Influence of the Screw Positioning on the Stability of Locking Plate for Proximal Tibial Fractures: A Numerical Approach
Abstract
1. Introduction
- Maintenance of the primary reduction, as the implant blocks the bone segments in their respective positions regardless of the reduction degree;
- Stability under load which entails a lower risk of a secondary loss of the intraoperative reduction;
- Greater blood supply to the cortical bone.
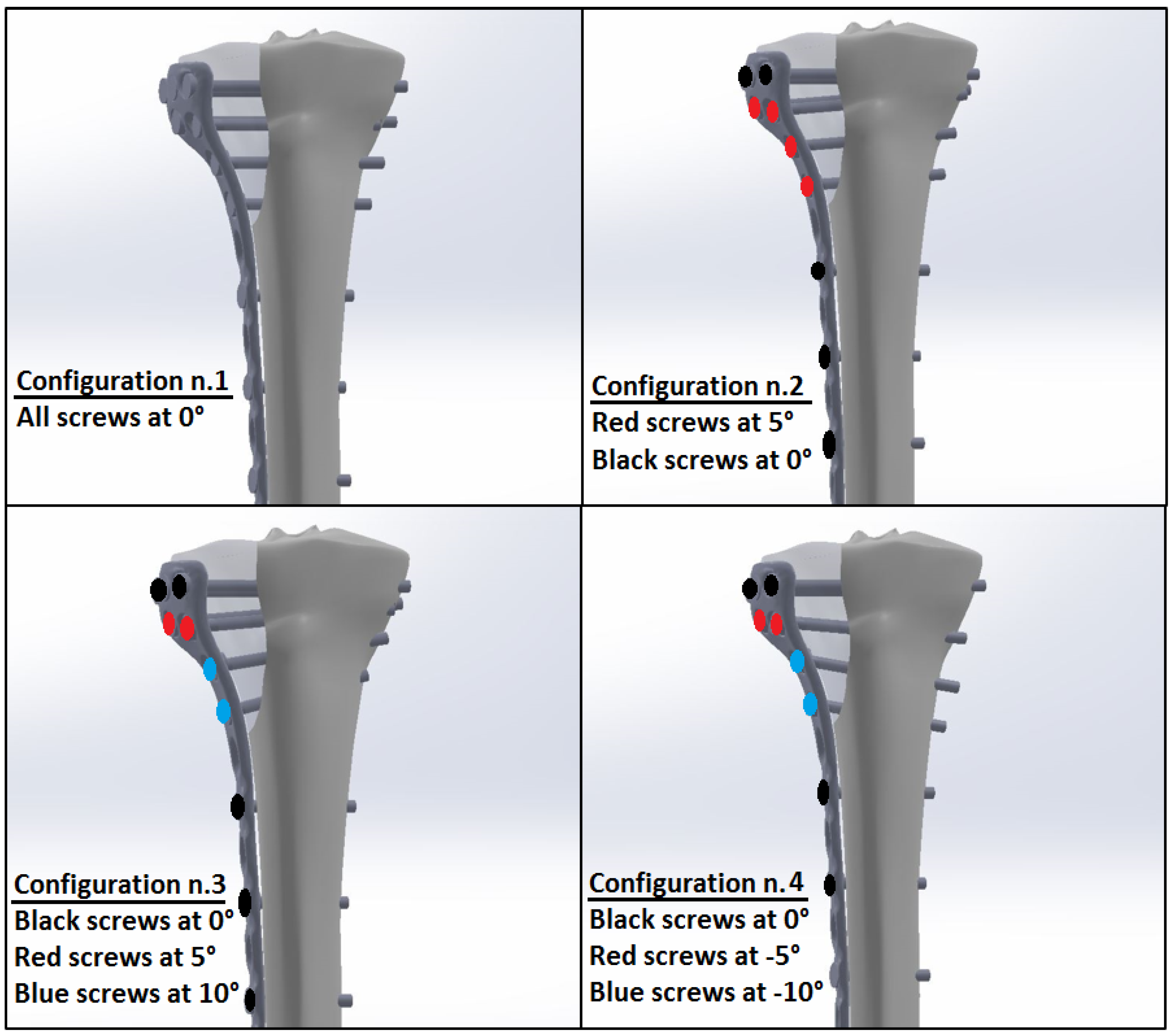
2. Materials and Methods
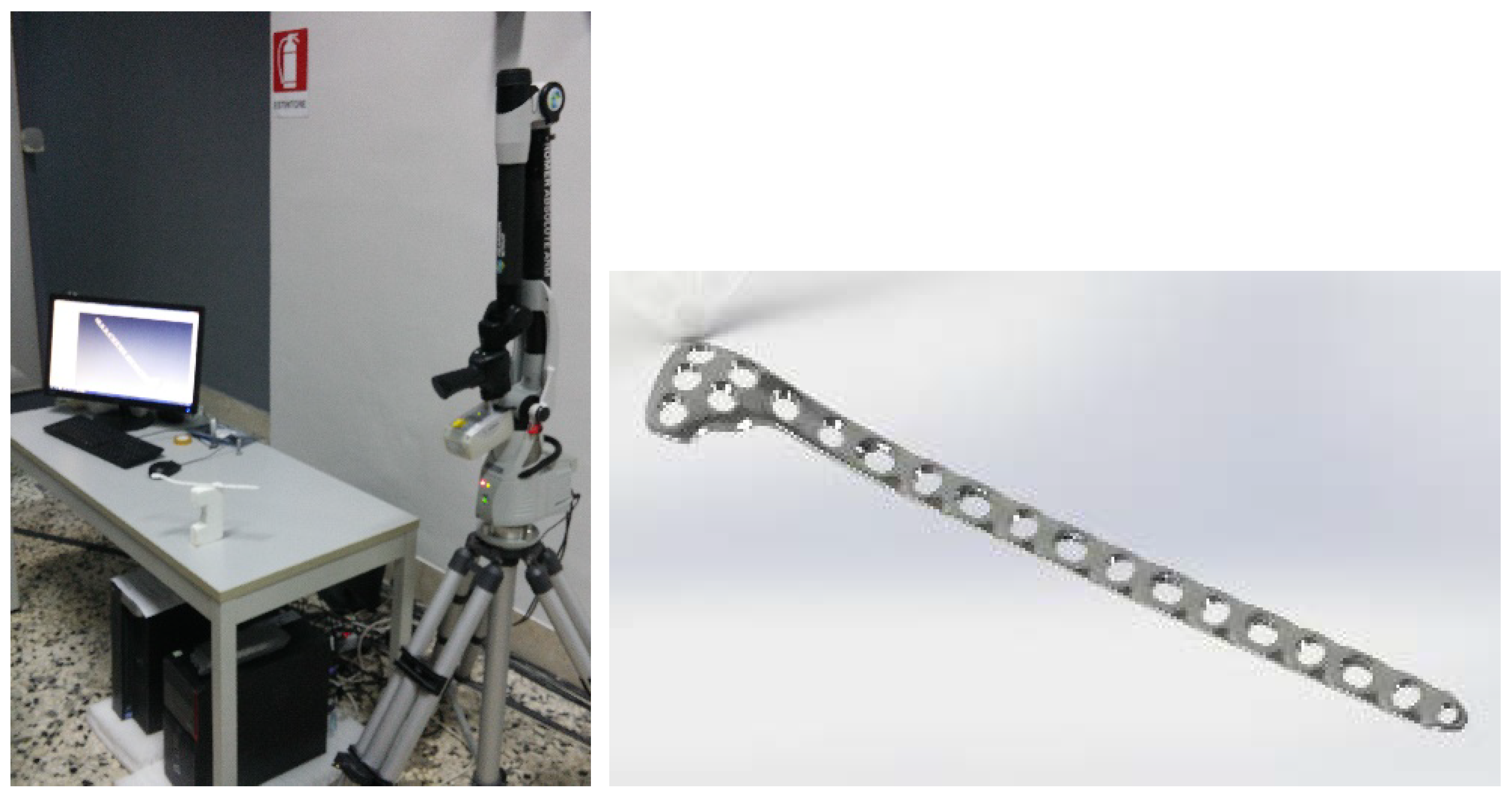
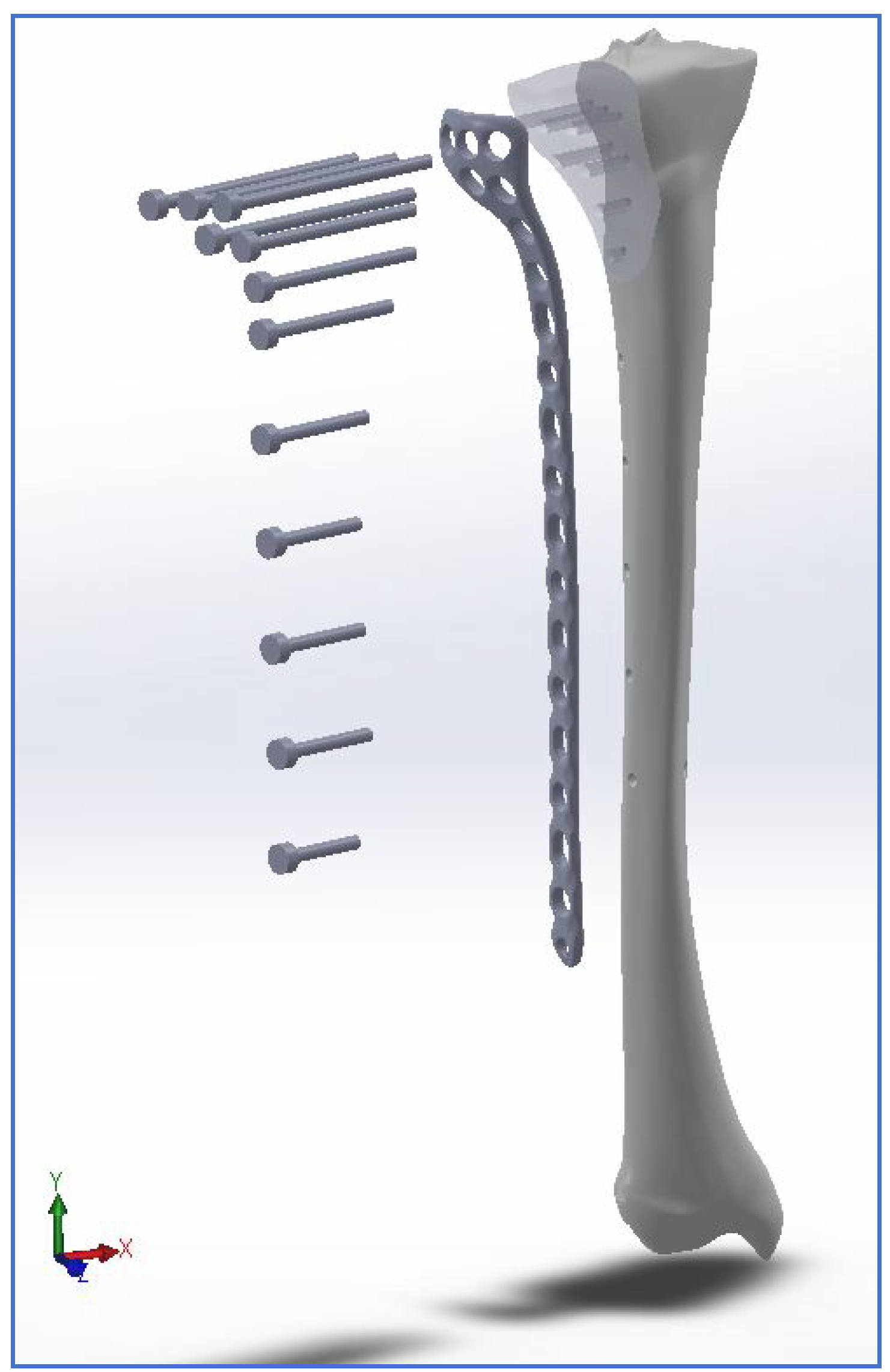
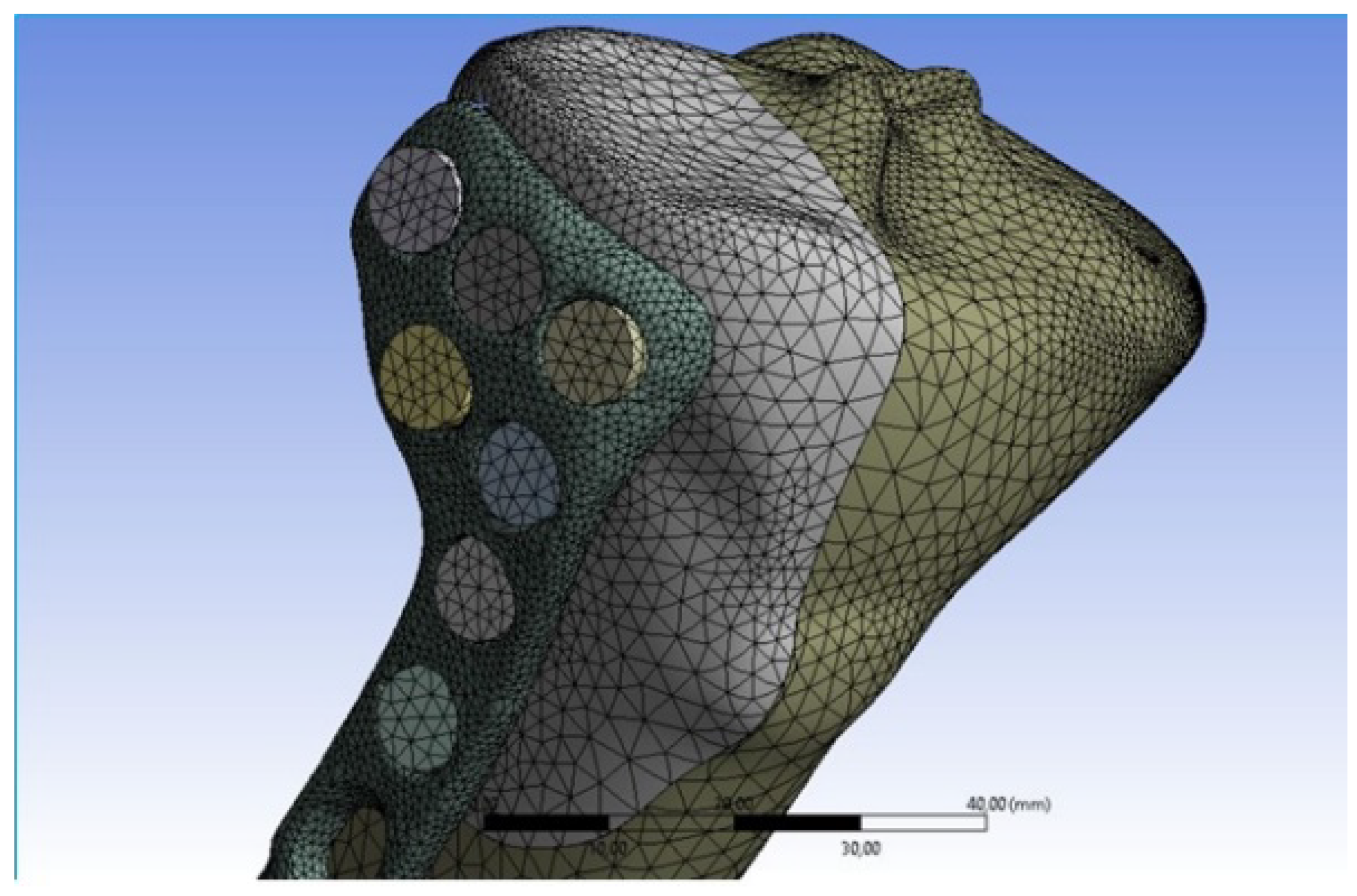
2.1. 3D Acquisition and CAD Modelling
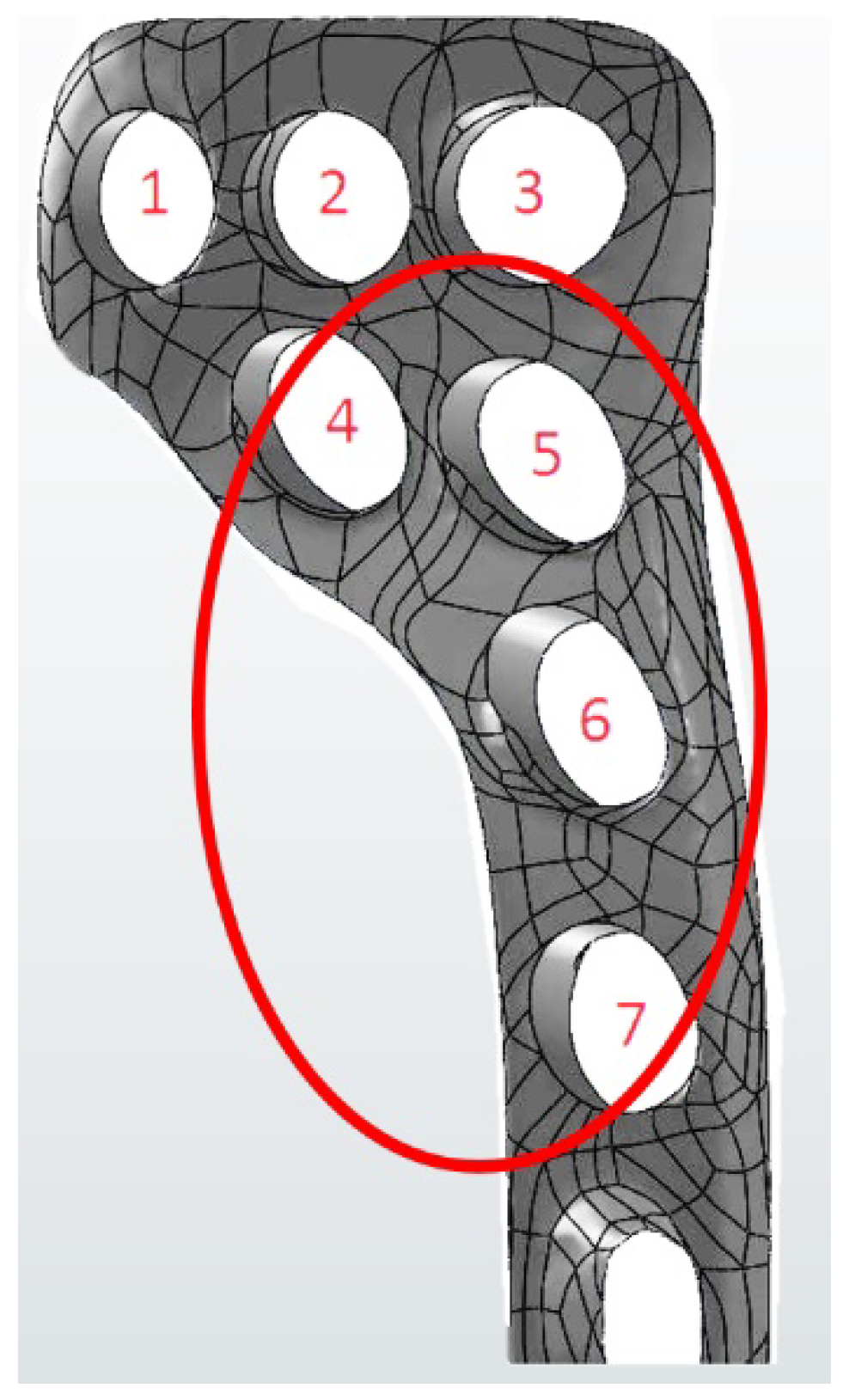
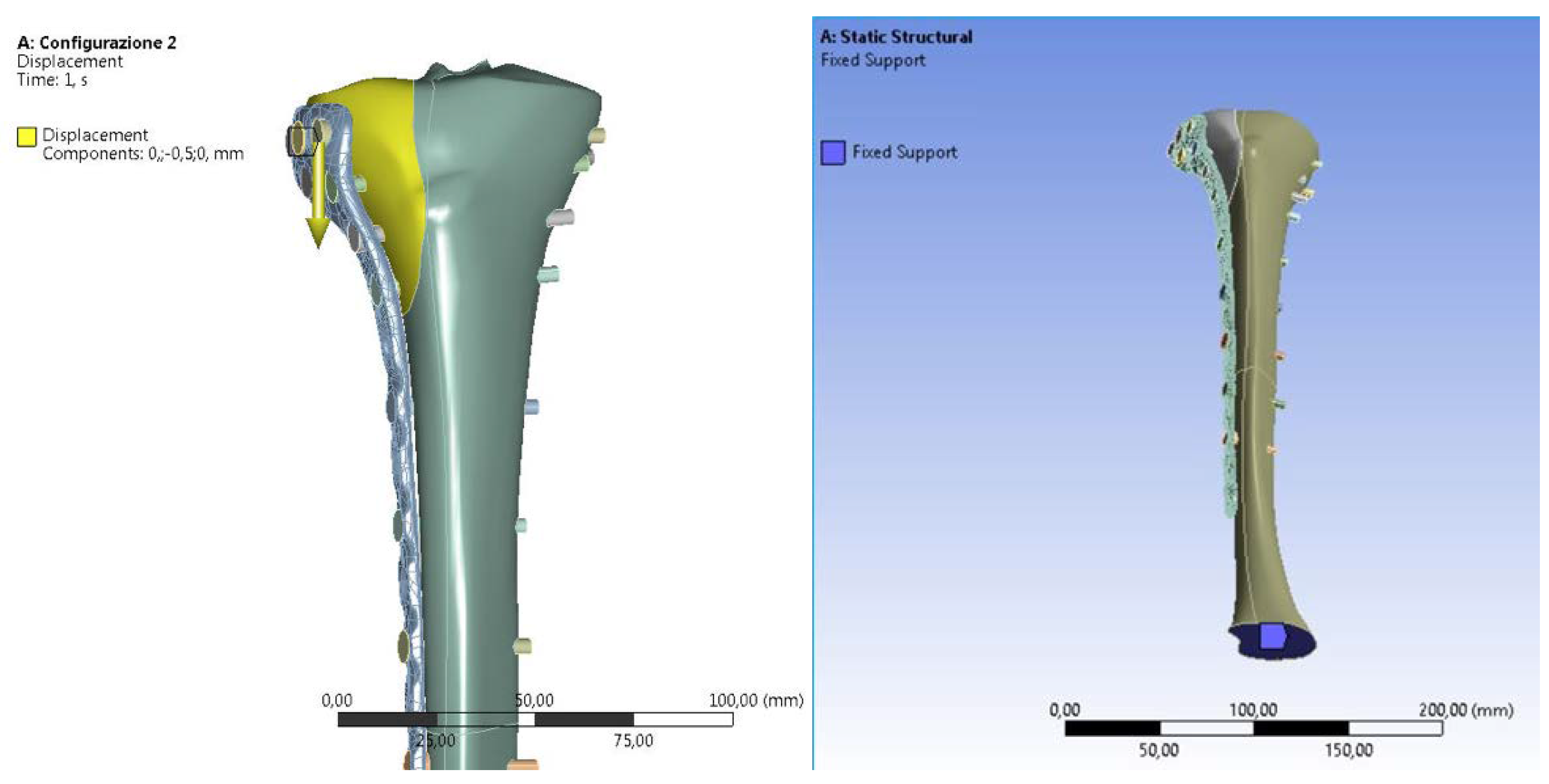
