A Review of Carpal Tunnel Syndrome and Its Association with Age, Body Mass Index, Cardiovascular Risk Factors, Hand Dominance, and Sex
Abstract
:Featured Application
Abstract
1. Introduction
2. Methodology
2.1. Search Strategy
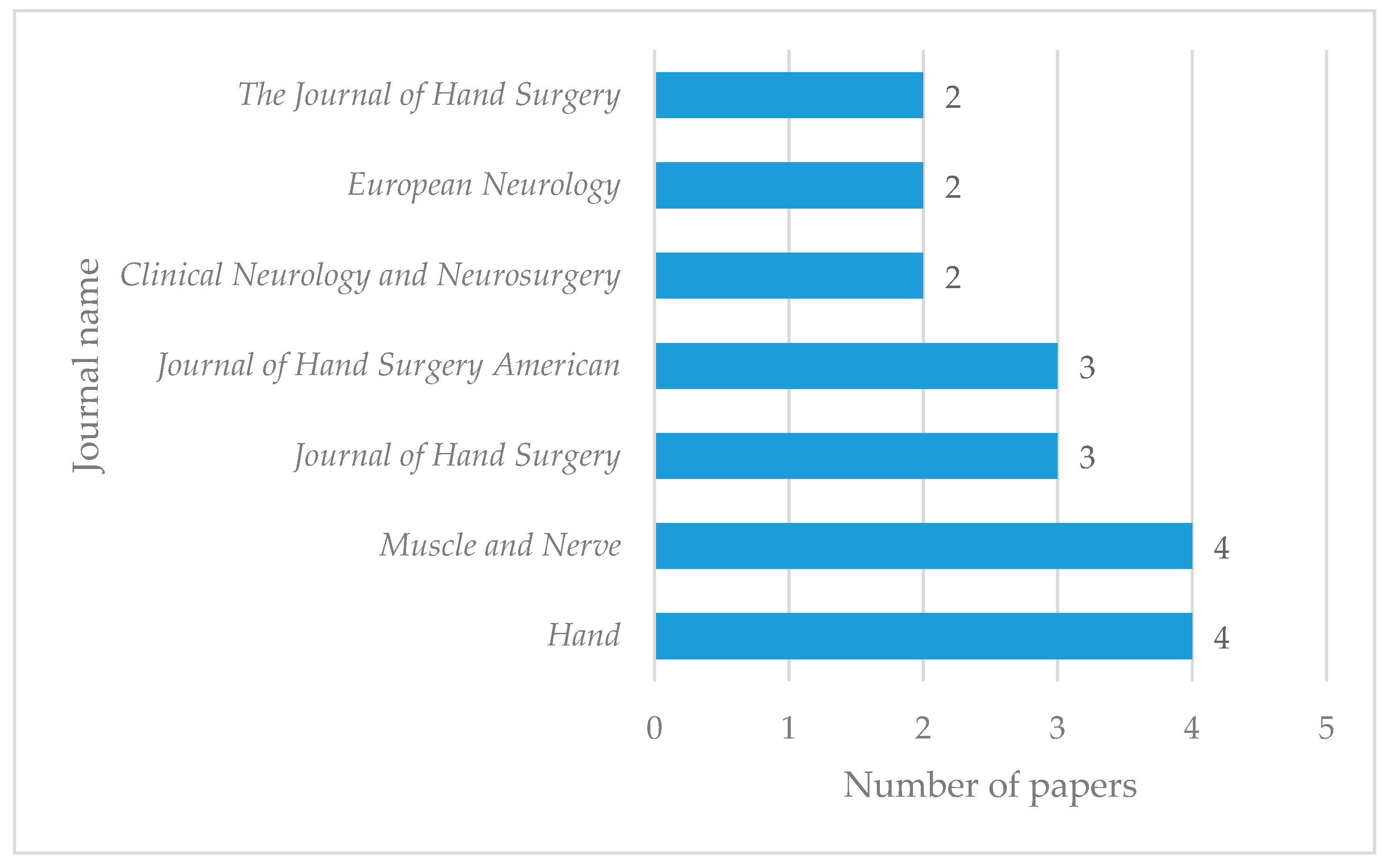
2.2. Screening and Eligibility Results
3. Results
3.1. Association of Age with Carpal Tunnel Syndrome
3.2. Association of Body Mass Index with Carpal Tunnel Syndrome
3.3. Association of Cardiovascular Factor with Carpal Tunnel Syndrome
3.4. Association of Hand Dominance with Carpal Tunnel Syndrome
3.5. Association of Sex with Carpal Tunnel Syndrome
3.6. Association of Multifactors with Carpal Tunnel Syndrome
4. Trends and Future Challenges
5. Limitations
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A. Journals with One Publication
| Journal | Year of Publication |
| Pakistan Journal Medical Sciences | 2019 |
| Rev. Chir. Orthop. Traumatol | 2018 |
| Nigerian Journal of Clinical Practice | 2018 |
| Advanced Biomedical Research | 2018 |
| Clinical Neurophysiology | 2018 |
| Psychiatry Neurosurgery | 2018 |
| Clinical Anatomy | 2018 |
| Neurological Sciences Journal | 2017 |
| Journal of Occupational Health | 2017 |
| Asian Journal of Neurosurgery | 2017 |
| BMJ Open | 2017 |
| Annals of Rehabilitation Medicine | 2017 |
| Cureus | 2017 |
| Journal of Clinical Neurophysiology | 2017 |
| J. Med. Ultrason. | 2016 |
| J. Clin. Diagnostic Res. | 2016 |
| Ar. of Physical Medicine Rehab. | 2016 |
| Radiologia Brasileira | 2015 |
| Plastic. Reconstruction. Surgery | 2015 |
| J. of Turgut Ozal Medical Center | 2015 |
| Coll Antropol. | 2014 |
| Neurol. Med. Chir | 2014 |
| Occup. Environ. Med. | 2013 |
| Egyptian J. of Neurol., Psychiat. & Neurosurg. | 2013 |
| Trauma Mon | 2012 |
| BioMed Central Musculoskeletal Disorders | 2011 |
| Clin. Orthop. Relat. Res. | 2010 |
| J. of Brachial Plexus and Peripheral Nerve Injury | 2009 |
| J. Hand Surgery—European | 2009 |
| Occupational and Environmental Medicine | 2009 |
| Scand. J. Work Environ. Health | 2009 |
| Int. Orthop. | 2008 |
| Folia Morphologica | 2008 |
| J. Gen. Pract. | 2007 |
| Arch. Phys. Med. Rehabil. | 2007 |
| British Society for Clinical Neurophysiology | 2006 |
| Neurophysiologie Clinique | 2006 |
| Ortopedia Traumatologia Rehabilitacja | 2006 |
| Hand Surg. | 2005 |
| Acta Neurologica Scandinavica | 2005 |
| European Journal of Neurology | 2005 |
| Clin. Neurol. Neurosurg. | 2004 |
| Clin. Neurophysiol. | 2002 |
| American J.of Physical Medicine & Rehab. | 2002 |
| The Journal of Bone & Joint Surgery | 2002 |
| Am. J. Ind. Med. | 2002 |
| Annals of Epidemiology | 2000 |
| Arq. Neuropsiquiatr. | 2000 |
| Environ. Res. | 2000 |
References
- Padua, L.; Coraci, D.; Erra, C.; Pazzaglia, C.; Paolasso, I.; Loreti, C.; Caliandro, P.; Hobson-Webb, L.D. Carpal tunnel syndrome: Clinical features, diagnosis, and management. Lancet Neurol. 2016, 15, 1273–1284. [Google Scholar] [CrossRef]
- Jesensek Papez, B.; Palfy, M.; Turk, Z. Infrared Thermography Based on Artificial Intelligence for Carpal Tunnel Syndrome Diagnosis. J. Int. Med Res. 2008, 1363–1370. [Google Scholar] [CrossRef]
- Petit, A.; Ha, C.; Bodin, J.; Rigouin, P.; Descatha, A.; Brunet, R.; Goldberg, M.; Roquelaure, Y. Risk factors for carpal tunnel syndrome related to the work organization: A prospective surveillance study in a large population. Appl. Ergon. 2015, 47, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Vázquez, M.F.; Briseño Pérez, J.; Cano Rebolledo, R. Simultaneous bilateral open surgery for carpal tunnel syndrome. In Degree of Satisfaction; Mexican Orthopedic Act: Mexico City, Mexico, 2009; pp. 80–84. [Google Scholar]
- Roel-Valdés, J.; Arizo-Luque, V.; Ronda-Pérez, E. Epidemiology of Occupational Carpal Tunnel Syndrome in Alicante Province, 1996–2004. Spain Public Health Mag. 2006, 80, 395–409. [Google Scholar]
- Raja, S.; Carlos, A.J. Carpal tunnel syndrome—Current controversies. Orthop. Trauma 2015, 29, 273–277. [Google Scholar] [CrossRef]
- Komurcu, H.F.; Kilic, S.; Anlar, O. Relationship of age, body mass index, wrist and waist circumferences to carpal tunnel syndrome severity. Neurol. Med. Chir. 2014, 54, 395–400. [Google Scholar] [CrossRef] [Green Version]
