Abstract
Occlusal contact loss occasionally occurs following the placement of implant-supported fixed dental prostheses in the posterior region. This complication is caused by the change in the vertical dimension of occlusion after the recovery of mastication. The change is probably related to the prosthesis sinking phenomenon and previous mandibular dislocation. The use of interim prostheses could help re-establish the vertical dimension of occlusion. The definitive prostheses can then be accurately fabricated using digital techniques in the newly established vertical dimension. In this case report, we introduce a protocol incorporating a computer-aided design and computer-aided manufacturing (CAD-CAM) interim prosthesis and digital techniques to minimize the occurrence of unexpected initial occlusal changes in the prosthetic treatment of implant-supported prostheses in the posterior region.
1. Introduction
Severe dental caries, extensive tooth fracture, and severe periodontitis can result in impaired masticatory ability, and subsequent tooth loss is very debilitating in elderly people [1,2,3]. Replacement of the missing teeth with dental implants is a common treatment modality for restoring the masticatory ability [4,5]. Restoring the posterior edentulous area with implant-supported restorations can not only significantly improve the patient’s masticatory function [6], but also relieve the psychological stress by its chewing effect [7]. A patient-centered retrospective study reported that the oral health-related quality of life and overall treatment satisfaction were high in the implant-supported fixed dental restorations [8].
Occlusal contact loss can occur after the delivery of implant-supported fixed dental prostheses. There are several possible reasons for the changes in occlusion following the prosthetic restoration of the posterior area. First, the prosthesis sinking phenomenon can be caused by the loading applied to the implant-abutment connection in clinical practice [9,10]. The micro-roughness and irregularity of the surface at the connection of the implant and abutment can get flattened by the torque tightening, resulting in a reduced distance between the contacting surfaces [7]. Moreover, compressive force by long-term occlusal loading could generate plastic deformation of the interface of connection [11]. This settling phenomenon induces the axial displacement of the prosthesis [12]. The amount of settling of abutments to implants varies in all implant systems, and it has been reported that the implants with internal conical connection have higher settling values than those with external hexagonal connection [9,12]. Mandibular dislocation was reported in partially edentulous patients without molar supports [13]. In the unilateral occlusal support, the loss of vertical support resulted in the upward movement of the mandible in the posterior region during clenching. Analysis of the movement amplitude showed a significant difference between the edentulous conditions of the posterior teeth [14]. Analysis of electromyographic activity also revealed that the unilateral occlusal support tended to cause a unilateral activity of the masticatory muscles [14]. The muscle activity caused larger compressive loading in the contralateral temporomandibular joint that was related to the movement of the mandible. A persistent loss of posterior support could be problematic. Repetitive loading on the joint could reset the three-dimensional positions of the condyle and mandible differently from the previous position with the posterior teeth. When the upward movement on the edentulous side is applied consistently, the mandible could be settled in the displaced position.
Implant treatments involve a period of edentulous state for the healing of extraction site and osseointegration of the implants except for the concept of immediate placement and loading [15]. Thus, mandibular dislocation could be crucial in posterior edentulous patients who are planned to receive implant-supported fixed dental prostheses. After prosthesis delivery, the functional forces of the constrictor muscles are recovered that could induce changes in the mandible in the maximal intercuspal position. Thus, this resettling could be the cause of the loss of occlusal contact that occasionally occurs after the delivery of the implant-supported prostheses in the free-end edentulous cases. The present case demonstrates a strategic workflow for minimizing the initial occlusal contact loss of implant-supported fixed prostheses in the posterior region by using a computer-aided design and computer-aided manufacturing (CAD-CAM) interim prosthesis, further intraoral optical impression for registration of the newly established vertical dimension of occlusion, digital image matching technique, and computer design modification.
2. Case Presentation
A 54-year-old female patient visited the clinic with missing teeth 46 and 47. The patient mentioned that the extraction of teeth was performed over 10 years ago because of severe dental caries. Unilateral chewing habit on the left side was found owing to loss of teeth on the right posterior side. The patient had no medical history or temporomandibular disorders. Two implants (OneQ-SL, Dentis, Daegu, Korea) were placed with the insertion torque of 40 Ncm using an open flap technique, and transmucosal healing abutments were then connected on the day of the surgery. The protocol of surgical and prosthetic treatment of this study was approved by the Institutional Review Board of Kyungpook National University dental hospital (2019-08-01-00).