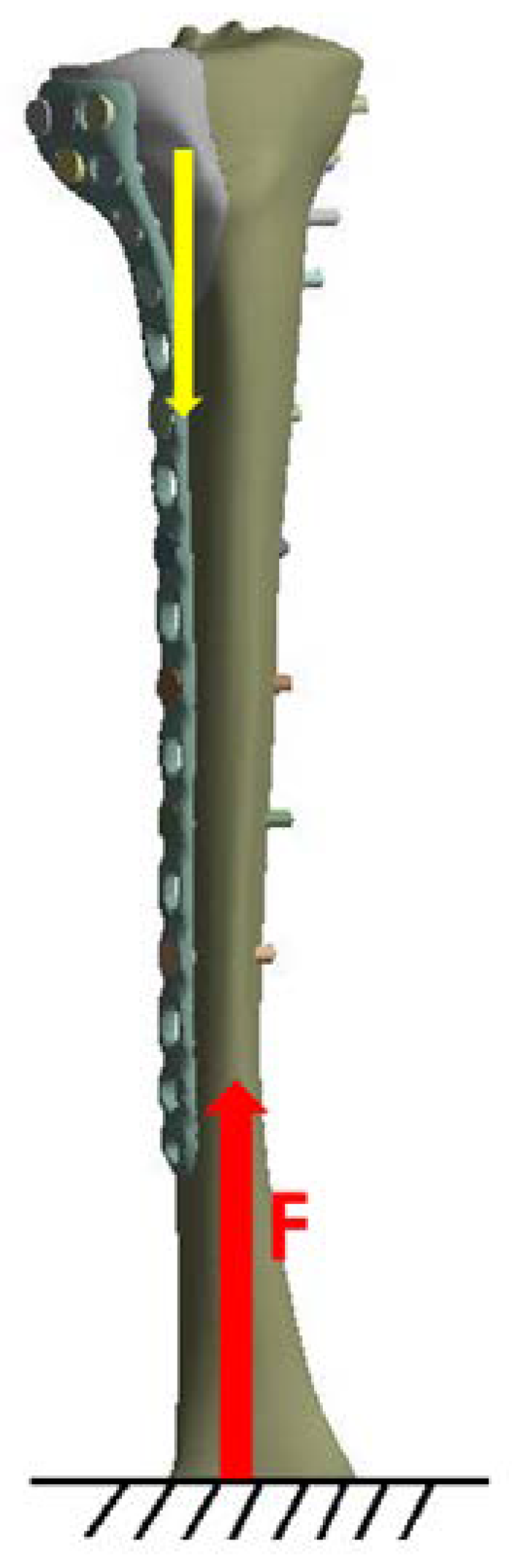
2.2. FEM Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Schatzker, J.; Tile, M. The Rationale of Operative Fracture Care, 3rd ed.; Springer: Heidelberg, Germany, 2005; Chapter 19; pp. 447–469. [Google Scholar]
- Burdin, G. Arthroscopic management of tibial plateau fractures: Surgical technique. Orthop. Traumatol. Surg. Res. 2013, 99, 208–218. [Google Scholar] [CrossRef] [PubMed]
- Märdian, S.; Landmann, F.; Wichlas, F.; Haas, N.P.; Schaser, K.-D.; Schwabe, P. Outcome of angular stable locking plate fixation of tibial plateau fractures Midterm results in 101 patients. Indian. J. Orthop. 2015, 49, 620–629. [Google Scholar] [CrossRef]