- Sousa, E.; Vardasca, R.; Teixeira, S.; Seixas, A.; Mendes, J.; Costa-Ferreira, A. A review on the application of medical infrared thermal imaging in hands. Infrared Phys. Technol. 2017, 85, 315–323. [Google Scholar] [CrossRef]
- Zyluk, A.; Puchalski, P. A comparison of the results of carpal tunnel release in patients in different age groups. Neurol. I Neurochir. Pol. 2013, 47, 241–246. [Google Scholar] [CrossRef]
- Porter, P.; Venkateswaran, B.; Stephenson, H.; Wray, C.C. The influence of age on outcome after operation for the carpal tunnel syndrome. J. Bone Jt. Surg. 2002, 84, 688–691. [Google Scholar] [CrossRef]
- Hansen, T.; Larsen, K. Age is an important predictor of short-term outcome in endoscopic carpal tunnel release. J. Hand Surg. Eur. 2009, 34, 660–664. [Google Scholar] [CrossRef]
- Haghighat, A.; Khosrawi, S.; Kelishadi, A.; Sajadieh, S.; Badrian, H. Prevalence of clinical findings of carpal tunnel syndrome in Isfahanian dentists. Adv. Biomed. Res. 2012, 1, 13. [Google Scholar] [PubMed]
- Moschovos, C.; Tsivgoulis, G.; Kyrozis, A.; Ghika, A.; Karachalia, P.; Voumvourakis, K.; Chroni, E. The diagnostic accuracy of high-resolution ultrasound in screening for carpal tunnel syndrome and grading its severity is moderated by age. Clin. Neurophysiol. 2019, 130, 321–330. [Google Scholar] [CrossRef] [PubMed]
- Wilgis, E.F.; Burke, F.D.; Dubin, N.H.; Sinha, S.; Bradley, M.J. A prospective assessment of carpal tunnel surgery with respect to age. J. Hand Surg. Br. 2006, 31, 401–406. [Google Scholar] [CrossRef] [PubMed]
- de Saboya Lenzi, L.G.; Fernandes, C.H.; Myiamoto Meirelles, L.; Baptista Gomes Dos Santos, J.; Faloppa, F.; Raduan Neto, J. Triggering of Carpal Tunnel Syndrome Symptoms in Patients Using Urban Public Transportation. Hand 2016, 11, 257–261. [Google Scholar] [CrossRef] [Green Version]
- Ozcakir, S.; Sigirli, D.; Avsaroglu, H. High wrist ratio is a risk factor for carpal tunnel syndrome. Clin. Anat. 2018, 31, 698–701. [Google Scholar] [CrossRef]
- Sharifi-Mollayousef, A.; Yazdchi-Marand, M.; Ayramlou, H.; Heidar, P.; Salavati, A.; Zarrintan, S.; Sharifi-Mollayousefi, A. Assessment of body mass index and hand anthropometric measurements as independent risk factors for carpal tunnel syndrome. Folia Morphol. 2008, 67, 36–42. [Google Scholar]
- Ünaldı, H.K.; Kurt, S.; Çevik, B.; Mumcuoğlu, İ.; Sümbül, O. The Relationship Between Waist Circumference, Wrist Circumference, and Body Mass Index in Carpal Tunnel Syndrome. J. Turgut Ozal Med Cent. 2015, 22, 152–157. [Google Scholar]
- Kurt, S.; Kisacik, B.; Kaplan, Y.; Yildirim, B.; Etikan, I.; Karaer, H. Obesity and carpal tunnel syndrome: Is there a causal relationship? Eur. Neurol. 2008, 59, 253–257. [Google Scholar] [CrossRef]
- Landau, M.E.; Barner, K.C.; Campbell, W.W. Effect of body mass index on ulnar nerve conduction velocity, ulnar neuropathy at the elbow, and carpal tunnel syndrome. Muscle Nerve 2005, 32, 360–363. [Google Scholar] [CrossRef]
- Hassan, M.M.; Al-Hawary, M.A. Body Mass Index and Motor Distal Latency as Independent Risk Factors for Recurrent Carpal Tunnel Syndrome Following an Open Release Surgery. Egypt. J. Neurol. Psychiatry Neurosurg. 2013, 50, 13–17. [Google Scholar]
- Bodavula, V.K.; Burke, F.D.; Dubin, N.H.; Bradley, M.J.; Wilgis, E.F. A prospective, longitudinal outcome study of patients with carpal tunnel surgery and the relationship of body mass index. Hand 2007, 2, 27–33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mansoor, S.; Siddiqui, M.; Mateen, F.; Saadat, S.; Khan, Z.H.; Zahid, M.; Khan, H.H.; Malik, S.A.; Assad, S. Prevalence of Obesity in Carpal Tunnel Syndrome Patients: A Cross-Sectional Survey. Cureus 2017, 9, e1519. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aygul, R.; Ulvi, H.; Kotan, D.; Kuyucu, M.; Demir, R. Sensitivities of conventional and new electrophysiological techniques in carpal tunnel syndrome and their relationship to body mass index. J. Brachial Plex. Peripher. Nerve Inj. 2009, 4, 12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kouyoumdjian, J.A.; Morita, M.D.P.A.; Rocha, P.R.F.; Miranda, R.C.; Gouveia, G.M. Body Mass Index and Carpal Tunnel Syndrome. Arch. Neuropsychiatry 2000, 58, 252–256. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, D.K.; Kim, B.S.; Kim, M.J.; Kim, K.H.; Park, B.K.; Kim, D.H. Electrophysiologic and Ultrasonographic Assessment of Carpal Tunnel Syndrome in Wheelchair Basketball Athletes. Ann. Rehabil. Med. 2017, 41, 58–65. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nageeb, R.S.; Shehta, N.; Nageeb, G.S.; Omran, A.A. Body mass index and vitamin D level in carpal tunnel syndrome patients. Egypt. J. Neurol. Psychiatry Neurosurg. 2018, 54, 14. [Google Scholar] [CrossRef]
