Conceptual Frameworks Linking Sexual Health to Physical, Mental, and Interpersonal Well-Being: A Comprehensive Systematic Review and Meta-Analysis
Abstract
1. Introduction
1.1. Conceptualizing Sexual Health
1.2. Overview of Research on Orgasms
1.3. Sexual Health Correlates
1.4. Organizing Conceptual Framework
1.5. Previous Reviews
1.6. Present Meta-Analysis
2. Method
2.1. Eligibility Criteria
- written in any language that could be translated using AI tools;
- consisted of human participants only;
- contained independent samples (i.e., providing effects within a group of participants that have not been previously published in other articles out of that sample);
- included a measure of sexual satisfaction;
- Included at least one other dimension of sexual health OR included a measure of individual functioning (i.e., attachment, depression, distress, life satisfaction, loneliness, psychological well-being, negative affect, stress, well-being, vitality) OR relationship functioning (i.e., relationship quality, relationship satisfaction, attachment avoidance, attachment anxiety);
- provided statistical indices of a link between at least one aspect of sexual health and either another facet of sexual health OR one of the corresponding correlates (individual or relationship functioning). If relevant variables were measured but an effect of their association was not reported, authors of the record were contacted via repeated emails in an attempt to collect the relevant statistic;
- reported an effect size specifically either in the form of a Pearson’s r correlation coefficient, a standardized regression coefficient, or other statistical value from which a Pearson’s r correlation coefficient or standardized regression coefficient could be computed (e.g., a 2 by 2 chi-squared, a Cohen’s d; see Section 2.7 for transformation formulas used).
2.2. Information Sources
2.3. Search Strategy
2.4. Data Collection Process
2.5. Data Items
2.6. Classification of Variable Domains
2.7. Statistical Analyses
3. Results
3.1. Yield of Comprehensive Literature Search
3.2. Overview of Records
3.3. Meta-Analytic Correlations
3.4. Meta-Analytic Path Analyses
3.5. Moderation Effects
3.6. Publication Bias
4. Discussion
4.1. Implications
4.2. Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Abdel-Hamid, I. A., & Saleh, E. S. (2011). Primary lifelong delayed ejaculation: Characteristics and response to bupropion. Journal of Sexual Medicine, 8, 1772–1779. [Google Scholar] [CrossRef] [PubMed]
- Abedi, P., Afrazeh, M., Javadifar, N., & Saki, A. (2015). The relation between stress and sexual function and satisfaction in reproductive-age women in Iran: A cross-sectional study. Journal of Sex & Marital Therapy, 41, 384–390. [Google Scholar] [CrossRef]
- Abedi, P., Afshari, P., Yaralizadeh, M., & Dastoorpoor, M. (2020). Does loneliness following empty nest impair sexual function and satisfaction of middle-aged Iranian women? Sexuality & Culture, 24(6), 2045–2055. [Google Scholar] [CrossRef]
- Abramov, L. A. (1976). Sexual life and sexual frigidity among women developing acute myocardial infarction. Psychosomatic Medicine, 38, 418–425. [Google Scholar] [CrossRef]
- Adam, F., De Sutter, P., Day, J., & Grimm, E. (2020). A randomized study comparing video-based mindfulness-based cognitive therapy with video-based traditional cognitive behavioral therapy in a sample of women struggling to achieve orgasm. The Journal of Sexual Medicine, 17, 312–324. [Google Scholar] [CrossRef]
- Aerts, L., Enzlin, P., Verhaeghe, J., Poppe, W., Vergote, I., & Amant, F. (2015). Sexual functioning in women after surgical treatment for endometrial cancer: A prospective controlled study. Journal of Sexual Medicine, 12, 198–209. [Google Scholar] [CrossRef]
- Alvisi, S., Baldassarre, M., Lambertini, M., Martelli, V., Berra, M., Moscatiello, S., Marchesini, G., Venturoli, S., & Meriggiola, M. C. (2014). Sexuality and psychopathological aspects in premenopausal women with metabolic syndrome. Journal of Sexual Medicine, 11, 2020–2028. [Google Scholar] [CrossRef]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (DSM-5) (5th ed.). American Psychiatric Association. [Google Scholar]
- Amiri, S. E., Brassard, A., Rosen, N. O., Rossi, M. A., Beaulieu, N., Bergeron, S., & Péloquin, K. (2021). Sexual function and satisfaction in couples with infertility: A closer look at the role of personal and relational characteristics. The Journal of Sexual Medicine, 18(12), 1984–1997. [Google Scholar] [CrossRef]
- Andrejek, N., Fetner, T., & Heath, M. (2022). Climax as work: Heteronormativity, gender labor, and the gender gap in orgasms. Gender & Society, 36(2), 189–213. [Google Scholar] [CrossRef]
- Andrejek, N., Fetner, T., & Heath, M. (2025). Climax as work: Heteronormativity, gender labor, and the gender gap in orgasms. In V. Taylor, L. J. Rupp, A. D. Crossley, & N. E. Whittier (Eds.), Feminist frontiers: Readings on gender, sexuality, and society (pp. 194–211). Bloomsbury. [Google Scholar]
- Appa, A. A., Creasman, J., Brown, J. S., Van Den Eeden, S. K., Thom, D. H., Subak, L. L., & Huang, A. J. (2014). The impact of multimorbidity on sexual function in middle-aged and older women: Beyond the single disease perspective. Journal of Sexual Medicine, 11, 2744–2755. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, E. A., England, P., & Fogarty, A. C. K. (2012). Accounting for women’s orgasm and sexual enjoyment in college hookups and relationships. American Sociological Review, 77, 435–462. [Google Scholar] [CrossRef]
- Artune-Ulkumen, B., Erkan, M. M., Pala, H. G., & Bulbul, Y. B. (2014). Sexual dysfunction in Turkish women with dyspareunia and its impact on the quality of life. Clinical and Experimental Obstetrics & Gynecology, 41, 567–571. [Google Scholar] [CrossRef]
- Asselmann, E., Hoyer, J., Wittchen, H. U., & Martini, J. (2016). Sexual problems during pregnancy and after delivery among women with and without anxiety and depressive disorders prior to pregnancy: A prospective-longitudinal study. Journal of Sexual Medicine, 13, 95–104. [Google Scholar] [CrossRef]
- Assimakopoulos, K., Panayiotopoulos, S., Iconomou, G., Karaivazoglou, K., Matzaroglou, C., Vagenas, K., & Kalfarentzos, F. (2006). Assessing sexual function in obese women preparing for bariatric surgery. Obesity Surgery, 16, 1087–1091. [Google Scholar] [CrossRef]
- Atarodi-Kashani, Z., Kariman, N., Ebadi, A., Majd, H. A., & Beladi-Moghadam, N. (2017). Sexual function and related factors in Iranian woman with epilepsy. Seizure: European Journal of Epilepsy, 52, 147–153. [Google Scholar] [CrossRef]
- Atis, G., Dalkilinc, A., Altuntas, Y., Atis, A., Gurbuz, C., Ofluoglu, Y., Cil, E., & Caskurlu, T. (2011). Hyperthyroidism: A risk factor for female sexual dysfunction. Journal of Sexual Medicine, 8, 2327–2333. [Google Scholar] [CrossRef]
- Attaky, A., Kok, G., & Dewitte, M. (2022). Attachment orientation moderates the sexual and relational implications of sexual desire discrepancies. Journal of Sex & Marital Therapy, 48(4), 343–362. [Google Scholar] [CrossRef]
- Aubin, S., Berger, R., Heiman, J. R., & Ciol, M. (2008). The association between sexual function, pain, and psychological adaptation of men diagnosed with chronic pelvic pain syndrome type III. Journal of Sexual Medicine, 5, 657–667. [Google Scholar] [CrossRef]
- Aubrey, J. S., Harrison, K., Kramer, L., & Yellin, J. (2003). Variety versus timing: Gender differences in college students’ sexual expectations as predicted by exposure to sexually oriented television. Communication Research, 30, 432–460. [Google Scholar] [CrossRef]
- Bakhtiari, A., Basirat, Z., & Nasiri-Amiri, F. (2016). Sexual dysfunction in women undergoing fertility treatment in Iran: Prevalence and associated risk factors. Journal of Reproduction & Infertility, 17, 26–33. [Google Scholar]
- Barbara, G., Pifarotti, P., Facchin, F., Cortinovis, I., Dridi, D., Ronchetti, C., Calzolari, L., & Vercellini, P. (2016). Impact of mode of delivery on female postpartum sexual functioning: Spontaneous vaginal delivery and operative vaginal delivery vs. cesarean section. The Journal of Sexual Medicine, 13, 393–401. [Google Scholar] [CrossRef]
- Barrientos, J. E., & Páez, D. (2006). Psychosocial variables of sexual satisfaction in Chile. Journal of Sex & Marital Therapy, 32, 351–368. [Google Scholar] [CrossRef] [PubMed]
- Battaglia, C., Battaglia, B., Mancini, F., Nappi, R. E., Paradisi, R., & Venturoli, S. (2011). Moderate alcohol intake, genital vascularization, and sexuality in young, healthy, eumenorrheic women. A pilot study. Journal of Sexual Medicine, 8, 2334–2343. [Google Scholar] [CrossRef] [PubMed]
- Beaber, T. E., & Werner, P. D. (2009). The relationship between anxiety and sexual functioning in lesbians and heterosexual women. Journal of Homosexuality, 56, 639–654. [Google Scholar] [CrossRef] [PubMed]
- Beaulieu, N., Bergeron, S., Brassard, A., Byers, E. S., & Péloquin, K. (2023). Toward an integrative model of intimacy, sexual satisfaction, and relationship satisfaction: A prospective study in long-term couples. The Journal of Sex Research, 60(8), 1100–1112. [Google Scholar] [CrossRef]
- Beck, A. T., Steer, R. A., & Brown, G. K. (1996). Manual for the beck depression inventory-II. Psychological Corporation. [Google Scholar]
- Berenguer, C., Rebôlo, C., & Costa, R. M. (2019). Interoceptive awareness, alexithymia, and sexual function. Journal of Sex & Marital Therapy, 45, 729–738. [Google Scholar] [CrossRef]
- Berman, J. R., Berman, L. A., Lin, H., Flaherty, E., Lahey, N., & Cantey-Kiser, J. (2011). Effect of sildenafil on subjective and physiologic parameters of the female sexual response in women with sexual arousal disorder. Journal of Sex & Marital Therapy, 27, 411–420. [Google Scholar] [CrossRef]
- Blair, K. L., Cappell, J., & Pukall, C. F. (2018). Not all orgasms were created equal: Differences in frequency and satisfaction of orgasm experiences by sexual activity in same-sex versus mixed-sex relationships. Journal of Sex Research, 55, 719–733. [Google Scholar] [CrossRef]
- Bodenmann, G., Atkins, D. C., Schär, M., & Poffet, V. (2010). The association between daily stress and sexual activity. Journal of Family Psychology, 24, 271–279. [Google Scholar] [CrossRef]
- Borenstein, M., Hedges, L. V., Higgins, J. P. T., & Rothstein, H. R. (2009). Introduction to meta-analysis. John Wiley & Sons Ltd. [Google Scholar]
- Borissova, A. M., Kovatcheva, R., Shinkov, A., & Vukov, M. (2001). A study of the psychological status and sexuality in middle-aged Bulgarian women: Significance of the hormone replacement therapy (HRT). Maturitas, 39, 177–183. [Google Scholar] [CrossRef] [PubMed]
- Boudreau, G., Brassard, A., Beaulieu, N., Audet, A., & Péloquin, K. (2024). Attachment and sexual functioning in couples seeking fertility treatment: The role of infertility-specific coping strategies. Journal of Sex & Marital Therapy, 50(3), 395–412. [Google Scholar] [CrossRef] [PubMed]
- Bouhlel, S., Derbel, C. H., Nakhli, J., Bellazreg, F., Meriem, H. B., Omezzine, A., & Hadj, B. B. (2017). Sexual dysfunction in Tunisian patients living with HIV. Sexologies, 26, e11–e16. [Google Scholar] [CrossRef]
- Bowlby, J. (1969). Attachment and loss: Vol. 1. Attachment (2nd ed.). Basic Books. [Google Scholar]
- Bowlby, J. (1973). Attachment and loss: Vol. 2. Separation: Anxiety and anger. Basic Books. [Google Scholar]
- Bowlby, J. (1980). Attachment and loss: Vol. 3. Sadness and depression. Basic Books. [Google Scholar]
- Bowlby, J. (1988). A secure base: Clinical applications of attachment theory. Routledge. [Google Scholar]
- Brezsnyak, M., & Whisman, M. A. (2004). Sexual desire and relationship functioning: The effects of marital satisfaction and power. Journal of Sex & Marital Therapy, 30(3), 199–217. [Google Scholar] [CrossRef]
- Brody, S. (2006). Penile—Vaginal intercourse is better: Evidence trumps ideology. Sexual and Relationship Therapy, 21, 393–403. [Google Scholar] [CrossRef]
- Brody, S. (2007). Vaginal orgasm is associated with better psychological function. Sexual and Relationship Therapy, 22, 173–191. [Google Scholar] [CrossRef]
- Brody, S. (2010). The relative health benefits of different sexual activities. Journal of Sexual Medicine, 7, 1336–1361. [Google Scholar] [CrossRef]
- Brody, S. (2017). Evaluation of female orgasmic disorder. In W. W. Ishak (Ed.), Textbook of clinical sexual medicine (pp. 203–218). Springer. [Google Scholar]
