Negotiating Autonomy: The Linkages between Intimate Partner Violence, Women’s Paid Work Status and Birth Outcomes
Abstract
1. Introduction
2. Review of Literature
3. Data Source and Study Variables
3.1. Variables Studied
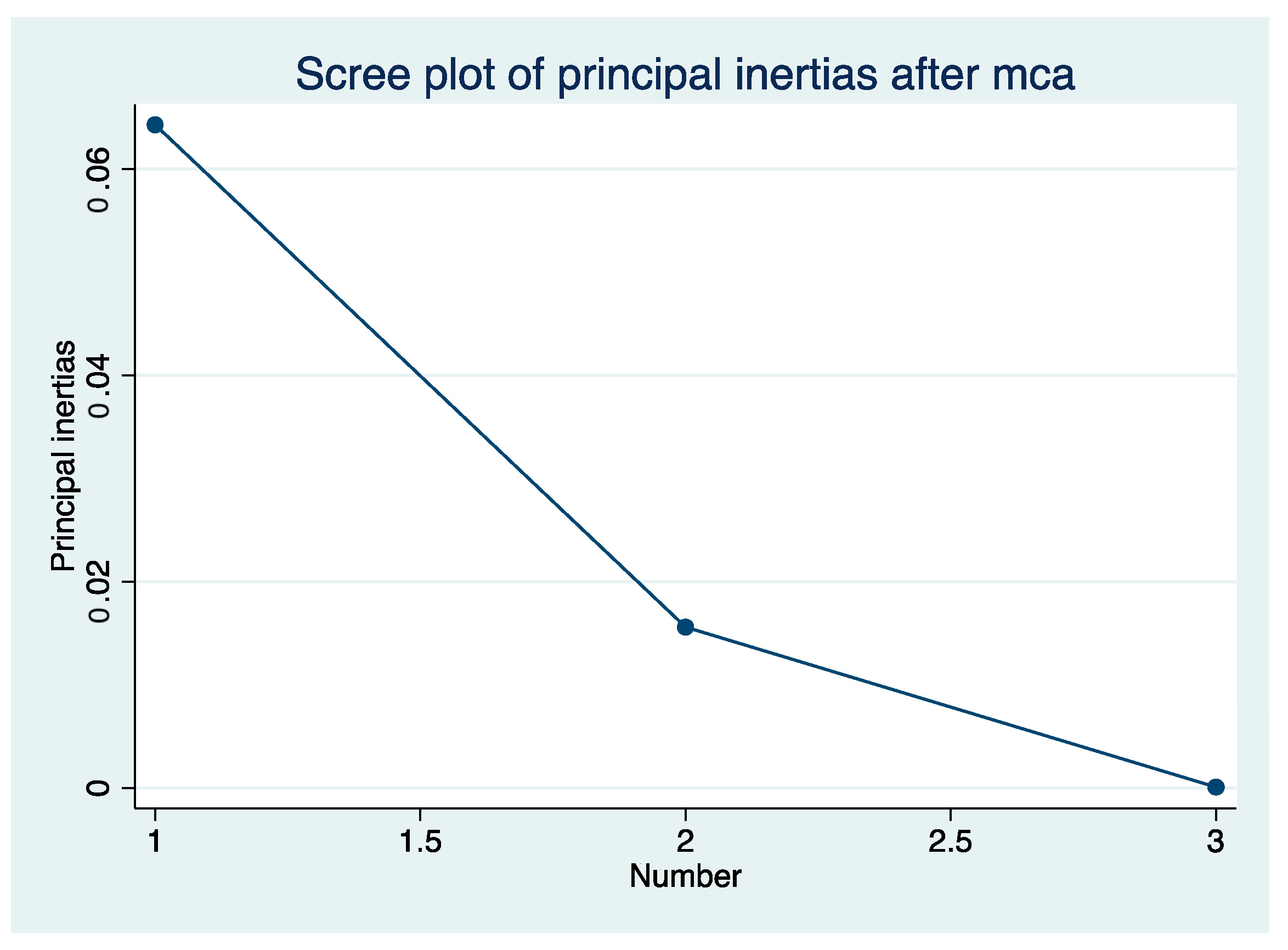
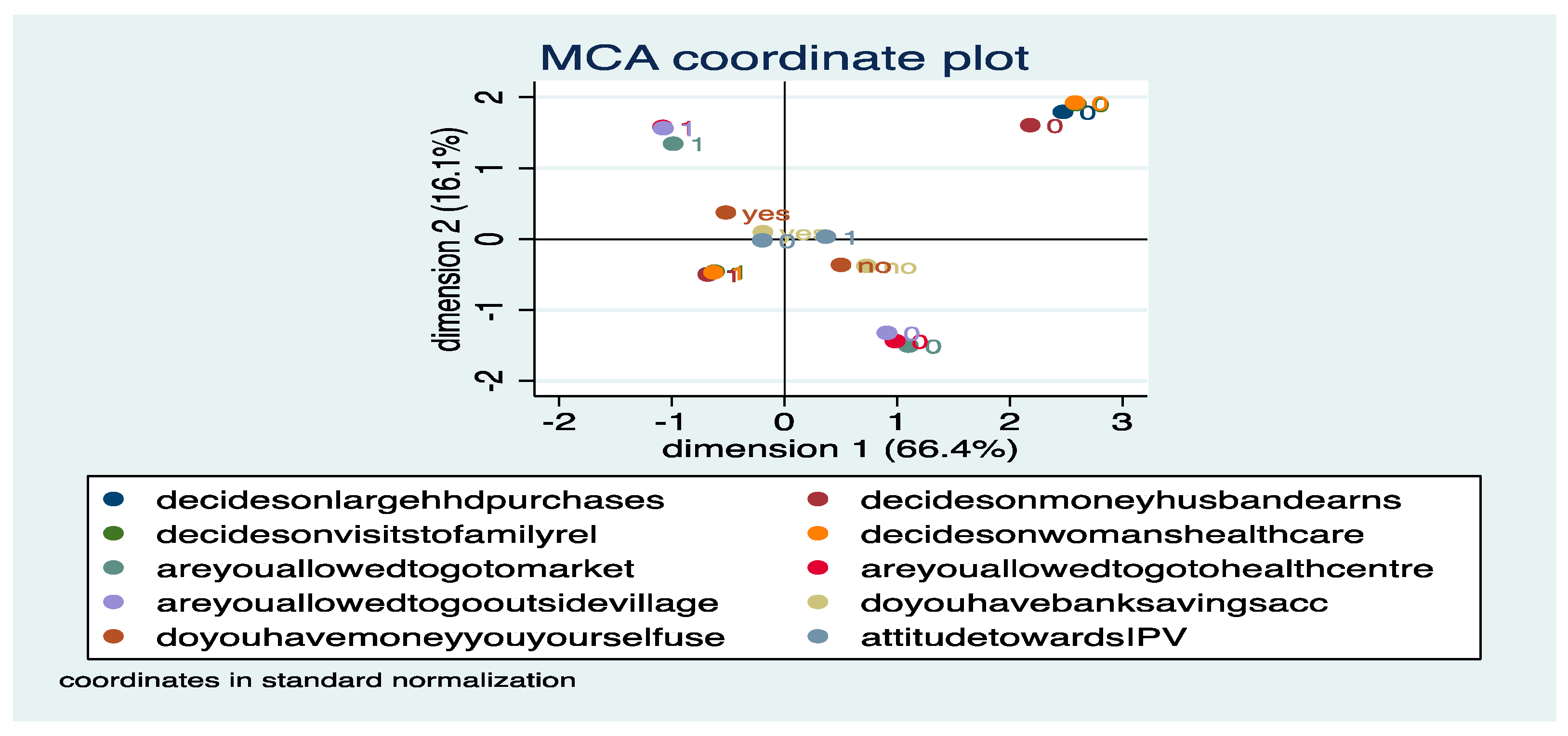
3.1.1. Women’s Autonomy (Autonomy)
3.1.2. Lifetime Experience of Intimate Partner Violence (pofipv)
3.1.3. Marital Controlling Behaviour (mcb)
3.1.4. Working Status of the Respondent (ws)
3.1.5. Residence (res)
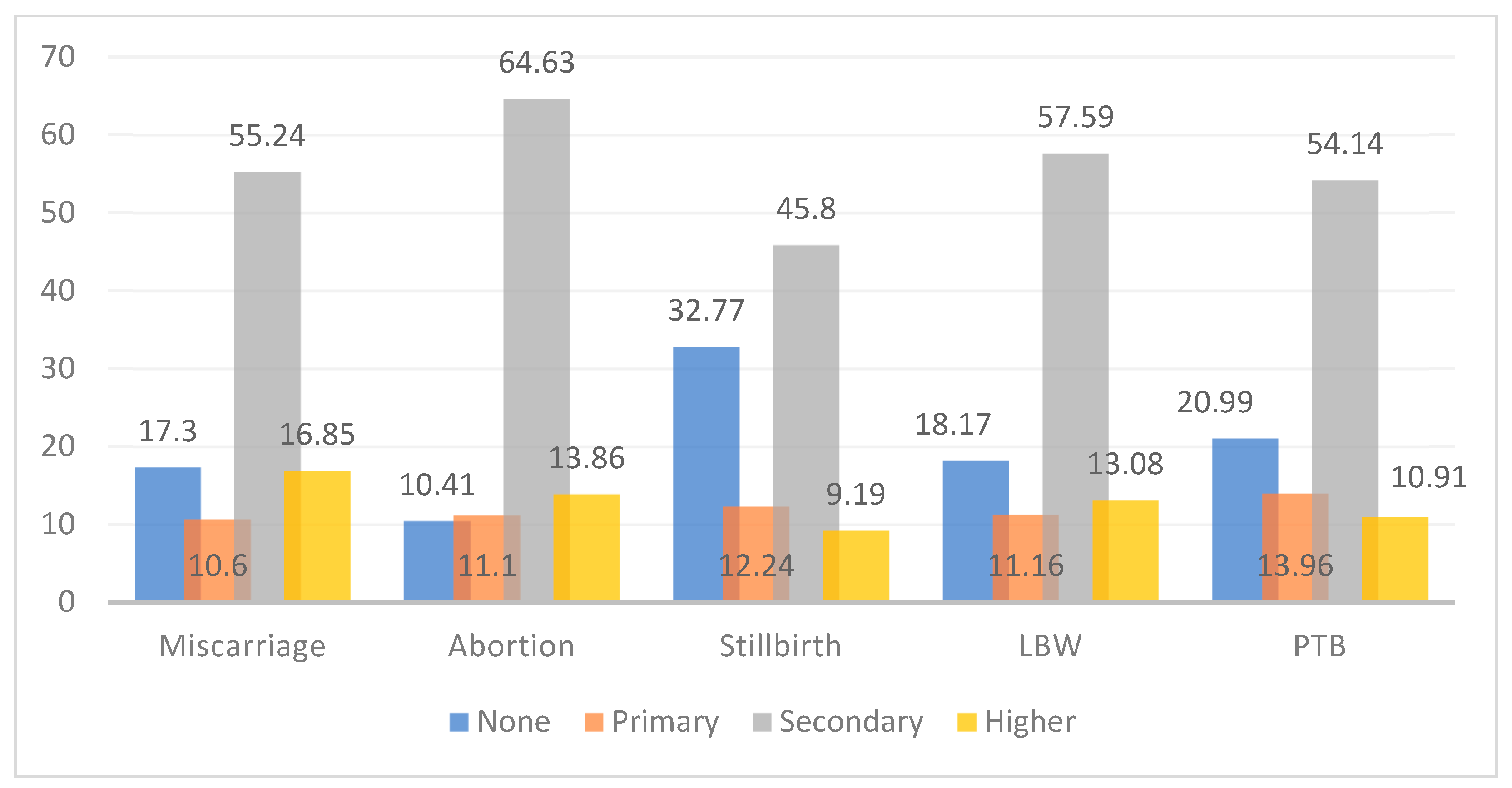
3.1.6. Educational Attainment (educ)
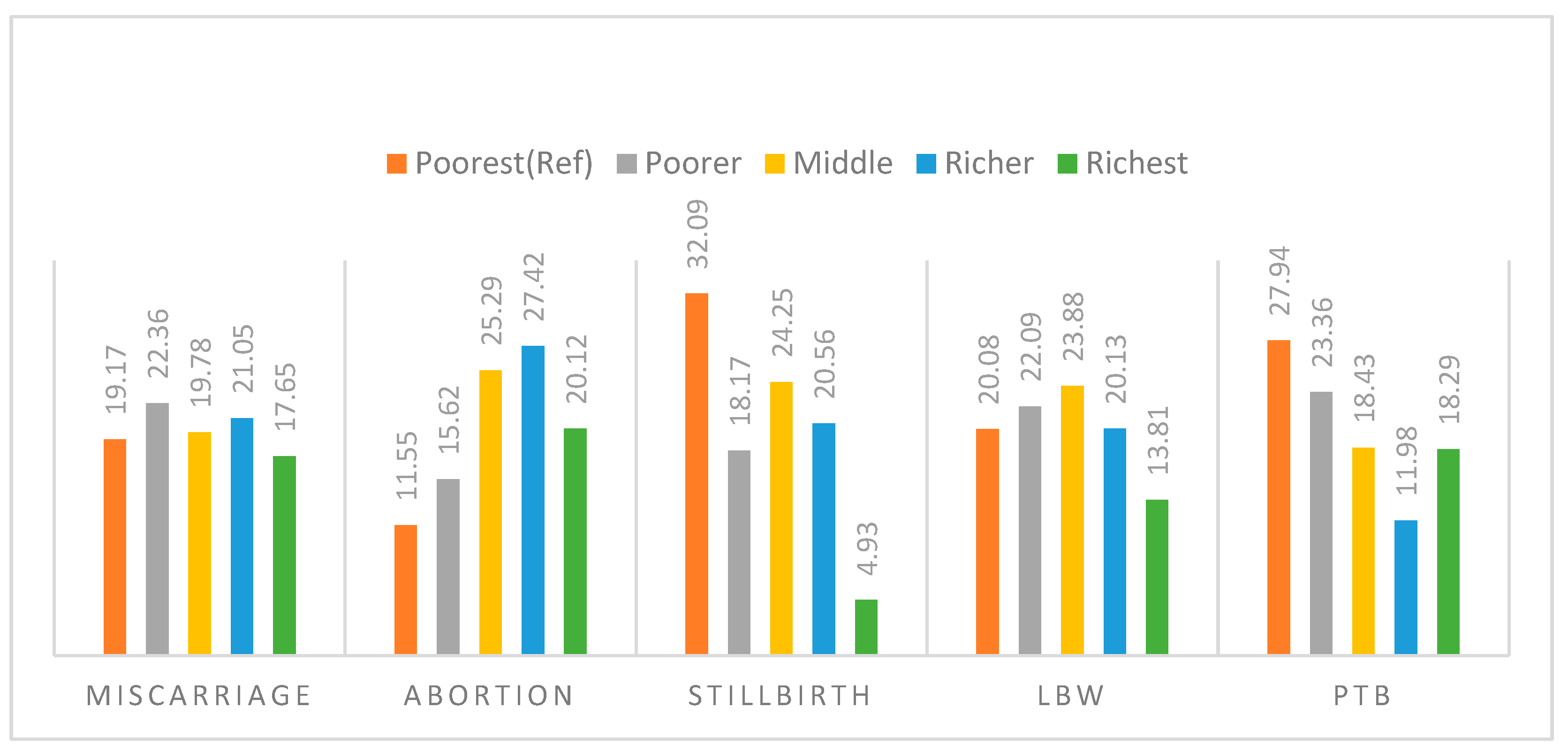
3.1.7. Wealth Index (wi)
3.1.8. Present Age (Agegroup)
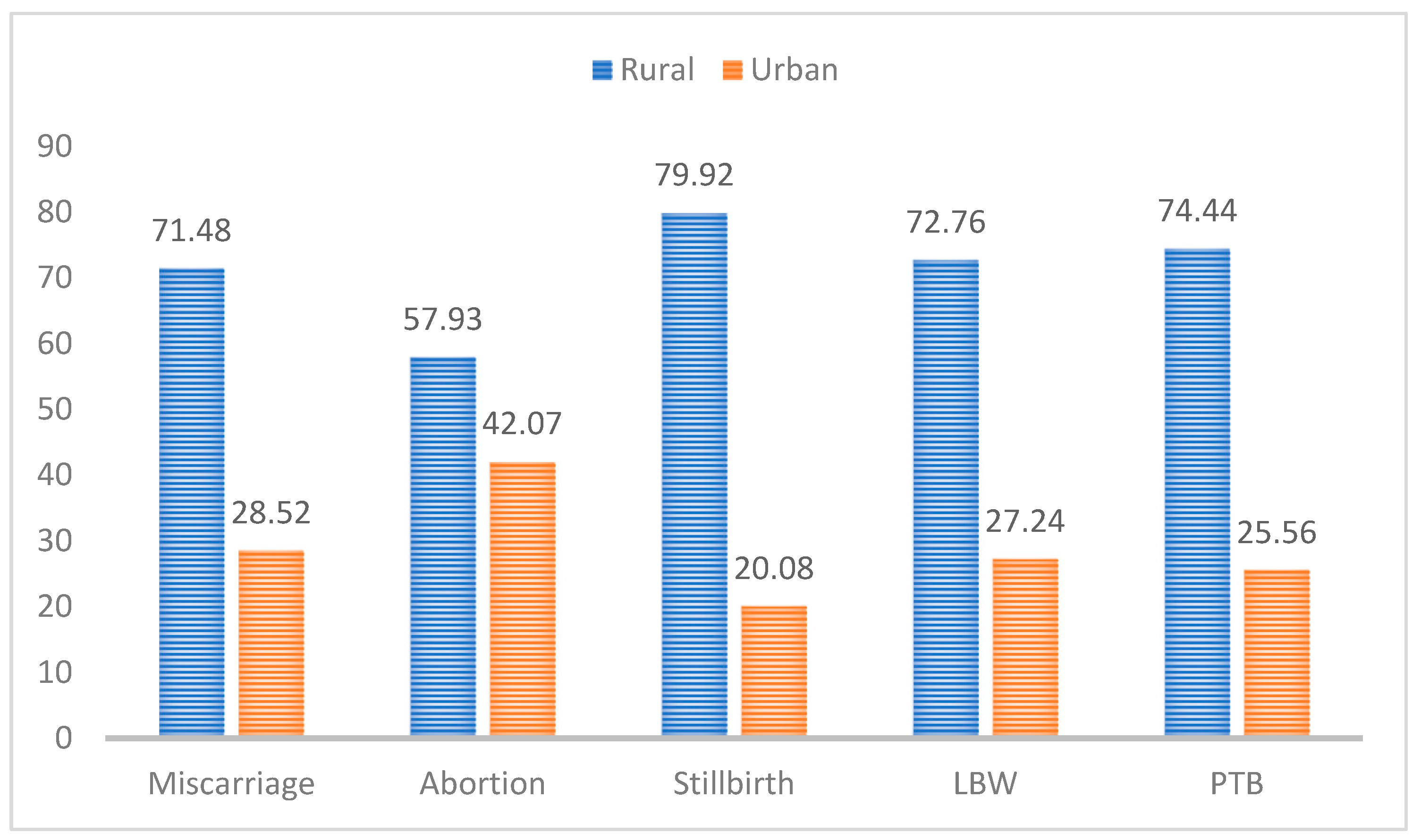
3.2. Patterns of Adverse Birth Outcomes
4. Results and Discussion
5. Robustness Checks
6. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Appendix A
| Adverse Birth Outcome | Woman’s Autonomy | IPV | Working Status | Marital Controlling Behaviour | Residence | Education | Wealth Index | Age Group | |
|---|---|---|---|---|---|---|---|---|---|
| Adverse birth outcome | 1 | ||||||||
| Woman’s autonomy | 0.0035 | 1 | |||||||
| IPV | 0.025 | 0.1305 | 1 | ||||||
| Working status | 0.0125 | −0.0929 | 0.742 | 1 | |||||
| Marital controlling behaviour | 0.0002 | 0.1328 | 0.3936 | 0.0159 | 1 | ||||
| Residence | 0.0017 | 0.0627 | 0.0392 | 0.0572 | 0.0456 | 1 | |||
| Education | 0.0064 | −0.0808 | −0.1255 | −0.0543 | −0.1105 | 0.2147 | 1 | ||
| Wealth index | 0.0023 | −0.04 | −0.1261 | −0.0881 | −0.1115 | 0.4562 | 0.4852 | 1 | |
| Age group | 0.0151 | −0.1187 | 0.0165 | 0.109 | −0.0436 | 0.0656 | −0.124 | 0.047 | 1 |
| 1 | IPV is characterised by derogatory behaviour, acts of physical aggression, sexual coercion, psychological triggers etc., that potentially lead to physical, sexual, and psychological harm in an intimate relationship (Garcia-Moreno et al. 2005). |
| 2 | The extent of the problem can be ascertained from the fact that adverse birth outcomes result in maternal deaths of about 810 women every day, and between 20 and 30 more women suffer short- and long-term disabilities for every such death (Tadese et al. 2022). |
| 3 | For reference, the prevalence of adverse birth outcomes is to the tune of 27.8% in Nepal (Khanal et al. 2016), 29.7% in Sub-Saharan Africa (Tamirat et al. 2021), 15.61% in Zimbabwe (Chaibva et al. 2019), 1/3rd of reproductive-age women in Uganda reported at least one adverse pregnancy outcome (Asiki et al. 2015). |
| 4 | Even though IPV can harm either of the partners, the overwhelming global burden is mostly borne by women (WHO 2012). |
| 5 | The region reports excessively higher poor pregnancy outcomes while maintaining the highest rates of IPV (Devries et al. 2014). |
| 6 | Similar results have been derived in other cross-country analyses as well (Sigalla et al. 2017 for Tanzania; Dhar et al. 2018 for India; Mehari et al. 2020 for Ethiopia). |
| 7 | Similar results have been confirmed in previous studies as Singh et al. (2018); Chandrasekaran et al. (2020). |
References
