Assessment of the Different Types of Failure on Anterior Cantilever Resin-Bonded Fixed Dental Prostheses Fabricated with Three Different Materials: An In Vitro Study
Abstract
1. Introduction
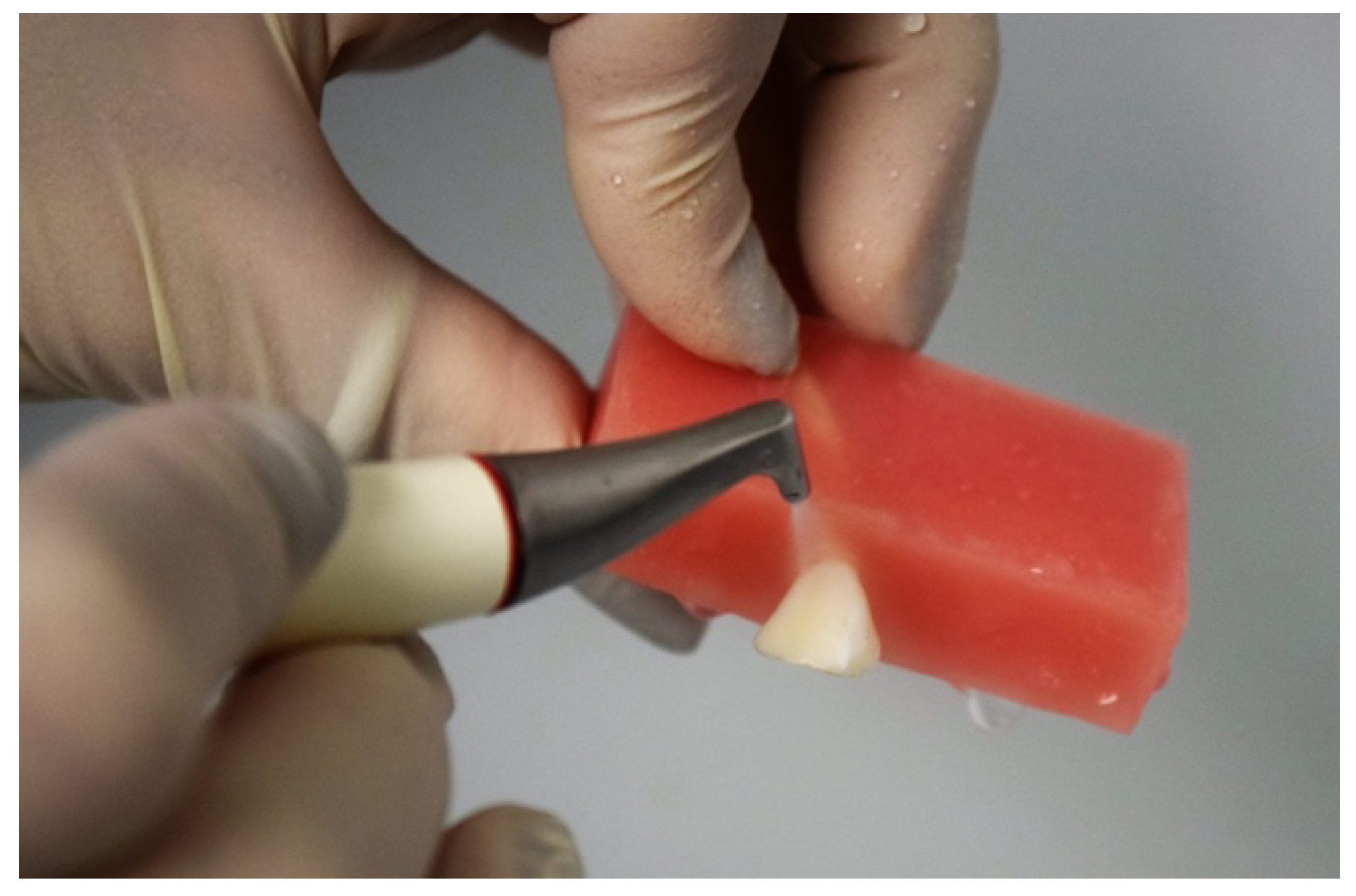
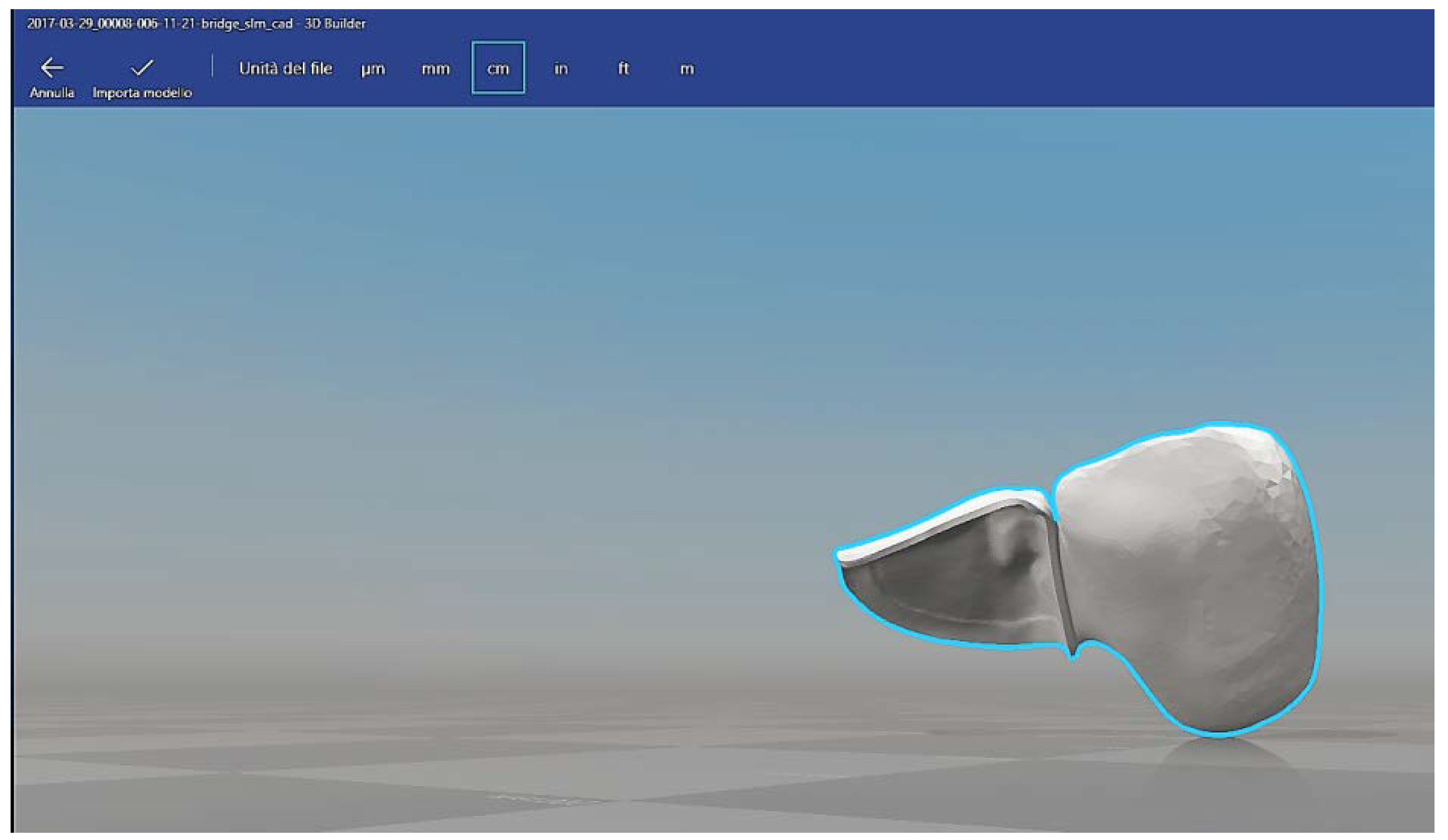
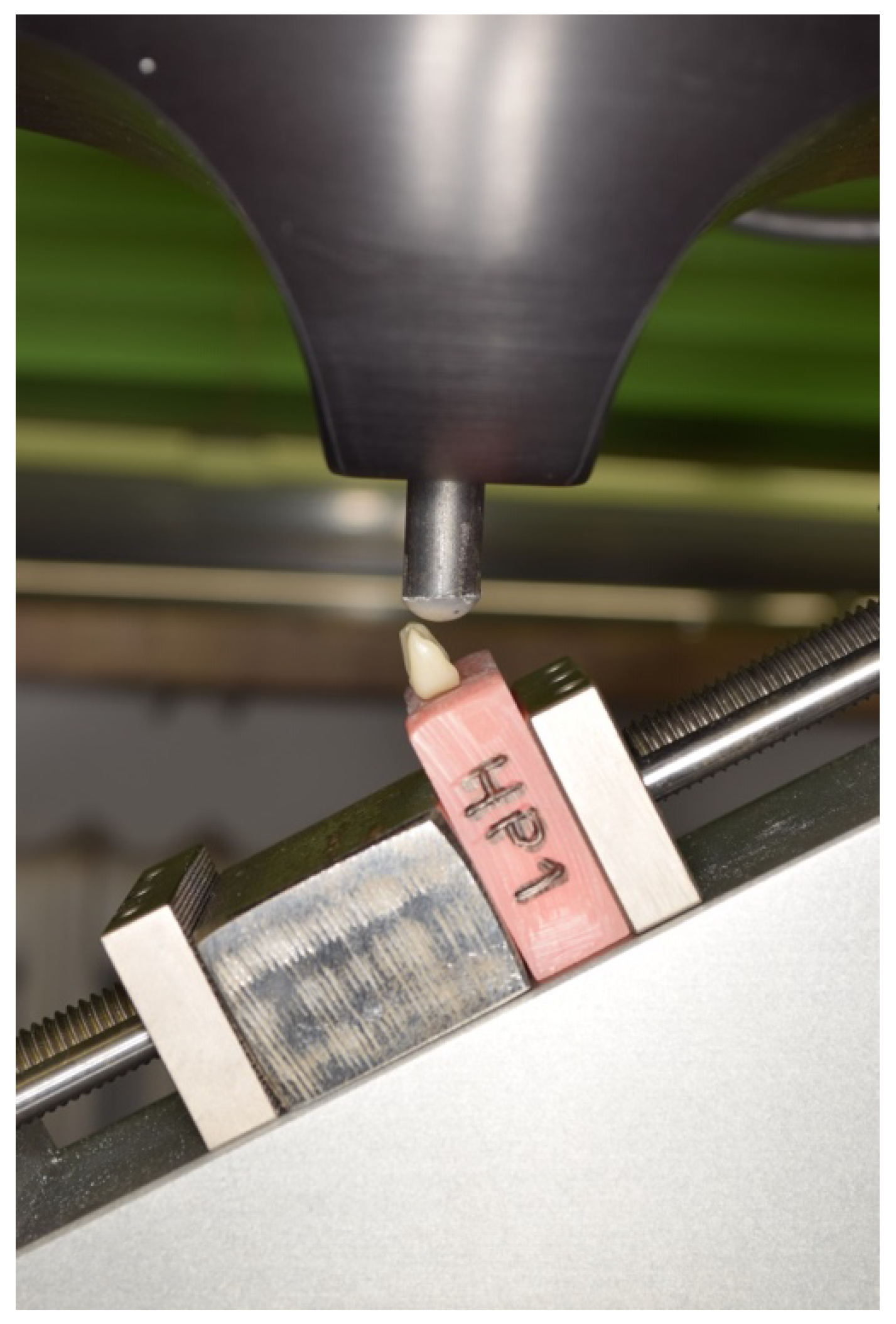
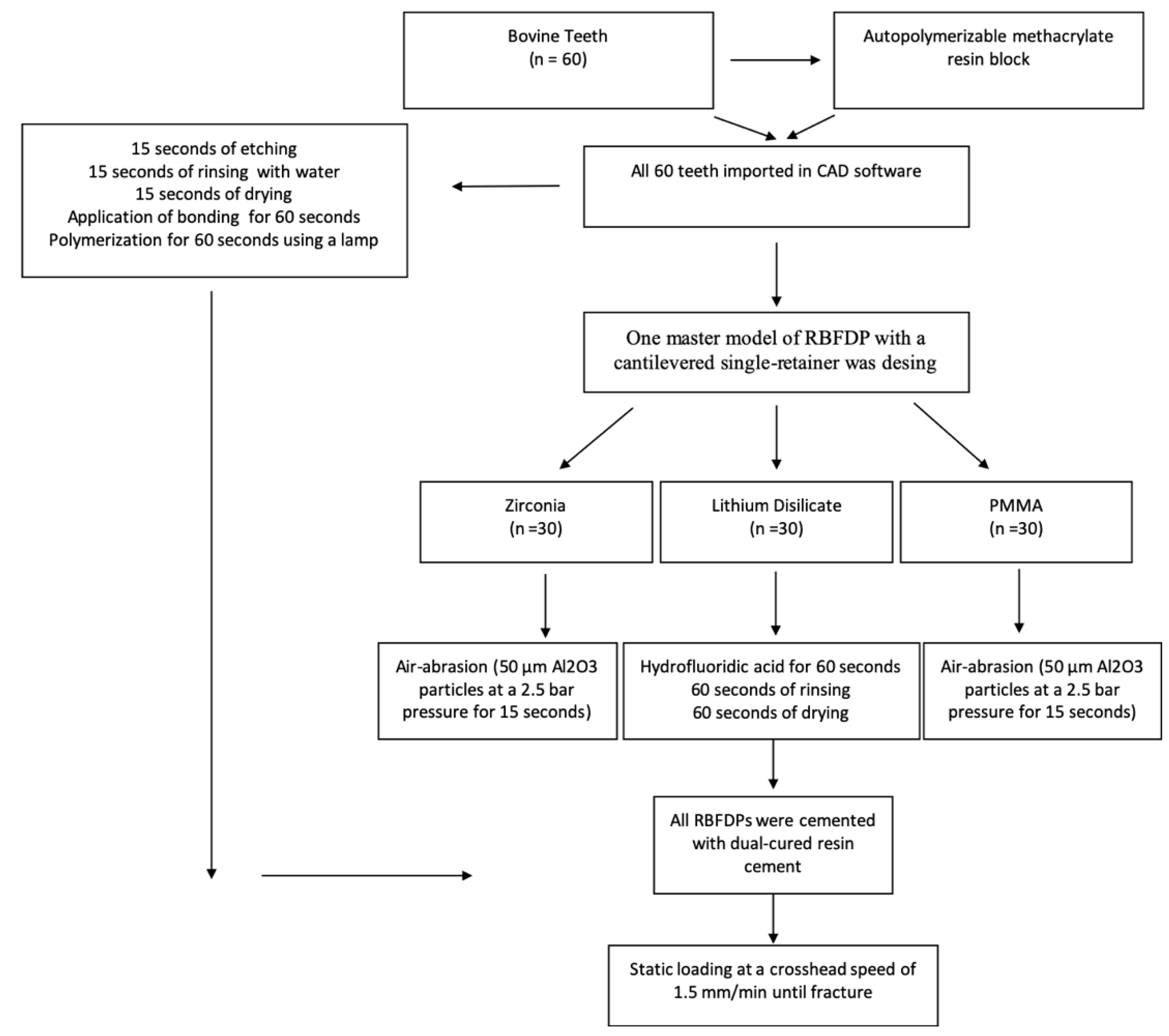
2. Materials and Methods
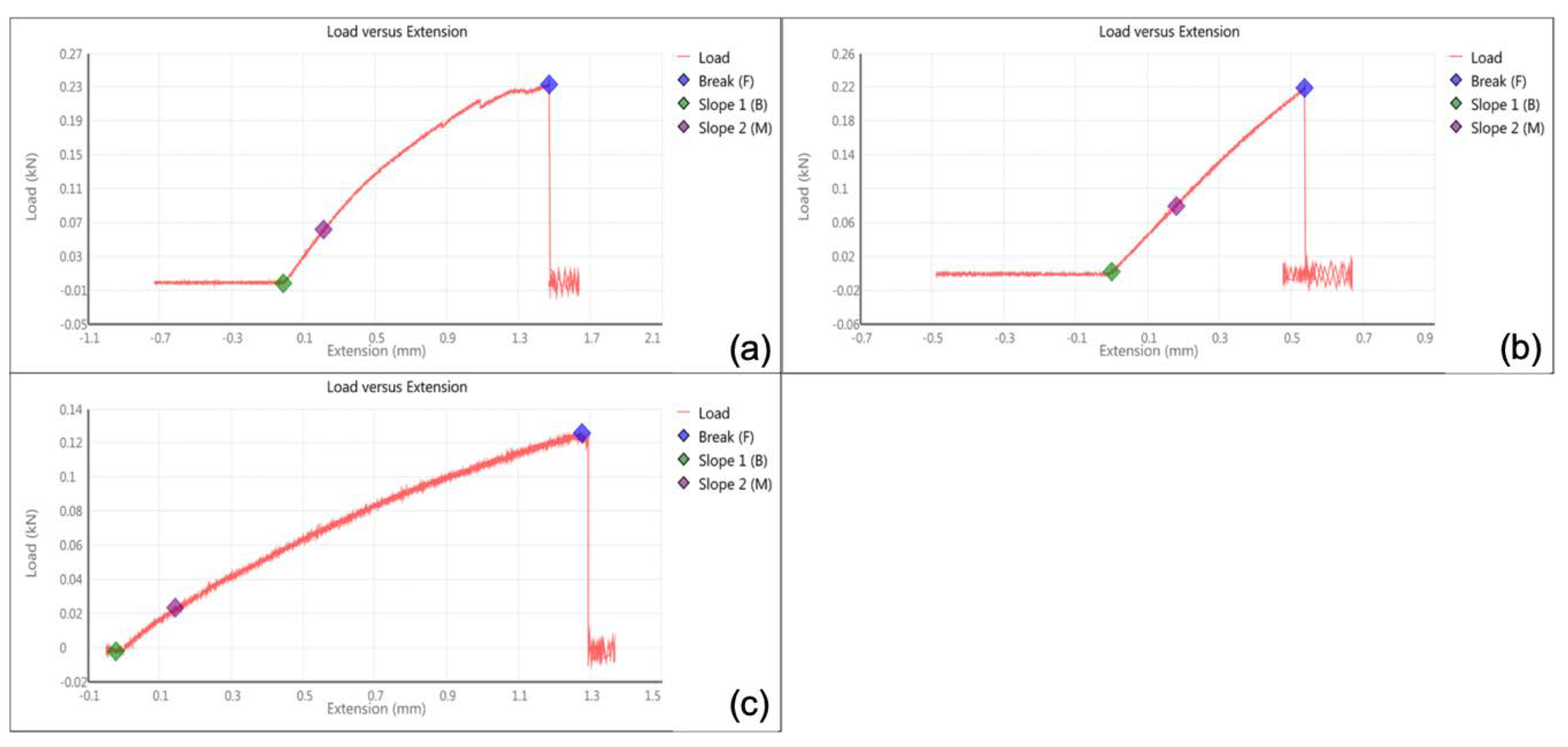
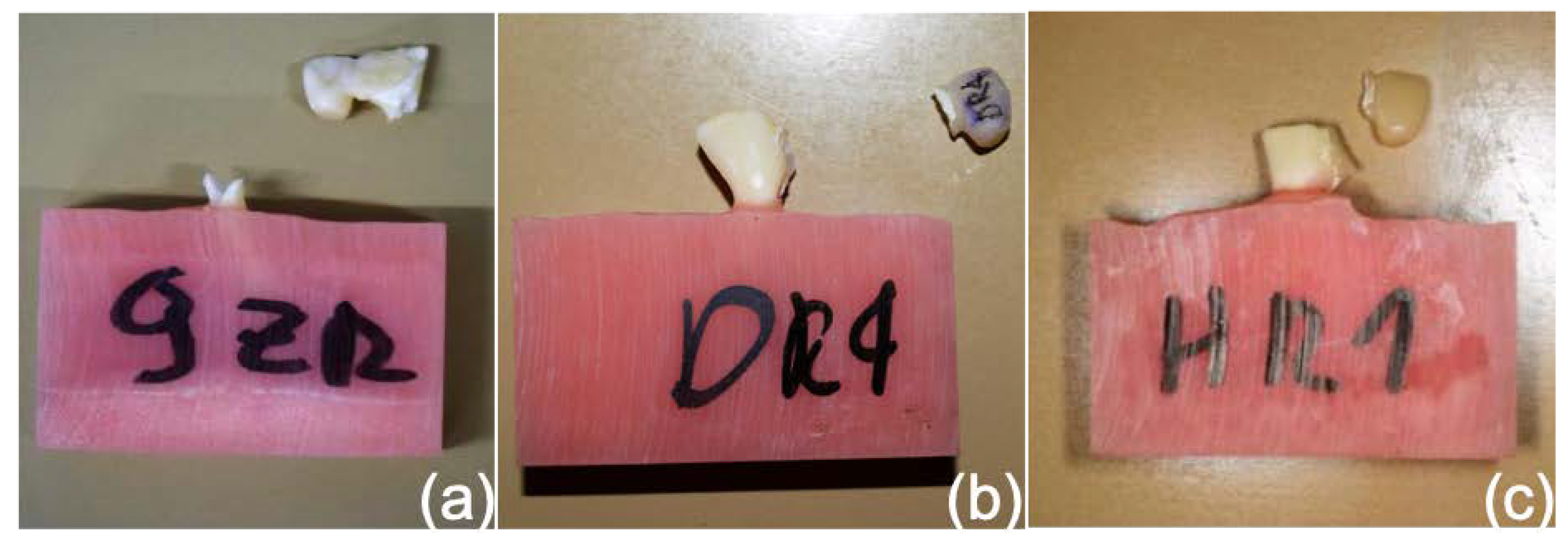
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Borum, M.K.; Andreasen, J.O. Therapeutic and economic implications of traumatic dental injuries in Denmark: An estimate based on 7549 patients treated at a major trauma centre. Int. J. Paediatr. Dent. 2001, 11, 249–258. [Google Scholar] [CrossRef]
- Andrade, D.C.; Loureiro, C.A.; Araujo, V.E.; Riera, R.; Atallah, A.N. Treatment for agenesis of maxillary lateral incisors: A systematic review. Orthod. Craniofac. Res. 2013, 16, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Wei, Y.R.; Wang, X.D.; Zhang, Q.; Li, X.X.; Blatz, M.B.; Jian, Y.T.; Zhao, K. Clinical