- Shiri, R.; Heliovaara, M.; Moilanen, L.; Viikari, J.; Liira, H.; Viikari-Juntura, E. Associations of cardiovascular risk factors, carotid intima-media thickness and manifest atherosclerotic vascular disease with carpal tunnel syndrome. BMC Musculoskelet. Disord. 2011, 12, 80. [Google Scholar] [CrossRef]
- Tang, Q.Y.; Lai, W.H.; Tay, S.C. The Effect of Hand Dominance on Patient-Reported Outcomes of Carpal Tunnel Release in Patients with Bilateral Carpal Tunnel Syndrome. J. Hand Surg. (Asian-Pacific Vol.) 2017, 22, 303–308. [Google Scholar] [CrossRef] [Green Version]
- McDiarmid, M.; Oliver, M.; Ruser, J.; Gucer, P. Male and female rate differences in carpal tunnel syndrome injuries: Personal attributes or job tasks? Environ. Res. 2000, 83, 23–32. [Google Scholar] [CrossRef]
- Roquelaure, Y.; Ha, C.; Fouquet, N.; Descatha, A.; Leclerc, A.; Goldberg, M.; Imbernon, E. Attributable risk of carpal tunnel syndrome in the general population implications for intervention programs in the workplace. Scand. J. Work. Environ. Heal. 2009, 35, 342–348. [Google Scholar] [CrossRef] [Green Version]
- Giersiepen, K.; Eberle, A.; Pohlabeln, H. Gender differences in carpal tunnel syndrome? occupational and non-occupational risk factors in a population-based case-control study. Ann. Epidemiol. 2000, 10, 481. [Google Scholar] [CrossRef]
- Ulusoy, E.; Çıraklı, A.; Ekinci, Y. The role of electrophysiological examination in the diagnosis of carpal tunnel syndrome: Analysis of 2516 patients. Niger. J. Clin. Pract. 2018, 21, 731–734. [Google Scholar] [CrossRef]
- Sassi, S.A.; Giddins, G. Gender differences in carpal tunnel relative cross-sectional area: A possible causative factor in idiopathic carpal tunnel syndrome. J. Hand Surg. Eur. Vol. 2016, 41, 638–642. [Google Scholar] [CrossRef] [PubMed]
- El-Helaly, M.; Balkhy, H.H.; Vallenius, L. Carpal tunnel syndrome among laboratory technicians in relation to personal and ergonomic factors at work. J. Occup. Health 2017, 59, 513–520. [Google Scholar] [CrossRef] [Green Version]
- Gruber, L.; Gruber, H.; Djurdjevic, T.; Schullian, P.; Loizides, A. Gender influence on clinical presentation and high-resolution ultrasound findings in primary carpal tunnel syndrome: Do women only differ in incidence? J. Med. Ultrason. 2016, 43, 413–420. [Google Scholar] [CrossRef] [PubMed]
- Arslan, Y.; Bulbul, I.; Ocek, L.; Sener, U.; Zorlu, Y. Effect of hand volume and other anthropometric measurements on carpal tunnel syndrome. Neurol. Sci. 2017, 38, 605–610. [Google Scholar] [CrossRef] [PubMed]
- Boz, C.; Ozmenoglu, M.; Altunayoglu, V.; Velioglu, S.; Alioglu, Z. Individual risk factors for carpal tunnel syndrome: An evaluation of body mass index, wrist index and hand anthropometric measurements. Clin. Neurol. Neurosurg. 2004, 106, 294–299. [Google Scholar] [CrossRef] [PubMed]
- Mondelli, M.; Curti, S.; Mattioli, S.; Aretini, A.; Ginanneschi, F.; Greco, G.; Farioli, A. Associations Between Body Anthropometric Measures and Severity of Carpal Tunnel Syndrome. Arch. Phys. Med. Rehabil. 2016, 97, 1456–1464. [Google Scholar] [CrossRef]
- Kouyoumdjian, J.A.; Zanetta, D.M.; Morita, M.P. Evaluation of age, body mass index, and wrist index as risk factors for carpal tunnel syndrome severity. Muscle Nerve 2002, 25, 93–97. [Google Scholar] [CrossRef]
- Hlebs, S.; Majhenic, K.; Vidmar, G. Body mass index and anthropometric characteristics of the hand risk factors for carpal tunnel syndrome. Coll. Antropol. 2014, 38, 219–226. [Google Scholar]
- Thiese, M.S.; Merryweather, A.; Koric, A.; Ott, U.; Wood, E.M.; Kapellusch, J.; Fosterr, J.; Garg, A.; Deckow-Schaefer, G.; Tomich, S.; et al. Association between wrist ratio and carpal tunnel syndrome: Effect modification by body mass index. Muscle Nerve 2017, 56, 1047–1053. [Google Scholar] [CrossRef] [PubMed]
