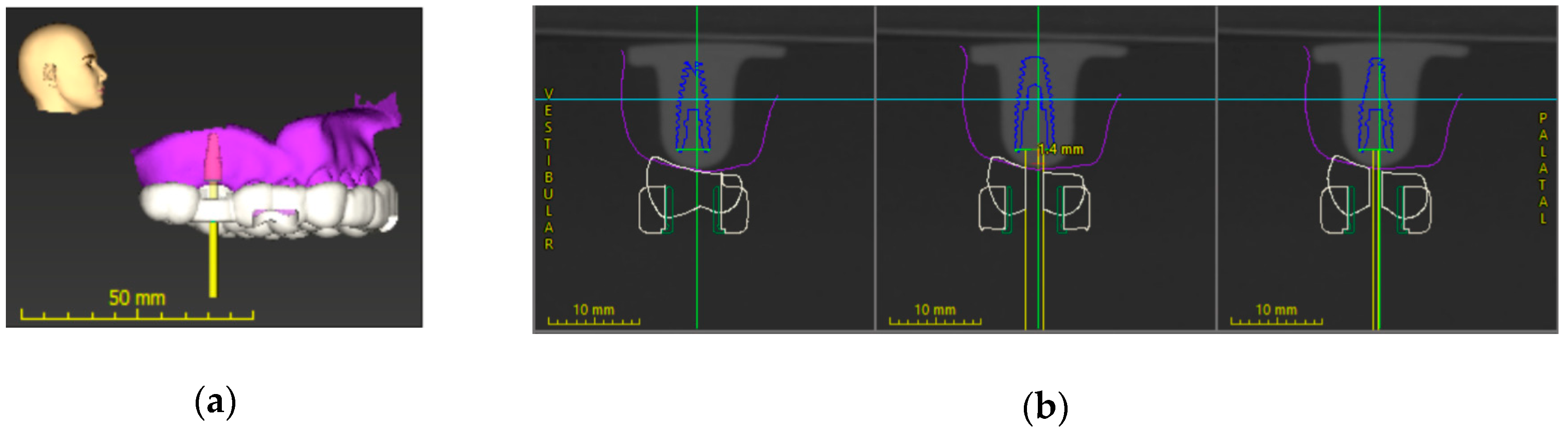
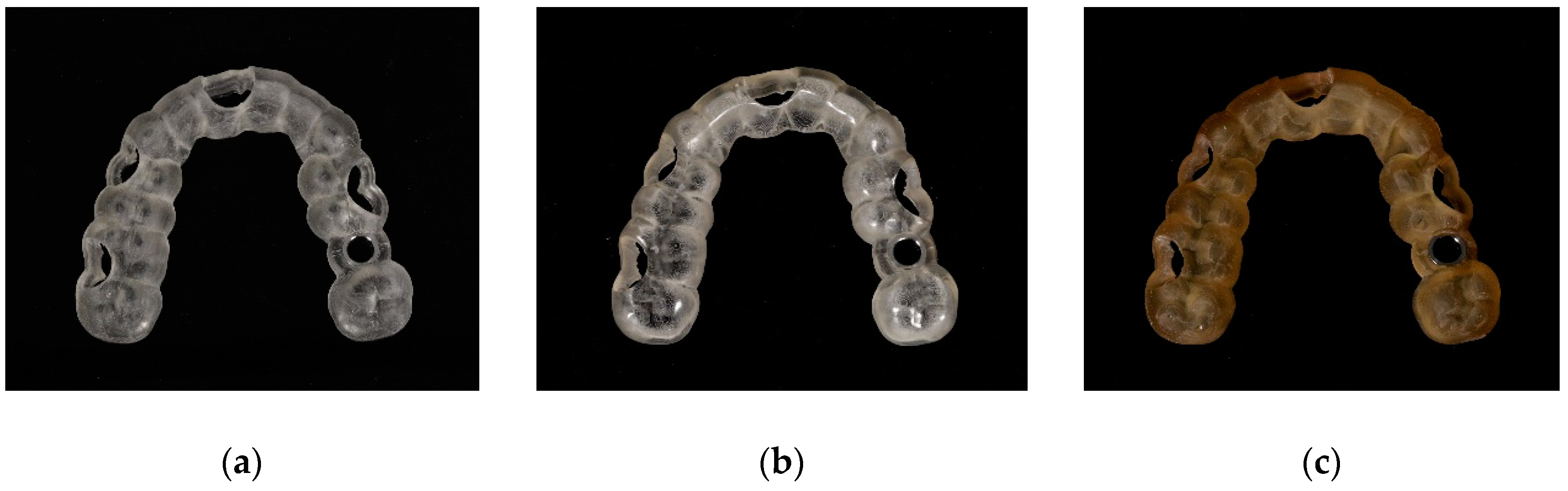
2.2. Implant Position Planning Procedure and Surgical Guide Fabrication
2.3. Post-Processing
2.4. Implant Placement Procedure
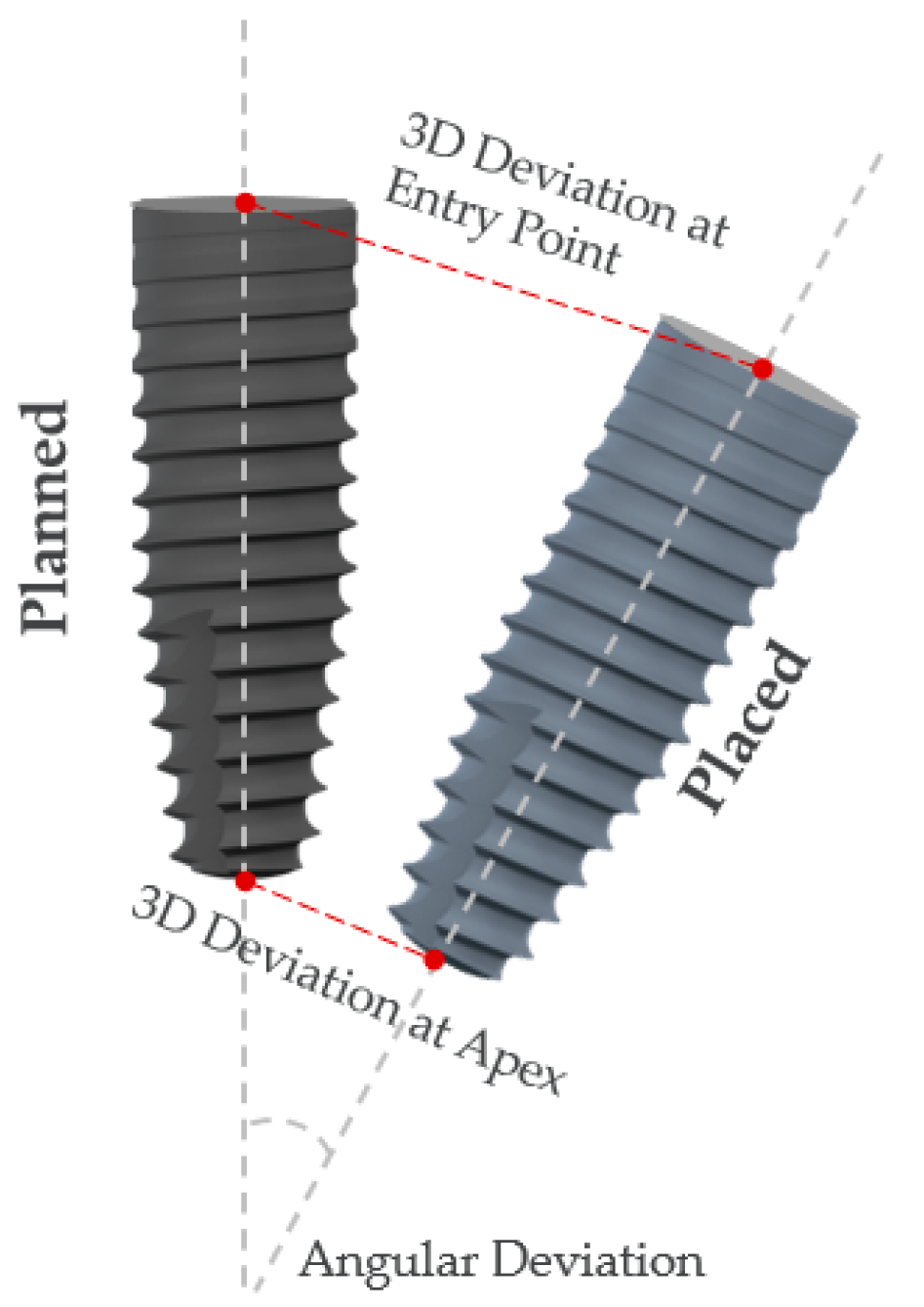
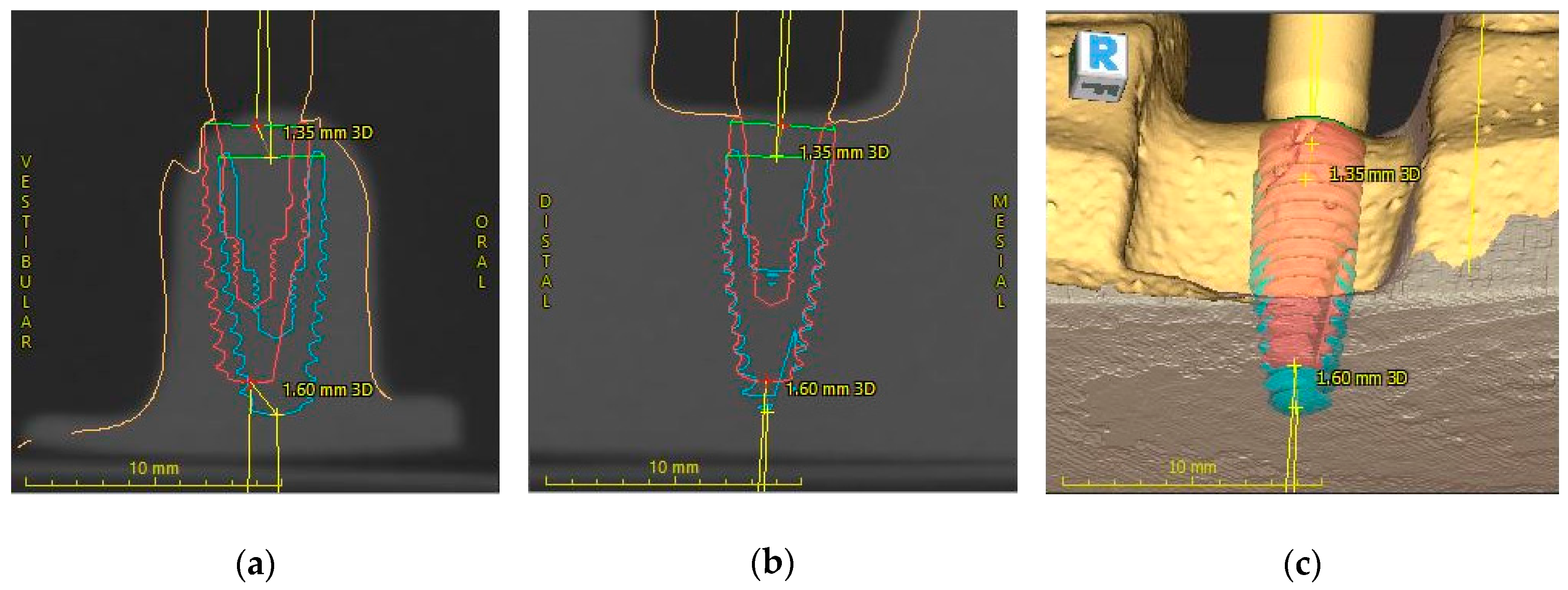
2.5. Implant Position Accuracy Measurement
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Kernen, F.; Kramer, J.; Wanner, L.; Wismeijer, D.; Nelson, K.; Flügge, T. A review of virtual planning software for guided implant surgery-data import and visualization, drill guide design and manufacturing. BMC Oral Health 2020, 20, 251. [Google Scholar] [CrossRef]
- Kessler, A.; Hickel, R.; Reymus, M. 3D Printing in Dentistry-State of the Art. Oper Dent 2020, 45, 30–40. [Google Scholar] [CrossRef]
- Kim, S.Y.; Shin, Y.S.; Jung, H.D.; Hwang, C.J.; Baik, H.S.; Cha, J.Y. Precision and trueness of dental models manufactured with different 3-dimensional printing techniques. Am. J. Orthod. Dentofac. Orthop. 2018, 153, 144–153. [Google Scholar] [CrossRef]
- Oberoi, G.; Nitsch, S.; Edelmayer, M.; Janjić, K.; Müller, A.S.; Agis, H. 3D Printing—Encompassing the Facets of Dentistry. Front. Bioeng. Biotechnol. 2018, 6. [Google Scholar] [CrossRef]
- Rungrojwittayakul, O.; Kan, J.Y.; Shiozaki, K.; Swamidass, R.S.; Goodacre, B.J.; Goodacre, C.J.; Lozada, J.L. Accuracy of 3D Printed Models Created by Two Technologies of Printers with Different Designs of Model Base. J. Prosthodont. 2020, 29, 124–128. [Google Scholar] [CrossRef]
- Brown, G.B.; Currier, G.F.; Kadioglu, O.; Kierl, J.P. Accuracy of 3-dimensional printed dental models reconstructed from digital intraoral impressions. Am. J. Orthod. Dentofac. Orthop. 2018, 154, 733–739. [Google Scholar] [CrossRef]