- Chen, F.; Huang, X.; Ya, Y.; Ma, F.; Qian, Z.; Shi, J.; Guo, S.; Yu, B. Finite element analysis of intramedullary nailing and double locking plate for treating extra-articular proximal tibial fractures. J. Orthop. Surg. Res. 2018, 13, 12. [Google Scholar] [CrossRef] [PubMed]
- Chen, F.; Zhao, Z.; Liu, J.; Cui, X.; Zhang, D.; Su, X.; Zhao, J.; Tang, P.; Liao, H. Automatic estimation of morphological characteristics of proximal tibia for precise plate treatment using model matching. Comput. Med. Imaging Graph. 2020, 81, 101714. [Google Scholar] [CrossRef] [PubMed]
- Ingrassia, T.; Mancuso, A. Virtual prototyping of a new intramedullary nail for tibial fractures. Int. J. Interact. Des. Manuf. 2013, 7, 159–169. [Google Scholar] [CrossRef][Green Version]
- Hasenboehler, E.; Rikli, D.; Babst, R. Locking compression plate with minimally invasive plate osteosynthesis in diaphyseal and distal tibial fracture: A retrospective study of 32 patients. Inj. Int. J. Care Inj. 2007, 38, 365–370. [Google Scholar] [CrossRef] [PubMed]
- Chen, P.; Lu, H.; Shen, H.; Wang, W.; Ni, B.; Chen, J. Newly designed anterolateral and posterolateral locking anatomic plates for lateral tibial plateau fractures: A finite element study. J. Orthop. Surg. Res. 2017, 12, 35. [Google Scholar] [CrossRef]
- Ma, C.H.; Wu, C.H.; Tu, Y.K.; Lin, T.S. Metaphyseal locking plate as a definitive external fixator for treating open tibial fractures—Clinical outcome and a finite element study. Inj. Int. J. Care Inj. 2013, 44, 1097–1101. [Google Scholar] [CrossRef]
