Featured Application
The influence of brushing motion on root canal anatomy preservation after shaping with NiTi single file reciprocating instruments was evaluated. The brushing movement may accentuate canal transportation especially in the coronal third.
Abstract
Brushing motion has been proposed for endodontic single-file reciprocating systems to eliminate coronal interferences, but it may hesitate in a less conservative root canal shaping. The aim of the study was to compare the maintenance of the original root canal anatomy using the WaveOne Gold (WOG) technique with or without a brushing motion. Sixty extracted human mandibular first molars were selected. Manual canal scouting and mechanical glide path were performed. Samples were randomized into two groups (n = 30): WOG Primary was used to shape the mesio-lingual canals without (NB group) or with (B group) an intentional brushing motion. Specimens were scanned with micro-computed tomography (micro-CT) before and after instrumentation in order to match the volumes. Increases in canal volume and surface area were measured. Centroid shift and thickness of removed dentine from the inner curvature were assessed at the furcation, 1.5 mm and 3 mm apically from the furcation, and in relation to the point of maximum curvature. Data were analyzed by one-way ANOVA and post-hoc Student–Newmann–Keuls tests (p < 0.05). No brushing technique resulted in being significantly associated with a better maintenance of the canal anatomy, especially in the coronal third (p < 0.05). When using the WOG system, a no-brushing technique resulted in less invasive shaping, reducing the risk of stripping.
1. Introduction
Root canal shaping is essential to achieve optimal results in the subsequent cleaning and filling procedures [1,2]. This process aims to create an adequate space for irrigation while preserving the original anatomy [3].
Maintaining the original canal shape through the use of a minimally invasive technique is associated with better endodontic outcomes [1,4,5]. Nickel–titanium (NiTi) rotary systems have been shown to reduce shaping time, operator fatigue, and root canal transportation [6,7]. A reciprocating single instrument approach has been introduced to simplify root canal shaping [8,9,10]. This technique uses only one file after the initial canal scouting and glide path to create a continuous tapered preparation [11,12]. The reciprocating movement limits the torsional stress placed on the shank of the single file during shaping, reducing the risk of instrument fracture [9,10,13,14]. Recently, the WaveOne Gold (WOG) reciprocating system has been introduced. The evolved parallelogram cross section and the Gold-Wire technology are claimed to optimize root canal centering ability and fracture resistance [15,16]. This WOG directions of use suggest utilizing a brushing motion on the outstroke to eliminate coronal interferences and to enhance shaping results [17].
Therefore, brushing motion is widely suggested to remove restrictive coronal dentine using a painting movement towards the outside of the canal curvature. It was clinically adopted for multi-file shaping systems to improve the efficiency of the finishing files after deleting coronal constriction, especially for mesial canals of mandibular molars [18]. However, brushing motion was also proposed for single-file reciprocating systems to eliminate coronal interferences before filling with a warm gutta-percha technique, or to improve shaping outcomes in canals that exhibit irregular cross-sections [19]. There is currently insufficient information regarding the shaping ability and the maintenance of the original canal anatomy of reciprocating single-file instruments when used in a brushing motion.
Micro-computed tomography (micro-CT) has emerged as a powerful device for the in vitro evaluation of root canal shaping outcomes. It enables the analysis of volume changes, cross-sectional shape, taper, and proportion of prepared surface by matching reconstructed sample volumes of pre-operative and post-operative canal systems [20,21].
The aim of this study was to evaluate the ability of reciprocating WaveOne Gold single files to maintain the original root canal anatomy when used with or without an intentional brushing motion. The correct clinical use of the reciprocating instrumentation could improve the maintenance of the sound tooth structure, reducing the risk of root canal transportation and positively influencing the long-term prognosis of the endodontic treatments. The null hypothesis is that both instrumentation techniques will equally maintain the original root canal anatomy.