- Brody, S., & Costa, R. M. (2008). Vaginal orgasm is associated with less use of immature psychological defense mechanisms. Journal of Sexual Medicine, 5, 1167–1176. [Google Scholar] [CrossRef]
- Brody, S., & Costa, R. M. (2009). Satisfaction (sexual, life, relationship, and mental health) is associated directly with penile-vaginal intercourse, but inversely with other sexual behavior frequencies. Journal of Sexual Medicine, 6, 1947–1954. [Google Scholar] [CrossRef]
- Brody, S., Costa, R. M., Klapilová, K., & Weiss, P. (2018). Specifically penile-vaginal intercourse frequency is associated with better relationship satisfaction: A commentary on Hicks, McNulty, Meltzer, and Olson (2016). Psychological Science, 29(4), 667–669. [Google Scholar] [CrossRef]
- Brody, S., Houde, S., & Hess, U. (2010). Greater tactile sensitivity and less use of immature psychological defense mechanisms predict women’s penile-vaginal intercourse orgasm. Journal of Sexual Medicine, 7, 3057–3065. [Google Scholar] [CrossRef] [PubMed]
- Brody, S., & Weiss, P. (2010). Vaginal orgasm is associated with vaginal (not clitoral) sex education, focusing mental attention on vaginal sensations, intercourse duration, and a preference for a longer penis. Journal of Sexual Medicine, 7, 2774–2781. [Google Scholar] [CrossRef] [PubMed]
- Brody, S., & Weiss, P. (2011). Simultaneous penile-vaginal intercourse orgasm is associated with satisfaction (sexual, life, partnership, and mental health). Journal of Sexual Medicine, 8, 734–741. [Google Scholar] [CrossRef] [PubMed]
- Brotto, L., Atallah, S., Johnson-Agbakwu, C., Rosenbaum, T., Abdo, C., Byers, E. S., Graham, C., Nobe, P., & Wylie, K. (2016). Psychological and interpersonal dimensions of sexual function and dysfunction. The Journal of Sexual Medicine, 13(4), 538–571. [Google Scholar] [CrossRef]
- Brotto, L. A., Heiman, J. R., Goff, B., Greer, B., Lentz, G. M., Swisher, E., Tamimi, H., & Van Blaricom, A. (2008). A Psychoeducational Intervention for Sexual Dysfunction in Women with Gynecologic Cancer. Archives of Sexual Behavior, 37, 317–329. [Google Scholar] [CrossRef]
- Burleson, M. H., Trevathan, W. R., & Todd, M. (2007). In the mood for love or vice versa? Exploring the relations among sexual activity, physical affection, affect, and stress in the daily lives of mid-aged women. Archives of Sexual Behavior, 36, 357–368. [Google Scholar] [CrossRef]
- Burri, A. (2017). Sexual sensation seeking, sexual compulsivity, and gender identity and its relationship with sexual functioning in a population sample of men and women. The Journal of Sexual Medicine, 14, 69–77. [Google Scholar] [CrossRef]
- Burri, A., Hilpert, P., & Spector, T. (2015). Longitudinal evaluation of sexual function in a cohort of pre- and postmenopausal women. Journal of Sexual Medicine, 12, 1427–1435. [Google Scholar] [CrossRef]
- Burri, A., Spector, T., & Rahman, Q. (2013). A discordant monozygotic twin approach to testing environmental influences on sexual dysfunction in women. Archives of Sexual Behavior, 42, 961–972. [Google Scholar] [CrossRef]
- Busby, D. M., Hanna-Walker, V., & Leavitt, C. E. (2022). Is kissing a bellwether of sexual and relationship satisfaction and dissatisfaction? Journal of Sex & Marital Therapy, 48(2), 133–146. [Google Scholar] [CrossRef]
- Busby, D. M., Hanna-Walker, V., & Leavitt, C. E. (2023). A kiss is not just a kiss: Kissing frequency, sexual quality, attachment, and sexual and relationship satisfaction. Sexual and Relationship Therapy, 38(1), 7–23. [Google Scholar] [CrossRef]
- Busch, T. M., Goodwin, G. J., Dempsey, M. R., Conrads, G. S., & Wilson, S. M. (2025). Exploring the Impact of Fantasizing on Romantic Relationships and Attachment. Sexuality & Culture, 29(2), 610–635. [Google Scholar] [CrossRef]
- Cagnacci, A., Venier, M., Xholli, A., Paglietti, C., & Caruso, S. (2020). Female sexuality and vaginal health across the menopausal age. Menopause, 27, 14–19. [Google Scholar] [CrossRef] [PubMed]
- Calvillo, C., Sánchez-Fuentes, M. D. M., & Sierra, J. C. (2020). An explanatory model of sexual satisfaction in adults with a same-sex partner: An analysis based on gender differences. International Journal of Environmental Research and Public Health, 17(10), 3393. [Google Scholar] [CrossRef] [PubMed]
- Canat, M., Canat, L., Öztürk, F. Y., Eroğlu, H., Atalay, H. A., & Altuntaş, Y. (2016). Vitamin D 3 deficiency is associated with female sexual dysfunction in premenopausal women. International Urology and Nephrology, 48, 1789–1795. [Google Scholar] [CrossRef]
- Carmen, R. A. (2014). Untangling the complexities of female sexuality: A mixed approach [Master’s Thesis, State University of New York at New Paltz]. Available online: http://hdl.handle.net/1951/63469 (accessed on 25 April 2025).
- Carmichael, M. S., Humbert, R., Dixen, J., Palmisano, G., Greenleaf, W., & Davidson, J. M. (1987). Plasma oxytocin increases in the human sexual response. The Journal of Clinical Endocrinology & Metabolism, 64, 27–31. [Google Scholar] [CrossRef]
- Carrobles, J. A., Guadix, M. G., & Almendros, C. (2011). Funcionamiento sexual, satisfacción sexual y bienestar psicológico y subjetivo en una muestra de mujeres españolas. Anales de Psicología/Annals of Psychology, 27, 27–34. Available online: https://revistas.um.es/analesps/article/view/113441 (accessed on 25 April 2025).
- Carter, C. S. (1992). Oxytocin and sexual behavior. Neuroscience & Biobehavioral Reviews, 16, 131–144. [Google Scholar] [CrossRef]
- Caruso, S., Cicero, C., Romano, M., Presti, L. L., Ventura, B., & Malandrino, C. (2012). Tadalafil 5 mg daily treatment for type 1 diabetic premenopausal women affected by sexual genital arousal disorder. Journal of Sexual Medicine, 9, 2057–2065. [Google Scholar] [CrossRef]
- Castellini, G., Mannucci, E., Mazzei, C., Lo Sauro, C., Faravelli, C., Rotella, C. M., Maggi, M., & Ricca, V. (2010). Sexual function in obese women with and without binge eating disorder. Journal of Sexual Medicine, 7, 3969–3978. [Google Scholar] [CrossRef]
- Celikel, E., Ozel-kizil, E. T., Akbostanci, M. C., & Cevik, A. (2008). Assessment of sexual dysfunction in patients with Parkinson’s disease: A case–control study. European Journal of Neurology, 15, 1168–1172. [Google Scholar] [CrossRef]
- Ceyhan, O., Ozen, B., Simsek, N., & Dogan, A. (2019). Sexuality and marital adjustment in women with hypertension in Turkey: How culture affects sex. Journal of Human Hypertension, 33, 378–384. [Google Scholar] [CrossRef]
- Chadwick, S. B., Francisco, M., & van Anders, S. M. (2019). When orgasms do not equal pleasure: Accounts of “bad” orgasm experiences during consensual sexual encounters. Archives of Sexual Behavior, 48, 2435–2459. [Google Scholar] [CrossRef] [PubMed]
- Chadwick, S. B., & van Anders, S. M. (2017). Do women’s orgasms function as a masculinity achievement for men? The Journal of Sex Research, 54(9), 1141–1152. [Google Scholar] [CrossRef]
- Chang, S., Ho, H., Chen, K., Shyu, M., Huang, L., & Lin, W. (2012). Depressive symptoms as a predictor of sexual function during pregnancy. Journal of Sexual Medicine, 9, 2582–2589. [Google Scholar] [CrossRef] [PubMed]
- Chang, S. R., Yang, C. F., & Chen, K. H. (2019). Relationships between body image, sexual dysfunction, and health-related quality of life among middle-aged women: A cross-sectional study. Maturitas, 126, 45–50. [Google Scholar] [CrossRef]
- Charbonneau-Lefebvre, V., Rosen, N. O., Bosisio, M., Vaillancourt-Morel, M. P., & Bergeron, S. (2021). An attachment perspective on partner responses to genito-pelvic pain and their associations with relationship and sexual outcomes. The Journal of Sex Research, 58(2), 235–247. [Google Scholar] [CrossRef]
- Chatterji, S., Bay-Cheng, L. Y., Schick, V., Dodge, B., Baldwin, A., Van Der Pol, B., & Fortenberry, J. D. (2017). The year’s best: Interpersonal elements of bisexual women’s most satisfying sexual experiences in the past year. The Journal of Sex Research, 54, 887–898. [Google Scholar] [CrossRef]
- Cheng, J. Y. W., Ng, E. M. L., & Ko, J. S. N. (2007). Depressive symptomatology and male sexual functions in late life. Journal of Affective Disorders, 104, 225–229. [Google Scholar] [CrossRef]
- Chivers, M. L., Pittini, R., Grigoriadis, S., Villegas, L., & Ross, L. E. (2011). The relationship between sexual functioning and depressive symptomatology in postpartum women: A pilot study. Journal of Sexual Medicine, 8, 792–799. [Google Scholar] [CrossRef]
- Ciftci, H., Savas, M., Gulum, M., Yeni, E., Verit, A., & Topal, U. (2011). Evaluation of sexual function in men with orchialgia. Archives of Sexual Behavior, 40, 631–634. [Google Scholar] [CrossRef] [PubMed]
- Cinek, B. Y., Varan, M. P., Yaprak, G., & Altıntaş, M. (2025). Cognitive Emotion Regulation and Its Impact on Sexual Function, Body Image, and Depression in Breast Cancer Survivors. Psychiatry Investigation, 22(3), 330–339. [Google Scholar] [CrossRef] [PubMed]
- Cochran, W. G. (1954). The combination of estimates from different experiments. Biometrics, 10, 101–129. [Google Scholar] [CrossRef]
- Cohen, D. L., & Belsky, J. (2008). Avoidant romantic attachment and female orgasm: Testing an emotion-regulation hypothesis. Attachment and Human Development, 10, 1–10. [Google Scholar] [CrossRef]
- Cohen, J. (1992). A power primer. Psychological Bulletin, 112, 155–159. [Google Scholar] [CrossRef]
- Cohen, S., Kamarck, T., & Mermelstein, R. (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24, 385–396. [Google Scholar] [CrossRef]
- Conroy, A. A., Ruark, A., Neilands, T. B., Darbes, L. A., Johnson, M. O., Tan, J. Y., & Mkandawire, J. (2021). Development and validation of the couple sexual satisfaction scale for HIV and sexual health research. Archives of Sexual Behavior, 50(7), 3297–3311. [Google Scholar] [CrossRef]
- Conroy, K. (2018). The relationship between sexual activity and sexual function in breast and gynecologic cancer patients during adjuvant chemotherapy [Master’s Thesis, Ohio State University]. Available online: http://hdl.handle.net/1811/84805 (accessed on 25 April 2025).
- Constantine, S. (2017). Women’s sexual fantasies in context: The emotional content of sexual fantasies, psychological and interpersonal distress, and satisfaction in romantic relationships [Doctoral Dissertation, City University of New York]. Available online: https://academicworks.cuny.edu/gc_etds/2162 (accessed on 25 April 2025).
- Cook, W. L., & Kenny, D. A. (2005). The actor–partner interdependence model: A model of bidirectional effects in developmental studies. International Journal of Behavioral Development, 29, 101–109. [Google Scholar] [CrossRef]
- Cooper, E. B., Fenigstein, A., & Fauber, R. L. (2014). The faking orgasm scale for women: Psychometric properties. Archives of Sexual Behavior, 43, 423–435. [Google Scholar] [CrossRef]
- Cooper, H., Hedges, L. V., & Valentine, J. C. (2009). The handbook of research synthesis and meta-analysis (2nd ed.). Russell Sage Foundation. [Google Scholar]
- Costa, R. M., & Brody, S. (2007). Women’s relationship quality is associated with specifically penile-vaginal intercourse orgasm and frequency. Journal of Sex & Marital Therapy, 33, 319–327. [Google Scholar] [CrossRef]
- Costa, R. M., & Brody, S. (2011). Anxious and avoidant attachment, vibrator use, anal sex, and impaired vaginal orgasm. Journal of Sexual Medicine, 8, 2493–2500. [Google Scholar] [CrossRef]
- Costa, R. M., & Brody, S. (2012). Greater resting heart rate variability is associated with orgasms through penile–vaginal intercourse, but not with orgasms from other sources. The Journal of Sexual Medicine, 9, 188–197. [Google Scholar] [CrossRef] [PubMed]
- Costa, R. M., Pestana, J., Costa, D., & Wittmann, M. (2016). Altered states of consciousness are related to higher sexual responsiveness. Consciousness and Cognition, 42, 135–141. [Google Scholar] [CrossRef] [PubMed]
- Cruz, R. V., & Caringal-Go, J. F. (2021). Filipinos behind closed doors: Nonsexual and sexual constructs as predictors of sexual and relationship satisfaction in Filipino individuals. Sexuality & Culture, 25(3), 807–834. [Google Scholar] [CrossRef]
- Dashti, S., Latiff, L. A., Hamid, H. A., Sani, S. M., Akhtari-Zavare, M., Bakar, A., Sabiri, N. A., Ismail, M., & Esfehani, A. J. (2016). Sexual dysfunction in patients with polycystic ovary syndrome in Malaysia. Asian Pacific Journal of Cancer Prevention, 17, 3747–3751. Available online: http://journal.waocp.org/article_33048.html (accessed on 25 April 2025).