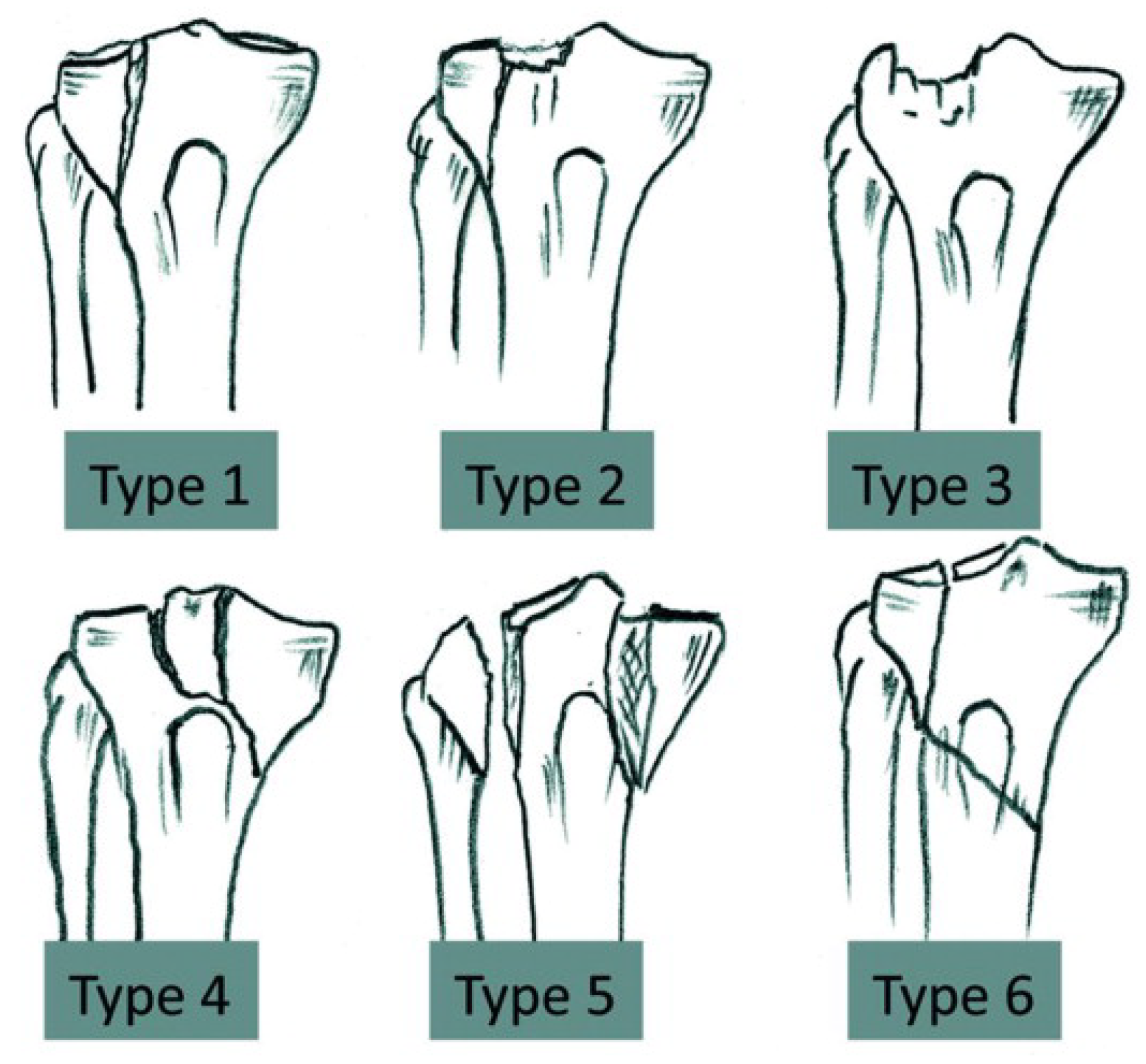
- Kfuri Júnior, M.; Fogagnolo, F.; Carneiro Bitar, R.; Lara Freitas, R.; Salim, R.; Jansen Paccola, C.A. Tibial Plateau Fractures. Rev. Bras. Orthop. 2009, 44, 468–474. [Google Scholar] [CrossRef]
- Kfuri, M.; Schatzker, J. Revisiting the Schatzker classification of tibial plateau fractures. Inj. Int. J. Care Inj. 2018, 49, 2252–2263. [Google Scholar] [CrossRef]
- Biggi, F.; Di Fabio, S.; D’Antimo, C.; Trevisani, S. Tibial plateau fractures: Internal fixation with locking plates and the MIPO technique. Inj. Int. J. Care Inj. 2010, 41, 1178–1182. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://gha.health/produkt/loqteq-proximal-lateral-tibia-plate-3-5-4-5/ (accessed on 22 June 2020).