2. Materials and Methods
Mandibular first permanent molars with a fully formed apex and extracted for periodontal disease were considered. The patients signed an informed consent for the treatment and for the use of the extracted tooth for research purposes, and the local scientific committee authorized the in-vitro study. Only teeth free of caries, cracks, and artificial alterations were included in the study. After root surface debridement to remove periodontal debris, plaque, and calculus, specimens were dipped in a 0.01% NaOCl solution at 4 °C and then, after 24 h, were stored in saline solution at the same temperature. A sample size of 30 molars per group was calculated with G*Power 3.1.4 (Kiel University, Kiel, Germany) to set the study power at 80%. A custom-made support was created in order to scan the specimens. Low-resolution preliminary micro-CT scans were performed to ensure that inclusion criteria were met (SkyScan 1172, Bruker micro-CT, Kontich, Belgium). Preliminary scans were conducted with the following parameters: a total of 450 projections throughout a 225° rotation (180° plus cone angle of the X-ray source) using a 1.0 mm-thick aluminum filter, voltage = 100 kV, current = 80 μA, source-to-object distance = 80 mm, source-to-detector distance = 220 mm, pixel binning = 8 × 8, and exposure time/projection = 0.2s. Morphological parameters of the mesial canals were obtained. Mesio-lingual separated canals, 12 ± 2 mm in length from canal orifice to apical foramen, with moderate curvature (10°–30°), and 2 < r ≤ 6 curvature radius were selected to ensure sample homogeneity.
Out of 72 teeth assessed for inclusion, 12 teeth not meeting the inclusion criteria or with prominent intracanal isthmus or significant calcifications were excluded. Sixty samples were randomly assigned to two groups by a blinded operator through random number tables: WaveOne Gold Primary with no brushing technique (NB group) (n = 30) and WaveOne Gold Primary with brushing technique (B group) (n = 30).
A blinded operator performed randomization, allocation, and statistical analysis, and a single expert operator with over ten years of experience in endodontics and blinded to the objectives of the study prepared the samples. After access cavity preparation, canal scouting was performed with #10 K-file at working length (WL) using Glyde (Dentsply Sirona) as a lubricating agent (0.80 mg). WL was determined under 10X magnification (OPMI Pro Ergo, Carl Zeiss) by subtracting 0.5 mm from the length at which the tip was visible at the apical foramen. In both groups, glide path was performed with a Proglider single file (size 0.16, taper 0.02 to 0.085) (Dentsply Sirona) using an X-Smart Plus motor (Dentsply Sirona) (300 rpm, 4 Ncm) at WL.
In the NB group, root canal shaping was performed with a WaveOne Gold Primary single file (size 0.25, taper 0.07) (Dentsply Sirona) using X-Smart Plus (reciprocating movement settings as suggested by the manufacturer) at WL with an in-and-out motion and no intentional brushing effect. In the B group, root canal shaping was performed with a WaveOne Gold Primary single file (size 0.25, 0.07) using X-Smart Plus (reciprocating movement settings as suggested by the manufacturer) at WL with a brushing motion consisting of four strokes towards the root canal wall opposite to the furcation. Instruments were removed from the canal and cleaned after three pecking motions until WL was reached. Slow in-and-out pecking motions (amplitude less than 3 mm) were used in both groups, and new instruments were employed for each specimen.
Irrigation was performed with a 30-gauge needle syringe alternating 5% NaOCl with 10% EDTA during instrumentation for a total of 6 mL of NaOCl and 4 mL of EDTA for each specimen.
The selected samples were scanned at a higher spatial resolution before and after root canal preparation (SkyScan, Bruker-microCT). The microCT scanning parameters were 100 kV, 100 μA, 16 μm resolution, Au filter and 360° rotation, for a total of 2400 projections. The images were reconstructed with NRecon (Bruker-microCT) using standard parameters for beam hardening (60%) and ring artefact correction (7%). Each root canal path was analyzed with high-resolution three-dimensional (3D) rendering and orthogonal bidimensional (2D) cross sections. Reconstructed volumes were analyzed with CTAn (Bruker-microCT), and the measurements were performed. The increase in canal volume and surface area were calculated for each group through the superimposition of the pre- and post-operative scanned volumes. The centroid shift and the amount of removed dentine up to the furcation in the middle and coronal third of the canals were measured using ImageJ 1.43u 64-bit software (National Institute of Health, Bethesda). A minimum threshold algorithm was set to avoid manual errors [22]. Root sections orthogonal to the canal axis were set at 4 different levels: at the furcation (F), 1.5 mm apically from the furcation (1.5F), 3 mm apically from the furcation (3F), and in correspondence to the point of maximum curvature (M).
Results were analyzed by one-way ANOVA and post-hoc Student–Newmann–Keuls test (p < 0.05) using SPSS (version 12.0).