- Davidson, J. K., & Hoffman, L. E. (1986). Sexual fantasies and sexual satisfaction: An empirical analysis of erotic thought. The Journal of Sex Research, 22, 184–205. [Google Scholar] [CrossRef]
- De Amicis, L. A., Goldberg, D. C., Lopiccolo, J., & Davies, L. (1984). Three-year follow-up of couples evaluated for sexual dysfunction. Journal of Sex & Marital Therapy, 10, 215–228. [Google Scholar] [CrossRef]
- Deci, E. L., & Ryan, R. M. (2000). The “what” and “why” of goal pursuits: Human needs and the self-determination of behavior. Psychological Inquiry, 11, 227–268. [Google Scholar] [CrossRef]
- de Jong, D. C. (2016). Validation of a measure of implicit sexual desire for romantic partners [Doctoral Dissertation, University of Rochester]. Available online: https://search.proquest.com/docview/1823257882?pq-origsite=gscholar (accessed on 25 April 2025).
- Delavierre, D. (2008). Diagnosis of male anorgasmia. Progres en Urologie: Journal de l’Association Francaise D’urologie et de la Societe Francaise D’urologie, 18, F8–F10. Available online: https://europepmc.org/article/med/18773846 (accessed on 25 April 2025). [CrossRef]
- de Lucena, B. B., & Abdo, C. H. N. (2014). Personal factors that contribute to or impair women’s ability to achieve orgasm. International Journal of Impotence Research, 26, 177–181. [Google Scholar] [CrossRef]
- Demir, S. E., Rezvani, A., & Ok, S. (2013). Assessment of sexual functions in female patients with ankylosing spondylitis compared with healthy controls. Rheumatology International, 33, 57–63. [Google Scholar] [CrossRef]
- Denes, A. (2012). Pillow talk: Exploring disclosures after sexual activity. Western Journal of Communication, 76, 91–108. [Google Scholar] [CrossRef]
- Denes, A. (2018). Toward a post-sex disclosures model: Exploring the associations among orgasm, self-disclosure, and relationship satisfaction. Communication Research, 45, 297–318. [Google Scholar] [CrossRef]
- Denes, A., Crowley, J. P., & Bennett, M. (2020). Between the sheets: Investigating young adults’ communication during sexual activity. Personal Relationships, 27(2), 484–501. [Google Scholar] [CrossRef]
- Denes, A., Horan, S. M., & Bennett, M. (2019). “Faking it” and affectionate communication: Exploring the authenticity of orgasm and relational quality indicators. Personality and Individual Differences, 151, 109470. [Google Scholar] [CrossRef]
- de Oliveira, L., Vallejo-Medina, P., & Carvalho, J. (2025). The mediating role of sexual boredom in women’s sexual desire and satisfaction. Journal of Sex & Marital Therapy, 51(1), 96–109. [Google Scholar]
- de Oliveira Ferro, J. K., Lemos, A., da Silva, C. P., de Paiva Lima, C. R. O., Raposo, M. C. F., de Aguiar Cavalcanti, G., & de Oliveira, D. A. (2019). Predictive factors of male sexual dysfunction after traumatic spinal cord injury. Spine, 44, 1228–1237. [Google Scholar] [CrossRef]
- Derogatis, L. R. (1997). The Derogatis Interview for Sexual Functioning (DISF/DISF-SR): An introductory report. Journal of Sex & Marital Therapy, 23, 291–304. [Google Scholar] [CrossRef]
- Derogatis, L. R., & Melisaratos, N. (1979). The DSFI: A multidimensional measure of sexual functioning. Journal of Sex & Marital Therapy, 5, 244–281. [Google Scholar] [CrossRef] [PubMed]
- Dèttore, D., Pucciarelli, M., & Santarnecchi, E. (2013). Anxiety and female sexual functioning: An empirical study. Journal of Sex & Marital Therapy, 39, 216–240. [Google Scholar] [CrossRef]
- Dienberg, M. F., Oschatz, T., Piemonte, J. L., & Klein, V. (2023). Women’s orgasm and its relationship with sexual satisfaction and well-being. Current Sexual Health Reports, 15(3), 223–230. [Google Scholar] [CrossRef]
- Diener, E. D., Emmons, R. A., Larsen, R. J., & Griffin, S. (1985). The satisfaction with life scale. Journal of Personality Assessment, 49, 71–75. [Google Scholar] [CrossRef] [PubMed]
- Dion, J., Hamel, C., Prévost, B., Bergeron-Leclerc, C., Pouliot, E., Maltais, D., Grenier, J., Dubé, M., Ouellet-Plamondon, C., & Vaillancourt-Morel, M.-P. (2023). Stressed and distressed: How is the COVID-19 pandemic associated with sexual frequency, sexual satisfaction, and relationship satisfaction? The Journal of Sexual Medicine, 20(2), 152–160. [Google Scholar] [CrossRef] [PubMed]
- Dissiz, M. (2018). The effect of heroin use disorder on the sexual functions of women. Journal of Psychiatry and Neurological Sciences, 31, 238–245. [Google Scholar] [CrossRef]
- Dogan, V. B., Dagdeviren, H., Dirican, A., Dirican, A. C., Tutar, N. K., Yayla, V. A., & Cengiz, H. (2017). Hormonal effect on the relationship between migraine and female sexual dysfunction. Neurological Sciences, 38, 1651–1655. [Google Scholar] [CrossRef]
- do Rosário Ramos Nunes Bacalhau, M., Pedras, S., & da Graça Pereira Alves, M. (2020). Attachment style and body image as mediators between marital adjustment and sexual satisfaction in women with cervical daspecancer. Supportive Care in Cancer, 28(12), 5813–5819. [Google Scholar] [CrossRef]
- Dosch, A., Ghisletta, P., & Van der Linden, M. (2016). Body image in dyadic and solitary sexual desire: The role of encoding style and distracting thoughts. The Journal of Sex Research, 53(9), 1193–1206. [Google Scholar] [CrossRef]
- Du, J., Ruan, X., Gu, M., Bitzer, J., & Mueck, A. O. (2016). Prevalence of and risk factors for sexual dysfunction in young Chinese women according to the Female Sexual Function Index: An internet-based survey. European Journal of Contraception & Reproductive Health Care, 21, 259–263. [Google Scholar] [CrossRef]
- Duits, A., Van Oirschot, N., Van Oostenbrugge, R. J., & Van Lankveld, J. (2009). The relevance of sexual responsiveness to sexual function in male stroke patients. The Journal of Sexual Medicine, 6, 3320–3326. [Google Scholar] [CrossRef]
- Dunkley, C. R., Dang, S. S., Chang, S. C. H., & Gorzalka, B. B. (2016). Sexual functioning in young women and men: Role of attachment orientation. Journal of Sex and Marital Therapy, 42, 413–430. [Google Scholar] [CrossRef]
- Dunn, K. M., Croft, P. R., & Hackett, G. I. (1999). Association of sexual problems with social, psychological, and physical problems in men and women: A cross sectional population survey. Journal of Epidemiology & Community Health, 53, 144–148. [Google Scholar] [CrossRef]
- Duval, S., & Tweedie, R. (2000). Trim and fill: A simple funnel-plot–based method of testing and adjusting for publication bias in meta-analysis. Biometrics, 56, 455–463. [Google Scholar] [CrossRef] [PubMed]
- Dyar, C., Newcomb, M. E., Mustanski, B., & Whitton, S. W. (2020). A structural equation model of sexual satisfaction and relationship functioning among sexual and gender minority individuals assigned female at birth in diverse relationships. Archives of Sexual Behavior, 49(2), 693–710. [Google Scholar] [CrossRef] [PubMed]
- Eaton, L., Kueck, A., Maksut, J., Gordon, L., Metersky, K., Miga, A., Brewer, M., Siembida, E., & Bradley, A. (2017). Sexual health, mental health, and beliefs about cancer treatments among women attending a gynecologic oncology clinic. Sexual Medicine, 5, e175–e183. [Google Scholar] [CrossRef] [PubMed]
- Egger, M., Davey Smith, G., Schneider, M., & Minder, C. (1997). Bias in meta-analysis detected by a simple, graphical test. British Medical Journal, 315, 629–634. [Google Scholar] [CrossRef]
- Eichel, E. W., De Simone Eichel, J., & Kule, S. (1988). The technique of coital alignment and its relation to female orgasmic response and simultaneous orgasm. Journal of Sex and Marital Therapy, 14, 129–141. [Google Scholar] [CrossRef]
- Ellero, J. (2019). Altered states of consciousness, absorption, and sexual responsiveness [Master’s Thesis, ISPA—Instituto Universitário]. Available online: http://hdl.handle.net/10400.12/7173 (accessed on 25 April 2025).
- Ellsworth, R. M., & Bailey, D. H. (2013). Human female orgasm as evolved signal: A test of two hypotheses. Archives of Sexual Behavior, 42, 1545–1554. [Google Scholar] [CrossRef]
- Fabre, L. F., Clayton, A. H., Smith, L. C., Goldstein, I. M., & Derogatis, L. R. (2013). Association of major depression with sexual dysfunction in men. Journal of Neuropsychiatry and Clinical Neurosciences, 25, 308–318. [Google Scholar] [CrossRef]
- Fabre, L. F., & Smith, L. C. (2012). The effect of major depression on sexual function in women. Journal of Sexual Medicine, 9, 231–239. [Google Scholar] [CrossRef]
- Fahs, B. (2014). Coming to power: Women’s fake orgasms and best orgasm experiences illuminate the failures of (hetero) sex and the pleasures of connection. Culture, Health & Sexuality, 16, 974–988. [Google Scholar] [CrossRef]
- Fahs, B., & Plante, R. (2017). On ‘good sex’ and other dangerous ideas: Women narrate their joyous and happy sexual encounters. Journal of Gender Studies, 26, 33–44. [Google Scholar] [CrossRef]
- Fan, X., Henderson, D. C., Chiang, E., Briggs, L. B. N., Freudenreich, O., Evins, A. E., Cather, C., & Goff, D. C. (2007). Sexual functioning, psychopathology and quality of life in patients with schizophrenia. Schizophrenia Research, 94, 119–127. [Google Scholar] [CrossRef] [PubMed]
- Farnam, F., Pakgohar, M., Mirmohamadali, M., & Mahmoodi, M. (2008). Effect of sexual education on sexual health in Iran. Sex Education, 8(2), 159–168. [Google Scholar] [CrossRef]
- Feder, H. (2023). Is pornography good for women’s sexual well-being?: Depends on why they watch it [Master’s Thesis, University of Haifa]. [Google Scholar]
- Feldman, J., & Larsen, K. (2014). Sexual dysfunction. In S. Richards, & M. W. O’Hara (Eds.), Oxford handbook of depression and comorbidity (pp. 218–235). Oxford University Press, Incorporated. [Google Scholar]
- Fisher, W. A., Rosen, R. C., Eardley, I., Sand, M., & Goldstein, I. (2005). Sexual experience of female partners of men with erectile dysfunction: The female experience of men’s attitudes to life events and sexuality (FEMALES) study. Journal of Sexual Medicine, 2, 675–684. [Google Scholar] [CrossRef] [PubMed]
- Fleishman, J. M., Crane, B., & Koch, P. B. (2020). Correlates and predictors of sexual satisfaction for older adults in same-sex relationships. Journal of Homosexuality, 67(14), 1974–1998. [Google Scholar] [CrossRef]
- Flynn, K. E., Lin, L., Cyranowski, J. M., Reeve, B. B., Reese, J. B., Jeffery, D. D., Smith, A. W., Porter, L. S., Dombeck, C. B., Burner, D. W., Keefe, F. J., & Weinfurt, K. P. (2013). Development of the NIH PROMIS® sexual function and satisfaction measures in patients with cancer. Journal of Sexual Medicine, 10, 43–52. [Google Scholar] [CrossRef]
- Forbes, M. K., Baillie, A. J., & Schniering, C. A. (2016). Should sexual problems be included in the internalizing spectrum? A comparison of dimensional and categorical models. Journal of Sex & Marital Therapy, 42, 70–90. [Google Scholar] [CrossRef]
- Fragla, E., Privitera, S., Giardina, R., Di Rosa, A., Russo, G. I., Favilla, V., Caramma, A., Patti, F., Cimino, S., & Morgia, G. (2014). Determinants of sexual impairment in multiple sclerosis in male and female patients with lower urinary tract dysfunction: Results from an Italian cross-sectional study. Journal of Sexual Medicine, 11, 2406–2413. [Google Scholar] [CrossRef]
- Fraley, R. C., Waller, N. G., & Brennan, K. A. (2000). An item response theory analysis of self-report measures of adult attachment. Journal of Personality and Social Psychology, 78, 350–365. [Google Scholar] [CrossRef]
- Frederick, D. A., Lever, J., Gillespie, B. J., & Garcia, J. R. (2017). What keeps passion alive? Sexual satisfaction is associated with sexual communication, mood setting, sexual variety, oral sex, orgasm, and sex frequency in a national U.S. study. Journal of Sex Research, 54, 186–201. [Google Scholar] [CrossRef]