- Aizer, Anna. 2010. The Gender Wage Gap and Domestic Violence. The American Economic Review 100: 1847–59. [Google Scholar] [CrossRef]
- Alemu, Abebe, Mulatu Abageda, Biruk Assefa, and Getnet Melaku. 2019. Low birth weight: Prevalence and associated factors among newborns at hospitals in Kambata-Tembaro zone, southern Ethiopia 2018. Pan African Medical Journal 34. [Google Scholar] [CrossRef]
- Akerlof, A. George, and Rachel E. Kranton. 2000. Economics and Identity. The Quarterly Journal of Economics 115: 715–53. [Google Scholar] [CrossRef]
- Agarwal, Bina. 1997. “Bargaining’’ and Gender Relations: Within and Beyond the Household. Feminist Economics 3: 1–51. [Google Scholar] [CrossRef]
- Atkinson, Maxine P., Theodore N. Greenstein, and Molly Monahan Lang. 2005. For Women, Breadwinning Can Be Dangerous: Gendered Resource Theory and Wife Abuse. Journal of Marriage and Family 67: 1137–48. [Google Scholar] [CrossRef]
- Asiki, Gershim, Kathy Baisley, Rob Newton, Lena Marions, Janet Seeley, Anatoli Kamali, and Lars Smedman. 2015. Adverse pregnancy outcomes in rural Uganda (1996–2013): Trends and associated factors from serial cross sectional surveys. BMC Pregnancy and Childbirth 15: 1–12. [Google Scholar] [CrossRef] [PubMed]
- Avanigadda, Durga B., and Ravisankar A. Kulasekaran. 2021. Associations between intimate partner violence and pregnancy complications: A cross-sectional study in India. Journal of Family and Community Medicine 28: 17–27. [Google Scholar]
- Babu, Bontha V., and Shantanu K. Kar. 2009. Domestic violence against women in eastern India: A population-based study on prevalence and related issues. BMC Public Health 9: 129. [Google Scholar] [CrossRef]
- Bailey, Beth A. 2010. Partner violence during pregnancy: Prevalence, effects, screening, and management. International Journal of Women’s Health 2: 183–97. [Google Scholar] [CrossRef]
- Beck, Stacy, Daniel Wojdyla, Lale Say, Ana Pilar Betran, Mario Merialdi, Jennifer Harris Requejo, Craig Rubens, Ramkumar Menon, and Paul F. A. Van Look. 2010. The worldwide incidence of preterm birth: A systematic review of maternal mortality and morbidity. Bulletin of the World Health Organization 88: 31–38. [Google Scholar] [CrossRef]
- Blasius, Jorg, and Michael Greenacre, eds. 2014. Visualization and Verbalization of Data, 1st ed. Boca Raton: Chapman and Hall/CRC. [Google Scholar]
- Bloom, Shelah S., David Wypij, and Monica Das Gupta. 2001. Dimensions of women’s autonomy and the influence on maternal health care utilization in a north Indian city. Demography 38: 67–78. [Google Scholar] [CrossRef] [PubMed]
- Bramhankar, Mahadev, and R. S. Reshmi. 2021. Spousal violence against women and its consequences on pregnancy outcomes and reproductive health of women in India. BMC Women’s Health 21: 1–9. [Google Scholar] [CrossRef] [PubMed]
- Campbell, Jacquelyn, Sara Torres, Josephine Ryan, Christine King, Doris W. Campbell, Rebecca Y. Stallings, and Sandra C. Fuchs. 1999. Physical and nonphysical partner abuse and other risk factors for low birth weight among full term and preterm babies: A multi-ethnic case-control study. American Journal of Epidemiology 150: 714–26. [Google Scholar] [CrossRef] [PubMed]
