The Synergy Tool: Making Important Quality Gains within One Healthcare Organization
Abstract
:1. Introduction
When Did We Begin Our Journey?
2. Materials and Methods
3. Results
3.1. Spider Charts of Typical Patient Profiles by Site
3.2. Nurse Perceptions of Workload Management
3.3. Staff Experience
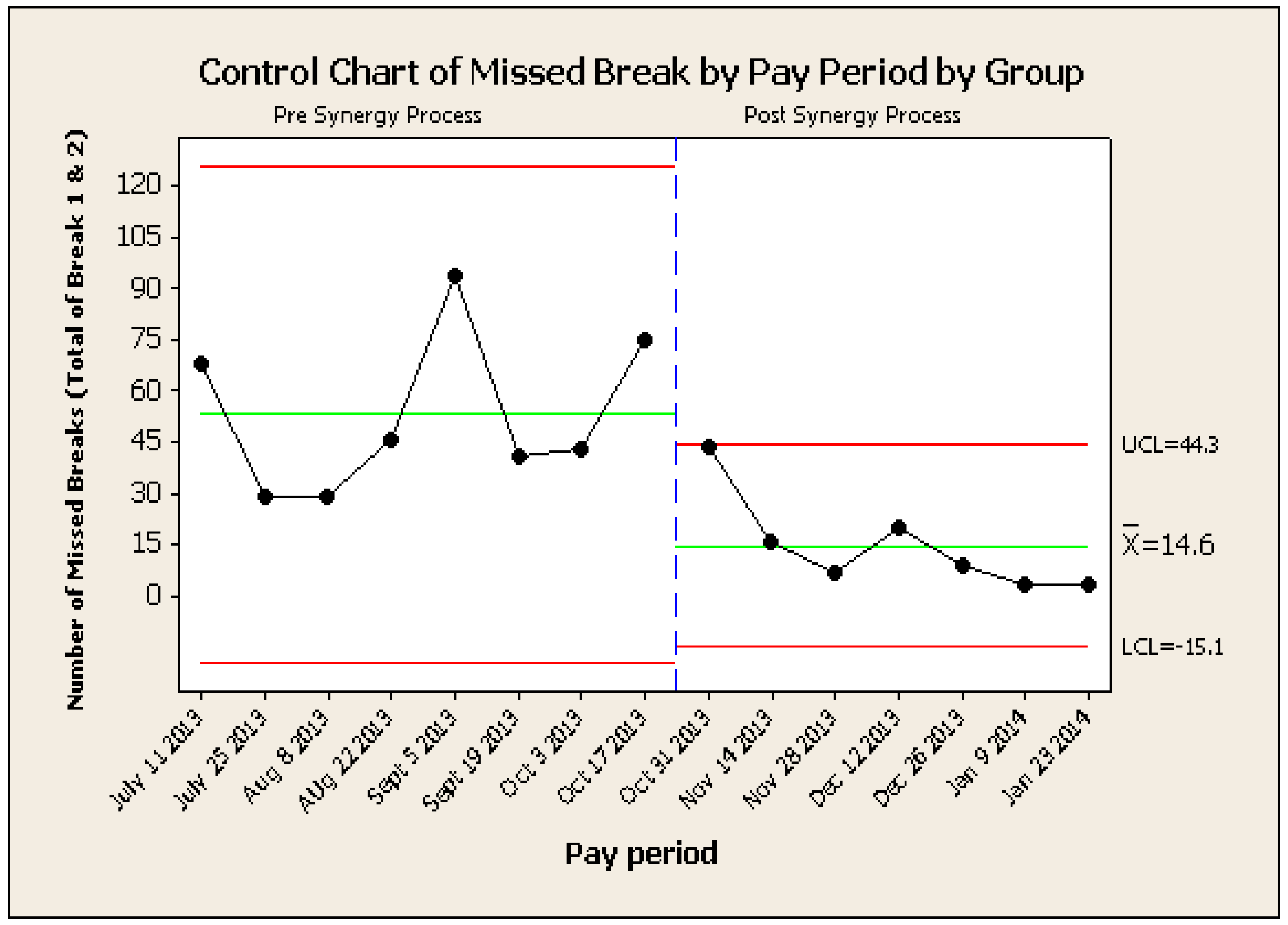
3.4. Nurses’ Missed Breaks
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Appendix A
| Activity | Timeline |
|---|---|
| Plan (Identify Problem, Gather Data, Interpret Data) | |
| Group kick off meeting | Week 1 |
| Revise staff surveys | Week 1 |
| Staff engagement and communication | Week 1–2 |
Data collection: baseline data
| Week 3 |
| Patient characteristic tool development (including face and construct validity) | Week 3 |
| Do (Act on Evidence) | |
| Training of nurses on patient scoring | Week 5 |
| Pilot patient characteristic tool for 2 weeks | Weeks 6 & 7 |
| Study (Evaluate Results) | |
| Analyze data collected from patient characteristic tool | Week 8 |
| Analyze baseline data and correlate with patient characteristic tool | Week 8 |
| Develop staffing guidelines | Week 9 |
| Act (Identify and Implement Next Steps) | |
| Charge nurse training for patient assignment | Week 9 |
| Identify changes in unit | Week 9 |
| Go live: Implementation of new process | Week 10 |
| PDSA #2 (one month post implementation) | |
| Data collection Analyze and modify tools, improve staffing guidelines | 2 weeks |
| Identify and implement changes in unit | 2 weeks |
| PDSA #3 (6 months post implementation) | 2 weeks |
References
- Bakker, Arnold B., Wilmar B. Schaufeli, Michael P. Leiter, and Toon W. Taris. 2008. Work engagement: An emerging concept in occupational health psychology. Work & Stress 22: 187–200. [Google Scholar]
- Berwick, Donald M. 1996. A primer on leading the improvement of systems. BMJ: British Medical Journal 312: 619. [Google Scholar] [CrossRef] [PubMed]
- Brewer, Barbara B., Anne W. Wojner-Alexandrov, Nora Triola, Christine Pacini, Melanie Cline, Jo Ellen Rust, and Karlene Kerfoot. 2007. AACN Synergy Model’s characteristics of patients: Psychometric analyses in a tertiary care health system. American Journal of Critical Care 16: 158–67. [Google Scholar] [PubMed]
- Brown, Diane Storer, Nancy Donaldson, Linda Burnes Bolton, and Carolyn E. Aydin. 2010. Nursing-sensitive benchmarks for hospitals to gauge high-reliability performance. Journal for Healthcare Quality 32: 9–17. [Google Scholar] [CrossRef] [PubMed]
- Carter, Kimberly F., and Hilda D. Burnette. 2011. Creating patient-nurse synergy on a medical-surgical unit. MEDSURG Nursing Journal 20: 249–53. [Google Scholar]
- Chambers, John, William Cleveland, Beat Kleiner, and Paul Tukey. 1983. Graphical Methods for Data Analysis. Murray Hill: Wadsworth & Brooks Publishing Company, pp. 158–62. [Google Scholar]