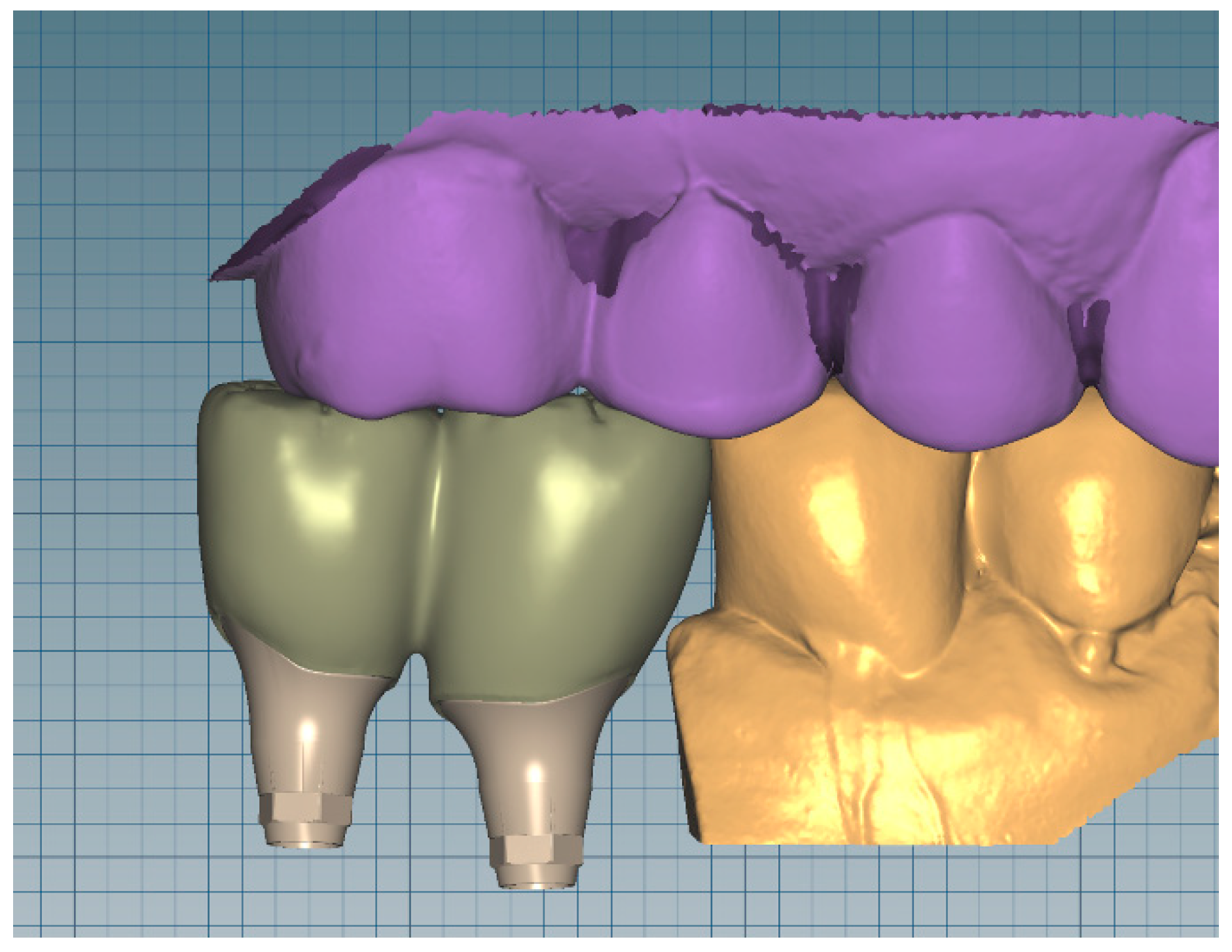
After a healing period of 3 months, a silicone impression (Aquasil Ultra XLV Regular Set and Aquasil Ultra Heavy, Dentsply Sinora, Philadelphia, PA, USA) was taken for the implants using an open tray technique with pick-up type impression copings. The fabricated stone cast was digitized using a desktop scanner (IDC S1, Amann Girrbach, Koblach, Austria) and transferred to the dental CAD software (IDC D1, Amann Girrbach, Koblach, Austria) where monotype custom prosthetic abutments and interim prosthesis were designed (Figure 1).
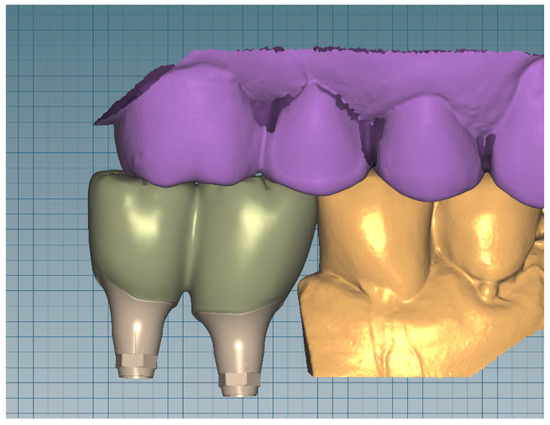
Figure 1.