- Egol, K.A.; Kubiak, E.N.; Fulkerson, E.; Kummer, F.J.; Koval, K.J. Biomechanics of Locked Plates and Screws. J. Orthop. Trauma. 2004, 18, 488–493. [Google Scholar] [CrossRef]
- Cordey, J.; Borgeaud, M.; Perren, S.M. Force Transfer between the Plate and the Bone: Relative Importance of the Bending Stiffness of the Screws Friction Between Plate and Bone. Inj. Int. J. Care Inj. 2000, 3, C21–C28. [Google Scholar] [CrossRef]
- Cronier, P.; Pietu, G.; Dujardin, C.; Bigorre, N.; Ducellier, F.; Gerard, R. The concept of locking plates. Orthop. Traumatol. Surg. Res. 2010, 96, S17–S36. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Chang, C.; Li, C.; Chen, C.; Chung, C.; Chang, C.; Peng, Y. Biomechanical investigation of the type and configuration of screws used in high tibial osteotomy with titanium locking plate and screw fixation. J. Orthop. Surg. Res. 2019, 14, 35. [Google Scholar] [CrossRef]
- Ren, D.; Liu, Y.; Lu, J.; Xu, R.; Wang, P. A Novel Design of a Plate for Posterolateral Tibial Plateau Fractures through Traditional Anterolateral Approach. Sci. Rep. 2018, 8, 16418. [Google Scholar] [CrossRef] [PubMed]
- Jacquet, C.; Marret, A.; Myon, R.; Ehlinger, M.; Bahlouli, N.; Wilson, A.; Kley, K.; Rossi, J.-M.; Parratte, S.; Ollivier, M. Adding a protective screw improves hinge′s axial and torsional stability in High Tibial Osteotomy. Clin. Biomech. 2020, 74, 96–102. [Google Scholar] [CrossRef] [PubMed]
- Chieh-Szu Yang, J.; Chen, C.-F.; Lee, O.K. Benefits of opposite screw insertion technique in medial open-wedge high tibial osteotomy: A virtual biomechanical study. J. Orthop. Transl. 2020, 20, 31–36. [Google Scholar] [CrossRef]
- Ghimire, S.; Miramini, S.; Richardson, M.; Mendis, P.; Zhang, L. Effects of dynamic loading on fracture healing under different locking compression plate configurations: A finite element study. J. Mech. Behav. Biomed. Mater. 2019, 94, 74–85. [Google Scholar] [CrossRef]
- Chang, C.; Chen, Y.; Li, C.; Chung, C.; Tseng, C.; Chang, C.; Peng, T. Biomechanical investigation of tibial tubercle osteotomy fixed with various screw configurations. Inj. Int. J. Care Inj. 2019, 50, 263–271. [Google Scholar] [CrossRef]
- Ingrassia, T.; Nalbone, L.; Nigrelli, V.; Pisciotta, D.; Ricotta, V. Influence of the Metaphysis Positioning in a New Reverse Shoulder Prosthesis; AG Advances on Mechanics, Design Engineering and Manufacturing, Lecture Notes in Mechanical Engineering; Springer International Publishing: Cham, Switzerland, 2017; pp. 469–478. [Google Scholar]
- Ingrassia, T.; Nigrelli, V.; Ricotta, V.; Nalbone, L.; D’Arienzo, A.; D’Arienzo, M.; Porcellini, G. A new method to evaluate the influence of the glenosphere positioning on stability and range of motion of a reverse shoulder prosthesis. Inj. Int. J. Care Inj. 2019, 50, S12–S17. [Google Scholar] [CrossRef] [PubMed]
- Ingrassia, T.; Nalbone, L.; Nigrelli, V.; Ricotta, V.; Pisciotta, D. Biomechanical analysis of the humeral tray positioning in reverse shoulder arthroplasty design. Int. J. Interact. Des. Manuf. 2018, 12, 651–661. [Google Scholar] [CrossRef]
- Inzana, J.A.; Varga, P.; Windolf, M. Implicit modeling of screw threads for efficient finite element analysis of complex bone-implant systems. J. Biomech 2016, 49, 1836–1844. [Google Scholar] [CrossRef] [PubMed]
- Carrera, I.; Gelber, P.E.; Chary, G.; Gonzalez-Ballester, M.A.; Monllau, J.C.; Noailly, J. Fixation of a split fracture of the lateral tibial plateau with a locking screw plate instead of cannulated screws would allow early weight bearing: A computational exploration. Int. Orthop. 2016, 40, 2163–2169. [Google Scholar] [CrossRef]