- Curley, Martha A. Q. 2007. Synergy: The Unique Relationship between Nurses and Patients, the AACN Synergy Model for Patient Care. Indianapolis: Sigma Theta Tau International. [Google Scholar]
- Gralton, Karen S., and Stacy A. Brett. 2012. Integrating the Synergy Model for patient care at Children’s Hospital of Wisconsin. Journal of Pediatric Nursing 27: 74–81. [Google Scholar] [CrossRef] [PubMed]
- Holden, Richard J., Matthew C. Scanlon, Neal R. Patel, Rainu Kaushal, Kamisha Escoto, Roger Brown, Samuel J. Alper, Judi M. Arnold, Theresa M. Shalaby, Kathleen Murkowski, and et al. 2011. A human factors framework and study of the effect of nursing workload on patient safety and employee quality of working life. Quality and Safety in Health Care 20: 15–24. [Google Scholar] [CrossRef] [PubMed]
- Khalifehzadeh, Asghar, Mahdi Karimyar Jahromi, and Ahmadreza Yazdannik. 2012. The impact of the Synergy Model on nurses’ performance and the satisfaction of patients with acute coronary syndrome. Iranian Journal of Nursing and Midwifery Research 17: 16–20. [Google Scholar] [PubMed]
- Lowe, Graham. 2012. How employee engagement matters for hospital employment. Healthcare Quarterly (Toronto, Ont.) 15: 29–39. [Google Scholar] [CrossRef]
- MacPhee, Maura, Andrea Wardrop, Cheryl Campbell, and Patricia Wejr. 2011. The Synergy professional practice model and its patient characteristics tool: A staff empowerment strategy. Nursing Leadership (Toronto, Ont.) 24: 42–56. [Google Scholar] [CrossRef]
- MacPhee, Maura, V. Susan Dahinten, and Farinaz Havaei. 2017. The impact of heavy perceived nurse workloads on patient and nurse outcomes. Administrative Sciences 7: 7. [Google Scholar] [CrossRef]
- Mainz, Jan. 2003. Defining and classifying clinical indicators for quality improvement. International Journal for Quality in Health Care 15: 523–30. [Google Scholar] [CrossRef] [PubMed]
- Mawhinney, Lynnette. 2010. Let’s lunch and learn: Professional knowledge sharing in teachers’ lounges and other congregational spaces. Teaching and Teacher Education 26: 972–78. [Google Scholar] [CrossRef]
- Rozdilsky, Janlyn, and Amber Alecxe. 2012. Saskatchewan: Improving patient, nursing and organizational outcomes utilizing formal nurse-patient ratios. Nursing Leadership (Toronto, Ont.) 25: 103–13. [Google Scholar] [CrossRef]
- Schouten, Loes M. T., Marlies E. J. L. Hulscher, Jannes J. E. van Everdingen, Robbert Huijsman, and Richard P. T. M. Grol. 2008. Evidence for the impact of quality improvement collaboratives: Systematic review. BMJ 336: 1491–94. [Google Scholar] [CrossRef] [PubMed]
- Straka, Kristen L., Patricia Brandt, and Jeanne Brytus. 2013. Brief report: Creating a culture of evidence-based practice and nursing research in a pediatric hospital. Journal of Pediatric Nursing 28: 374–78. [Google Scholar] [CrossRef] [PubMed]



| Characteristic | Operational Definition |
|---|---|
| Stability | The ability to maintain a steady state. Stability can be used to describe physiological, psychological, emotional, and family or social stability. |