- Favero, C.S.; English, J.D.; Cozad, B.E.; Wirthlin, J.O.; Short, M.M.; Kasper, F.K. Effect of print layer height and printer type on the accuracy of 3-dimensional printed orthodontic models. Am. J. Orthod. Dentofac. Orthop. 2017, 152, 557–565. [Google Scholar] [CrossRef]
- Park, M.-E.; Shin, S.-Y. Three-dimensional comparative study on the accuracy and reproducibility of dental casts fabricated by 3D printers. J. Prosthet. Dent. 2018, 119, 861.e1–861.e7. [Google Scholar] [CrossRef]
- Sun, Y.; Ding, Q.; Tang, L.; Zhang, L.; Sun, Y.; Xie, Q. Accuracy of a chairside fused deposition modeling 3D-printed single-tooth surgical template for implant placement: An in vitro comparison with a light cured template. J. Cranio-Maxillofac. Surg. 2019, 47, 1216–1221. [Google Scholar] [CrossRef]
- Di Giacomo, G.A.; Cury, P.R.; de Araujo, N.S.; Sendyk, W.R.; Sendyk, C.L. Clinical application of stereolithographic surgical guides for implant placement: Preliminary results. J. Periodontol. 2005, 76, 503–507. [Google Scholar] [CrossRef]
- Arisan, V.; Karabuda, C.Z.; Mumcu, E.; Özdemir, T. Implant positioning errors in freehand and computer-aided placement methods: A single-blind clinical comparative study. Int. J. Oral Maxillofac. Implants 2013, 28, 190–204. [Google Scholar] [CrossRef]
- Vercruyssen, M.; Hultin, M.; Van Assche, N.; Svensson, K.; Naert, I.; Quirynen, M. Guided surgery: Accuracy and efficacy. Periodontology 2000 2014, 66, 228–246. [Google Scholar] [CrossRef] [PubMed]
- Cassetta, M.; Di Mambro, A.; Giansanti, M.; Stefanelli, L.V.; Barbato, E. Is it possible to improve the accuracy of implants inserted with a stereolithographic surgical guide by reducing the tolerance between mechanical components? Int. J. Oral Maxillofac. Surg. 2013, 42, 887–890. [Google Scholar] [CrossRef] [PubMed]