3. Results
3.1. Geometrical Analysis
Canal volumes, surface areas, and mean apical diameters at baseline are presented in Table 1. Pre-operative values displayed homogeneity between groups (p > 0.05).

Table 1.
Sample baseline characteristics in the no-brushing and brushing groups (mean ± STD). Statistical significance indicated by p < 0.05. *Apical diameters (mean ± STD) at 1 mm from the apical foramen. B = brushing group; NB = no-brushing group; STD = standard deviation.
The mean curvature of the specimens was 21.2° ± 2.3° and 19.8° ± 3.1° in the NB and B groups, respectively, with no statistical difference between the groups (p = 0.12). There was no incidence of instrument fracture during canal preparation.
The mean increases in canal volume and surface area after shaping are reported in Table 2. Brushing technique led to a significant increase in canal volume (p = 0.026) and surface area (p = 0.019) compared to no-brushing technique. The differences in centroid shift and dentinal removal from the furcation at each level of analysis are presented in Table 2. Both 2D parameters showed significant differences for all levels of analysis (p < 0.05), except at the point of maximum curvature (M) (p > 0.05).

Table 2.
Variations in 3D and 2D parameters in both groups after shaping (mean ± STD). Statistical significance indicated by p < 0.05. Superscript letters in the same column indicate significant differences between groups (p < 0.05). For 2D parameters, significance was compared for the same level of analysis. (1.5F = 1.5 mm from the furcation; 2D = two-dimensional; 3D = three-dimensional; 3F = 3 mm from the furcation; B = brushing group; F = furcation; M = point of maximum curvature; NB = no-brushing group; STD = standard deviation; IQR = interquartile range). Different superscript letters (a, b) in the same column indicate significant differences between groups (p < 0.05).
3.2. Images Matching
Figure 1 and Figure 2 represent 2D and 3D matching of pre-operative (green) and post-shaping (red) sections at the four levels of analysis in both groups.
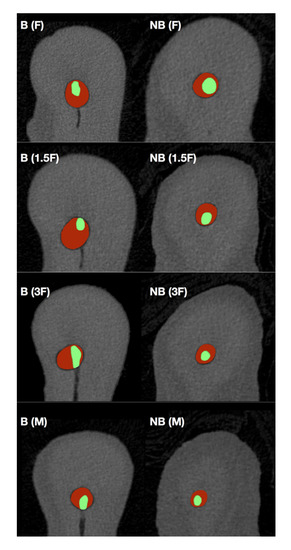
Figure 1.
Micro-CT scan matching of pre- and post-shaping sections, according to previously selected cutting planes. Note the difference between pre-operative (green) and post-shaping with WaveOne Gold Primary (red) specimens at the furcation (F), 1.5 mm apically from the furcation (1.5F), 3 mm apically from the furcation (3F), and in correspondence with the point of maximum curvature (M). B = brushing group; NB = no-brushing group.
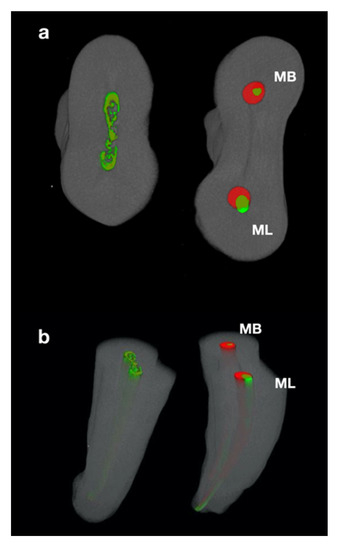
Figure 2.
Micro-CT scan matching of pre- and post-shaping volumes from a coronal (a) and lingual (b) projection. Note the difference between pre-operative (green) and post-shaping with WaveOne Gold Primary (red) volumes. In this representative sample the mesial root was shaped with (ML) and without (MB) brushing motion in the two different root canals. Note the wear at the furcation level “danger zone” especially in the ML canal.