- Anderson, D.D.; Thomas, T.P.; Marin, A.C.; Elkins, J.M.; Lack, W.D.; Lacroix, D. Computational Techniques for the Assessment of Fracture Repair. Inj. Int. J. Care Inj. 2014, 45, S23–S31. [Google Scholar] [CrossRef]
- Byrne, D.P.; Lacroix, D.; Prendergast, P.J. Simulation of Fracture Healing in the Tibia: Mechanoregulation of Cell Activity Using a Lattice Modeling Approach. J. Orthop. Res. 2011, 29, 1496–1503. [Google Scholar] [CrossRef]
- Tumino, D.; Ingrassia, T.; Nigrelli, V.; Pitarresi, G.; Urso Miano, V. Mechanical behavior of a sandwich with corrugated GRP core: Numerical modeling and experimental validation. Frat. ed Integrità Strutt. 2014, 30, 317–326. [Google Scholar] [CrossRef]
- Mirulla, A.I.; Bragonzoni, L.; Zaffagnini, S.; Bontempi, M.; Nigrelli, V.; Ingrassia, T. Virtual simulation of an osseointegrated trans-humeral prosthesis: A falling scenario. Inj. Int. J. Care Inj. 2018, 49, 784–791. [Google Scholar] [CrossRef]
- Perez, A.; Mahar, A.; Negus, C.; Newton, P.; Impelluso, T. A computational evaluation of the effect of intramedullary nail material properties on the stabilization of simulated femoral shaft fractures. Med. Eng. Phys. 2008, 30, 755–760. [Google Scholar] [CrossRef]
- Cerniglia, D.; Ingrassia, T.; D’Acquisto, L.; Saporito, M.; Tumino, D. Contact between the components of a knee prosthesis: Numerical and experimental study. Fract. Struct. Integr. 2012, 22, 56–68. [Google Scholar] [CrossRef]
- Anwar, A.; Lv, D.; Zhao, Z.; Zhang, Z.; Lu, M.; Nazir, M.U.; Qasim, W. Finite element analysis of the three different posterior malleolus fixation strategies in relation to different fracture sizes. Inj. Int. J. Care Inj. 2017, 48, 825–832. [Google Scholar] [CrossRef] [PubMed]
- Knežević, J.; Kodvanj, J.; Čukelj, F.; Pamuković, F.; Pavić, A. A biomechanical comparison of four fixed-angle dorsal plates in a finite element model of dorsally-unstable radius fracture. Inj. Int. J. Care Inj. 2017, 48, S41–S46. [Google Scholar] [CrossRef]
- Simo, J.C.; Laursen, T.A. An Augmented Lagrangian Treatment of Contact Problems Involving Friction. Comput. Struct. 1992, 42, 97–116. [Google Scholar] [CrossRef]
- Ji, W.; Luo, C.; Zhan, S.; Zhan, Y.; Xie, X.; Zhang, B. Combined proximal tibial osteotomy for varus osteoarthritis of the knee: Biomechanical tests and finite-element analyses. Knee 2020, 27, 863–870. [Google Scholar] [CrossRef] [PubMed]
- Götz, R.; Gebhard, F.; Duerselen, L.; Ignatius, A.; Claes, L. Delayed bone healing following high tibial osteotomy related to increased implant stiffness in locked plating. Inj. Int. J. Care Inj. 2014, 45, 1648–1652. [Google Scholar]
- Luo, C.-A.; Hwa, S.-Y.; Lin, S.-C.; Chen, C.-M.; Tseng, C.-S. Placement-induced effects on high tibial osteotomized construct—Biomechanical tests and finite-element analyses. BMC Musculoskelet. Disord. 2015, 16, 1–10. [Google Scholar] [CrossRef]
- Kandemir, U.; Herfat, S.; Herzog, M.; Viscogliosi, P.; Pekmezci, M. Fatigue failure in extra-articular proximal tibia fractures: Locking Intramedullary nail versus double locking plates—A biomechanical study. J. Orthop. Trauma. 2017, 31, 49–54. [Google Scholar] [CrossRef]
- Huang, X.; Zhi, Z.; Yu, B.; Chen, F. Stress and stability of plate-screw fixation and screw fixation in the treatment of Schatzker type IV medial tibial plateau fracture: A comparative finite element study. J. Orthop. Surg. Res. 2015, 10, 182. [Google Scholar] [CrossRef]
- Prat-Fabregat, S.; Camacho-Carrasco, P. Treatment strategy for tibial plateau fractures: An update. EFORT Open Rev. 2016, 1, 225–232. [Google Scholar] [CrossRef]