- Chaibva, Blessmore Vimbai, Steve Olorunju, Simon Nyadundu, and Andy Beke. 2019. Adverse pregnancy outcomes, ‘stillbirths and early neonatal deaths’ in Mutare district, Zimbabwe (2014): A descriptive study. BMC Pregnancy and Childbirth 19: 1–7. [Google Scholar] [CrossRef]
- Chandrasekaran, Sruthi, Nadia Diamond-Smith, Karthik Srinivasan, and Suchitra Dalvie. 2020. Preparing for an Increased Need for Abortion Access in India during and after COVID-19: Challenges and Strategies. Studies in Family Planning 51: 377–83. [Google Scholar] [CrossRef]
- Costa, Diogo, E. Hatzidimitriadou, E. Ioannidi-Kapolou, J. Lindert, Joaquim J. Soares, Örjan Sundin, and H. Barros. 2016. Male and female physical intimate partner violence and socio-economic position: A cross-sectional international multicentre study in Europe. Public Health 139: 44–52. [Google Scholar] [CrossRef]
- Dadi, Abel Fekadu, Emma R. Miller, Telake Azale Bisetegn, and Lillian Mwanri. 2020. Global burden of antenatal depression and its association with adverse birth outcomes: An umbrella review. BMC Public Health 20: 1–16. [Google Scholar] [CrossRef]
- Dalal, Koustuv, and Kent Lindqvist. 2012. A national study of the prevalence and correlates of domestic violence among women in India. Asia-Pacific Journal of Public Health 24: 265–77. [Google Scholar] [CrossRef]
- Devries, Karen M., Jennifer C. Child, Loraine J. Bacchus, Joelle Mak, Gail Falder, Kathryn Graham, Charlotte Watts, and Lori Heise. 2014. Intimate partner violence victimization and alcohol consumption in women: A systematic review and meta-analysis. Addiction 109: 379–91. [Google Scholar] [CrossRef]
- Dhanaraj, Sowmya, and Vidya Mahambare. 2021. Male Backlash and Female Guilt: Women’s Employment and Intimate Partner Violence in Urban India. Feminist Economics 28: 170–98. [Google Scholar] [CrossRef]
- Dhar, Diva, Lotus McDougal, Katherine Hay, Yamini Atmavilas, Jay Silverman, Daniel Triplett, and Anita Raj. 2018. Associations between intimate partner violence and reproductive and maternal health outcomes in Bihar, India: A cross-sectional study. Reproductive Health 15: 109. [Google Scholar] [CrossRef]
- Eswaran, Mukesh, and Nisha Malhotra. 2011. Domestic violence and women’s autonomy in developing countries: Theory and evidence. Canadian Journal of Economics/Revue Canadienne D’économique 44: 1222–63. [Google Scholar] [CrossRef]
- Fikree, Fariyal F., and Omrana Pasha. 2004. Role of gender in health disparity: The South Asian context. BMJ (Clinical Research ed.) 328: 823–26. [Google Scholar] [CrossRef] [PubMed]
- Frey, Heather A., and Mark A. Klebanoff. 2016. The epidemiology, etiology, and costs of preterm birth. Seminars in Fetal and Neonatal Medicine 21: 68–73. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Moreno, Claudia, H. A. F. M. Jansen, Mary Ellsberg, Lori Heise, and Charlotte Watts. 2005. WHO Multi-Country Study on Women’s Health and Domestic Violence against Women: Report on the First Results. Geneva: World Health Organization, pp. 55–89. [Google Scholar]