performance of anterior resin-bonded fixed dental prostheses with different framework designs: A systematic review and meta-analysis. J. Dent. 2016, 47, 1–7. [Google Scholar] [CrossRef]
- Robertsson, S.; Mohlin, B. The congenitally missing upper lateral incisor: A retrospective study of orthodontic space closure versus restorative treatment. Eur. J. Orthod. 2000, 22, 697–709. [Google Scholar] [CrossRef]
- Thoma, D.S.; Sailer, I.; Ioannidis, A.; Zwahlen, M.; Makarov, N.; Pjetursson, B.E. A systematic review of the survival and complication rates of resin-bonded fixed dental prostheses after a mean observation period of at least 5 years. Clin. Oral. Implant. Res. 2017, 28, 1421–1432. [Google Scholar] [CrossRef] [PubMed]
- Botelho, M.G.; Ma, X.; Cheung, G.J.; Law, R.K.; Tai, M.T.; Lam, W.Y. Long-term clinical evaluation of 211 two-unit cantilevered resin-bonded fixed partial dentures. J. Dent. 2014, 42, 778–784. [Google Scholar] [CrossRef] [PubMed]
- Sasse, M.; Eschbach, S.; Kern, M. Randomized clinical trial on single retainer all-ceramic resin-bonded fixed partial dentures: Influence of the bonding system after up to 55 months. J. Dent. 2012, 40, 783–786. [Google Scholar] [CrossRef]
- El-Mowafy, O.; Rubo, M.H. Resin-bonded fixed partial dentures-a literature review with presentation of a novel approach. Int. J. Prosthodont. 2000, 13, 460–467. [Google Scholar]
- Keulemans, F.; Shinya, A.; Lassila, L.V.; Vallittu, P.K.; Kleverlaan, C.J.; Feilzer, A.J.; De Moor, R.J. Three-dimensional finite element analysis of anterior two-unit cantilever resin-bonded fixed dental prostheses. Sci. World J. 2015, 2015, 864389. [Google Scholar] [CrossRef]
- Kern, M.; Sasse, M. Ten-year survival of anterior all-ceramic resin-bonded fixed dental prostheses. J. Adhes. Dent. 2011, 13, 407–410. [Google Scholar]
- Kern, M. Clinical long-term survival of two-retainer and single-retainer all-ceramic resin-bonded fixed partial dentures. Quintessence Int. 2005, 36, 141–147. [Google Scholar] [PubMed]
- Botelho, M.G.; Leung, K.C.; Ng, H.; Chan, K. A retrospective clinical evaluation of two-unit cantilevered resin-bonded fixed partial dentures. J. Am. Dent. Assoc. 2006, 137, 783–788. [Google Scholar] [CrossRef] [PubMed]