Design of the monotype custom prosthetic abutments and interim prosthesis.
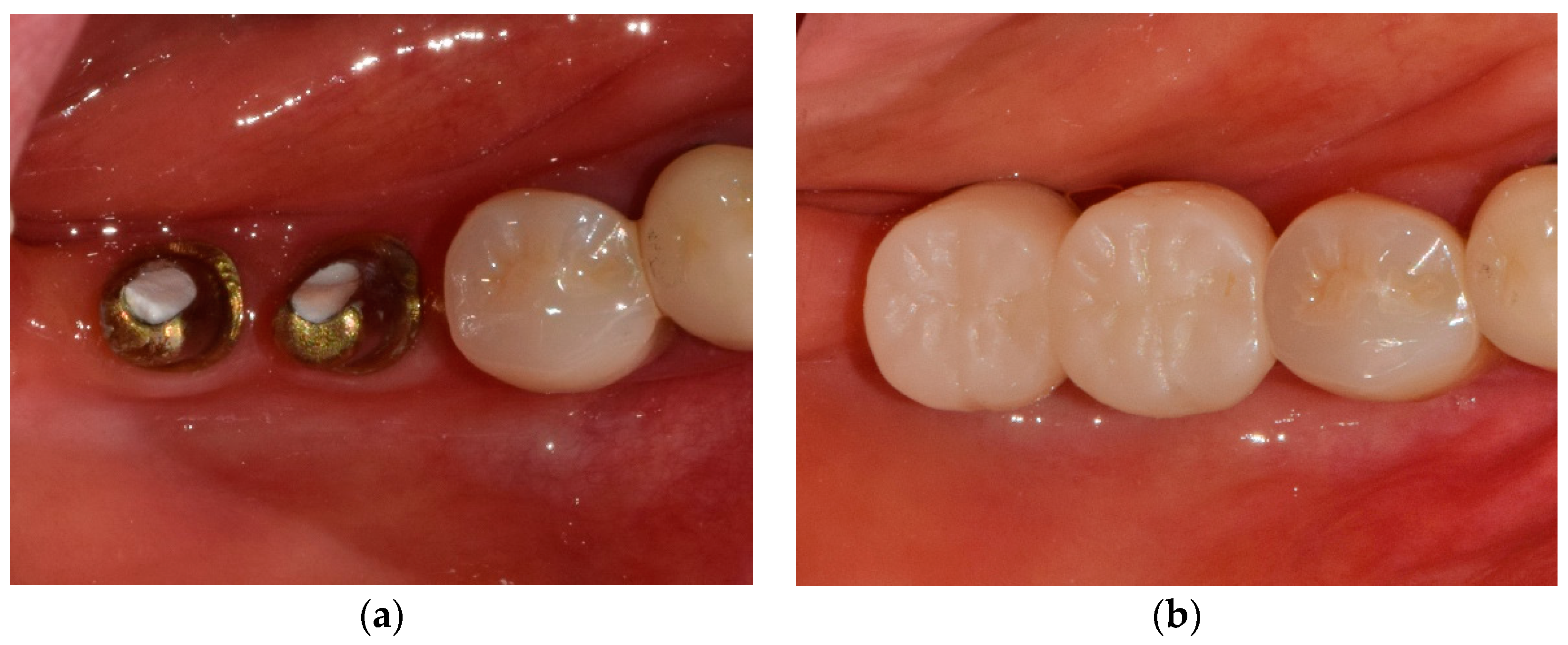
The interim prosthesis was fabricated with subtractive manufacturing using a 5-axis milling machine (ICD MILL 5X, Amann Girrbach, Koblach, Austria) and methacrylic acid ester-based cross-linked resin blocks (Ceramill TEMP, Amann Girrbach, Koblach, Austria). The custom prosthetic abutments (Ti6Al-4V ELI, Perryman Company, Houston, PA, USA) were connected to the implants, followed by cementation of the interim prosthesis using a glass ionomer cement (Fuji I, GC, Tokyo, Japan) (Figure 2). Occlusal contact points were set at maximum intercuspation, and all the lateral contacts were removed.

Figure 2.
(a) Connection of the custom prosthetic abutments to the implants. (b) Cementation of the interim prosthesis on the abutments.