- Ghosh, Arabinda, and Rohini Ghosh. 2020. Maternal health care in India: A reflection of 10 years of National Health Mission on the Indian maternal health scenario. Sexual and Reproductive Healthcare: Official Journal of the Swedish Association of Midwives 25: 100530. [Google Scholar] [CrossRef] [PubMed]
- Goemans, Sophie L., Abhishek Singh, Ajit Kumar Yadav, Lotus McDougal, Anita Raj, and Sarah H. Averbach. 2021. The association between intimate partner violence and recent self-managed abortion in India. AJOG Global Reports 1: 100029. [Google Scholar] [CrossRef]
- Gracia, Enrique, Antonio López-Quílez, Miriam Marco, and Marisol Lila. 2018. Neighborhood characteristics and violence behind closed doors: The spatial overlap of child maltreatment and intimate partner violence. PLoS ONE 13: e0198684. [Google Scholar] [CrossRef]
- Greenacre, Michael, and Jorg Blasius. 2006. Multiple Correspondence Analysis and Related Methods. Boca Raton: Chapman and Hall/CRC. [Google Scholar]
- Islam, Mansura, Md Sabbir Ahmed, and Sabuj Kanti Mistry. 2021. Factors associated with women’s approval on intimate partner violence in Bangladesh: A cross-sectional analysis of latest demographic and health survey 2017–2018. Heliyon 7: e08582. [Google Scholar] [CrossRef] [PubMed]
- Jejeebhoy, Shireen. 2000. Women’s Empowerment and Demographic Processes. In Moving Beyond Cairo. Edited by Harriet B. Presser and G. Sen. New York: Oxford University Press. [Google Scholar]
- Kant, Shashi, Rahul Srivastava, Sanjay Kumar Rai, Puneet Misra, Lena Charlette, and Chandrakant S. Pandav. 2015. Induced abortion in villages of Ballabgarh HDSS: Rates, trends, causes and determinants. Reproductive Health 12: 1–7. [Google Scholar] [CrossRef]
- Karp, Celia, Shannon N. Wood, Hadiza Galadanci, Simon P. Sebina Kibira, Fredrick Makumbi, Elizabeth Omoluabi, and Caroline Moreau. 2020. ‘I am the master key that opens and locks’: Presentation and application of a conceptual framework for women’s and girls’ empowerment in reproductive health. Social Science & Medicine 258: 113086. [Google Scholar]
- Khanal, Vishnu, Rajendra Karkee, Andy H. Lee, and Colin W. Binns. 2016. Adverse obstetric symptoms and rural-urban difference in caesarean delivery in Rupandehi district, Western Nepal: A cohort study. Reproductive Health 13: 17. [Google Scholar] [CrossRef] [PubMed]
- Krishnamoorthy, Yuvaraj, Karthika Ganesh, and Karthiga Vijayakumar. 2020. Physical, emotional and sexual violence faced by spouses in India: Evidence on determinants and help-seeking behaviour from a nationally representative survey. Journal Epidemiology and Community Health 74: 732–40. [Google Scholar] [CrossRef] [PubMed]
- Kumar, Sunil, Anupama Sharma, and Chaoba Kshetrimayum. 2019. Environmental and occupational exposure and female reproductive dysfunction. The Indian Journal of Medical Research 150: 532–45. [Google Scholar] [CrossRef] [PubMed]
- Lee-Rife, Susan M. 2010. Women’s empowerment and reproductive experiences over the life course. Social Science and Medicine 71: 634–42. [Google Scholar] [CrossRef]