- Zhou, W.; Liu, Z.; Song, L.; Kuo, C.-L.; Shafer, D. Clinical Factors Affecting the Accuracy of Guided Implant Surgery—A Systematic Review and Meta-analysis. J. Evid. Based Dent. Pract. 2017, 18. [Google Scholar] [CrossRef]
- Al Yafi, F.; Camenisch, B.; Al-Sabbagh, M. Is Digital Guided Implant Surgery Accurate and Reliable? Dent. Clin. N. Am. 2019, 63, 381–397. [Google Scholar] [CrossRef] [PubMed]
- El Kholy, K.; Janner, S.F.M.; Schimmel, M.; Buser, D. The influence of guided sleeve height, drilling distance, and drilling key length on the accuracy of static Computer-Assisted Implant Surgery. Clin. Implant Dent. Relat. Res. 2019, 21, 101–107. [Google Scholar] [CrossRef]
- Deeb, G.R.; Allen, R.K.; Hall, V.P.; Whitley, D., 3rd; Laskin, D.M.; Bencharit, S. How Accurate Are Implant Surgical Guides Produced with Desktop Stereolithographic 3-Dimentional Printers? J. Oral Maxillofac. Surg. 2017, 75, 2559.e1–2559.e8. [Google Scholar] [CrossRef]
- Herschdorfer, L.; Negreiros, W.M.; Gallucci, G.O.; Hamilton, A. Comparison of the accuracy of implants placed with CAD-CAM surgical templates manufactured with various 3D printers: An in vitro study. J. Prosthet. Dent. 2020. [Google Scholar] [CrossRef]
- Bover-Ramos, F.; Viña-Almunia, J.; Cervera-Ballester, J.; Peñarrocha-Diago, M.; García-Mira, B. Accuracy of Implant Placement with Computer-Guided Surgery: A Systematic Review and Meta-Analysis Comparing Cadaver, Clinical, and In Vitro Studies. Int. J. Oral Maxillofac. Implants 2018, 33, 101–115. [Google Scholar] [CrossRef]