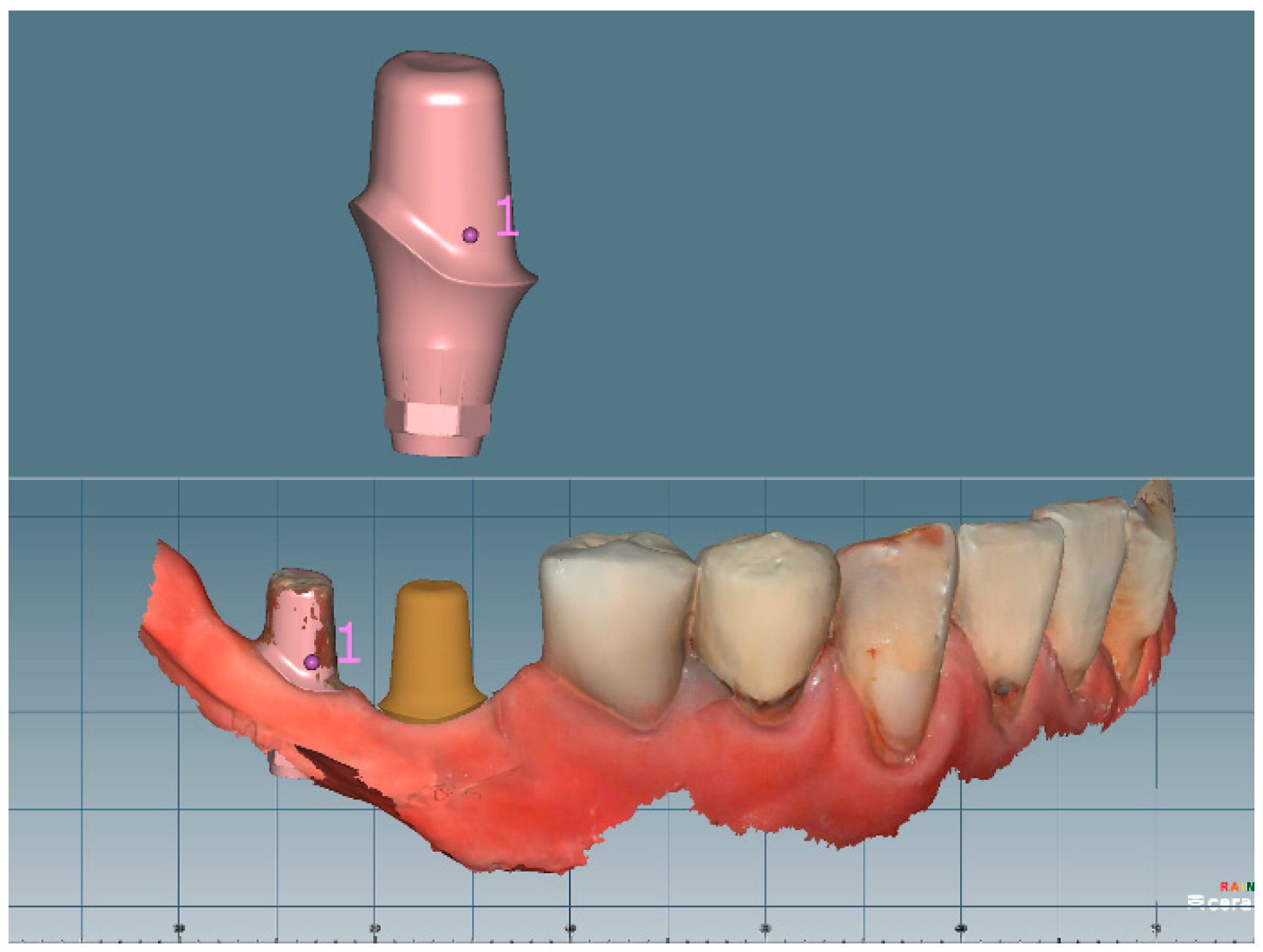
After a 3-month neuromuscular adaptation period, the interim prosthesis was removed using a reverse crown ejector (Crown remover, YDM, Tokyo, Japan), and new impressions and vertical dimension of occlusion were recorded with an intraoral optical scanner (CS3600, Carestream, Rochester, NY, USA). The scan data of the oral cavity in the polygon file format (PLY) were loaded on to the CAD software, and the abutment scan parts were replaced with the abutment designs using the point-based best-fit algorithm embedded in the software (Figure 3). This image substitution enabled the setting of an image of the intact custom abutment in the scan data. Thereafter, the design of the interim crowns was recalled, and the occlusal surface and the design margins were modified as per the newly created vertical dimension.