- Frederick, D. A., St. John, H. K. S., Garcia, J. R., & Lloyd, E. A. (2018). Differences in orgasm frequency among gay, lesbian, bisexual, and heterosexual men and women in a U.S. national sample. Archives of Sexual Behavior, 47, 273–288. [Google Scholar] [CrossRef]
- Gades, N. M., Jacobson, D. J., McGree, M. E., Sauver, J. L. S., Lieber, M. M., Nehra, A., Girman, C. J., Klee, G. G., & Jacobsen, S. J. (2008). The associations between serum sex hormones, erectile function, and sex drive: The Olmsted county study of urinary symptoms and health status among men. The Journal of Sexual Medicine, 5, 2209–2220. [Google Scholar] [CrossRef]
- Gaither, T. W., Shahrvini, T., Vincent, N. W., Russell, M. M., & Litwin, M. S. (2024). Anorectal sexual function index: Development and validation of a health-related quality of life measure. Urology, 188, 87–93. [Google Scholar] [CrossRef]
- Galinsky, A. M. (2012). Sexual touching and difficulties with sexual arousal and orgasm among U.S. older adults. Archives of Sexual Behavior, 41, 875–890. [Google Scholar] [CrossRef]
- Gallup, G. G., Ampel, B. C., Wedberg, N., & Pogosjan, A. (2014). Do orgasms give women feedback about mate choice? Evolutionary Psychology, 12, 958–978. [Google Scholar] [CrossRef]
- Georgiadis, J. R., & Kringelbach, M. L. (2012). The human sexual response cycle: Brain imaging evidence linking sex to other pleasures. Progress in Neurobiology, 98, 49–81. [Google Scholar] [CrossRef]
- Georgiadis, J. R., Reinders, A. S., Paans, A. M., Renken, R., & Kortekaas, R. (2009). Men versus women on sexual brain function: Prominent differences during tactile genital stimulation, but not during orgasm. Human Brain Mapping, 30, 3089–3101. [Google Scholar] [CrossRef]
- Gesselman, A. N., Wion, R. K., Garcia, J. R., & Miller, W. R. (2021). Relationship and sexual satisfaction are associated with better disease self-management in persons with epilepsy. Epilepsy & Behavior, 119, 107937. [Google Scholar] [CrossRef] [PubMed]
- Gewirtz-Meydan, A. (2017). Why do narcissistic individuals engage in sex? Exploring sexual motives as a mediator for sexual satisfaction and function. Personality and Individual Differences, 105, 7–13. [Google Scholar] [CrossRef]
- Gewirtz-Meydan, A., & Finzi-Dottan, R. (2018). Sexual satisfaction among couples: The role of attachment orientation and sexual motives. The Journal of Sex Research, 55, 178–190. [Google Scholar] [CrossRef] [PubMed]
- Gérard, M., Charvier, K., Leduc, H., & Courtois, F. (2025). Looking beyond the chair: Psycho-perceptual predictors of sexual distress and sexual satisfaction in individuals with spinal cord injury. The Journal of Sex Research, 62(1), 65–82. [Google Scholar] [CrossRef]
- Giordano, F. G., & Rush, C. L. (2010). Self-esteem and sexuality: An exploration of differentiation and attachment. In Self-esteem across the lifespan: Issues and interventions (pp. 205–218). Routledge. [Google Scholar]
- Girouard, A., Dion, J., Bőthe, B., O’Sullivan, L., & Bergeron, S. (2021). Bullying victimization and sexual wellbeing in sexually active heterosexual, cisgender and sexual/gender minority adolescents: The mediating role of emotion regulation. Journal of Youth and Adolescence, 50(11), 2136–2150. [Google Scholar] [CrossRef]
- Gomes, A. L. Q., & Nobre, P. (2012). The International Index of Erectile Function (IIEF-15): Psychometric properties of the Portuguese version. Journal of Sexual Medicine, 9, 180–187. [Google Scholar] [CrossRef]
- Goodman, D. L. (2011). Associations of attachment style and reasons to pretend orgasm; development and validation of reasons to pretend orgasm measure in a relational context [Doctoral Dissertation, University of Kansas]. Available online: http://hdl.handle.net/1808/13008 (accessed on 25 April 2025).
- Goodman, D. L., Gillath, O., & Haj-Mohamadi, P. (2017). Development and validation of the pretending orgasm reasons measure. Archives of Sexual Behavior, 46, 1973–1991. [Google Scholar] [CrossRef]
- Gracia, C. R., Freeman, E. W., Sammel, M. D., Lin, H., & Mogul, M. (2007). Hormones and sexuality during transition to menopause. Obstetrics & Gynecology, 109, 831–840. [Google Scholar] [CrossRef] [PubMed]
- Graham, C. A. (2014). Orgasm Disorders in Women. In Y. M. Binik, & K. S. K. Hall (Eds.), Principles and practice of sex therapy (5th ed., pp. 89–111). The Guildford Press. [Google Scholar]
- Granata, A., Tirabassi, G., Pugni, V., Arnaldi, G., Boscaro, M., Carani, C., & Balercia, G. (2013). Sexual dysfunctions in men affected by autoimmune Addison’s disease before and after short-term gluco- and mineralocorticoid replacement therapy. The Journal of Sexual Medicine, 10, 2036–2043. [Google Scholar] [CrossRef] [PubMed]
- Grose, R. G. (2016). Critical consciousness and sexual pleasure: Evidence for a sexual empowerment process for heterosexual and sexual minority women [Doctoral Dissertation, University of California, Santa Cruz]. Available online: https://escholarship.org/uc/item/61r1d1sm (accessed on 25 April 2025).
- Gunst, A., Ventus, D., Kärnä, A., Salo, P., & Jern, P. (2017). Female sexual function varies over time and is dependent on partner-specific factors: A population-based longitudinal analysis of six sexual function domains. Psychological Medicine, 47, 341–352. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y. N., Ng, E. M. L., & Chan, K. (2004). Foreplay, orgasm, and after-play among Shanghai couple and its integrative relation with their marital satisfaction. Sexual and Relationship Therapy, 19, 63–78. [Google Scholar] [CrossRef]
- Gutsche, M., & Burri, A. (2017). What women want—An explorative study on women’s attitudes toward sexuality boosting medication in a sample of Swiss women. Journal of Sexual Medicine, 14, 404–412. [Google Scholar] [CrossRef]
- Haavio-Mannila, E., & Kontula, O. (1997). Correlates of increased sexual satisfaction. Archives of Sexual Behavior, 26, 399–419. [Google Scholar] [CrossRef]
- Hangen, F., Crasta, D., & Rogge, R. D. (2020). Delineating the boundaries between nonmonogamy and infidelity: Bringing consent back into definitions of consensual nonmonogamy with latent profile analysis. The Journal of Sex Research, 57, 438–457. [Google Scholar] [CrossRef]
- Hangen, F., & Rogge, R. D. (2022). Focusing the Conceptualization of Erotophilia and Erotophobia on global attitudes toward sex: Development and validation of the sex positivity-negativity scale. Archives of Sexual Behavior, 51, 521–545. [Google Scholar] [CrossRef] [PubMed]
- Harte, C. B., & Meston, C. M. (2012). Recreational use of erectile dysfunction medications and its adverse effects on erectile function in young healthy men: The mediating role of confidence in erectile ability. The Journal of Sexual Medicine, 9, 1852–1859. [Google Scholar] [CrossRef] [PubMed]
- Hassan, A., El-Hadidy, M., El-Deeck, B. S., & Mostafa, T. (2008). Couple satisfaction to different therapeutic modalities for organic erectile dysfunction. The Journal of Sexual Medicine, 5, 2381–2391. [Google Scholar] [CrossRef] [PubMed]
- Hazewinkel, M. H., Laan, E. T., Sprangers, M. A., Fons, G., Burger, M. P., & Roovers, J. P. W. (2012). Long-term sexual function in survivors of vulvar cancer: A cross-sectional study. Gynecologic Oncology, 126, 87–92. [Google Scholar] [CrossRef]
- Heinrichs, D. W., Hanlon, T. E., & Carpenter, W. T., Jr. (1984). The quality of life scale: An instrument for rating the schizophrenic deficit syndrome. Schizophrenia Bulletin, 10, 388–398. [Google Scholar] [CrossRef]
- Hendrick, S. S., Dicke, A., & Hendrick, C. (1998). The relationship assessment scale. Journal of Social and Personal Relationships, 15, 137–142. [Google Scholar] [CrossRef]
- Hevesi, K., Gergely Hevesi, B., Kolba, T. N., & Rowland, D. L. (2020). Self-reported reasons for having difficulty reaching orgasm during partnered sex: Relation to orgasmic pleasure. Journal of Psychosomatic Obstetrics & Gynecology, 41, 106–115. [Google Scholar] [CrossRef]
- Hevesi, K., Mészáros, V., Kövi, Z., Márki, G., & Szabó, M. (2017). Different characteristics of the Female Sexual Function Index in a sample of sexually active and inactive women. The Journal of Sexual Medicine, 14, 1133–1141. [Google Scholar] [CrossRef]
- Holstege, G., & Huynh, H. K. (2011). Brain circuits for mating behavior in cats and brain activations and de-activations during sexual stimulation and ejaculation and orgasm in humans. Hormones and Behavior, 59, 702–707. [Google Scholar] [CrossRef]
- Horton, D. J. (1982). Sex-role orientation, sexual behavior and sexual satisfaction in women [Doctoral Dissertation, George Washington University]. Available online: https://www.elibrary.ru/item.asp?id=7351884 (accessed on 25 April 2025).
- Hoyer, J., Uhmann, S., Rambow, J., & Jacobi, F. (2009). Reduction of sexual dysfunction: By-product of cognitive-behavioural therapy for psychological disorders? Sexual and Relationship Therapy, 24, 64–73. [Google Scholar] [CrossRef]
- Hunter, C. L., & Goodie, J. L. (2017). Sexual problems. American Psychiatric Association. [Google Scholar]
- Huntingdon, B., Muscat, D. M., de Wit, J., Duracinsky, M., & Juraskova, I. (2020). Factors associated with general sexual functioning and sexual satisfaction among people living with HIV: A systematic review. The Journal of Sex Research, 57(7), 824–835. [Google Scholar] [CrossRef]
- Hurlbert, D. F., Apt, C., & Rabehl, S. M. (1993). Key variables to understanding female sexual satisfaction: An examination of women in nondistressed marriages. Journal of Sex and Marital Therapy, 19, 154–165. [Google Scholar] [CrossRef]
- Hurlbert, D. F., & Whittaker, K. E. (1991). The role of masturbation in marital and sexual satisfaction: A comparative study of female masturbators and nonmasturbators. Journal of Sex Education and Therapy, 17, 272–282. [Google Scholar] [CrossRef]
- Hwang, U. J., Lee, M. S., Jung, S. H., Ahn, S. H., & Kwon, O. Y. (2019). Pelvic floor muscle parameters affect sexual function after 8 weeks of transcutaneous electrical stimulation in women with stress urinary incontinence. Sexual Medicine, 7, 505–513. [Google Scholar] [CrossRef] [PubMed]
- Jannini, E. A., & Lenzi, A. (2005). Ejaculatory disorders: Epidemiology and current approaches to definition, classification and subtyping. World Journal of Urology, 23, 68–75. [Google Scholar] [CrossRef] [PubMed]
- Jensen, P. T., Klee, M. C., Tharanov, I., & Groenvold, M. (2004). Validation of a questionnaire for self-assesment of sexual function and vaginal changes after gynaecological cancer. Psycho-Oncology, 13, 577–592. [Google Scholar] [CrossRef]
- Jiann, B., Su, C., & Tsai, J. (2013). Is female sexual function related to the male partners’ erectile function? Journal of Sexual Medicine, 10, 420–429. [Google Scholar] [CrossRef]
- Jolink, T. A., Way, B. M., Younge, A., & Algoe, S. B. (2025). Do inflammation and relational motivation coordinate having better sex? The interplay between C-reactive protein and relational approach motivation on sexual well-being. Brain, Behavior, and Immunity, 123, 151–161. [Google Scholar] [CrossRef]
- Jones, A. C., Robinson, W. D., & Seedall, R. B. (2018). The role of sexual communication in couples’ sexual outcomes: A dyadic path analysis. Journal of Marital and Family Therapy, 44, 606–623. [Google Scholar] [CrossRef]
- Józefacka, N. M., Szpakiewicz, E., Lech, D., Guzowski, K., & Kania, G. (2023). What matters in a relationship—Age, sexual satisfaction, relationship length, and interpersonal closeness as predictors of relationship satisfaction in young adults. International Journal of Environmental Research and Public Health, 20(5), 4103. [Google Scholar] [CrossRef]
- Kahn, A. S. (2001). Entitlement and sexuality: An exploration of the relationship between entitlement level and female sexual attitudes, behaviors, and satisfaction [Doctoral Dissertation, Adelphi University]. Available online: https://www.elibrary.ru/item.asp?id=5346342 (accessed on 25 April 2025).