- Lin, Li, Ciyoung Lu, Weiqing Chen, Chunrong Li, and Vivian Yawei Guo. 2021. Parity and the risks of adverse birth outcomes: A retrospective study among Chinese. BMC Pregnancy and Childbirth 21: 1–11. [Google Scholar] [CrossRef]
- Luke, Nancy, and Kaivan Munshi. 2011. Women as agents of change: Female income and mobility in India. Journal of Development Economics 94: 1–17. [Google Scholar] [CrossRef]
- Macmillan, Ross, and Rosemary Gartner. 1999. When She Brings Home the Bacon: Labor-Force Participation and the Risk of Spousal Violence against Women. Journal of Marriage and the Family 61: 947. [Google Scholar] [CrossRef]
- Majlesi, Kaveh. 2016. Labor market opportunities and women’s decision making power within households. Journal of Development Economics 119: 34–47. [Google Scholar] [CrossRef]
- Mehari, Mihret-ab A., Hayat Maeruf, Carmen C. Robles, Solomon Woldemariam, Tesfay Adhena, Mussie Mulugeta, Abera Haftu, Hadgay Hagose, and Henok Kumsa. 2020. Advanced maternal age pregnancy and its adverse obstetrical and perinatal outcomes in Ayder comprehensive specialized hospital, Northern Ethiopia, 2017: A comparative cross-sectional study. BMC Pregnancy and Childbirth 20: 60. [Google Scholar] [CrossRef]
- Occean, James R., Nicholas Thomas, Andrew C. Lim, Sharonda M. Lovett, Abimbola Michael-Asalu, and Abraham A. Salinas-Miranda. 2021. Prevalence and Factors Associated with Intimate Partner Violence Among Women in Haiti: Understanding Household, Individual, Partner, and Relationship Characteristics. Journal of Interpersonal Violence 36: 11356–84. [Google Scholar] [CrossRef]
- Pallitto, Christina C., Claudia García-Moreno, Henrica A. Jansen, Lori Heise, Mary Ellsberg, and Charlotte Watts. 2013. Intimate partner violence, abortion, and unintended pregnancy: Results from the WHO Multi-country Study on Women’s Health and Domestic Violence. International Journal of Gynecology and Obstetrics 120: 3–9. [Google Scholar] [CrossRef]
- Rahman, Mostafizur, Helal Uddin, Lutfun Nahar Lata, and Jalal Uddin. 2021. Associations of forms of intimate partner violence with low birth weight in India: Findings from a population-based Survey. The Journal of Maternal-Fetal and Neonatal Medicine 35: 7972–7979. [Google Scholar] [CrossRef] [PubMed]
- Ram, Rajan, Manish Kumar, and Nutan Kumari. 2022. Association between women’s autonomy and unintended pregnancy in India. Clinical Epidemiology and Global Health 15: 101060. [Google Scholar] [CrossRef]
- Rao, Deepa, Shuba Kumar, Rani Mohanraj, Sarah Frey, Lisa E. Manhart, and L. Debra Kaysen. 2016. The impact of domestic violence and depressive symptoms on preterm birth in South India. Social Psychiatry and Psychiatric Epidemiology 51: 225–32. [Google Scholar] [CrossRef]
- Rayhan, Istihak, and Khaleda Akter. 2021. Prevalence and associated factors of intimate partner violence (IPV) against women in Bangladesh amid COVID-19 pandemic. Heliyon 7: e06619. [Google Scholar] [CrossRef] [PubMed]