- Sigcho López, D.A.; García, I.; Da Silva Salomao, G.; Cruz Laganá, D. Potential Deviation Factors Affecting Stereolithographic Surgical Guides: A Systematic Review. Implant Dent. 2019, 28, 68–73. [Google Scholar] [CrossRef]
- Tahmaseb, A.; Wu, V.; Wismeijer, D.; Coucke, W.; Evans, C. The accuracy of static computer-aided implant surgery: A systematic review and meta-analysis. Clin. Oral Implants Res. 2018, 29, 416–435. [Google Scholar] [CrossRef]
- Behneke, A.; Burwinkel, M.; Behneke, N. Factors influencing transfer accuracy of cone beam CT-derived template-based implant placement. Clin. Oral Implants Res. 2012, 23, 416–423. [Google Scholar] [CrossRef]
- Ersoy, A.E.; Turkyilmaz, I.; Ozan, O.; McGlumphy, E.A. Reliability of implant placement with stereolithographic surgical guides generated from computed tomography: Clinical data from 94 implants. J. Periodontol. 2008, 79, 1339–1345. [Google Scholar] [CrossRef]
- Ozan, O.; Turkyilmaz, I.; Yilmaz, B. A preliminary report of patients treated with early loaded implants using computerized tomography-guided surgical stents: Flapless versus conventional flapped surgery. J. Oral Rehabil. 2007, 34, 835–840. [Google Scholar] [CrossRef]
- Pozzi, A.; Polizzi, G.; Moy, P.K. Guided surgery with tooth-supported templates for single missing teeth: A critical review. Eur. J. Oral Implantol. 2016, 9 (Suppl. S1), S135–S153. [Google Scholar]
- Tahmaseb, A.; Wismeijer, D.; Coucke, W.; Derksen, W. Computer technology applications in surgical implant dentistry: A systematic review. Int. J. Oral Maxillofac. Implants 2014, 29, 25–42. [Google Scholar] [CrossRef]