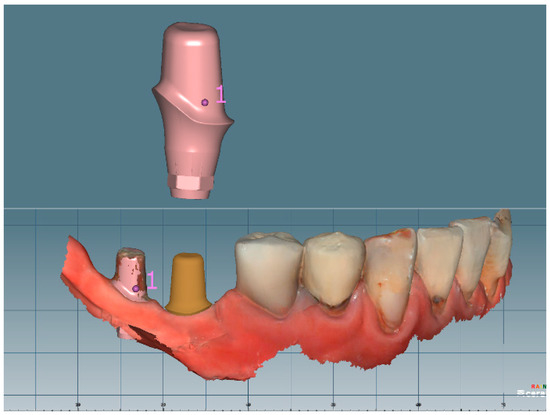
Figure 3.
Image overlapping and replacement of the abutment design with the intraoral scan data.
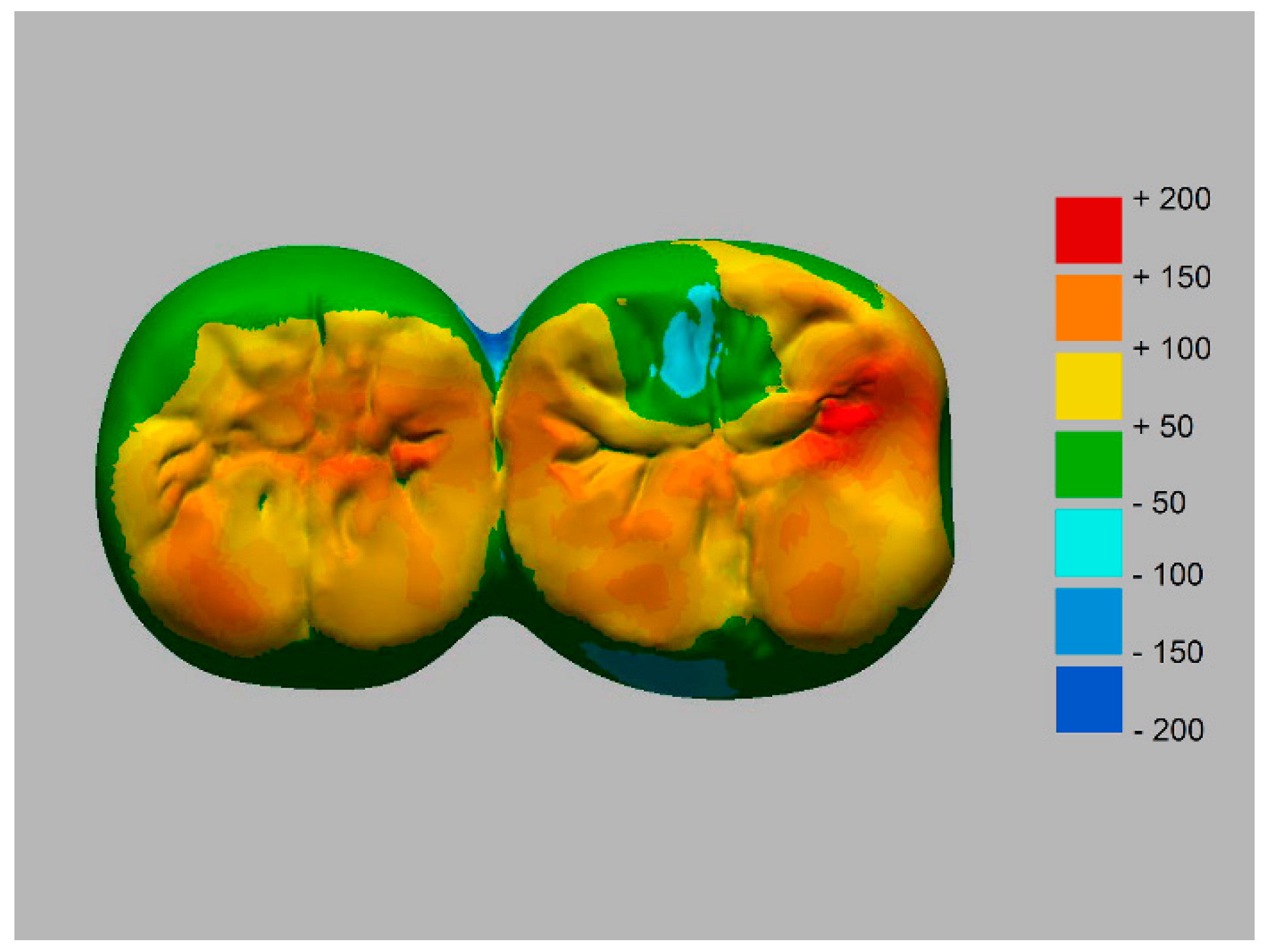
The morphological change in the prosthesis in the occlusal surface was investigated by superimposing the original and modified designs of the prosthesis in image analysis software (Geomagic DesignX, 3D Systems, Rock Hill, SC, USA) (Figure 4).