- Botelho, M.G.; Chan, A.W.; Leung, N.C.; Lam, W.Y. Long-term evaluation of cantilevered versus fixed-fixed resin-bonded fixed partial dentures for missing maxillary incisors. J. Dent. 2016, 45, 59–66. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Mourshed, B.; Samran, A.; Alfagih, A.; Samran, A.; Abdulrab, S.; Kern, M. Anterior cantilever resin-bonded fixed dental prostheses: A review of the literature. J. Prosthodont. 2018, 27, 266–275. [Google Scholar] [CrossRef]
- Kern, M. Fifteen-year survival of anterior all-ceramic cantilever resin-bonded fixed dental prostheses. J. Dent. 2017, 56, 133–135. [Google Scholar] [CrossRef]
- Sasse, M.; Kern, M. Survival of anterior cantilevered all-ceramic resin-bonded fixed dental prostheses made from zirconia ceramic. J. Dent. 2014, 42, 660–663. [Google Scholar] [CrossRef]
- Kern, M.; Passia, N.; Sasse, M.; Yazigi, C. Ten-year outcome of zirconia ceramic cantilever resin-bonded fixed dental prostheses and the influence of the reasons for missing incisors. J. Dent. 2017, 65, 51–55. [Google Scholar] [CrossRef]
- Sailer, I.; Bonani, T.; Brodbeck, U.; Hämmerle, C.H. Retrospective clinical study of single-retainer cantilever anterior and posterior glass-ceramic resin-bonded fixed dental prostheses at a mean follow-up of 6 years. Int. J. Prosthodont. 2013, 26, 443–450. [Google Scholar] [CrossRef]
- Di Fiore, A.; Meneghello, R.; Graiff, L.; Savio, G.; Vigolo, P.; Monaco, C.; Stellini, E. Full arch digital scanning systems performances for implant-supported fixed dental prostheses: A comparative study of 8 intraoral scanners. J. Prosthodont. Res. 2019, 63, 396–403. [Google Scholar] [CrossRef]
- Di Fiore, A.; Vigolo, P.; Graiff, L.; Stellini, E. Digital vs Conventional Workflow for Screw-Retained Single-Implant Crowns: A Comparison of Key Considerations. Int. J. Prosthodont. 2018, 31, 577–579. [Google Scholar] [CrossRef]
- Granata, S.; Giberti, L.; Vigolo, P.; Stellini, E.; Di Fiore, A. Incorporating a facial scanner into the digital workflow: A dental technique. J. Prosthet. Dent. 2019, 19, 30356–30357. [Google Scholar] [CrossRef] [PubMed]