- Kaighobadi, F., Shackelford, T. K., & Weekes-Shackelford, V. A. (2012). Do women pretend orgasm to retain a mate? Archives of Sexual Behavior, 41, 1121–1125. [Google Scholar] [CrossRef]
- Kalmbach, D. A., Arnedt, J. T., Pillai, V., & Ciesla, J. A. (2015). The impact of sleep on female sexual response and behavior: A pilot study. Journal of Sexual Medicine, 12, 1221–1232. [Google Scholar] [CrossRef]
- Kalmbach, D. A., Ciesla, J. A., Janata, J. W., & Kingsberg, S. A. (2012). Specificity of anhedonic depression and anxious arousal with sexual problems among sexually healthy young adults. Journal of Sexual Medicine, 9, 505–513. [Google Scholar] [CrossRef]
- Kalmbach, D. A., Kingsberg, S. A., Roth, T., Cheng, P., Fellman-Couture, C., & Drake, C. L. (2019). Sexual function and distress in postmenopausal women with chronic insomnia: Exploring the role of stress dysregulation. Nature and Science of Sleep, 11, 141–153. [Google Scholar] [CrossRef]
- Kalmbach, D. A., & Pillai, V. (2014). Daily affect and female sexual function. Journal of Sexual Medicine, 11, 2938–2954. [Google Scholar] [CrossRef] [PubMed]
- Kamrava, S. K., Tavakol, Z., Talebi, A., Farhadi, M., Jalessi, M., Hosseini, S. F., Amini, E., Chen, B., Hummel, T., & Alizadeh, R. (2021). A study of depression, partnership and sexual satisfaction in patients with post-traumatic olfactory disorders. Scientific Reports, 11(1), 20218. [Google Scholar] [CrossRef] [PubMed]
- Karabulutlu, E. Y., Okanli, A., & Sivrikaya, S. K. (2011). Sexual dysfunction and depression in Turkish female hemodialysis patients. Pakistan Journal of Medical Sciences, 27, 842–846. [Google Scholar]
- Karaçin, P., & Küçükşahin, İ. (2025). Sexual dysfunction in breast cancer survivors: The role of clinical, hormonal, and psychosocial factors. Healthcare, 13(16), 2061. [Google Scholar] [CrossRef]
- Karakose, S., Urs, M., Marshall, J. E., & Ledermann, T. (2023). Depression, anxiety, stress, and sexual satisfaction in couples. Journal of Sex & Marital Therapy, 49(6), 616–629. [Google Scholar] [CrossRef]
- Karney, B. R., & Bradbury, T. N. (1995). The longitudinal course of marital quality and stability: A review of theory, methods, and research. Psychological Bulletin, 118, 3–34. [Google Scholar] [CrossRef]
- Kelley, E. L., & Gidycz, C. A. (2017). Mediators of the relationship between sexual assault and sexual behaviors in college women. Journal of Interpersonal Violence, 7, 574–582. [Google Scholar] [CrossRef]
- Keskin, G., Babacan Gümüş, A., & Taşdemir Yiğitoğlu, G. (2019). Sexual dysfunctions and related variables with sexual function in patients who undergo dialysis for chronic renal failure. Journal of Clinical Nursing, 28, 257–269. [Google Scholar] [CrossRef]
- Kfoury, M., Barakat, H., Hallit, S., & Saliba, S. (2023). Association between endometriosis and sexual satisfaction among a sample of lebanese women. BMC Women’s Health, 23(1), 164. [Google Scholar] [CrossRef]
- Khajehei, M., Doherty, M., Tilley, P. J. M., & Sauer, K. (2015). Prevalence and risk factors of sexual dysfunction in postpartum Australian women. Journal of Sexual Medicine, 12, 1415–1426. [Google Scholar] [CrossRef]
- Khazaie, H., Rezaie, L., Payam, N. R., & Najafi, F. (2015). Antidepressant-induced sexual dysfunction during treatment with fluoxetine, sertraline and trazodone: A randomized controlled trial. General Hospital Psychiatry, 37, 40–45. [Google Scholar] [CrossRef]
- Khnaba, D., Rostom, S., Lahlou, R., Bahiri, R., Abouqal, R., & Hajjaj-Hassouni, N. (2016). Sexual dysfunction and its determinants in Moroccan women with rheumatoid arthritis. Pan African Medical Journal, 24, 16. [Google Scholar] [CrossRef] [PubMed]
- Kikusui, T., Winslow, J. T., & Mori, Y. (2006). Social buffering: Relief from stress and anxiety. Philosophical Transactions of the Royal Society B: Biological Sciences, 361, 2215–2228. [Google Scholar] [CrossRef] [PubMed]
- Klapilová, K., Brody, S., Krejčová, L., Husárová, B., & Binter, J. (2015). Sexual satisfaction, sexual compatibility, and relationship adjustment in couples: The role of sexual behaviors, orgasm, and men’s discernment of women’s intercourse orgasm. Journal of Sexual Medicine, 12, 667–675. [Google Scholar] [CrossRef] [PubMed]
- Komisaruk, B. R., & Whipple, B. (2005). Functional MRI of the brain during orgasm in women. Annual Review of Sex Research, 16, 62–86. [Google Scholar] [CrossRef]
- Kračun, I., Tul, N., Blickstein, I., & Velikonja, V. G. (2019). Quantitative and qualitative assessment of maternal sexuality during pregnancy. Journal of Perinatal Medicine, 47, 335–340. [Google Scholar] [CrossRef]
- Kreuter, M., Dahllöf, A. G., Gudjonsson, G., Sullivan, M., & Siösteen, A. (1998). Sexual adjustment and its predictors after traumatic brain injury. Brain Injury, 12, 349–368. [Google Scholar] [CrossRef]
- Krishna, K., Avasthi, A., & Grover, S. (2011). Prevalence and psychological impact of antidepressant-associated sexual dysfunction: A study from North India. Journal of Clinical Psychopharmacology, 31, 457–462. [Google Scholar] [CrossRef] [PubMed]
- Krüger, T. H., Haake, P., Hartmann, U., Schedlowski, M., & Exton, M. S. (2002). Orgasm-induced prolactin secretion: Feedback control of sexual drive? Neuroscience & Biobehavioral Reviews, 26(1), 31–44. [Google Scholar] [CrossRef] [PubMed]
- Krüger, T. H., Hartmann, U., & Schedlowski, M. (2005). Prolactinergic and dopaminergic mechanisms underlying sexual arousal and orgasm in humans. World Journal of Urology, 23(2), 130–138. [Google Scholar] [CrossRef] [PubMed]
- Kuffel, S. W., & Heiman, J. R. (2006). Effects of depressive symptoms and experimentally adopted schemas on sexual arousal and affect in sexually healthy women. Archives of Sexual Behavior, 35, 163–177. [Google Scholar] [CrossRef]
- Laan, E., & Rellini, A. H. (2012). Can we treat anorgasmia in women? The challenge to experiencing pleasure. Sexual and Relationship Therapy, 26, 329–341. [Google Scholar] [CrossRef]
- Lafortune, D., Girard, M., Bolduc, R., Boislard, M. A., & Godbout, N. (2022). Insecure attachment and sexual satisfaction: A path analysis model integrating sexual mindfulness, sexual anxiety, and sexual self-esteem. Journal of Sex & Marital Therapy, 48(6), 535–551. [Google Scholar] [CrossRef]
- Lafortune, D., Girard, M., Dussault, É., Philibert, M., Hébert, M., Boislard, M. A., Goyette, M., & Godbout, N. (2023). Who seeks sex therapy? Sexual dysfunction prevalence and correlates, and help-seeking among clinical and community samples. PLoS ONE, 18(3), e0282618. [Google Scholar] [CrossRef]
- Lamela, D., Figueiredo, B., Jongenelen, I., Morais, A., & Simpson, J. A. (2020). Coparenting and relationship satisfaction in mothers: The moderating role of sociosexuality. Archives of Sexual Behavior, 49(3), 861–870. [Google Scholar] [CrossRef]
- Laumann, E. O., Gagnon, J. H., Michael, R. T., & Michaels, S. (2000). The social organization of sexuality: Sexual practices in the United States. University of Chicago Press. [Google Scholar]
- Laurent, S. M., & Simons, A. D. (2009). Sexual dysfunction in depression and anxiety: Conceptualizing sexual dysfunction as part of an internalizing dimension. Clinical Psychology Review, 29, 573–585. [Google Scholar] [CrossRef]
- Leavitt, C. E., Leonhardt, N. D., Busby, D. M., & Clarke, R. W. (2021). When is enough enough? Orgasm’s curvilinear association with relational and sexual satisfaction. The Journal of Sexual Medicine, 18(1), 167–178. [Google Scholar] [CrossRef]
- Leeners, B., Hengartner, M. P., Rössler, W., Ajdacic-Gross, V., & Angst, J. (2014). The role of psychopathological and personality covariates in orgasmic difficulties: A prospective longitudinal evaluation in a cohort of women from age 30 to 50. Journal of Sexual Medicine, 11, 2928–2937. [Google Scholar] [CrossRef]
- Leeners, B., Kruger, T. H., Brody, S., Schmidlin, S., Naegeli, E., & Egli, M. (2013). The quality of sexual experience in women correlates with post-orgasmic prolactin surges: Results from an experimental prototype study. The Journal of Sexual Medicine, 10, 1313–1319. [Google Scholar] [CrossRef]
- Leonhardt, N. D., Willoughby, B. J., Busby, D. M., Yorgason, J. B., & Holmes, E. K. (2018). The significance of the female orgasm: A nationally representative, dyadic study of newlyweds’ orgasm experience. The Journal of Sexual Medicine, 15, 1140–1148. [Google Scholar] [CrossRef]
- Levin, R. J. (2007). Sexual activity, health and well-being—The beneficial roles of coitus and masturbation. Sexual and Relationship Therapy, 22, 135–148. [Google Scholar] [CrossRef]
- Levin, R. J. (2012a). The ever continuing life of that ‘little death’—The human orgasm. Sexual and Relationship Therapy 26, 299–300. [Google Scholar] [CrossRef]
- Levin, R. J. (2012b). The human female orgasm: A critical evaluation of its proposed reproductive functions. Sexual and Relationship Therapy, 26(4), 301–314. [Google Scholar] [CrossRef]
- Levin, R. J. (2014). The pharmacology of the human female orgasm—Its biological and physiological backgrounds. Pharmacology Biochemistry and Behavior, 121, 62–70. [Google Scholar] [CrossRef] [PubMed]
- Lew-Starowicz, M., & Rola, R. (2014). Correlates of sexual function in male and female patients with multiple sclerosis. Journal of Sexual Medicine, 11, 2172–2180. [Google Scholar] [CrossRef] [PubMed]
- Lipe, H., Longstreth, W. T., Bird, T. D., & Linde, M. (1990). Sexual function in married men with Parkinson’s disease compared to married men with arthritis. Neurology, 40, 1347–1349. [Google Scholar] [CrossRef]
- Lipinski, A. J., & Beck, J. G. (2022). Sexual functioning and satisfaction among college survivors of sexual violence: Examining PTSD symptoms and sexual schemas. Journal of Interpersonal Violence, 37(3–4), NP2408–NP2427. [Google Scholar] [CrossRef]
- Lipsey, M. W., & Wilson, D. B. (2001). Practical meta-analysis. Sage Publications, Inc. [Google Scholar]
- Llaneza, P., Fernández-Iñarrea, J. M., Arnott, B., García-Portilla, M. P., Chedraui, P., & Pérez-López, F. R. (2011). Sexual function assessment in postmenopausal women with the 14-item changes in sexual functioning questionnaire. Journal of Sexual Medicine, 8, 2144–2151. [Google Scholar] [CrossRef]
- Lopes, S. D. S. T. (2022). “No vale dos lençóis”: A qualidade subjetiva do sono e a sua associação com o funcionamento sexual [Master’s Thesis, Instituto Superior de Psicologia Aplicada]. [Google Scholar]
- Maassen, G. H., & Bakker, A. B. (2001). Suppressor variables in path models: Definitions and interpretations. Sociological Methods & Research, 30(2), 241–270. [Google Scholar]
- Macia, E., Diop-Dubois, A., Ka, K., & Duboz, P. (2025). Women’s orgasms in Senegal: An exploratory mixed methods study of orgasm frequency, pleasure, and meaning among Senegalese women. Culture, Health & Sexuality, 27(10), 1327–1343. [Google Scholar] [CrossRef] [PubMed]
- Madewell, A. N. (2013). Knowing thyself: Constructing women’s sexual identity theory with sexual anatomy knowledge, vulva genital awareness, and sociopolitical ideations [Doctoral Dissertation, Oklahoma State University]. Available online: https://www.proquest.com/docview/1428424242 (accessed on 25 April 2025).
- Maes, C. A. (2017). A descriptive analysis of perceived stress and sexual function among community-dwelling older adult males [Doctoral Dissertation, University of Arizona]. Available online: https://repository.arizona.edu/handle/10150/625647 (accessed on 25 April 2025).