- Ingrassia, T.; Lombardo, B.; Nigrelli, V.; Ricotta, V.; Nalbone, L.; D’Arienzo, A.; D’Arienzo, M.; Porcellini, G. Influence of sutures configuration on the strength of tendon-patch joints for rotator cuff tears treatment. Inj. Int. J. Care Inj. 2019, 50, S18–S23. [Google Scholar] [CrossRef]
- Feng, W.; Fu, L.; Liu, J.; Qi, X.; Li, D.; Yang, C. Biomechanical evaluation of various fixation methods for proximal extra-articular tibial fractures. J. Surg. Res. 2012, 178, 722–727. [Google Scholar] [CrossRef] [PubMed]
- Farouk, O.; Krettek, C.; Miclau, T.; Schandelmaier, P.; Guy, P.; Tscherne, H. Minimally invasive plate osteosynthesis: Does percutaneous plating disrupt femoral blood supply less than the traditional technique? J. Orthop. Trauma. 1999, 13, 401–406. [Google Scholar] [CrossRef] [PubMed]
- Hu, X.J.; Wang, H. Biomechanical assessment and 3D finite element analysis of the treatment of tibial fractures using minimally invasive percutaneous plates. Exp. Ther. Med. 2017, 14, 1692–1698. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sun, H.; He, Q.; Zhang, B.; Zhu, Y.; Zhang, W.; Chai, Y. A biomechanical evaluation of different fixation strategies for posterolateral fragments in tibial plateau fractures and introduction of the ‘magic screw’. Knee 2018, 25, 417–426. [Google Scholar] [CrossRef]
- MacLeod, A.R.; Serrancoli, G.; Fregly, B.J.; Toms, A.D.; Gill, H.S. The effect of plate design, bridging span, and fracture healing on the performance of high tibial osteotomy plates: An experimental and finite element study. Bone Jt. Res. 2019, 7, 639–649. [Google Scholar] [CrossRef]
- Kaze, A.D.; Maas, S.; Waldmann, D.; Zilian, A.; Dueck, K.; Pape, D. Biomechanical properties of five different currently used implants for open-wedge high tibial osteotomy. J. Exp. Orthop. 2015, 2, 14. [Google Scholar] [CrossRef]



| E1 (GPa) | E2 (GPa) | E3 (GPa) | G12 (GPa) | G13 (GPa) | G23 (GPa) | n12 | n13 | n23 |
|---|---|---|---|---|---|---|---|---|
| 6.91 | 8.51 | 18.4 | 2.41 | 3.56 | 4.91 | 0.49 | 0.12 | 0.14 |
| Material | E (GPa) | n |
|---|---|---|
| Ti6Al4V | 115 | 0.33 |
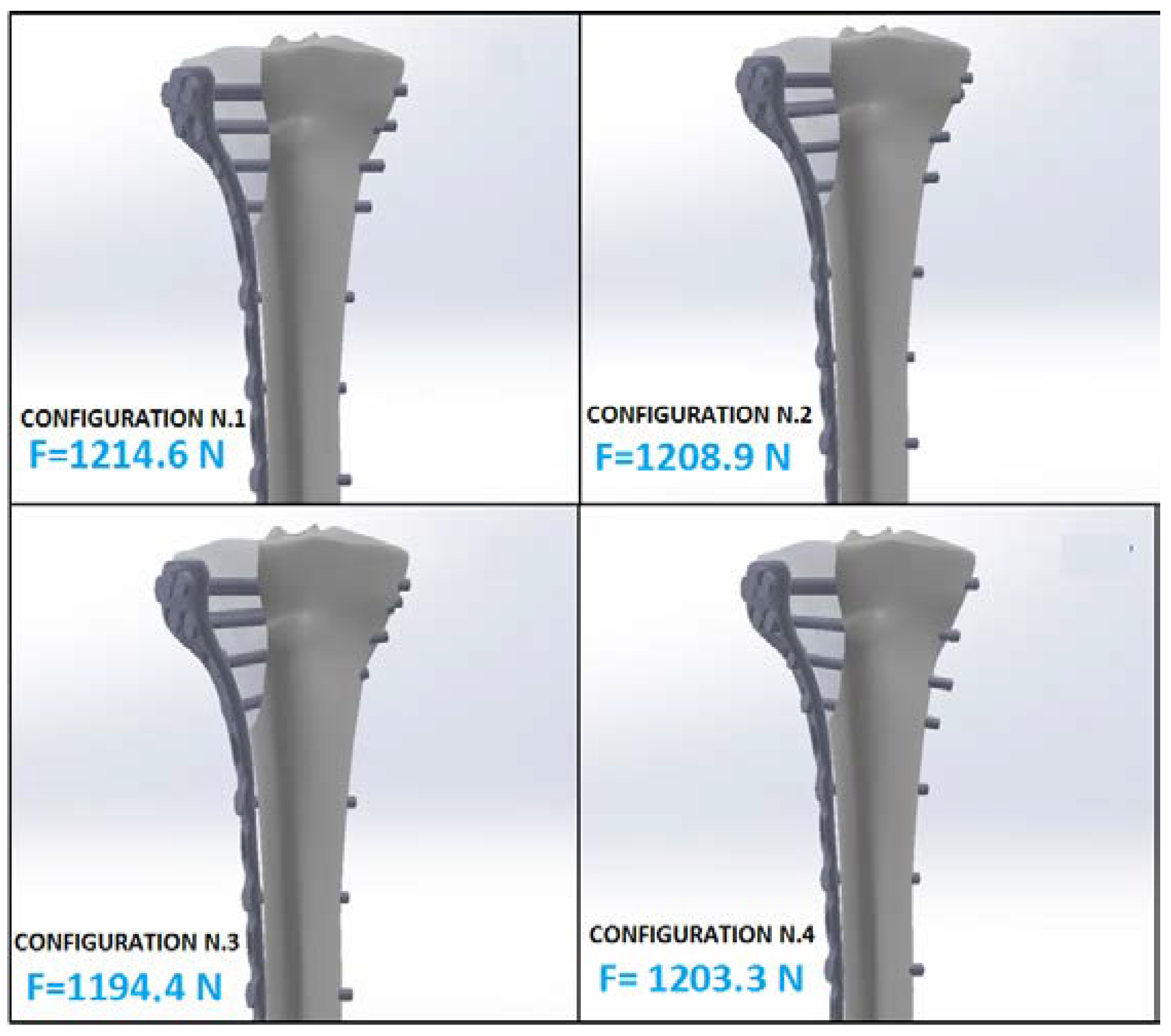
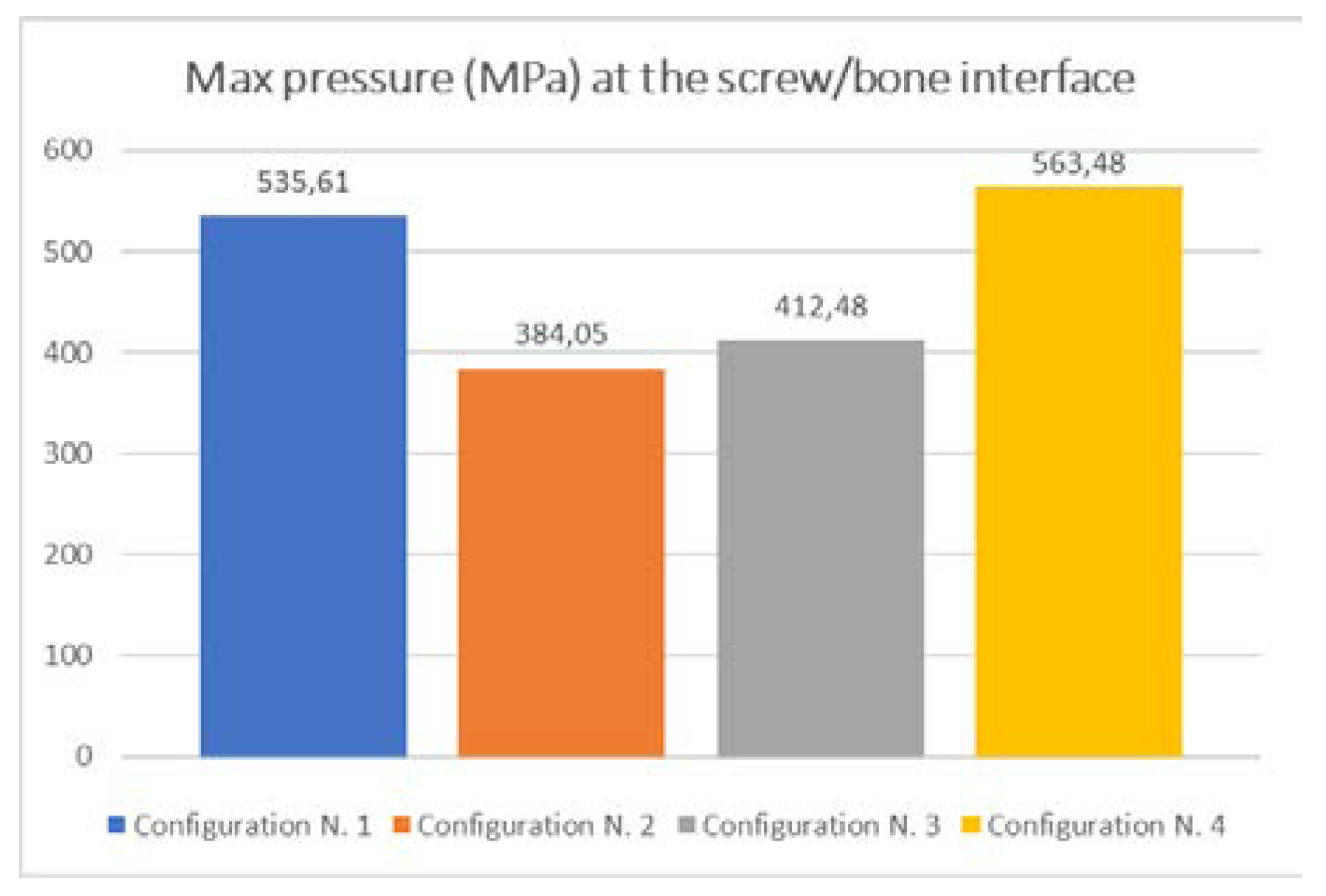
| Configuration Number | Reaction Force F (N) | Pressure Max pmax (MPa) |
|---|---|---|
| 1 | 1214.6 | 535.61 |
| 2 | 1208.9 | 384.05 |
| 3 | 1194.4 | 412.48 |
| 4 | 1203.3 | 563.48 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ingrassia, T.; Nigrelli, V.; Pecorella, D.; Bragonzoni, L.; Ricotta, V. Influence of the Screw Positioning on the Stability of Locking Plate for Proximal Tibial Fractures: A Numerical Approach. Appl. Sci. 2020, 10, 4941. https://doi.org/10.3390/app10144941
Ingrassia T, Nigrelli V, Pecorella D, Bragonzoni L, Ricotta V. Influence of the Screw Positioning on the Stability of Locking Plate for Proximal Tibial Fractures: A Numerical Approach. Applied Sciences. 2020; 10(14):4941. https://doi.org/10.3390/app10144941
Chicago/Turabian StyleIngrassia, Tommaso, Vincenzo Nigrelli, Daniele Pecorella, Laura Bragonzoni, and Vito Ricotta. 2020. "Influence of the Screw Positioning on the Stability of Locking Plate for Proximal Tibial Fractures: A Numerical Approach" Applied Sciences 10, no. 14: 4941. https://doi.org/10.3390/app10144941
APA StyleIngrassia, T., Nigrelli, V., Pecorella, D., Bragonzoni, L., & Ricotta, V. (2020). Influence of the Screw Positioning on the Stability of Locking Plate for Proximal Tibial Fractures: A Numerical Approach. Applied Sciences, 10(14), 4941. https://doi.org/10.3390/app10144941