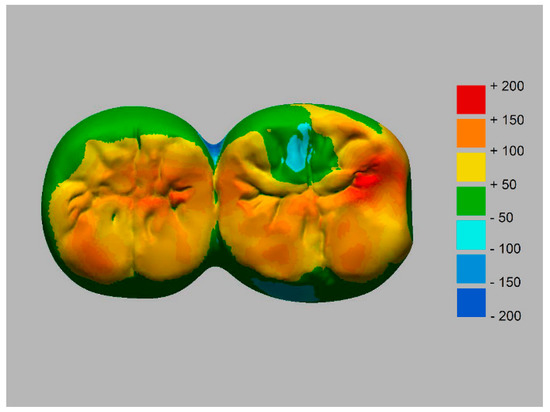
Figure 4.
Superimposed occlusal image between the original and modified designs of the prosthesis.
The final design of the crowns was converted into monolithic zirconia prosthesis using the 5-axis milling machine and a zirconium dioxide block (Prettau, Zirkonzhan, Bruneck, Italy). On the day of delivery, the definitive monolithic zirconia prosthesis was cemented using a resin-based luting cement (RelyX Unicem Clicker; 3M ESPE AG, Seefeld, Germany). Stable occlusal contact points were maintained at maximum intercuspation during the 8-month follow-up after the restoration delivery (Figure 5).

Figure 5.
Follow-up image 8 months after the end of the treatment.
3. Discussion
Loss of occlusal support can impair the masticatory performance and change the neuromuscular pattern of the jaw during masticatory activity [16,17]. When the posterior molars are missing for a long time, interim restorations are required to establish a new vertical dimension of occlusion and to give the joint and neuromuscular system the time to adapt [18]. In particular, the long-term use of interim restorations during implant treatment has been recommended [19]. In this clinical report, the interim restorations were fabricated using the CAD-CAM method, and used for 3 months to allow the settling of the abutment to the implant and stabilization of the temporomandibular joint and neuromuscular system. Afterward, the crown design was modified in accordance with the newly established vertical dimension with digital techniques, and then converted to monolithic zirconia using the milling method. The use of CAD allowed the application of modifications according to functional and aesthetic demands [20]. Image replacement of the abutments using the image superimposition technique enhanced the marginal fit of the definitive restorations. The workflow is also applicable to prefabricated abutments and different types of retention systems, such as screw-or cement-retained prosthesis.
Long-term use of interim restorations is necessary during the course of treatment using oral implants or in situations involving comprehensive occlusal reconstruction [19,20]. Since the introduction of computer-aided design and computer-aided manufacturing (CAD-CAM) to dentistry by Duret et al. [21], CAD-CAM has become an alternative to the conventional methods used for fabricating fixed interim restorations [22]. Papadiochou et al. [23] demonstrated that CAD-CAM poly (methyl methacrylate)-based interim crowns had a superior marginal fit and a uniform internal gap compared to manually fabricated crowns. Rayyan et al. [24] reported that CAD-CAM interim crowns had higher surface hardness and wear resistance. Alp et al. [25] showed high flexural strength in CAD-CAM interim polymers than in the bis-acrylate composite resin and conventional acrylic resin. Reeponmaha et al. [20] mentioned the use of CAD-CAM-fabricated high-density interim restorations enabled predictable and easier results in the prolonged pretreatment phase.
Even though this digital method can overcome the challenge of occlusal changes in the initial period after the delivery of restorations, a reliable connection between the implant and abutment should be confirmed to decrease the axial displacement of the abutment under functional loading [10,12,26]. The implant screw must be tightened with adequate torque to achieve the optimum preload [12,27,28]. In the present study, the abutment screw was retightened when the interim restoration was removed for taking the second impression, three months after the abutment connection. This additional retightening would be beneficial to compensate for the loss of vertical position of restoration caused by settling in actual clinical practice. Although the use of dental implants to restore edentulous sites is recognized as a verified treatment modality, a longitudinal outcome study [29] reported the incidence of early and late infectious postoperative complications that could lead to treatment failure, including the loss of vertical dimension. Thus, careful clinical and paraclinical examinations on postoperative infection are also needed for the maintenance of oral function.