- Magon, N., & Kalra, S. (2011). The orgasmic history of oxytocin: Love, lust, and labor. Indian Journal of Endocrinology and Metabolism, 15, S156–S161. [Google Scholar] [CrossRef]
- Mallory, A. B. (2022). Dimensions of couples’ sexual communication, relationship satisfaction, and sexual satisfaction: A meta-analysis. Journal of Family Psychology, 36(3), 358–371. Available online: https://psycnet.apa.or (accessed on 25 April 2025). [CrossRef] [PubMed]
- Mangas, P., Sierra, J. C., & Granados, R. (2024). Effects of subjective orgasm experience in sexual satisfaction: A dyadic analysis in same-sex Hispanic couples. Journal of Sex & Marital Therapy, 50(3), 346–368. [Google Scholar] [CrossRef]
- Martin, L. R., Friedman, H. S., Tucker, J. S., Schwartz, J. E., Criqui, M. H., Wingard, D. L., & Tomlinson-Keasey, C. (1995). An archival prospective study of mental health and longevity. Health Psychology, 14(5), 381–387. [Google Scholar] [CrossRef] [PubMed]
- Maslow, A. H. (1943). A theory of human motivation. Psycholgical Review, 50, 370–396. [Google Scholar] [CrossRef]
- Masmoudi, R., Aissi, M., Halouani, N., Fathallah, S., Louribi, I., Aloulou, J., Amami, O., & Frih, M. (2018). Female sexual dysfunction and multiple sclerosis: A case-control study. Progres en Urologie: Journal de l’Association Francaise D’urologie et de la Societe Francaise D’urologie, 28, 530–535. [Google Scholar] [CrossRef]
- McKay, C. L., Van Niekerk, L. M., & Matthewson, M. L. (2022). An exploration of dyadic relationship approach-avoidance goals and relationship and sexual satisfaction in couples coping with endometriosis. Archives of Sexual Behavior, 51(3), 1637–1646. [Google Scholar] [CrossRef]
- McNicoll, G., Corsini-Munt, S., O. Rosen, N., McDuff, P., & Bergeron, S. (2017). Sexual assertiveness mediates the associations between partner facilitative responses and sexual outcomes in women with provoked Vestibulodynia. Journal of Sex & Marital Therapy, 43, 663–677. [Google Scholar] [CrossRef]
- McShane, B. B., Bockenholt, U., & Hansen, K. T. (2016). Adjusting for publication bias in meta-analysis: An evaluation of selection methods and some cautionary notes. Perspectives on Psychological Science, 11, 730–749. [Google Scholar] [CrossRef] [PubMed]
- Meadow, R. M. (1982). Factors contributing to the sexual satisfaction of married women: A multiple regression analysis [Doctoral Dissertation, Arizona State University]. Available online: https://www.elibrary.ru/item.asp?id=7354749 (accessed on 25 April 2025).
- Meltzer, A. L., Makhanova, A., Hicks, L. L., French, J. E., McNulty, J. K., & Bradbury, T. N. (2017). Quantifying the sexual afterglow: The lingering benefits of sex and their implications for pair-bonded relationships. Psychological Science, 28, 587–598. [Google Scholar] [CrossRef]
- Mendes, A. K., Cardoso, F. L., & Savall, A. C. R. (2008). Sexual satisfaction in people with spinal cord injury. Sexuality and Disability, 26, 137–147. [Google Scholar] [CrossRef]
- Mernone, L., Fiacco, S., & Ehlert, U. (2019). Psychobiological factors of sexual health in aging women-findings from the women 40+ healthy aging study. Frontiers in Psychology, 10, 546. [Google Scholar] [CrossRef]
- Merwin, K. E., & Rosen, N. O. (2020). Perceived partner responsiveness moderates the associations between sexual talk and sexual and relationship well-being in individuals in long-term relationships. The Journal of Sex Research, 57(3), 351–364. [Google Scholar] [CrossRef]
- Meston, C. M., Freihart, B. K., Crosby, C. L., Stephenson, K. R., & Trapnell, P. D. (2024). Psychometric evaluation and adaptation of the five-factor Sexual Satisfaction Scale (SSS-W) for use in men: The Sexual Satisfaction Scale (SSS). Journal of Sex & Marital Therapy, 50(2), 216–229. [Google Scholar] [CrossRef]
- Meston, C. M., Hull, E., Levin, R. J., & Sipski, M. (2004a). Disorders of orgasm in women. Journal of Sexual Medicine, 1, 66–68. [Google Scholar] [CrossRef]
- Meston, C. M., Levin, R. J., Sipski, M. L., Hull, E. M., & Heiman, J. R. (2004b). Women’s orgasm. Annual Review of Sex Research, 15, 173–257. [Google Scholar] [CrossRef]
- Mialon, H. M. (2012). The economics of faking ecstasy. Economic Inquiry, 50, 277–285. [Google Scholar] [CrossRef] [PubMed]
- Moher, D., Liberati, A., Tetzlaff, J., & Altman, D. G. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Annals of Internal Medicine, 151, 264–269. [Google Scholar] [CrossRef] [PubMed]
- Monga, T. N., Tan, G., Ostermann, H. J., Monga, U., & Grabois, M. (1998). Sexuality and sexual adjustment of patients with chronic pain. Disability and Rehabilitation, 20, 317–329. [Google Scholar] [CrossRef] [PubMed]
- Morales, M. G., Rubio, J. C., Peralta-Ramirez, M. I., Romero, L. H., Fernández, R. R., García, M. C., Navarrete, N. N., & Centeno, N. O. (2013). Impaired sexual function in women with systemic lupus erythematosus: A cross-sectional study. Lupus, 22, 987–995. [Google Scholar] [CrossRef]
- Morokqff, P. J., & Gillilland, R. (1993). Stress, sexual functioning, and marital satisfaction. Journal of Sex Research, 30, 43–53. [Google Scholar] [CrossRef]
- Moshfeghy, Z., Tahari, S., Janghorban, R., Najib, F. S., Mani, A., & Sayadi, M. (2020). Association of sexual function and psychological symptoms including depression, anxiety and stress in women with recurrent vulvovaginal candidiasis. Journal of the Turkish-German Gynecological Association, 21, 90–96. [Google Scholar] [CrossRef]
- Muehlenhard, C. L., & Shippee, S. K. (2010). Men’s and women’s reports of pretending orgasm. Journal of Sex Research, 47, 552–567. [Google Scholar] [CrossRef]
- Murphy, M. R., Checkley, S. A., Seckl, J. R., & Lightman, S. L. (1990). Naloxone inhibits oxytocin release at orgasm in man. The Journal of Clinical Endocrinology & Metabolism, 71, 1056–1058. [Google Scholar] [CrossRef]
- Murphy, M. R., Seckl, J. R., Burton, S., Checkley, S. A., & Lightman, S. L. (1987). Changes in oxytocin and vasopressin secretion during sexual activity in men. The Journal of Clinical Endocrinology & Metabolism, 65, 738–741. [Google Scholar] [CrossRef]
- Najafabady, M. T., Salmani, Z., & Abedi, P. (2011). Prevalence and related factors for anorgasmia among reproductive aged women in Hesarak, Iran. Clinics, 66, 83–86. [Google Scholar] [CrossRef]
- Nascimento, E. R., Maia, A. C. O., Nardi, A. E., & Silva, A. C. (2015). Sexual dysfunction in arterial hypertension women: The role of depression and anxiety. Journal of Affective Disorders, 181, 96–100. [Google Scholar] [CrossRef] [PubMed]
- Norhayati, M. N., & Azman Yacob, M. (2017). Long-term postpartum effect of severe maternal morbidity on sexual function. The International Journal of Psychiatry in Medicine, 52, 328–344. [Google Scholar] [CrossRef] [PubMed]
- Ogallar-Blanco, A. I., Lara-Moreno, R., & Godoy-Izquierdo, D. (2022). Going beyond “with a partner” and “intercourse”: Does anything else influence sexual satisfaction among women? The sexual satisfaction comprehensive index. International Journal of Environmental Research and Public Health, 19(16), 10232. [Google Scholar] [CrossRef] [PubMed]
- Ogawa, S., Kudo, S., Kitsunai, Y., & Fukuchi, S. (1980). Increase in oxytocin secretion at ejaculation in male. Clinical Endocrinology, 13, 95–97. [Google Scholar] [CrossRef]
- Onem, K., Erol, B., Sanli, O., Kadioglu, P., Yalin, A. S., Canik, U., Cuhadaroglu, C., & Kadioglu, A. (2008). Is sexual dysfunction in women with obstructive sleep apnea-hypopnea syndrome associated with the severity of the disease? A pilot study. Journal of Sexual Medicine, 5, 2600–2609. [Google Scholar] [CrossRef]
- Opperman, E., Braun, V., Clarke, V., & Rogers, C. (2014). “It feels so good it almost hurts”: Young adults’ experiences of orgasm and sexual pleasure. The Journal of Sex Research, 51(5), 503–515. [Google Scholar] [CrossRef]
- Opperman, E. A., Benson, L. E., & Milhausen, R. R. (2013). Confirmatory factor analysis of the Female Sexual Function Index. Journal of Sex Research, 50, 29–36. [Google Scholar] [CrossRef]
- Ourania, P., Dimitra, M., Athina, D., & Victoria, V. (2024). Etiological factors affecting female sexuality: A systematic review. Journal of Sexual Medicine & Research, 3(1), 1–16. [Google Scholar] [CrossRef]
- Özcan, T., Benli, E., Demir, E. Y., Özer, F., Kaya, Y., & Haytan, C. E. (2015). The relation of sexual dysfunction to depression and anxiety in patients with Parkinson’s disease. Acta Neuropsychiatrica, 27, 33–37. [Google Scholar] [CrossRef]
- Özdemir, C., Eryılmaz, M., Yurtman, F., & Karaman, T. (2007). Sexual functioning after renal transplantation. Transplantation Proceedings, 39, 1451–1454. [Google Scholar] [CrossRef]
- Pakpour, A. H., Yekaninejad, M. S., Pallich, G., & Burri, A. (2015). Using ecological momentary assessment to investigate short-term variations in sexual functioning in a sample of peri-menopausal women from Iran. PLoS ONE, 10, e0117299. [Google Scholar] [CrossRef] [PubMed]
- Palmore, E. B. (1982). Predictors of the longevity difference: A 25-year follow-up. The Gerontologist, 22, 513–518. [Google Scholar] [CrossRef] [PubMed]
- Papini, M. N., Fioravanti, G., Talamba, G., Benni, L., Pracucci, C., Godini, L., Lazzeretti, L., Casale, S., & Faravelli, C. (2013). Female sexual functioning: The role of psychopathology. Rivista di Psichiatria, 48, 400–405. [Google Scholar] [CrossRef]
- Parish, W. L., Luo, Y., Stolzenberg, R., Laumann, E. O., Farrer, G., & Pan, S. (2007). Sexual practices and sexual satisfaction: A population based study of Chinese urban adults. Archives of Sexual Behavior, 36, 5–20. [Google Scholar] [CrossRef]
- Park, Y., Impett, E. A., & MacDonald, G. (2021). Singles’ sexual satisfaction is associated with more satisfaction with singlehood and less interest in marriage. Personality and Social Psychology Bulletin, 47(5), 741–752. [Google Scholar] [CrossRef]
- Pascoal, P. M., Byers, E. S., Alvarez, M. J., Santos-Iglesias, P., Nobre, P. J., Pereira, C. R., & Laan, E. (2018). A dyadic approach to understanding the link between sexual functioning and sexual satisfaction in heterosexual couples. The Journal of Sex Research, 55, 1155–1166. [Google Scholar] [CrossRef]
- Peixoto, C., Carrilho, C. G., Ribeiro, T. T. D. S. B., da Silva, L. M., Gonçalves, E. A., Fernandes, L., Nardi, A. E., Cardoso, A., & Veras, A. B. (2019). Relationship between sexual hormones, quality of life and postmenopausal sexual function. Trends in Psychiatry and Psychotherapy, 41, 136–143. [Google Scholar] [CrossRef]
- Peixoto, M. M., & Nobre, P. (2015). Prevalence and sociodemographic predictors of sexual problems in Portugal: A population-based study with women aged 18 to 79 years. Journal of Sex & Marital Therapy, 41(2), 169–180. [Google Scholar]
- Persson, G. (1981). Five-year mortality in a 70-year-old urban population in relation to psychiatric diagnosis, personality, sexuality and early parental death. Acta Psychiatrica Scandinavica, 64, 244–253. [Google Scholar] [CrossRef]
- Peters, S. D., & Meltzer, A. L. (2021). Newlywed couples’ own and partner sexual disgust sensitivities interact to predict their marital satisfaction through their sexual satisfaction. Archives of Sexual Behavior, 50(6), 2563–2577. [Google Scholar] [CrossRef]
- Péloquin, K., Dutrisac, C., Jean, M., Benoit, Z., Brassard, A., Mondor, J., & Lussier, Y. (2022). Relational instability in couples seeking therapy: The contribution of attachment, caregiving and sex. Journal of Sex & Marital Therapy, 48(8), 804–818. [Google Scholar] [CrossRef]
- Philippsohn, S., & Hartmann, U. (2009). Determinants of sexual satisfaction in a sample of German women. Journal of Sexual Medicine, 6, 1001–1010. [Google Scholar] [CrossRef]
- Pickering, T. G. (2003). Men are from Mars, women are from Venus: Stress, pets, and oxytocin. The Journal of Clinical Hypertension, 5, 86–88. [Google Scholar] [CrossRef]
- Pinney, E. M., Gerrard, M., & Denney, N. W. (1987). The pinney sexual satisfaction inventory. Journal of Sex Research, 23, 233–251. [Google Scholar] [CrossRef]
- Pinsky, I. S. (2016). Attachment quality and sexual satisfaction and sexual functioning in romantic relationships for combat veterans [Master’s Thesis, University of Kentucky]. [Google Scholar] [CrossRef]
- Pollard, A. E., & Rogge, R. D. (2022). Love in the time of COVID-19: A multi-wave study examining the salience of sexual and relationship health during the COVID-19 pandemic. Archives of Sexual Behavior, 51(1), 247–271. [Google Scholar] [CrossRef] [PubMed]
- Powers, C. R. (2012). Female orgasm from intercourse: Importance, partner characteristics, and health [Doctoral Dissertation, University of North Texas]. Available online: https://www.semanticscholar.org/paper/Female-Orgasm-From-Intercourse%3A-Importance%2C-Partner-Powers/af8da4739c7dd49aadebf0042a99b0a4b534658f (accessed on 25 April 2025).