- Rizkianti, Anissa, Tin Afifah, Ika Saptarini, and Mukhammad Fajar Rakhmadi. 2020. Women’s decision-making autonomy in the household and the use of maternal health services: An Indonesian case study. Midwifery 90: 102816. [Google Scholar] [CrossRef]
- Sanawar, Saifa Binte, Mohammad Amirul Islam, Shankar Majumder, and Farjana Misu. 2018. Women’s Empowerment and Intimate Partner Violence in Bangladesh: Investigating the complex relationship. Journal of Biosocial Science 51: 188–202. [Google Scholar] [CrossRef] [PubMed]
- Sarkar, N. N. 2008. The impact of intimate partner violence on women’s reproductive health and pregnancy outcome. Journal of Obstetrics and Gynaecology 28: 266–71. [Google Scholar] [CrossRef]
- Shome, Suparna, Manoranjan Pal, and Premananda Bharati. 2018. Influence of maternal autonomy and socioeconomic factors on birth weight of infants in India. Malaysian Journal of Nutrition 24: 35–46. [Google Scholar]
- Sigalla, Geofrey N., Declare Mushi, Dan Wolf Meyrowitsch, Rachel Manongi, Jane Januarius Rogathi, Tine Gammeltoft, and Vibeke Rasch. 2017. Intimate partner violence during pregnancy and its association with preterm birth and low birth weight in Tanzania: A prospective cohort study. PLoS ONE 12: e0172540. [Google Scholar] [CrossRef]
- Silverman, Jay G., Sabrina C. Boyce, Nabamallika Dehingia, Namratha Rao, Dharmoo Chandurkar, Priya Nanda, Katherine Hay, Yamini Atmavilas, Niranjan Saggurti, and Anita Raj. 2019. Reproductive coercion in Uttar Pradesh, India: Prevalence and associations with partner violence and reproductive health. SSM–Population Health 9: 100484. [Google Scholar] [CrossRef] [PubMed]
- Singh, Susheela, Chander Shekhar, Rajib Acharya, Ann M. Moore, Melissa Stillman, Manas R. Pradhan, Jennifer J. Frost, Harihar Sahoo, Manoj Alagarajan, Rubina Hussain, and et al. 2018. The incidence of abortion and unintended pregnancy in India, 2015. The Lancet Global Health 6: e111–e120. [Google Scholar] [CrossRef]
- Stephenson, Rob, Apoorva Jadhav, Amy Winter, and Michelle Hindin. 2016. Domestic violence and abortion among rural women in four Indian states. Violence Against Women 22: 1642–58. [Google Scholar] [CrossRef]
- Tadese, Mesfin, Kefyalew Dagne, Abate Dargie Wubetu, Shiferaw Abeway, Alemayehu Bekele, Worku Misganaw Kebede, and Getaneh Baye Mulu. 2022. Assessment of the adverse pregnancy outcomes and its associated factors among deliveries at Debre Berhan Comprehensive Specialized Hospital, Northeast Ethiopia. PLoS ONE 17: e0271287. [Google Scholar] [CrossRef] [PubMed]
- Tamirat, Koku Sisay, Malede Mequanent Sisay, Getayeneh Antehunegn Tesema, and Zemenu Tadesse Tessema. 2021. Determinants of adverse birth outcome in Sub-Saharan Africa: Analysis of recent demographic and health surveys. BMC Public Health 21: 1092. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization WHO. 2011. Putting Women First: Ethical and Safety Recommendations for Research on Domestic Violence against Women. No. WHO/FCH/GWH/01.1. Geneva: WHO. [Google Scholar]
- World Health Organization WHO. 2012. Understanding and Addressing Violence against Women. Available online: https://apps.who.int/iris/handle/10665/77432 (accessed on 23 December 2022).