- Younes, F.; Cosyn, J.; De Bruyckere, T.; Cleymaet, R.; Bouckaert, E.; Eghbali, A. A randomized controlled study on the accuracy of free-handed, pilot-drill guided and fully guided implant surgery in partially edentulous patients. J. Clin. Periodontol. 2018, 45, 721–732. [Google Scholar] [CrossRef]
- Derksen, W.; Wismeijer, D.; Flügge, T.; Hassan, B.; Tahmaseb, A. The accuracy of computer-guided implant surgery with tooth-supported, digitally designed drill guides based on CBCT and intraoral scanning. A prospective cohort study. Clin. Oral Implants Res. 2019, 30, 1005–1015. [Google Scholar] [CrossRef]
- Pozzi, A.; Tallarico, M.; Marchetti, M.; Scarfò, B.; Esposito, M. Computer-guided versus free-hand placement of immediately loaded dental implants: 1-year post-loading results of a multicentre randomised controlled trial. Eur. J. Oral Implantol. 2014, 7, 229–242. [Google Scholar]
- Vercruyssen, M.; Cox, C.; Coucke, W.; Naert, I.; Jacobs, R.; Quirynen, M. A randomized clinical trial comparing guided implant surgery (bone- or mucosa-supported) with mental navigation or the use of a pilot-drill template. J. Clin. Periodontol. 2014, 41, 717–723. [Google Scholar] [CrossRef]
- Amorfini, L.; Migliorati, M.; Drago, S.; Silvestrini-Biavati, A. Immediately Loaded Implants in Rehabilitation of the Maxilla: A Two-Year Randomized Clinical Trial of Guided Surgery versus Standard Procedure. Clin. Implant Dent. Relat. Res. 2017, 19, 280–295. [Google Scholar] [CrossRef]
- Bencharit, S.; Staffen, A.; Yeung, M.; Whitley, D., 3rd; Laskin, D.M.; Deeb, G.R. In Vivo Tooth-Supported Implant Surgical Guides Fabricated With Desktop Stereolithographic Printers: Fully Guided Surgery Is More Accurate Than Partially Guided Surgery. J. Oral Maxillofac. Surg. 2018, 76, 1431–1439. [Google Scholar] [CrossRef]