- Moghtaderi, A.; Izadi, S.; Sharafadinzadeh, N. An evaluation of gender, body mass index, wrist circumference and wrist ratio as independent risk factors for carpal tunnel syndrome. Acta Neurol. Scand. 2005, 112, 375–379. [Google Scholar] [CrossRef] [PubMed]
- Iwuagwu, O.C.; Bajalan, A.A.; Reese, A.; Drew, P.J. Macromastia and carpal tunnel syndrome – Is there an association? Clin. Neurophysiol. 2007, 118, e155–e156. [Google Scholar] [CrossRef]
- Sousa Vasconcelos, J.T.; Freitas Paiva, A.M.; Cavalcanti, M.F.; de Carvalho, J.F.; Bonfa, E.; Borba, E.F. Carpal tunnel syndrome and prediabetes: Is there a true association? Clin. Neurol. Neurosurg. 2015, 137, 57–61. [Google Scholar] [CrossRef]
- Zambelis, T.; Tsivgoulis, G.; Karandreas, N. Carpal tunnel syndrome: Associations between risk factors and laterality. Eur. Neurol. 2010, 63, 43–47. [Google Scholar] [CrossRef]
- Becker, J.; Nora, D.B.; Gomes, I.; Stringari, F.F.; Seitensus, R.; Panosso, J.S.; Ehlers, J.A.C. An evaluation of gender, obesity, age and diabetes mellitus as risk factors for carpal tunnel syndrome. Clin. Neurophysiol. 2002, 113, 1429–1434. [Google Scholar] [CrossRef]
- Karne, S.S.; Bhalerao, N.S. Carpal Tunnel Syndrome in Hypothyroidism. J. Clin. Diagn. Res. 2016, 10, OC36–OC38. [Google Scholar] [CrossRef]
- Geoghegan, J.M.; Clark, D.I.; Bainbridge, L.C.; Smith, C.; Hubbard, R. Risk factors in carpal tunnel syndrome. J. Hand Surg. Br. 2004, 29, 315–320. [Google Scholar] [CrossRef]
- Solmaz, V.; Yavuz, S.; Inanr, A.; Aksoy, D.; Pektas, E.; Tekatas, A.; Kurt, S.G. Investigation of Nerve Conduction Studies of Carpal Tunnel Syndrome Cases With Different Risk Factors: An Electrodiagnostic Study. J. Clin. Neurophysiol. 2017, 34, 139–143. [Google Scholar] [CrossRef]
- Zhang, D.; Collins, J.E.; Earp, B.E.; Blazar, P. Surgical Demographics of Carpal Tunnel Syndrome and Cubital Tunnel Syndrome Over 5 Years at a Single Institution. J. Hand Surg. Am. 2017, 42, 929 e1–929 e8. [Google Scholar] [CrossRef]
- Law, H.Z.; Amirlak, B.; Cheng, J.; Sammer, D.M. An Association between Carpal Tunnel Syndrome and Migraine Headaches-National Health Interview Survey 2010. Plast. Reconstr. Surg. Glob. Open 2015, 3, e333. [Google Scholar] [CrossRef] [PubMed]
- Bland, J.D.; Rudolfer, S.M. Ultrasound imaging of the median nerve as a prognostic factor for carpal tunnel decompression. Muscle Nerve 2014, 49, 741–744. [Google Scholar] [CrossRef] [PubMed]
- Bae, J.Y.; Kim, J.K.; Yoon, J.O.; Kim, J.H.; Ho, B.C. Preoperative predictors of patient satisfaction after carpal tunnel release. Orthop. Traumatol. Surg. Res. 2018, 104, 907–909. [Google Scholar] [CrossRef]
- Fakhouri, F.; Alsukhni, R.A.; Altunbi, B.; Hawoot, Z.; Dabbagh, R. Factors Correlated with Unfavorable Outcome after Carpal Tunnel Release Surgery. Asian J. Neurosurg. 2017, 12, 670–673. [Google Scholar] [CrossRef] [PubMed]
- Hobby, J.L.; Venkatesh, R.; Motkur, P. The effect of age and gender upon symptoms and surgical outcomes in carpal tunnel syndrome. J. Hand Surg. Br. 2005, 30, 599–604. [Google Scholar] [CrossRef] [PubMed]
- English, J.H.; Gwynne-Jones, D.P. Incidence of Carpal Tunnel Syndrome Requiring Surgical Decompression: A 10.5-Year Review of 2,309 Patients. J. Hand Surg. Am. 2015, 40, 2427–2434. [Google Scholar] [CrossRef]
- Roh, Y.H.; Chung, M.S.; Baek, G.H.; Lee, Y.H.; Rhee, S.H.; Gong, H.S. Incidence of clinically diagnosed and surgically treated carpal tunnel syndrome in Korea. J. Hand Surg. Am. 2010, 35, 1410–1417. [Google Scholar] [CrossRef]
- Ghasemi, M.; Rezaee, M.; Chavoshi, F.; Mojtahed, M.; Shams Koushki, E. Carpal tunnel syndrome: The role of occupational factors among 906 workers. Trauma Mon. 2012, 17, 296–300. [Google Scholar] [CrossRef] [Green Version]
- Bongers, F.J.; Schellevis, F.G.; van den Bosch, W.J.; van der Zee, J. Carpal tunnel syndrome in general practice (1987 and 2001): Incidence and the role of occupational and non-occupational factors. Br. J. Gen. Pract. 2007, 57, 36–39. [Google Scholar]
- Mattioli, S.; Baldasseroni, A.; Curti, S.; Cooke, R.M.; Mandes, A.; Zanardi, F.; Farioli, A.; Buiatti, E.; Campo, G.; Violante, F.S. Incidence rates of surgically treated idiopathic carpal tunnel syndrome in blue- and white-collar workers and housewives in Tuscany, Italy. Occup. Environ. Med. 2009, 66, 299–304. [Google Scholar] [CrossRef] [Green Version]