- Malaguti, G.; Rossi, R.; Marziali, B.; Esposito, A.; Bruno, G.; Dariol, C.; Di Fiore, A. In vitro evaluation of prosthodontic impression on natural dentition: A comparison between traditional and digital techniques. Oral Implantol. 2017, 9, 21–27. [Google Scholar] [CrossRef] [PubMed]
- Sirisha, K.; Rambabu, T.; Ravishankar, Y.; Ravikumar, P. Validity of bond strength tests: A critical review-Part II. J. Conserv. Dent. 2014, 17, 420–426. [Google Scholar] [CrossRef]
- Koutayas, S.O.; Kern, M.; Ferraresso, F.; Strub, J.R. Influence of framework design on fracture strength of mandibular anterior all-ceramic resin-bonded fixed partial dentures. Int. J. Prosthodont. 2002, 15, 223–229. [Google Scholar]
- Yokoyama, D.; Shinya, A.; Lassila, L.V.; Gomi, H.; Nakasone, Y.; Vallittu, P.K.; Shinya, A. Framework design of an anterior fiber-reinforced hybrid composite fixed partial denture: A 3D finite element study. Int. J. Prosthodont. 2009, 22, 405–412. [Google Scholar] [PubMed]
- Koutayas, S.O.; Kern, M.; Ferraresso, F.; Strub, J.R. Influence of design and mode of loading on the fracture strength of all-ceramic resin-bonded fixed partial dentures: An in vitro study in a dual-axis chewing simulator. J. Prosthet. Dent. 2000, 84, 112. [Google Scholar] [CrossRef]
- De Boever, J.A.; McCall, W.D., Jr.; Holden, S.; Ash, M.M., Jr. Functional occlusal forces: An investigation by telemetry. J. Prosthet. Dent. 1978, 40, 326–333. [Google Scholar] [CrossRef]
- Kiliaridis, S.; Kjellberg, H.; Wenneberg, B.; Engstrom, C. The relationship between maximal force, bite force endurance, and facial morphology during growth. A cross-sectional study. Acta. Odontol. Scand. 1993, 51, 323–331. [Google Scholar] [CrossRef]


© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Di Fiore, A.; Stellini, E.; Savio, G.; Rosso, S.; Graiff, L.; Granata, S.; Monaco, C.; Meneghello, R. Assessment of the Different Types of Failure on Anterior Cantilever Resin-Bonded Fixed Dental Prostheses Fabricated with Three Different Materials: An In Vitro Study. Appl. Sci. 2020, 10, 4151. https://doi.org/10.3390/app10124151