- World Health Organization WHO. 2018. Global, Regional and National Estimates for Intimate Partner Violence against Women and Global and Regional Estimates for Non-Partner Sexual Violence against Women. UNDP-UNFPA-UNICEF-WHO-World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP) for the United Nations Inter-Agency Working Group on Violence Against Women Estimation and Data. Geneva: World Health Organization. [Google Scholar]
- Yogi, Abinath, K. C. Prakash, and Subas Neupane. 2018. Prevalence and factors associated with abortion and unsafe abortion in Nepal: A nationwide cross-sectional study. BMC Pregnancy and Childbirth 18: 376. [Google Scholar] [CrossRef]
- Yokoe, Ryo, Rachel Rowe, Saswati Sanyal Choudhury, Anjali Rani, Farzana Zahir, and Manisha Nair. 2019. Unsafe abortion and abortion-related death among 1.8 million women in India. BMJ Global Health 4: e001491. [Google Scholar] [CrossRef]
- Zorrilla, Belen, Marisa Pires, Luisa Lasheras, Consuelo Morant, Luis Seoane, Luis M. Sanchez, Maria Durbán, Iñaki Galán, Ramón Aguirre, and Rosa Ramírez. 2010. Intimate partner violence: Last year prevalence and association with socio-economic factors among women in Madrid, Spain. European Journal of Public Health 20: 169–75. [Google Scholar] [CrossRef]

| Variables | Frequency | Percentage |
|---|---|---|
| Birth outcomes | ||
| Non-adverse | 12,834 | 74.25 |
| Adverse | 4452 | 25.75 |
| Total | 17,286 | 100.00 |
| Perpetration of IPV | ||
| No experience of IPV | 12,252 | 70.88 |
| Faced some form of IPV | 5034 | 29.12 |
| Marital controlling behaviour | ||
| No marital control | 9650 | 55.83 |
| Somewhat control | 4866 | 28.15 |
| Full marital control | 2770 | 16.02 |
| Residential site | ||
| Urban | 4029 | 23.31 |
| Rural | 13,257 | 76.69 |
| Educational attainment | ||
| No education | 3628 | 20.99 |
| Primary | 2242 | 12.97 |
| Secondary | 9123 | 52.78 |
| Higher | 2293 | 13.27 |
| Wealth index | ||
| Poorest | 4437 | 25.67 |
| Poorer | 3957 | 22.89 |
| Middle | 3372 | 19.51 |
| Richer | 3103 | 17.95 |
| Richest | 2417 | 13.98 |
| Age group | ||
| 15–19 | 339 | 1.96 |
| 20–24 | 4073 | 23.56 |
| 25–29 | 6649 | 38.46 |
| 30–34 | 3996 | 23.12 |
| 35–39 | 1715 | 9.92 |
| 40–44 | 411 | 2.38 |
| 45–49 | 103 | 0.6 |
| Items | Coding Criteria |
|---|---|
| Decision-Making Power 1. Who decides on the woman’s healthcare? 2. Who decides on large household purchases? 3. Who decides on visits to family or relatives? 4. Who decides what is to be done with the money the respondent’s husband earns? | If answered ‘respondent alone’ or ‘jointly with husband’, it is coded as ‘1’. If answered anything otherwise, it is coded as ‘0’. |
| Freedom of Mobility 5. Are you usually ‘allowed’ to go to the market? 6. Are you usually ‘allowed’ to go to the health facility? 7. Are you usually ‘allowed’ to go the outside the village? | If answered ‘alone’, coded as ‘1’; ‘not at all’ and ‘with someone else only’, coded as ‘0’. |
| Financial Stability 8. Do you own money that you yourself can use? 9. Do you have a bank or savings account that you can use? | If answered ‘Yes’, coded as ‘1’; ‘No’ coded as ‘0’. |
| Attitude Towards IPV 10. Justifies IPV on grounds: She goes out without telling her husband, neglects children, argues with the husband, refuses to have sex with the husband, burns the food. | Does not justify is coded as ‘0’; Justifies is coded as ‘1’. |
| Variables | All Adverse Birth Outcomes (1) | Miscarriage (2) | Abortion (3) | Stillbirth (4) | LBW (5) | PTB (6) |
|---|---|---|---|---|---|---|
| Autonomy | 1.06 | 1.14 | 0.8 | 0.49 * | 1.12 | 1.44 |
| IPV | ||||||
| 0 (Ref) | ||||||
| 1 | 1.17 * | 1.29 * | 1.33 | 1.23 | 0.93 | 1.08 |
| 2 | 1.22 | 1.05 | 1.6 | 0.97 | 1.26 | 1.32 |
| 3 | 1.48 * | 1.01 | 1.89 * | 0.75 | 1.62 | 2.93 ** |
| Working Status | ||||||
| No (Ref) | ||||||
| Yes | 1.20 * | 1.29 * | 1.56 ** | 0.69 | 0.99 | 1.34 |
| Perpetration of IPV * Working Status | ||||||
| 0 * Yes (Ref) | ||||||
| 1 * Yes | 1.14 | 0.75 | 1.1 | 2.23 | 1.81 ** | 0.86 |
| 2 * Yes | 0.64 * | 0.65 | 0.34 * | 1.35 | 0.69 | 0.86 |