- Ibrahim, T.; Majid, I.; Clarke, M.; Kershaw, C.J. Outcome of carpal tunnel decompression: The influence of age, gender, and occupation. Int. Orthop. 2009, 33, 1305–1309. [Google Scholar] [CrossRef] [Green Version]
- Mondelli, M.; Grippo, A.; Mariani, M.; Baldasseroni, A.; Ansuini, R.; Ballerini, M.; Bandinelli, C.; Graziani, M.; Luongo, F.; Mancini, R.; et al. Carpal tunnel syndrome and ulnar neuropathy at the elbow in floor cleaners. Neurophysiol. Clin. 2006, 36, 245–253. [Google Scholar] [CrossRef]
- Rosecrance, J.C.; Cook, T.M.; Anton, D.C.; Merlino, L.A. Carpal tunnel syndrome among apprentice construction workers. Am. J. Ind. Med. 2002, 42, 107–116. [Google Scholar] [CrossRef]
- Cosgrove, J.L.; Chase, P.M.; Mast, N.J.; Reeves, R. Carpal tunnel syndrome in railroad workers. Am. J. Phys. Med. Rehabil. 2002, 81, 101–107. [Google Scholar] [CrossRef] [PubMed]
- Nathan, P.A.; Meadows, K.D.; Istvan, J.A. Predictors of carpal tunnel syndrome: An 11-year study of industrial workers. J. Hand Surg. Am. 2002, 27, 644–651. [Google Scholar] [CrossRef] [PubMed]
- Wolf, J.M.; Mountcastle, S.; Owens, B.D. Incidence of carpal tunnel syndrome in the US military population. Hand 2009, 4, 289–293. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harris-Adamson, C.; Eisen, E.A.; Dale, A.M.; Evanoff, B.; Hegmann, K.T.; Thiese, M.S.; Kapellusch, J.M.; Garg, A.; Burt, S.; Bao, S.; et al. Personal and workplace psychosocial risk factors for carpal tunnel syndrome: A pooled study cohort. Occup. Environ. Med. 2013, 70, 529–537. [Google Scholar] [CrossRef] [PubMed]
- Mohammad, W.S. Work-related risk factors for Carpal Tunnel Syndrome among Majmaah University female touchscreen users. Pak. J. Med. Sci. 2019, 35, 1221–1226. [Google Scholar] [CrossRef] [Green Version]
- Mondelli, M.; Aprile, I.; Ballerini, M.; Ginanneschi, F.; Reale, F.; Romano, C.; Rossi, S.; Padua, L. Sex differences in carpal tunnel syndrome: Comparison of surgical and non-surgical populations. Eur. J. Neurol. 2005, 12, 976–983. [Google Scholar] [CrossRef]
- do Amaral e Castro, A.; Skare, T.L.; Nassif, P.A.; Sakuma, A.K.; Barros, W.H. Sonographic diagnosis of carpal tunnel syndrome: A study in 200 hospital workers. Radiol. Bras. 2015, 48, 287–291. [Google Scholar] [CrossRef] [Green Version]
- Jerosch-Herold, C.; Houghton, J.; Blake, J.; Shaikh, A.; Wilson, E.C.; Shepstone, L. Association of psychological distress, quality of life and costs with carpal tunnel syndrome severity: A cross-sectional analysis of the PALMS cohort. BMJ Open 2017, 7, e017732. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Day, C.S.; Makhni, E.C.; Mejia, E.; Lage, D.E.; Rozental, T.D. Carpal and cubital tunnel syndrome: Who gets surgery? Clin. Orthop. Relat. Res. 2010, 468, 1796–1803. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harada, K.; Nakashima, H.; Teramoto, K.; Nagai, T.; Hoshino, S.; Yonemitsu, H. Trigger Digits-Associated Carpal Tunnel Syndrome: Relationship Between Carpal Tunnel Release and Trigger Digits. Hand Surg. 2005, 10, 205–208. [Google Scholar] [CrossRef] [PubMed]
- McCabe, S.J.; Gupta, A.; Tate, D.E.; Myers, J. Preferred sleep position on the side is associated with carpal tunnel syndrome. Hand 2011, 6, 132–137. [Google Scholar] [CrossRef] [Green Version]
- Kwon, B.C.; Jung, K.I.; Baek, G.H. Comparison of sonography and electrodiagnostic testing in the diagnosis of carpal tunnel syndrome. J. Hand Surg. Am. 2008, 33, 65–71. [Google Scholar] [CrossRef]
- Al Rouq, F.; Ahmed, T.S.; Meo, I.M.U.; Al-Drees, A.M.; Meo, S.A. Distribution of clinical symptoms in carpal tunnel syndrome. J. Coll. Physicians Surg. Pak. 2014, 1, 30–33. [Google Scholar]
- Saeed, M.A.; Irshad, M. Seasonal variation and demographical characteristics of carpal tunnel syndrome in a Pakistani population. J. Coll. Physicians Surg. Pak. 2010, 12, 798–801. [Google Scholar]
- Chan, L.; Turner, J.A.; Comstock, B.A.; Levenson, L.M.; Hollingworth, W.; Heagerty, P.J.; Kliot, M.; Jarvik, J.G. The relationship between electrodiagnostic findings and patient symptoms and function in carpal tunnel syndrome. Arch. Phys. Med. Rehabil. 2007, 88, 19–24. [Google Scholar] [CrossRef]