The limitation of this workflow is that the types of prostheses for which the described digital techniques can be applied are limited to the monolithic zirconia because the prostheses are mainly designed using computer software. Further comprehensive clinical studies on diverse edentulous patients are required to validate the effects of this digital technique.
4. Conclusions
Unexpected occlusal changes can be anticipated after treatment with implant-supported prostheses in the posterior area. A digital workflow, involving CAD-CAM interim restorations, intraoral scanning in the newly established vertical dimension, and digital matching technique, can be used to rehabilitate the masticatory system and minimize the possible errors due to changes in occlusion after definitive prosthesis delivery.
Author Contributions
Conceptualization, H.Y.M. and D.-H.L.; methodology, H.Y.M. and D.-H.L.; data curation, H.Y.M., J.-M.S., J.-K.J. and D.-H.L.; formal analysis, H.Y.M. and D.-H.L.; investigation, H.Y.M., J.-M.S., J.-K.J. and D.-H.L.; writing—original draft preparation, H.Y.M.; writing—review and editing, J.-M.S., J.-K.J. and D.-H.L.; supervision, D.-H.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Yamaga, T.; Ogawa, H.; Miyazaki, H. Influence of occlusal deterioration considering prosthetics on subsequent all-cause mortality in a Japanese elderly independent population. Gerodontology 2019, 36, 163–170. [Google Scholar] [CrossRef] [PubMed]
- Park, H.-E.; Song, H.Y.; Han, K.; Cho, K.-H.; Kim, Y.-H. Number of remaining teeth and health-related quality of life: The Korean National Health and Nutrition Examination Survey 2010–2012. Health Qual. Life Outcomes 2019, 17, 5. [Google Scholar] [CrossRef] [PubMed]
- Campos, C.H.; Ribeiro, G.R.; Rodrigues Garcia, R.C.M. Mastication and oral health-related quality of life in removable denture wearers with Alzheimer disease. J. Prosthet. Dent. 2018, 119, 764–768. [Google Scholar] [CrossRef]
- Ruljancich, K. Implantology in oral & maxillofacial surgery. The complexity of ‘simple’ cases. J. Aus. Dent. 2018, 63 (Suppl. S1), S27–S34. [Google Scholar]
- Khoury-Ribas, L.; Ayuso-Montero, R.; Willaert, E.; Peraire, M.; Martinez-Gomis, J. Changes in masticatory laterality 3 months after treatment with unilateral implant-supported fixed partial prosthesis. J. Oral Rehabil. 2020, 47, 78–85. [Google Scholar] [CrossRef]
- Sato, Y.; Kitagawa, N.; Isobe, A. Implant treatment in ultra-aged society. Jpn. Dent. Sci. Rev. 2018, 54, 45–51. [Google Scholar] [CrossRef]
- Nam, D.H.; Lee, D.W.; Chung, C.J.; Kim, K.H.; Park, K.H.; Moon, I.S. Change in masticatory ability with the implant restoration of second molars. J. Prosthet. Dent. 2014, 111, 286–292. [Google Scholar] [CrossRef]
- Box, V.H.; Sukotjo, C.; Knoernschild, K.L.; Campbell, S.D.; Afshari, F.S. Patient-Reported and Clinical Outcomes of Implant-Supported Fixed Complete Dental Prostheses: A Comparison of Metal-Acrylic, Milled Zirconia, and Retrievable Crown Prostheses. J. Oral. Implantol. 2018, 44, 51–61. [Google Scholar] [CrossRef]
- Seol, H.W.; Heo, S.J.; Koak, J.Y.; Kim, S.K.; Kim, S.K. Axial displacement of external and internal implant-abutment connection evaluated by linear mixed model analysis. Int. J. Oral. Maxillofac. Implants. 2015, 30, 1387–1399. [Google Scholar] [CrossRef]
- Ko, K.H.; Huh, Y.H.; Park, C.J.; Cho, L.R. Axial displacement in cement-retained prostheses with different implant-abutment connections. Int. J. Oral Maxillofac. Implants 2019, 34, 1098–1104. [Google Scholar] [CrossRef]
- Curtis, D.; Sharma, A.; Finzen, F.; Kao, R. Occlusal considerations for implant restorations in the partially edentulous patient. J. Calif. Dent. Assoc. 2000, 28, 771–779. [Google Scholar] [PubMed]
- Kim, K.S.; Lim, Y.J. Axial Displacements and Removal Torque Changes of Five Different Implant-Abutment Connections under Static Vertical Loading. Materials 2020, 13, 699. [Google Scholar] [CrossRef] [PubMed]