| 3 * Yes | 0.94 | 1.24 | 0.86 | 1.2 | 0.94 | 0.46 |
| Marital Controlling Behaviour | ||||||
| 0 (Ref) | ||||||
| 1 | 0.94 | 0.99 | 0.98 | 0.78 | 0.83 | 1.06 |
| 2 | 0.82 ** | 0.94 | 0.72 | 0.6 | 0.88 | 0.54 ** |
| Residential Site | ||||||
| Urban (Ref) | ||||||
| Rural | 0.96 | 1.06 | 0.69 * | 1.16 | 1.03 | 1.01 |
| Educational Attainment | ||||||
| None (Ref) | ||||||
| Primary | 1.01 | 1.05 | 1.46 | 0.7 | 0.78 | 1.5 |
| Secondary | 1.02 | 1.15 | 1.39 | 0.60 ** | 0.75 * | 1.54 * |
| Higher | 0.92 | 1.28 | 0.82 | 0.57 | 0.70 * | 1.01 |
| Wealth Quintile | ||||||
| Poorest (Ref) | ||||||
| Poorer | 1.22 ** | 1.35 * | 1.46 * | 0.8 | 1.17 | 0.98 |
| Middle | 1.50 *** | 1.47 ** | 2.69 *** | 1.5 | 1.37 * | 0.92 |
| Richer | 1.48 *** | 1.59 *** | 3.04 *** | 1.37 | 1.24 | 0.62 |
| Richest | 1.38 ** | 1.58 * | 2.82 *** | 0.43 | 1.11 | 1.18 |
| Age Group | ||||||
| 15–19 (Ref) | ||||||
| 20–24 | 0.57 ** | 0.51 ** | 0.34 ** | 4.28 | 0.67 | 1.08 |
| 25–29 | 0.52 *** | 0.47 *** | 0.32 ** | 4.1 | 0.6 | 1.08 |
| 30–34 | 0.57 ** | 0.43 *** | 0.51 | 2.67 | 0.64 | 1.3 |
| 35–39 | 0.64 * | 0.57 * | 0.54 | 6.04 ** | 0.49 * | 1.91 |
| 40–44 | 0.73 | 0.6 | 0.87 | 4.65 | 0.5 | 2.14 |
| 45–49 | 0.87 | 0.5 | 1.04 | 14.88 ** | 1.05 | 8.72 × 10−7 *** |
| Constant | 0.26 *** | 0.10 *** | 0.02 *** | 0.00 *** | 0.12 *** | 0.00 *** |
| State Dummies | Included | Included | Included | Included | Included | Included |
| No. of Observations | 17,286 | 17,286 | 17,286 | 17,286 | 17,286 | 17,286 |
| Variables | Rural (1) | Urban (2) | Working (3) | Non-Working (4) |
|---|---|---|---|---|
| Autonomy | 1.07 | 0.98 | 0.59 * | 1.19 |
| IPV | ||||
| 0 (Ref) | ||||
| 1 | 1.29 ** | 0.91 | 1.44 ** | 1.15 |
| 2 | 1.33 * | 1.03 | 0.89 | 1.19 |
| 3 | 1.52 * | 1.29 | 1.75 * | 1.42 |
| Working Status | ||||
| No (Ref) | ||||
| Yes | 1.24 ** | 1.2 | - | - |
| Perpetration of IPV * Working Status | ||||
| 0 * Yes (Ref) | ||||
| 1 * Yes | 0.95 | 1.83 | - | - |
| 2 * Yes | 0.40 *** | 1.53 | - | - |
| 3 * Yes | 0.84 | 1.66 | - | - |
| Marital Controlling Behaviour | ||||
| 0 (Ref) | ||||
| 1 | 1.11 | 0.57 *** | 0.89 | 0.95 |
| 2 | 0.86 | 0.77 | 0.79 | 0.83 |
| Educational Attainment | ||||
| None (Ref) | ||||
| Primary | 1.14 | 0.72 | 0.91 | 1.03 |
| Secondary | 1.05 | 1.06 | 1.06 | 1.02 |
| Higher | 0.96 | 0.88 | 0.82 | 0.95 |
| Wealth Quintile | ||||
| Poorest (Ref) | ||||
| Poorer | 1.26 ** | 0.8 | 1.19 | 1.21 * |
| Middle | 1.39 *** | 1.32 | 1.61 ** | 1.45 *** |
| Richer | 1.81 *** | 0.79 | 1.86 ** | 1.41 ** |
| Richest | 1.63 ** | 0.9 | 1.62 | 1.38 * |
| Age Group | ||||
| 15–19 (Ref) | ||||
| 20–24 | 0.66 * | 0.28 ** | 1.06 | 0.54 ** |
| 25–29 | 0.62 ** | 0.25 *** | 1.07 | 0.49 *** |
| 30–34 | 0.7 | 0.26 *** | 0.94 | 0.56 ** |
| 35–39 | 0.79 | 0.26 ** | 1.32 | 0.59 ** |
| 40–44 | 1.04 | 0.21 *** | 1.64 | 0.65 |
| 45–49 | 0.91 | 0.6 | 5.03 ** | 0.48 |
| Residential Site | ||||
| Urban (Ref) | ||||
| Rural | - | - | 0.92 | 0.96 |
| Constant | 0.20 *** | 0.65 | 0.13 *** | 0.28 *** |
| State Dummies | Included | Included | Included | Included |
| No. of Observations | 13,257 | 4021 | 3845 | 13,438 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ghatak, S.; Dutta, M. Negotiating Autonomy: The Linkages between Intimate Partner Violence, Women’s Paid Work Status and Birth Outcomes. Adm. Sci. 2023, 13, 82. https://doi.org/10.3390/admsci13030082
Ghatak S, Dutta M. Negotiating Autonomy: The Linkages between Intimate Partner Violence, Women’s Paid Work Status and Birth Outcomes. Administrative Sciences. 2023; 13(3):82. https://doi.org/10.3390/admsci13030082
Chicago/Turabian StyleGhatak, Subhasree, and Meghna Dutta. 2023. "Negotiating Autonomy: The Linkages between Intimate Partner Violence, Women’s Paid Work Status and Birth Outcomes" Administrative Sciences 13, no. 3: 82. https://doi.org/10.3390/admsci13030082
APA StyleGhatak, S., & Dutta, M. (2023). Negotiating Autonomy: The Linkages between Intimate Partner Violence, Women’s Paid Work Status and Birth Outcomes. Administrative Sciences, 13(3), 82. https://doi.org/10.3390/admsci13030082