| Study | Influence Factors | Design Sample Size | p-Value | Effect Estimate | Related with CTS |
|---|---|---|---|---|---|
| Zyluk et al. [9] | Age | 386 patients with CTS | Total grip strength: p = 0.05 Key pinch strength: p = 0.18 | Total grip strength (%) ≤40 years: 138 (44) 41–65 years: 106 (53) >65 years: 87 (27) Key pinch strength: ≤40 years: 122 (43) 41–65 years: 102 (36) >65 years: 93 (22) | Yes |
| Porter et al. [10] | Age | Prospective study 87 patients with carpal tunnel decompression | Symptom severity score ≤50 years improvement: 1.60 >60 years improvement: 0.90 Functional status score ≤50 years improvement: 0.86 >60 years improvement: 0.49 | Yes | |
| Moschovos et al. [13] | Age | Case-control study 433 patients 92 healthy individuals | Age ≥65 years (moderate and severe CTS): p < 0.01 | c-statistic (95%CI) Cross-sectional area <65 years: 0.94 (0.92–0.97) ≥65 years: 0.85 (0.78–0.92) Wrist to forearm ratio <65 years: 0.96 (0.93–0.99) ≥65 years: 0.86 (0.79–0.94) | Yes |
| Hansen and Larsen [11] | Age (patient >65 year at risk) | 101 patients | p = 0.001 | OR (95% CI): 17.85 (3.47–91.87) | Yes |
| Haghighat et al. [12] | Ages > 55 | Cross-sectional descriptive study 240 dentists | Prevalence of CTS: 22.2% | Yes | |
| Wilgis et al. [14] | Age | Prospective assessment 490 patients | Tinel’s sign: p = 0.001 Phalen´s test: p < 0.001 Semmes–Weinstein test: p < 0.001 Symptom status scores: p < 0.001 | Tinel’s sign Prior to surgery: 68% positive After surgery: 32% positive Phalen´s test Prior to surgery: 89% positive After surgery: 11% positive Semmes–Weinstein test Prior to surgery: 2.4 ± 0.05 points After surgery: 1.97 ± 0.04 points Symptom status scores (average) Prior to surgery: 2.8 ± 0.04 After surgery: 1.1 ± 0.04 | Yes |
| de Saboya et al. [15] | Age (continuous) | 205 participants 285 hands with CTS diagnosed | |||
| Ozcakir et al. [16] | BMI | 27 patients with CTS symptoms 27 controls | |||
| Sharifi et al. [17] | BMI | 131 patients with CTS symptoms 131 controls | p < 0.001 | OR (95% CI): 1.323, correlation coefficient: r = 0.280 | |
| Ünaldı et al. [18] | BMI | 100 patients with CTS 100 healthy volunteers | p < 0.001 | Correlation coefficient CTS and BMI r = 0.285 | Yes |
| Kurt et al. [19] | BMI | 126 patients with BMI ≥ 30 | |||
| Landau et al. [20] | BMI | 50 patients with ulnar neuropathy at the elbow diagnosis 50 patients with CTS 50 control subjects | p = 0.007 | Positive correlation between BMI and ulnar nerve conduction velocity: r2 = 0.22 | Yes |
| Hassan et al. [21] | BMI | 120 patients with CTS symptoms | BMI and recurrence group: p < 0.0001 | Recurrent group mean values BMI: 43.8, motor distal latency: 6.85 non-recurrent group mean values BMI: 37.99 motor distal latency: 5.4 | Yes |
| Bodavula et al. [22] | BMI and sex | Prospective, longitudinal outcome study 598 cases (hands) with CTS diagnosed | |||
| Mansoor et al. [23] | BMI | Cross-sectional survey 112 patients | Frequency of obesity: 34% | ||
| Aygül et al. [24] | BMI | 92 patients with CTS 30 healthy subjects | p = 0.011 | Positive correlation between BMI and median motor distal latency: r = 0.20 | Yes |
| Kim et al. [26] | BMI | 15 players of wheelchair basketball | p = 0.04 | Average BMI of subjects with CTS (26.0 kg/m2) was greater than normal subjects (23.4 kg/m2) | Yes |
| Kouyoumdijan et al. [25] | BMI | 141 patients with CTS | p < 0.001 | Yes | |
| Nageeb et al. [27] | BMI and vitamin D | 50 CTS patients 50 controls | p = 0.01 | Correlation coefficient between BMI and vitamin D: r = −54 | Yes |
| Shiri et al. [28] | Obesity | Cross-sectional study 6254 participants | OR (95% CI): 2.4 (1.1–5.4) | Yes | |
| Tang et al. [29] | Dominant hand | 87 patients with bilateral CTS | |||
| McDiarmid et al. [30] | Sex | 29,937 CTS cases | CTS rate for data entry keyers Male: 1.17 Female: 1.10 | Yes | |
| Roquealure et al. [31] | Sex | 1168 participants | OR (95% CI): Higher PAF in male blue-collar workers: 50% (41–57) Higher PAF in female white-collar workers: 24% (19–29) | ||
| Giersiepen et al. [32] | BMI | Case–control study 808 participants with first surgery for CTS | OR (95% CI): 1.13 (1.06–1.20) | Yes | |
| Çirakli et al. [33] | Age and sex | 2516 patients with CTS symptoms | |||