Di Fiore A, Stellini E, Savio G, Rosso S, Graiff L, Granata S, Monaco C, Meneghello R. Assessment of the Different Types of Failure on Anterior Cantilever Resin-Bonded Fixed Dental Prostheses Fabricated with Three Different Materials: An In Vitro Study. Applied Sciences. 2020; 10(12):4151. https://doi.org/10.3390/app10124151
Chicago/Turabian StyleDi Fiore, Adolfo, Edoardo Stellini, Gianpaolo Savio, Stefano Rosso, Lorenzo Graiff, Stefano Granata, Carlo Monaco, and Roberto Meneghello. 2020. "Assessment of the Different Types of Failure on Anterior Cantilever Resin-Bonded Fixed Dental Prostheses Fabricated with Three Different Materials: An In Vitro Study" Applied Sciences 10, no. 12: 4151. https://doi.org/10.3390/app10124151
APA StyleDi Fiore, A., Stellini, E., Savio, G., Rosso, S., Graiff, L., Granata, S., Monaco, C., & Meneghello, R. (2020). Assessment of the Different Types of Failure on Anterior Cantilever Resin-Bonded Fixed Dental Prostheses Fabricated with Three Different Materials: An In Vitro Study. Applied Sciences, 10(12), 4151. https://doi.org/10.3390/app10124151