- Prause, N. (2012a). The human female orgasm: Critical evaluations of proposed psychological sequelae. Sexual and Relationship Therapy, 26(4), 315–328. [Google Scholar] [CrossRef]
- Prause, N. (2012b). A response to Brody, Costa and Hess (2012): Theoretical, statistical and construct problems perpetuated in the study of female orgasm. Sexual and Relationship Therapy, 27(3), 260–271. [Google Scholar] [CrossRef]
- Quinn-Nilas, C., Benson, L., Milhausen, R. R., Buchholz, A. C., & Goncalves, M. (2016). The relationship between body image and domains of sexual functioning among heterosexual, emerging adult women. Sexual Medicine, 4(3), e182–e189. [Google Scholar] [CrossRef]
- Ramos Costa, L. G., Mercês Pinheiro, A. C., Cabral Miranda, I. P., de Farias, A. L., da Silva, H. P., de Campos Gomes, F., Pascon Barbosa, A. M., da Luz Costa, T., & de Melo Neto, J. S. (2023). Aspects of Sexuality in Quilombola Communities’ Young Adults in Eastern Brazilian Amazon. Behavioral Sciences, 13(6), 492. [Google Scholar] [CrossRef]
- Randolph, M. E. (2002). The role of depression, relationship support, and child sexual abuse in predicting the impact of chronic pelvic pain on women’s sexual functioning [Doctoral Dissertation, University of Wisconsin—Milwaukee]. Available online: https://www.elibrary.ru/item.asp?id=5439148 (accessed on 25 April 2025).
- Rausch, D., & Rettenberger, M. (2021). Predictors of sexual satisfaction in women: A systematic review. Sexual Medicine Reviews, 9(3), 365–380. [Google Scholar] [CrossRef]
- R Core Team. (2017). Foreign: Read data stored by SPSS (R package version 0.8-70). R Core Team. [Google Scholar]
- R Core Team. (2018). R: A language and environment for statistical computing. R Foundation for Statistical Computing. [Google Scholar]
- Regan, P. C., & Atkins, L. (2006). Sex differences and similarities in frequency and intensity of sexual desire. Social Behavior and Personality: An International Journal, 34(1), 95–102. [Google Scholar] [CrossRef]
- Richters, J., de Visser, R., Rissel, C., & Smith, A. (2006). Sexual practices at last heterosexual encounter and occurrence of orgasm in a national survey. Journal of Sex Research, 43, 217–226. [Google Scholar] [CrossRef]
- Rosen, N. O., Dubé, J. P., Corsini-Munt, S., & Muise, A. (2019). Partners experience consequences, too: A comparison of the sexual, relational, and psychological adjustment of women with Sexual Interest/Arousal Disorder and their partners to control couples. The Journal of Sexual Medicine, 16, 83–95. [Google Scholar] [CrossRef] [PubMed]
- Rosen, N. O., Williams, L., Vannier, S. A., & Mackinnon, S. P. (2020). Sexual intimacy in first-time mothers: Associations with sexual and relationship satisfaction across three waves. Archives of Sexual Behavior, 49, 2849–2861. [Google Scholar] [CrossRef] [PubMed]
- Rosen, R., Brown, C., Heiman, J., Leiblum, S., Meston, C., Shabsigh, R., Ferguson, D., & D’Agostino, R. (2000). The Female Sexual Function Index (FSFI): A multidimensional self-report instrument for the assessment of female sexual function. Journal of Sex and Marital Therapy, 26, 191–205. [Google Scholar] [CrossRef] [PubMed]
- Rosen, R. C., Riley, A., Wagner, G., Osterloh, I. H., Kirkpatrick, J., & Mishra, A. (1997). The International Index of Erectile Function (IIEF): A multidimensional scale for assessment of erectile dysfunction. Urology, 49, 822–830. [Google Scholar] [CrossRef]
- Rosenberg, M. S. (2010). A generalized formula for converting chi-square tests to effect sizes for meta-analysis. PLoS ONE, 5, e10059. [Google Scholar] [CrossRef]
- Rottmann, N., Gilså Hansen, D., dePont Christensen, R., Hagedoorn, M., Frisch, M., Nicolaisen, A., Kroman, N., Flyger, H., & Johansen, C. (2017). Satisfaction with sex life in sexually active heterosexual couples dealing with breast cancer: A nationwide longitudinal study. Acta Oncologica, 56, 212–219. [Google Scholar] [CrossRef]
- Rowland, D. L., & Kolba, T. N. (2019). Relationship of specific sexual activities to orgasmic latency, pleasure, and difficulty during partnered sex. The Journal of Sexual Medicine, 16, 559–568. [Google Scholar] [CrossRef]
- Rowland, D. L., Sullivan, S. L., Hevesi, K., & Hevesi, B. (2018). Orgasmic latency and related parameters in women during partnered and masturbatory sex. The Journal of Sexual Medicine, 15, 1463–1471. [Google Scholar] [CrossRef]
- Sahay, R. D., Haynes, E. N., Rao, M. B., & Pirko, I. (2012). Assessment of sexual satisfaction in relation to potential sexual problems in women with multiple sclerosis: A pilot study. Sexuality and Disability, 30, 227–236. [Google Scholar] [CrossRef]
- Sakinci, M., Ercan, C. M., Olgan, S., Coksuer, H., Karasahin, K. E., & Kuru, O. (2016). Comparative analysis of copper intrauterine device impact on female sexual dysfunction subtypes. Taiwanese Journal of Obstetrics and Gynecology, 55, 30–34. [Google Scholar] [CrossRef]
- Salamon, E., Esch, T., & Stefano, G. B. (2005). Role of amygdala in mediating sexual and emotional behavior via coupled nitric oxide release. Acta Pharmacologica Sinica, 26, 389–395. [Google Scholar] [CrossRef]
- Salisbury, C. M. A., & Fisher, W. A. (2014). “Did you come?” A qualitative exploration of gender differences in beliefs, experiences, and concerns regarding female orgasm occurrence during heterosexual sexual interactions. The Journal of Sex Research, 51, 616–631. [Google Scholar] [CrossRef]
- Sariyildiz, M. A., Batmaz, I., Dilek, B., İnanir, A., Bez, Y., Tahtasiz, M., Em, S., & Çevik, R. (2013). Relationship of the sexual functions with the clinical parameters, radiological scores and the quality of life in male patients with ankylosing spondylitis. Rheumatology International, 33, 623–629. [Google Scholar] [CrossRef] [PubMed]
- Sarti, C. D., Graziottin, A., Mincigrucci, M., Ricci, E., Chiaffarino, F., Bonaca, S., Becorpi, A., & Parazzini, F. (2010). Correlates of sexual functioning in Italian menopausal women. Climacteric, 13, 447–456. [Google Scholar] [CrossRef] [PubMed]
- Sayin, H. Ü., & Schenck, C. H. (2019). Neuroanatomy and neurochemistry of sexual desire, pleasure, love and orgasm. SexuS Journal Winter, 4(11), 907–946. [Google Scholar]
- Scott, S. B., Ritchie, L., Knopp, K., Rhoades, G. K., & Markman, H. J. (2018). Sexuality within female same-gender couples: Definitions of sex, sexual frequency norms, and factors associated with sexual satisfaction. Archives of Sexual Behavior, 47, 681–692. [Google Scholar] [CrossRef]
- Seguin, L. J., Milhausen, R. R., & Kukkonen, T. (2015). The development and validation of the motives for feigning orgasms scale. The Canadian Journal of Human Sexuality, 24, 31–48. [Google Scholar] [CrossRef]
- Seldin, D. R., Friedman, H. S., & Martin, L. R. (2002). Sexual activity as a predictor of life-span mortality risk. Personality and Individual Differences, 33, 409–425. [Google Scholar] [CrossRef]
- Shaver, P. R., & Mikulincer, M. (2002). Attachment-related psychodynamics. Attachment & Human Development, 4, 133–161. [Google Scholar] [CrossRef]
- Shaw, A. M., & Rogge, R. D. (2016). Evaluating and refining the construct of sexual quality with item response Theory: Development of the Quality of Sex Inventory. Archives of Sexual Behavior, 45, 249–270. [Google Scholar] [CrossRef]
- Shifren, J. L., Monz, B. U., Russo, P. A., Segreti, A., & Johannes, C. B. (2008). Sexual problems and distress in United States women: Prevalence and correlates. Obstetrics & Gynecology, 112, 970–978. [Google Scholar] [CrossRef]
- Skoczyński, S., Nowosielski, K., Minarowski, Ł., Brożek, G., Oraczewska, A., Glinka, K., Ficek, K., Kotulska, B., Tobiczyk, E., Skomoro, R., Mróz, R., & Barczyk, A. (2019). May dyspnea sensation influence the sexual function in men with obstructive sleep apnea syndrome? A prospective control study. Sexual Medicine, 7, 303–310. [Google Scholar] [CrossRef] [PubMed]
- Smedley, D. K., Leavitt, C. E., Allsop, D. B., Nance, M., James, S. L., & Holmes, E. K. (2021). Mindfulness and sexual mindfulness as moderators between conflict resolution and sexual and relationship satisfaction. Journal of Sex & Marital Therapy, 47(8), 814–828. [Google Scholar] [CrossRef] [PubMed]
- Smith, A. B., Barton, D. L., Davis, M., Jackson, E. A., Smith, J., & Wittmann, D. (2022). A preliminary study of short-term sexual function and satisfaction among men post-myocardial infarction. Journal of Holistic Nursing, 40(3), 208–218. [Google Scholar] [CrossRef]
- Smith, A. S., & Wang, Z. (2014). Hypothalamic oxytocin mediates social buffering of the stress response. Biological Psychiatry, 76, 281–288. [Google Scholar] [CrossRef]
- Speer, J. J., Hillenberg, B., Sugrue, D. P., Blacker, C., Kresge, C. L., Decker, V. B., Zakalik, D., & Decker, D. A. (2005). Study of sexual functioning determinants in breast cancer survivors. The Breast Journal, 11, 440–447. [Google Scholar] [CrossRef]
- Spitalnick, J. S., & McNair, L. D. (2005). Couples therapy with gay and lesbian clients: An analysis of important clinical issues. Journal of Sex & Marital Therapy, 31, 43–56. [Google Scholar] [CrossRef]
- Stephenson, K. R., Ahrold, T. K., & Meston, C. M. (2011). The association between sexual motives and sexual satisfaction: Gender differences and categorical comparisons. Archives of Sexual Behavior, 40(3), 607–618. [Google Scholar] [CrossRef]
- Stephenson, K. R., Hughan, C. P., & Meston, C. M. (2012). Childhood sexual abuse moderates the association between sexual functioning and sexual distress in women. Child Abuse and Neglect, 36, 180–189. [Google Scholar] [CrossRef]
- Stephenson, K. R., & Meston, C. M. (2010). Differentiating components of sexual well-being in women: Are sexual satisfaction and sexual distress independent constructs? The Journal of Sexual Medicine, 7, 2458–2468. [Google Scholar] [CrossRef] [PubMed]
- Stephenson, K. R., & Meston, C. M. (2015). The conditional importance of sex: Exploring the association between sexual well-being and life satisfaction. Journal of Sex & Marital Therapy, 41(1), 25–38. [Google Scholar]
- Stern, J., Karastoyanova, K., Kandrik, M., Torrance, J., Hahn, A. C., Holzleitner, I., DeBruine, L. M., & Jones, B. C. (2020). Are sexual desire and sociosexual orientation related to men’s salivary steroid hormones? Adaptive Human Behavior and Physiology, 6(4), 447–466. [Google Scholar] [CrossRef] [PubMed]
- Stoeber, J., & Harvey, L. N. (2016). Multidimensional sexual perfectionism and female sexual function: A longitudinal investigation. Archives of Sexual Behavior, 45, 2003–2014. [Google Scholar] [CrossRef] [PubMed]
- Stoléru, S., Fonteille, V., Cornélis, C., Joyal, C., & Moulier, V. (2012). Functional neuroimaging studies of sexual arousal and orgasm in healthy men and women: A review and meta-analysis. Neuroscience & Biobehavioral Reviews, 36(6), 1481–1509. [Google Scholar] [CrossRef]
- Stotz, T., Mackelprang, J. L., Harkin, A., Hunt, D., & Buzwell, S. (2025). When is low sexual function problematic for women? A systematic review of factors associated with distress about low sexual function. The Journal of Sexual Medicine, 22(10), 1827–1838. [Google Scholar] [CrossRef]
- Strizzi, J., Landa, L. O., Pappadis, M., Olivera, S. L., Tangarife, E. R. V., Agis, I. F., Perrin, P. B., & Arango-Lasprilla, J. C. (2015). Sexual functioning, desire, and satisfaction in women with TBI and healthy controls. Behavioural Neurology, 2015, 1–7. [Google Scholar] [CrossRef]
- Strizzi, J. M., Øverup, C. S., Ciprić, A., Hald, G. M., & Træen, B. (2022). BDSM: Does it hurt or help sexual satisfaction, relationship satisfaction, and relationship closeness? The Journal of Sex Research, 59(2), 248–257. [Google Scholar] [CrossRef]
- Takahashi, M., Inokuchi, T., Watanabe, C., Saito, T., & Kai, I. (2011). The Female Sexual Function Index (FSFI): Development of a Japanese version. Journal of Sexual Medicine, 8, 2246–2254. [Google Scholar] [CrossRef]