4. Discussion
Brushing movement can be adopted after glide path to carry tapered files against the outer wall of the coronal curvature in order to obtain straight access to the apical third. It may be especially useful for the mesial canals of mandibular molars where it is intentionally directed against the outer side of the curvature where the dentine is thicker. This procedure should ease the use of shaping instruments up to WL and subsequent root canal filling, when using the continuous wave technique [18,23]. However, the instrument’s cutting action is not perfectly selective, and more aggressive shaping may lead to a weakening of the inner dentine walls [23,24]. The dentine in the mesial root of mandibular molars is thinner at the distal surface of the root, 1.5 mm below the furcation, which is generally only 1.2 mm thick [25,26,27]. Therefore, preservation of the original canal anatomy, without weakening the radicular structure, may lead to more favorable outcomes, in particular for the mesial root of the lower molars [4,24]. Moreover, the use of carrier-based techniques or single cones with bioceramic sealers could allow three-dimensional (3D) filling, even with low-tapered preparations [28,29].
This study evaluated the cutting efficiency and centering ability of WaveOne Gold Primary reciprocating single files used with or without brushing motion. Intentional brushing movement during shaping with the WaveOne Gold single-file technique led to a higher centroid shift and greater dentine removal from the inner aspect of the root canal, especially in the coronal third.
The evaluation of post-instrumentation geometrical variations is a reliable assessment of the ability of a shaping technique to preserve the canal anatomy [21]. An extracted tooth model is generally considered transferable to the clinical situation due to the similarity of the experimental conditions [30]. Homogeneity of pre-operative characteristics among selected samples is essential to ensure adequate standardization [24,31]. Micro-CT scans enable the identification of morphological changes associated with different biomechanical preparations, including canal transportation and dentine removal [20]. Moreover, the overlapping of pre- and post-operative root canal volumes allows for 3D quantitative analysis [1].
This study considered four levels of analysis in relation to the furcation area of the mesial root of mandibular molars where the dentine is thinner [27]. The limited amount of dentine at the furcal side of the mesial root of mandibular first molars means that this can be considered a ‘‘danger zone’’ [25,27]. Previous studies have reported that centering ability of the instruments is influenced by their design, the type of alloy, and the root canal anatomy [31,32], but no information is available about the effect of brushing motion on the shaping outcomes of single-file reciprocating instruments. The reciprocating motion helps to keep the instrument centered, promoting equal cutting force on the inner and external sides of the curvature [9,10,33]. Moreover, it allows the use of a single-file approach due to a reduction in the instrument’s torsional stress and wedging action [8,34]. Nevertheless, accomplishing glide path may reduce the number of pecking motions required to reach the full WL with the reciprocating instrument [5].
However, the significant increase in canal dimensions and the higher centroid shift and dentine removal from the inner curve suggests that increasing the number of brushing strokes could lead to a significant reduction in dentine wall thickness in both directions.
5. Conclusions
Within the limits of this study, the use of a brushing movement while shaping with WaveOne Gold Primary reciprocating instruments seemed to negatively impact the maintenance of the original root canal anatomy.
Author Contributions
Conceptualization, E.B., D.P., and M.A.; software, M.A. and E.M.; formal analysis, S.M.; data curation, A.C. and G.C.; writing—original draft preparation, S.M. and A.C.; writing—review and editing, G.C., M.A., and N.S.; visualization, N.S. and M.D.; supervision, E.B. and D.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Acknowledgments
Micro-CT scans were performed at C.I.R. Dental School—University of Turin (Italy).
Conflicts of Interest
The Authors declare no competing conflict of interests with the materials discussed in this manuscript.