- El Kholy, K.; Ebenezer, S.; Wittneben, J.G.; Lazarin, R.; Rousson, D.; Buser, D. Influence of implant macrodesign and insertion connection technology on the accuracy of static computer-assisted implant surgery. Clin. Implant Dent. Relat. Res. 2019, 21, 1073–1079. [Google Scholar] [CrossRef] [PubMed]
- Rungcharassaeng, K.; Caruso, J.M.; Kan, J.Y.; Schutyser, F.; Boumans, T. Accuracy of computer-guided surgery: A comparison of operator experience. J. Prosthet. Dent. 2015, 114, 407–413. [Google Scholar] [CrossRef] [PubMed]
- El Kholy, K.; Lazarin, R.; Janner, S.F.M.; Faerber, K.; Buser, R.; Buser, D. Influence of surgical guide support and implant site location on accuracy of static Computer-Assisted Implant Surgery. Clin. Oral Implants Res. 2019, 30, 1067–1075. [Google Scholar] [CrossRef] [PubMed]
- Henprasert, P.; Dawson, D.V.; El-Kerdani, T.; Song, X.; Couso-Queiruga, E.; Holloway, J.A. Comparison of the Accuracy of Implant Position Using Surgical Guides Fabricated by Additive and Subtractive Techniques. J. Prosthodont. 2020, 29, 534–541. [Google Scholar] [CrossRef]
- Dalal, N.; Ammoun, R.; Abdulmajeed, A.A.; Deeb, G.R.; Bencharit, S. Intaglio Surface Dimension and Guide Tube Deviations of Implant Surgical Guides Influenced by Printing Layer Thickness and Angulation Setting. J. Prosthodont. 2020, 29, 161–165. [Google Scholar] [CrossRef]
| Printer | DLP | PolyJet | SLA |
|---|---|---|---|
| Model | P30+ (Straumann) | Objet® Eden260VS (Stratasys) | Form2 (Formlabs) |
| Layer thickness | 100 µm | 16.5 µm | 50 µm |
| Material | P Pro Surgical Guide Clear | MED 610 | Dental SG Resin |
| DLP (n = 10) | PolyJet (n = 10) | SLA (n = 10) | ||
|---|---|---|---|---|
| Measurement | Mean ± SD * | p-Value | ||