| Sassi and Giddins [34] | Sex | 100 participants | Mean relative cross-sectional area (smaller in women than men): p < 0.05 | Yes | |
| El-Helaly et al. [35] | Sex | Cross-sectional study 279 laboratory technicians | CTS prevalence: 9.7% | Yes | |
| Gruber et al. [36] | Sex | Retrospective study 170 cases | |||
| Arslan et al. [37] | Age and BMI | 165 subjects with pre-diagnosis of CTS | Age: p = 0.60 BMI: p = 0.01 | OR (95% CI) Age: 0.96 (0.85–1.09) BMI: 0.59 (0.39–0.91) | Yes |
| Boz et al. [38] | BMI | Prospective study 198 CTS patients 194 control subjects | |||
| Mondelli et al. [39] | BMI | Case–control study 340 patients with CTS 747 patients without CTS | |||
| Kouyoumdijan et al. [40] | Age and BMI | 210 symptomatic CTS patients 320 controls subjects | p < 0.001 | OR (95% CI) BMI: 1.11 (1.05–1.16) | Yes |
| Hiebs et al. [41] | BMI | 50 patients with CTS 50 controls | Yes | ||
| Thiese et al. [42] | Age, BMI, and sex | 295 untreated CTS patients 50 healthy volunteers | Age: p < 0.0001 BMI: p < 0.005 | Adjusted prevalence ratio Age: 1.04 (1.02–1.06) BMI: 2.67 (1.50–4.85) Female sex: 1.39 (0.84–2.29) | Yes |
| Moghtaderi et al. [43] | BMI and sex | Case–control study 128 CTS patients 109 controls | BMI: p = 0.000 Sex: p = 0.001 | OR (95% CI) BMI: 1.75 (1.50–2.04) Sex: 9.95 (2.46–40.17) | Yes |
| Komurcu et al. [7] | Age and BMI | 547 patients | Age: p = 0.001 | OR (95% CI) Age ≥ 65: (1.86–9.35) | Yes |
| Iwuagwu et al. [44] | Age | 31 patients with macromastia and CTS | Yes | ||
| Sousa et al. [45] | BMI and sex | Cross-sectional study 115 idiopathic CTS patients 115 controls | |||
| Zambelis et al. [46] | Older age and higher BMI | 130 subjects with CTS only, or mainly, in the left hand 130 subjects with CTS only, or mainly, in the right hand. | Age: p = 0.006 BMI: p = 0.004 | OR (95% CI) Age: 1.03 (1.01–1.05) BMI: 1.09 (1.03–1.15) | Yes |
| Becker et al. [47] | Age, BMI, and sex | 791 CTS cases 981 controls | p < 0.001 | OR (95% CI) Age (41–60): 1.91 (1.58–2.31) BMI > 30: 2.90 (2.25–3.73) Female: 3.66 (2.84–4.71) | Yes |
| Kame et al. [48] | BMI | Cross-sectional study 36 patients | p = 0.03 | CTS prevalence: 16.67% | Yes |
| Geoghegan et al. [49] | BMI | 3391 cases | OR (95% CI): 2.06 (1.79–2.38) | Yes | |
| Solmaz et al. [50] | Age and sex | Electrodiagnostic study 295 untreated CTS patients 50 patients with no risk factor (idiopathic) 50 healthy volunteers | |||
| Zhang et al. [51] | Age, BMI, and sex | Retrospective cohort study 1114 patients with CTR 264 patients with cubital tunnel surgery 76 patients with both | p < 0.05 | OR (95% CI) Age: 1.02 (1.00–1.04) BMI: 1.01 (0.97–1.05) Sex: 2.18 (1.34–3.55) | Yes |
| Law et al. [52] | Age, BMI, and sex | Interview survey 25,880 respondents (952 with CTS) | OR (95% CI) Age ≥ 65: 18% (15.0%–20.9%) Women: 66.5% (62.8%–70.3%) Obese: 42.9% (39.1%–46.7%) | Yes | |
| Bland et al. [53] | BMI and sex | Observational study 145 patients with carpal tunnel decompressions | BMI: p < 0.05 Sex: p = 0.05 | Correlation between SSS and BMI r = −0.16 Mean change in SSS Women = −1.77 Men = −1.42 | |
| Bae et al. [54] | Age | Retrospective study 60 patients diagnosed with idiopathic CTS | p = 0.001 | OR (95% CI): 0.922 (0.877–0.969) | Yes |
| Fakhauri et al. [55] | Sex | 620 patients with CTS | |||
| Hobby et al. [56] | Age and sex | 97 patients with CTS | Age > 70 Symptom scale Preoperative: 3.05, Postoperative: 1.64 Function scale Preoperative: 2.88, Postoperative: 1.99 Male Symptom scale Preoperative: 2.65 Function scale Preoperative: 1.99 Female Symptom scale Preoperative: 3.08 Function scale Preoperative: 2.70 | Yes | |
| English et al. [57] | Age | Retrospective study 2313 patients with carpal tunnel decompression | Highest rates of carpal tunnel decompression 307 per 100,000 person-years (70–79 year age group) | Yes | |
| Roh et al. [58] | Sex | Retrospective, nationwide cohort study Population of Korea during 2005–2007 | Incidence rate ratio Male CTS diagnosed: 2.76 (2.74–2.78) Female CTS diagnosed: 7.12 (7.11–7.13) | ||
| Ghasemi et al. [59] | BMI | Descriptive cross-sectional study 906 cases | CTS prevalence Men: 14% Women: 8.9% | ||