References
- Burklein, S.; Schafer, E. Critical evaluation of root canal transportation by instrumentation. Endod. Topics 2013, 29, 110–124. [Google Scholar] [CrossRef]
- Hartmann, M.S.; Barletta, F.B.; Camargo Fontanella, V.R.; Vanni, J.R. Canal transportation after root canal instrumentation: A comparative study with computed tomography. J. Endod. 2007, 33, 962–965. [Google Scholar] [CrossRef] [PubMed]
- Hulsmann, M.; Peters, O.A.; Dummer, P.M.H. Mechanical preparation of root canals: Shaping goals, techniques and means. Endod. Topics 2005, 10, 30–76. [Google Scholar] [CrossRef]
- Jafarzadeh, H.; Abbott, P.V. Ledge formation: Review of a great challenge in endodontics. J. Endod. 2012, 33, 1155–1162. [Google Scholar] [CrossRef]
- Berutti, E.; Paolino, D.S.; Chiandussi, G.; Alovisi, M.; Cantatore, G.; Castellucci, A.; Pasqualini, D. Root canal anatomy preservation of Wave-One reciprocating files with or without glide path. J. Endod. 2012, 38, 101–104. [Google Scholar]
- Del Fabbro, M.; Afrashtehfar, K.I.; Corbella, S.; El-Kabbaney, A.; Perondi, I.; Taschieri, S. In Vivo and In Vitro Effectiveness of Rotary Nickel-Titanium vs Manual Stainless Steel Instruments for Root Canal Therapy: Systematic Review and Meta-analysis. J. Evid. Based Dent. Pract. 2018, 18, 59–69. [Google Scholar] [CrossRef]
- Haapasalo, M.; Shen, Y. Evolution of nickel–titanium instruments: From past to future. Endod. Topics 2013, 29, 3–17. [Google Scholar] [CrossRef]
- Yared, G. Canal preparation using only one Ni-Ti rotary instrument: Preliminary observations. Int. Endod. J. 2008, 41, 339–344. [Google Scholar] [CrossRef]
- Grande, N.M.; Ahmed, H.M.; Cohen, S.; Bukiet, F.; Plotino, G. Current assessment of reciprocation in endodontic preparation: A comprehensive review-part I: Historic perspectives and current applications. J. Endod. 2015, 41, 1778–1783. [Google Scholar] [CrossRef]
- Plotino, G.; Ahmed, H.M.; Grande, N.M.; Cohen, S.; Bukiet, F. Current assessment of reciprocation in endodontic preparation: A comprehensive review—Part II: Properties and effectiveness. J. Endod. 2015, 41, 1939–1950. [Google Scholar] [CrossRef]
- De-Deus, G.; Moreira, E.J.; Lopes, H.P.; Elias, C.N. Extended cyclic fatigue life of F2 ProTaper instruments used in reciprocating movement. Int. Endod. J. 2010, 43, 1063–1068. [Google Scholar] [CrossRef]
- Berutti, E.; Chiandussi, G.; Paolino, D.S.; Scotti, N.; Cantatore, G.; Castellucci, A.; Pasqualini, D. Effect of canal length and curvature on working length alteration with WaveOne reciprocating files. J. Endod. 2011, 37, 1687–1690. [Google Scholar] [CrossRef]
- You, S.Y.; Bae, K.S.; Baek, S.H.; Kum, K.Y.; Shon, W.J.; Lee, W. Lifespan of one nickel-titanium rotary file with reciprocating motion in curved root canals. J. Endod. 2010, 36, 1991–1994. [Google Scholar] [CrossRef]
- Varela-Patino, P.; Ibanez-Parraga, A.; Rivas-Mundina, B.; Cantatore, G.; Otero, X.L.; Martin-Biedma, B. Alternating versus continuous rotation: A comparative study of the effect on instrument life. J. Endod. 2010, 36, 157–159. [Google Scholar] [CrossRef] [PubMed]
- Haupt, F.; Wilhelm Pult, J.R.; Hülsmann, M. Micro-CT evaluation of the shaping ability of three reciprocating single-file NiTi-systems on single- and double-curved root canals. J. Endod. 2020. [Google Scholar] [CrossRef]
- Bueno, C.S.P.; Oliveira, D.P.; Pelegrine, R.A.; Fontana, C.E.; Rocha, D.G.P.; Gutmann, J.L.; Bueno, C.E.S. Fracture incidence of WaveOne Gold files: A prospective clinical study. Int. Endod. J. 2020. [Google Scholar] [CrossRef]
- WaveOne Gold Directions for Use. Available online: https://assets.dentsplysirona.com/master/product-procedure-brand-categories/endodontics/product-categories/files-motors-lubricants/rotary-files/reciprocating-files/waveone-gold/documents/END-DFU-WaveOne-Gold-Reciprocating-Files-EN.pdf (accessed on 15 February 2020).
- Alattar, S.; Nehme, W.; Diemer, F.; Naaman, A. The influence of brushing motion on the cutting behavior of 3 reciprocating files in oval-shaped canals. J. Endod. 2015, 41, 703–709. [Google Scholar] [CrossRef] [PubMed]
- WaveOne Gold DFU. Available online: https://www.dentsplysirona.com/content/dam/dentsply/pim/manufacturer/Endodontics/Glide_Path__Shaping/Rotary__Reciprocating_Files/Shaping/WaveOne_Gold_Reciprocating_Files/WaveOne%20Gold%202017_DFU_EN.pdf (accessed on 15 February 2020).