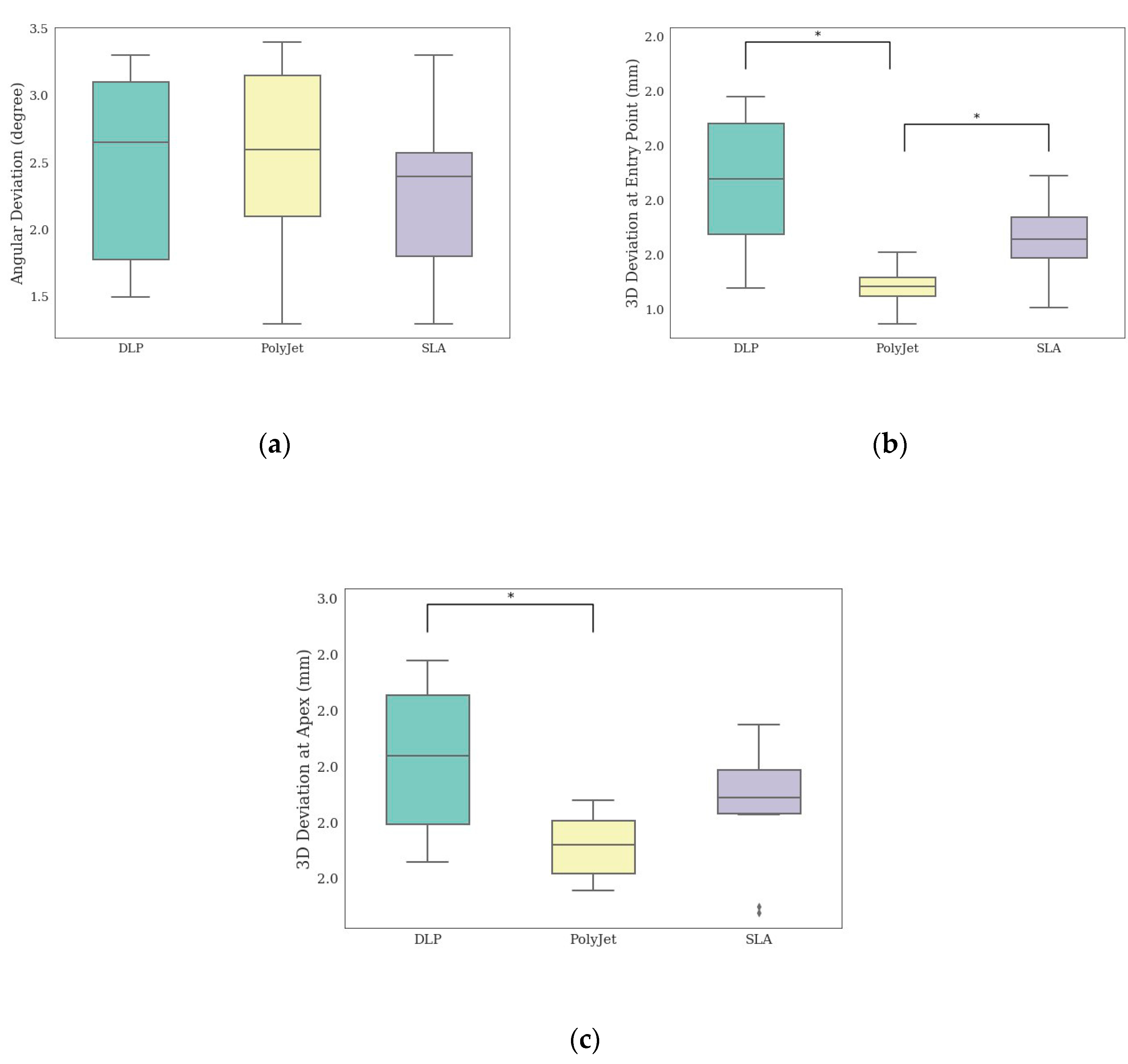
| Angular Deviation (degree) | 2.47 ± 0.72 | 2.54 ± 0.70 | 2.3 ± 0.61 | 0.72 |
| Deviation at entry point (mm) | 1.87 ± 0.25 a | 1.48 ± 0.07 b | 1.66 ± 0.15 a | <0.001 ** |
| Deviation at apex (mm) | 2.03 ± 0.26 a | 1.72 ± 0.12 b | 1.86 ± 0.22 a, b | 0.01 ** |
| Printer | DLP | PolyJet | SLA |
|---|---|---|---|
| Printing time (min) | 22 | 248 | 337 |
| Post-processing time (min) | 23 | 7 | 16 |
| Total (min) | 45 | 255 | 353 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Anunmana, C.; Ueawitthayasuporn, C.; Kiattavorncharoen, S.; Thanasrisuebwong, P. In Vitro Comparison of Surgical Implant Placement Accuracy Using Guides Fabricated by Three Different Additive Technologies. Appl. Sci. 2020, 10, 7791. https://doi.org/10.3390/app10217791
Anunmana C, Ueawitthayasuporn C, Kiattavorncharoen S, Thanasrisuebwong P. In Vitro Comparison of Surgical Implant Placement Accuracy Using Guides Fabricated by Three Different Additive Technologies. Applied Sciences. 2020; 10(21):7791. https://doi.org/10.3390/app10217791
Chicago/Turabian StyleAnunmana, Chuchai, Chananchida Ueawitthayasuporn, Sirichai Kiattavorncharoen, and Prakan Thanasrisuebwong. 2020. "In Vitro Comparison of Surgical Implant Placement Accuracy Using Guides Fabricated by Three Different Additive Technologies" Applied Sciences 10, no. 21: 7791. https://doi.org/10.3390/app10217791
APA StyleAnunmana, C., Ueawitthayasuporn, C., Kiattavorncharoen, S., & Thanasrisuebwong, P. (2020). In Vitro Comparison of Surgical Implant Placement Accuracy Using Guides Fabricated by Three Different Additive Technologies. Applied Sciences, 10(21), 7791. https://doi.org/10.3390/app10217791