| Bongers et al. [60] | Age and sex | 355,201 listed patients in 1987 364,998 listed patients in 2001 | Crude incidence rate 1.3 per 1000 (95% CI: 1.0 to 1.5) in 1987 1.8 per 1000 (95% CI: 1.7 to 2.0) in 2001. Males 0.6(95% CI: 0.5 to 0.7) in 1987 0.9 (95% CI: 0.8 to 1.0) in 2001 Females 1.9 (95% CI: 1.7 to 2.1) in 1987 2.8 (95% CI: 2.6 to 3.1) in 2001 | Yes | |
| Mattioli et al. [61] | Sex | 8801 cases | |||
| Ibrahim et al. [62] | Age and sex | 479 patients | |||
| Mondelli et al. [63] | Age, BMI, and sex | 179 cleaners | OR (95% CI) older age: 3.82 (1.43–10.22) BMI: 1.79 (0.85–3.78) | Yes | |
| Rosecrance et al. [64] | Age & BMI | Cross-sectional study 1142 participants | p < 0.0001 | OR (95% CI) Age: 4.9 (2.40–10.02) BMI: 4.12 (2.10–8.08) CTS prevalence: 8.2% | Yes |
| Cosgrove et al. [65] | Age and BMI | 900 subjects | Age and BMI: p < 0.001 | Unstandardized coefficient Age: 0.01361 BMI: 0.04765 | Yes |
| Nathan et al. [66] | Age, BMI, and sex | 256 participants without CTS | Age: p = 0.001 Sex: p = 0.02 BMI: p = 0.04 | OR (95% CI) Age ≥ 50: 6.58 (2.08–20.84) BMI ≥ 28.24: 4.02 (1.02–15.87) Sex: 1.53 (1.06–2.23) | Yes |
| Wolf et al. [67] | Age and sex | 48,957 cases of CTS | OR (95% CI): 11.63 (10.90–12.41) Incidence rate ratio Women: 3.29(3.28–3.35) Age ≥ 40: 11.63 (10.90–12.41) | Yes | |
| Harris-Adamson et al. [68] | Age, BMI, and sex | Pooled study cohort 3515 participants | Women: p = 0.07 Age and BMI: p = 0.00 | HR (95% CI) Women: 1.30 (0.98–1.72) Age ≥ 50: 3.04 (1.96–4.71) BMI ≥ 30 kg/m2: 1.67 (1.26–2.21) | Yes |
| Mohammad [69] | Age, BMI, and female sex | 222 female touchscreen users | CTS prevalence: 34.20% | ||
| Mondelli et al. [70] | Age, BMI, and sex | 172 subjects (non-surgical) 219 patients (surgical) | |||
| do Amaral et al. [71] | Age | 200 hospital workers | p < 0.0001 | OR (95% CI): 1.0 (0.97–1.03) CTS prevalence: 34% | Yes |
| Jerosch-Herold et al. [72] | Age, BMI, and sex | Prospective, multicenter cohort study 753 patients with CTS | p < 0.0001 | Yes | |
| Day et al. [73] | Age and sex | 273 patients (with diagnosis of carpal or cubital tunnel syndrome) | Age (most important predictor of surgical release): p < 0.001 More surgeries performed on male patients: p = 0.004 | Yes | |
| Harada et al. [74] | Age and sex | 875 idiopathic CTS cases | |||
| McCabe et al. [75] | Age, BMI, and sex | Case–control study 68 CTS cases 138 controls | p = 0.05 | OR (95% CI) Women aged < 60: 8.7 (1.9–39.4) | Yes |
| Kwon et al. [76] | Age, BMI, and sex | Prospective, case–control study 29 patients | |||
| Rouq et al. [77] | Age and sex | Cross-sectional observational study 227 subjects with CTS | |||
| Saeed and Irshad [78] | Age and sex | Observational study 213 patients with CTS | |||
| Chan et al. [79] | Age, BMI, and sex | Cross-sectional design 215 patients with CTS |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cazares-Manríquez, M.A.; Wilson, C.C.; Vardasca, R.; García-Alcaraz, J.L.; Olguín-Tiznado, J.E.; López-Barreras, J.A.; García-Rivera, B.R. A Review of Carpal Tunnel Syndrome and Its Association with Age, Body Mass Index, Cardiovascular Risk Factors, Hand Dominance, and Sex. Appl. Sci. 2020, 10, 3488. https://doi.org/10.3390/app10103488
Cazares-Manríquez MA, Wilson CC, Vardasca R, García-Alcaraz JL, Olguín-Tiznado JE, López-Barreras JA, García-Rivera BR. A Review of Carpal Tunnel Syndrome and Its Association with Age, Body Mass Index, Cardiovascular Risk Factors, Hand Dominance, and Sex. Applied Sciences. 2020; 10(10):3488. https://doi.org/10.3390/app10103488
Chicago/Turabian StyleCazares-Manríquez, Melissa Airem, Claudia Camargo Wilson, Ricardo Vardasca, Jorge Luis García-Alcaraz, Jesús Everardo Olguín-Tiznado, Juan Andrés López-Barreras, and Blanca Rosa García-Rivera. 2020. "A Review of Carpal Tunnel Syndrome and Its Association with Age, Body Mass Index, Cardiovascular Risk Factors, Hand Dominance, and Sex" Applied Sciences 10, no. 10: 3488. https://doi.org/10.3390/app10103488
APA StyleCazares-Manríquez, M. A., Wilson, C. C., Vardasca, R., García-Alcaraz, J. L., Olguín-Tiznado, J. E., López-Barreras, J. A., & García-Rivera, B. R. (2020). A Review of Carpal Tunnel Syndrome and Its Association with Age, Body Mass Index, Cardiovascular Risk Factors, Hand Dominance, and Sex. Applied Sciences, 10(10), 3488. https://doi.org/10.3390/app10103488