- Yamazaki, M.; Yugami, K.; Baba, K.; Ohyama, T. Effect of clenching level on mandibular displacement in Kennedy Class II partially edentulous patients. Int. J. Prosthodont. 2003, 16, 183–188. [Google Scholar] [CrossRef]
- Xu, L.; Fan, S.; Cai, B.; Fang, Z.; Jiang, X. Influence of sustained submaximal clenching fatigue test on electromyographic activity and maximum voluntary bite forces in healthy subjects and patients with temporomandibular disorders. J. Oral. Rehabil. 2017, 44, 340–346. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Cai, M.; Yang, J.; Aldhohrah, T.; Wang, Y. Immediate versus early or conventional loading dental implants with fixed prostheses: A systematic review and meta-analysis of randomized controlled clinical trials. J. Prosthet. Dent. 2019, 122, 516–536. [Google Scholar] [CrossRef]
- Yan, C.; Ye, L.; Zhen, J.; Ke, L.; Gang, L. Neuroplasticity of edentulous patients with implant-supported full dentures. Eur. J. Oral. Sci. 2008, 116, 387–393. [Google Scholar] [CrossRef]
- Bakke, M. Mandibular elevator muscles: Physiology, action, and effect of dental occlusion. Scand. J. Dent. Res. 1993, 101, 314–331. [Google Scholar] [CrossRef]
- Katyayan, P.; Katyayan, M.; Patel, G. Association of edentulousness and removable prosthesis rehabilitation with severity of signs and symptoms of temporomandibular disorders. Indian J. Dent. Res. 2016, 27, 127–136. [Google Scholar] [CrossRef]
- Mizrahi, B. Temporary restorations: The key to success. Br. Dent. J. 2019, 226, 761–768. [Google Scholar] [CrossRef]
- Reeponmaha, T.; Angwaravong, O.; Angwarawong, T. Comparison of fracture strength after thermo-mechanical aging between provisional crowns made with CAD/CAM and conventional method. J. Adv. Prosthodont. 2020, 12, 218–224. [Google Scholar] [CrossRef]
- Duret, F.; Blouin, J.L.; Duret, B. CAD-CAM in dentistry. J. Am. Dent. Assoc. 1988, 117, 715–720. [Google Scholar] [CrossRef] [PubMed]
- Mai, H.N.; Lee, K.B.; Lee, D.H. Fit of interim crowns fabricated using photopolymer-jetting 3D printing. J. Prosthet. Dent. 2017, 118, 208–215. [Google Scholar] [CrossRef] [PubMed]
- Papadiochou, S.; Pissiotis, A.L. Marginal adaptation and CAD-CAM technology: A systematic review of restorative material and fabrication techniques. J. Prosthet. Dent. 2018, 119, 545–551. [Google Scholar] [CrossRef]
- Rayyan, M.M.; Aboushelib, M.; Sayed, N.M.; Ibrahim, A.; Jimbo, R. Comparison of interim restorations fabricated by CAD/CAM with those fabricated manually. J. Prosthet. Dent. 2015, 114, 414–419. [Google Scholar] [CrossRef]
- Alp, G.; Murat, S.; Yilmaz, B. Comparison of Flexural Strength of Different CAD/CAM PMMA-Based Polymers. J. Prosthodont. 2019, 28, e491–e495. [Google Scholar] [CrossRef]
- Lee, J.H.; Lee, W.; Huh, Y.H.; Park, C.J.; Cho, L.R. Impact of Intentional Overload on Joint Stability of Internal Implant-Abutment Connection System with Different Diameter. J. Prosthodont. 2019, 28, e649–e656. [Google Scholar] [CrossRef]
- Gilbert, A.B.; Yilmaz, B.; Seidt, J.D.; McGlumphy, E.A.; Clelland, N.L.; Chien, H.H. Three-Dimensional Displacement of Nine Different Abutments for an Implant with an Internal Hexagon Platform. Int. J. Oral. Maxillofac. Implants 2015, 30, 781–788. [Google Scholar] [CrossRef]
- Rebeeah, H.A.; Yilmaz, B.; Seidt, J.D.; McGlumphy, E.; Clelland, N.; Brantley, W. Comparison of 3D displacements of screw-retained zirconia implant crowns into implants with different internal connections with respect to screw tightening. J. Prosthet. Dent. 2018, 119, 132–137. [Google Scholar] [CrossRef]
- Dallaserra, M.; Poblete, F.; Vergara, C.; Cortés, R.; Araya, I.; Yanine, N.; Villanueva, J. Infectious postoperative complications in oral surgery. An observational study. J. Clin. Exp. Dent. 2020, 12, e65–e70. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).