| Complexity | The intricate interplay of two or more systems, including body, family, and social systems. |
| Predictability | To expect a certain trajectory of illness. While most patients have a predictable course of illness, some individuals do not respond in the typical fashion. |
| Resiliency | The capacity to return to baseline functioning. |
| Vulnerability | Susceptibility to stressors that may adversely affect outcomes: risk of harm to self or others. |
| Participation in Decision-making | The extent to which the patient and/or family can engage in making informed decisions. |
| Participation in Care | The extent to which the patient and/or family participate in care activities. |
| Resource Availability | Patient, family, or community resources to support patient care and well-being (e.g., physiological, social, technical, financial resources). |
| Describe Your Workload | Ideal Work Place | Busy, But Manageable | Busy, Barely Manageable | Unmanageable |
|---|---|---|---|---|
| Pre-implementation (week 1) | 0% | 40% | 40% | 20% |
| Pre-implementation (week 2) | 0% | 50% | 50% | 0% |
| Post-implementation (week 3) | 0% | 100% | 0% | 0% |
| Post-implementation (week 4) | 0% | 64% | 18% | 18% |
| Post-implementation (week 5) | 0% | 100% | 0% | 0% |
| Post-implementation (week 6) | 0% | 100% | 0% | 0% |
| Post-implementation (week 7) | 20% | 0% | 80% | 0% |
| Staff Engagement Survey Results (Percentage of Positive Scores) | PRE SYNERGY N = 37 | POST SYNERGY N = 48 | Chi Square Test |
|---|---|---|---|
| Perception of feeling engaged | 43% | 62% | p < 0.05 |
| Perception of the quality of patient care | 62% | 76% | p < 0.05 |
| Perception of workload and work life balance | 24% | 50% | p < 0.05 |
| Stress Satisfaction Offset Scores | 26% | 56% | p < 0.05 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ho, E.; Principi, E.; Cordon, C.P.; Amenudzie, Y.; Kotwa, K.; Holt, S.; MacPhee, M. The Synergy Tool: Making Important Quality Gains within One Healthcare Organization. Adm. Sci. 2017, 7, 32. https://doi.org/10.3390/admsci7030032
Ho E, Principi E, Cordon CP, Amenudzie Y, Kotwa K, Holt S, MacPhee M. The Synergy Tool: Making Important Quality Gains within One Healthcare Organization. Administrative Sciences. 2017; 7(3):32. https://doi.org/10.3390/admsci7030032
Chicago/Turabian StyleHo, Enoch, Elaine Principi, Charissa P. Cordon, Yayra Amenudzie, Krista Kotwa, Sarah Holt, and Maura MacPhee. 2017. "The Synergy Tool: Making Important Quality Gains within One Healthcare Organization" Administrative Sciences 7, no. 3: 32. https://doi.org/10.3390/admsci7030032
APA StyleHo, E., Principi, E., Cordon, C. P., Amenudzie, Y., Kotwa, K., Holt, S., & MacPhee, M. (2017). The Synergy Tool: Making Important Quality Gains within One Healthcare Organization. Administrative Sciences, 7(3), 32. https://doi.org/10.3390/admsci7030032