- Paquè, F.; Ganahl, D.; Peters, O.A. Effects of root canal preparation on apical geometry assessed by micro-computed tomography. J. Endod. 2009, 35, 1056–1059. [Google Scholar] [CrossRef]
- Pasqualini, D.; Alovisi, M.; Cemenasco, A.; Mancini, L.; Paolino, D.S.; Bianchi, C.C.; Roggia, A.; Scotti, N.; Berutti, E. Micro-computed tomography evaluation of ProTaper Next and BioRace shaping outcomes in maxillary first molar curved canals. J. Endod. 2015, 41, 1706–1710. [Google Scholar] [CrossRef]
- Neves, A.A.; Silva, E.J.; Roter, J.M. Exploiting the potential of free software to evaluate root canal biomechanical preparation outcomes through micro-CT images. Int. Endod. J. 2014, 48, 1033–1042. [Google Scholar] [CrossRef] [PubMed]
- Ruddle, C. Endodontic canal preparation: Breakthrough cleaning and shaping strategies. Dent. Today 1994, 13, 48–49. [Google Scholar] [PubMed]
- Alovisi, M.; Cemenasco, A.; Mancini, L.; Paolino, D.; Scotti, N.; Bianchi, C.C.; Pasqualini, D. Micro-CT evaluation of several glide path techniques and ProTaper Next shaping outcomes in maxillary first molar curved canals. Int. Endod. J. 2017, 50, 387–397. [Google Scholar] [CrossRef]
- Harris, S.P.; Bowles, W.R.; Fok, A.; McClanahan, S.B. An Anatomic Investigation of the Mandibular First Molar Using Micro–Computed Tomography. J. Endod. 2013, 39, 1374–1378. [Google Scholar] [CrossRef] [PubMed]
- Berutti, E.; Fedon, G. Thickness of cementum/dentin in mesial roots of mandibular first molars. J. Endod. 1992, 18, 545–548. [Google Scholar] [CrossRef]
- De-Deus, G.; Rodrigues, E.A.; Belladonna, F.G.; Carvalho, M.S.; Cavalcante, D.M.; Oliveira, D.S.; Souza, E.M.; Giorgi, K.A.; Versiani, M.A.; Lopes, R.T.; et al. Anatomical danger zone reconsidered: A micro-CT study on dentine thickness in mandibular molars. Int. Endod. J. 2019, 52, 1501–1507. [Google Scholar] [CrossRef]
- Whitworth, J. Methods of filling root canals: Principles and practices. Endod. Topics 2005, 12, 2–24. [Google Scholar] [CrossRef]
- Haapasalo, M.; Parhar, M.; Huang, X.; Wei, X.; Lin, J.; Shen, Y. Clinical use of bioceramic materials. Endod. Topics 2015, I, 97–117. [Google Scholar] [CrossRef]
- Hashem, A.A.R.; Ghoneim, A.G.; Lutfy, R.A.; Foda, M.Y.; Omar, G.A.F. Geometric analysis of root canals prepared by four rotary NiTi shaping systems. J. Endod. 2012, 38, 996–1000. [Google Scholar] [CrossRef]
- Zhao, D.; Shen, Y.; Peng, B.; Haapasalo, M. Root canal preparation of mandibular molars with 3 nickel-titanium rotary instruments: A micro-computed tomographic study. J. Endod. 2014, 40, 1860–1864. [Google Scholar] [CrossRef]
- Capar, I.D.; Ertas, H.; Ok, E.; Arslan, H.; Ertas, E.T. Comparative study of different novel nickel- titanium rotary systems for root canal preparation in severely curved root canals. J. Endod. 2014, 40, 852–856. [Google Scholar] [CrossRef] [PubMed]
- Berutti, E.; Chiandussi, G.; Paolino, D.S.; Scotti, N.; Cantatore, G.; Castellucci, A.; Pasqualini, D. Canal shaping with WaveOne Primary reciprocating files and ProTaper system: A comparative study. J. Endod. 2012, 38, 505–509. [Google Scholar] [CrossRef] [PubMed]
- Roane, J.B.; Sabala, C. Clockwise or counterclockwise. J. Endod. 1984, 10, 349–353. [Google Scholar] [CrossRef]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).