- Tao, P., & Brody, S. (2011). Sexual behavior predictors of satisfaction in a Chinese sample. Journal of Sexual Medicine, 8, 455–460. [Google Scholar] [CrossRef] [PubMed]
- Tavares, I. M., Laan, E. T. M., & Nobre, P. J. (2017). Cognitive-affective dimensions of female orgasm: The role of automatic thoughts and affect during sexual activity. Journal of Sexual Medicine, 14, 818–828. [Google Scholar] [CrossRef] [PubMed]
- Thakurdesai, A., & Sawant, N. (2018). A prospective study on sexual dysfunctions in depressed males and the response to treatment. Indian Journal of Psychiatry, 60, 472–477. [Google Scholar] [CrossRef] [PubMed]
- Therrien, S., & Brotto, L. A. (2016). A critical examination of the relationship between vaginal orgasm consistency and measures of psychological and sexual functioning and sexual concordance in women with sexual dysfunction. Canadian Journal of Human Sexuality, 25, 109–118. [Google Scholar] [CrossRef]
- Thompson, A. E., Record, J. M., Miller, R., & Bjorback, H. (2024). Rose colored glasses: An exploration of the relationship between sexual nostalgia and sexual satisfaction. The Journal of Sex Research, 61(2), 274–284. [Google Scholar] [CrossRef]
- Tiihonen, J., Kuikka, J., Kupila, J., Partanen, K., Vainio, P., Airaksinen, J., Eronen, M., Hallikainen, T., Paanila, J., Kinnunen, I., & Huttunen, J. (1994). Increase in cerebral blood flow of right prefrontal cortex in man during orgasm. Neuroscience Letters, 170, 241–243. [Google Scholar] [CrossRef]
- Tracy, J. K., & Junginger, J. (2007). Correlates of lesbian sexual functioning. Journal of Women’s Health, 16, 499–509. [Google Scholar] [CrossRef]
- Træen, B. (2007). Sexual dissatisfaction among men and women with congenital and acquired heart disease. Sexual and Relationship Therapy, 22, 13–26. [Google Scholar] [CrossRef]
- Tuinman, M. A., Hoekstra, H. J., Vidrine, D. J., Gritz, E. R., Sleijfer, D. T., Fleer, J., & Hoekstra-Weebers, J. E. H. M. (2010). Sexual function, depressive symptoms and marital status in nonseminoma testicular cancer patients: A longitudinal study. Psycho-Oncology, 19, 238–247. [Google Scholar] [CrossRef]
- Tutino, J. S., Ouimet, A. J., & Shaughnessy, K. (2017). How do psychological risk factors predict sexual outcomes? A comparison of four models of young women’s sexual outcomes. The Journal of Sexual Medicine, 14, 1232–1240. [Google Scholar] [CrossRef]
- Twenge, J. M., Sherman, R. A., & Wells, B. E. (2017). Declines in sexual frequency among American adults, 1989–2014. Archives of Sexual Behavior, 46, 2389–2401. [Google Scholar] [CrossRef]
- Uddenberg, N. (1974). Psychological aspects of sexual inadequacy in women. Journal of Psychosomatic Research, 18, 33–47. [Google Scholar] [CrossRef] [PubMed]
- Uhlich, M., Nouri, N., Jensen, R., Meuwly, N., & Schoebi, D. (2022). Associations of conflict frequency and sexual satisfaction with weekly relationship satisfaction in Iranian couples. Journal of Family Psychology, 36(1), 140–146. [Google Scholar] [CrossRef] [PubMed]
- Urganci, B., Sevi, B., & Sakman, E. (2021). Better relationships shut the wandering eye: Sociosexual orientation mediates the association between relationship quality and infidelity intentions. Journal of Social and Personal Relationships, 38(4), 1401–1409. [Google Scholar] [CrossRef]
- Uvnas-Moberg, K. (1998). Antistress pattern induced by oxytocin. Physiology, 13, 22–25. [Google Scholar] [CrossRef]
- Vail-Smith, K., Chaney, B. H., & Williams, M. (2023). Differences in important components of sexual satisfaction as identified and experienced by undergraduate males and females. American Journal of Sexuality Education, 18(3), 504–522. [Google Scholar] [CrossRef]
- van de Grift, T. C., Mureau, M. A., Negenborn, V. N., Dikmans, R. E., Bouman, M. B., & Mullender, M. G. (2020). Predictors of women’s sexual outcomes after implant-based breast reconstruction. Psycho-Oncology, 29(8), 1272–1279. [Google Scholar] [CrossRef]
- van den Brink, F., Smeets, M. A. M., Hessen, D. J., & Woertman, L. (2016). Positive body image and sexual functioning in Dutch female university students: The role of adult romantic attachment. Archives of Sexual Behavior, 45, 1217–1226. [Google Scholar] [CrossRef]
- van Nimwegen, J. F., Arends, S., van Zuiden, G. S., Vissink, A., Kroese, F. G., & Bootsma, H. (2015). The impact of primary Sjögren’s syndrome on female sexual function. Rheumatology, 54, 1286–1293. [Google Scholar] [CrossRef]
- Velten, J., & Margraf, J. (2017). Satisfaction guaranteed? How individual, partner, and relationship factors impact sexual satisfaction within partnerships. PLoS ONE, 12(2), e0172855. [Google Scholar] [CrossRef]
- Viechtbauer, W. (2010). Conducting meta-analyses in R with the metafor package. Journal of Statistical Software, 36, 1–48. [Google Scholar] [CrossRef]
- Villeda Sandoval, C. I. V., Calao-Pérez, M., Enríquez González, A. B., Gonzalez-Cuenca, E., Ibarra-Saavedra, R., Sotomayor, M., & Castillejos Molina, R. A. (2014). Orgasmic dysfunction: Prevalence and risk factors from a cohort of young females in Mexico. The Journal of Sexual Medicine, 11, 1505–1511. [Google Scholar] [CrossRef] [PubMed]
- Vrangalova, Z., & Ong, A. D. (2014). Who benefits from casual sex? The moderating role of sociosexuality. Social Psychological and Personality Science, 5(8), 883–891. [Google Scholar] [CrossRef]
- Wade, L. (2015). Are women bad at orgasms? Understanding the gender gap. In S. Tarrant (Ed.), Gender, sex, and politics: In the streets and between the sheets in the 21st century (pp. 227–237). Routledge. [Google Scholar]
- Wade, L., Kremer, E. C., & Brown, J. (2005). The incidental orgasm: The presence of clitoral knowledge and the absence of orgasm for women. Women & Health, 42, 117–138. [Google Scholar] [CrossRef] [PubMed]
- Waite, L. J., & Joyner, K. (2001). Emotional satisfaction and physical pleasure in sexual unions: Time horizon, sexual behavior, and sexual exclusivity. Journal of Marriage and Family, 63, 247–264. [Google Scholar] [CrossRef]
- Walker, A. M., & Lutmer, A. (2023). Caring, chemistry, and orgasms: Components of great sexual experiences. Sexuality & Culture 27, 1735–1756. [Google Scholar] [CrossRef]
- Wallace, D. H., & Barbach, L. G. (1974). Preorgasmic group treatment. Journal of Sex & Marital Therapy, 1, 146–154. [Google Scholar] [CrossRef]
- Ware, J. E., Kosinski, M., & Keller, S. D. (1996). A 12-item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Medical Care, 34, 220–233. [Google Scholar] [CrossRef]
- Ware, J. E., & Sherbourne, C. D. (1992). A 36-item short-form health survey (SF-36), I: Conceptual framework and item selection. Medical Care, 30, 476–483. [Google Scholar] [CrossRef]
- Watson, D., & Clark, L. A. (1991). The Mood and Anxiety Symptom Questionnaire (MASQ). APA PsycTests. [Google Scholar] [CrossRef]
- Watson, D., Clark, L. A., & Tellegen, A. (1988). Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology, 54, 1063–1070. [Google Scholar] [CrossRef]
- Wei, Q., Zhang, H., Fan, S., & Yip, P. (2022). Dyadic association between sexual dysfunction and sexual satisfaction: A cross-sectional survey of heterosexual couples in Hong Kong. Journal of Sex & Marital Therapy, 47(4), 341–352. [Google Scholar] [CrossRef]
- Weiss, P., & Brody, S. (2011). International Index of Erectile Function (IIEF) scores generated by men or female partners correlate equally well with own satisfaction (sexual, partnership, life, and mental health). The Journal of Sexual Medicine, 8, 1404–1410. [Google Scholar] [CrossRef] [PubMed]
- White, S. E., & Reamy, K. (1982). Sexuality and pregnancy: A review. Archives of Sexual Behavior, 11(5), 429–444. [Google Scholar] [CrossRef] [PubMed]
- WHOQoL Group. (1998). Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychological Medicine, 28, 551–558. [Google Scholar] [CrossRef]
- Winter, V. R., O’Neill, E. A., Cook, M., Rose, K. L., & Hood, A. (2020). Sexual function in hook-up culture: The role of body image. Body Image, 34, 135–144. [Google Scholar] [CrossRef]
- Wiśniewski, M., & Zabłocka-Żytka, L. (2021). Sexual and mental health of woman suffering from selected connective tissue diseases: An original paper. Clinical Rheumatology, 40(8), 3319–3327. [Google Scholar] [CrossRef]
- Witting, K., Santtila, P., Alanko, K., Harlaar, N., Jern, P., Johansson, A., Von Der Pahlen, B., Varjonen, M., Algars, M., & Sandnabba, N. K. (2008a). Female sexual function and its associations with number of children, pregnancy, and relationship satisfaction. Journal of Sex & Marital Therapy, 34, 89–106. [Google Scholar] [CrossRef]
- Witting, K., Santtila, P., Jern, P., Varjonen, M., Wager, I., Höglund, M., Johansson, A., Vikstrom, N., & Sandnabba, N. K. (2008b). Evaluation of the Female Sexual Function Index in a population based sample from Finland. Archives of Sexual Behavior, 37, 912–924. [Google Scholar] [CrossRef]
- Wongsomboon, V., Burleson, M. H., & Webster, G. D. (2020). Women’s orgasm and sexual satisfaction in committed sex and casual sex: Relationship between sociosexuality and sexual outcomes in different sexual contexts. The Journal of Sex Research, 57, 285–295. [Google Scholar] [CrossRef]
- Wood, A., Runciman, R., Wylie, K. R., & McManus, R. (2012). An update on female sexual function and dysfunction in old age and its relevance to old age psychiatry. Aging and Disease, 3(5), 373–384. [Google Scholar]
- World Health Organization. (2002). Defining sexual health: Report of a technical consultation on sexual health 28–31 January 2002, Geneva. World Health Organization. Available online: https://www3.paho.org/hq/dmdocuments/2009/defining_sexual_health.pdf (accessed on 25 April 2025).
- Wójcik, N., & Rogowska, A. (2022). The level of sexual satisfaction and life satisfaction during the second wave of the COVID-19 pandemic in Poland. Epidemiological Review/Przegląd Epidemiologiczny, 76(4), 458–468. [Google Scholar] [CrossRef] [PubMed]
- Yangin, H. B., Sözer, G. A., Şengün, N., & Kukulu, K. (2008). The relationship between depression and sexual function in menopause period. Maturitas, 61, 233–237. [Google Scholar] [CrossRef] [PubMed]
- Yanikkerem, E., Goker, A., Ustgorul, S., & Karakus, A. (2016). Evaluation of sexual functions and marital adjustment of pregnant women in Turkey. International Journal of Impotence Research, 28, 176–183. [Google Scholar] [CrossRef] [PubMed]
- Yela, D. A., Soares, P. M., & Benetti-Pinto, C. L. (2018). Influence of sexual function on the social relations and quality of life of women with premature ovarian insufficiency. Revista Brasileira de Ginecologia e Obstetrícia/RBGO Gynecology and Obstetrics, 40, 066–071. [Google Scholar] [CrossRef]
- Yeoh, S. H., Razali, R., Sidi, H., Razi, Z. R. M., Midin, M., Jaafar, N. R. N., & Das, S. (2014). The relationship between sexual functioning among couples undergoing infertility treatment: A pair of perfect gloves. Comprehensive Psychiatry, 55, S1–S6. [Google Scholar] [CrossRef]
- Young, M., Denny, G., Luquis, R., & Young, T. (1998). Correlates of sexual satisfaction in marriage. Canadian Journal of Human Sexuality, 7, 115–128. Available online: https://www.researchgate.net/profile/Raffy_Luquis/publication/281691542_Correlates_of_sexual_satisfaction_in_marriage/links/5693e45d08ae3ad8e33b3f5d/Correlates-of-sexual-satisfaction-in-marriage.pdf (accessed on 25 April 2025).
- Zhang, H., Fan, S., & Yip, P. S. F. (2015). Sexual dysfunction among reproductive-aged Chinese married women in Hong Kong: Prevalence, risk factors, and associated consequences. Journal of Sexual Medicine, 12, 738–745. [Google Scholar] [CrossRef]
- Zhou, M. (1993). A survey of sexual states of married, healthy, reproductive age women. Journal of Psychology & Human Sexuality, 6, 15–28. [Google Scholar] [CrossRef]
- Zigmond, A. S., & Snaith, R. P. (1983). The hospital anxiety and depression scale. Acta Psychiatrica Scandinavia, 67, 361–370. [Google Scholar] [CrossRef]
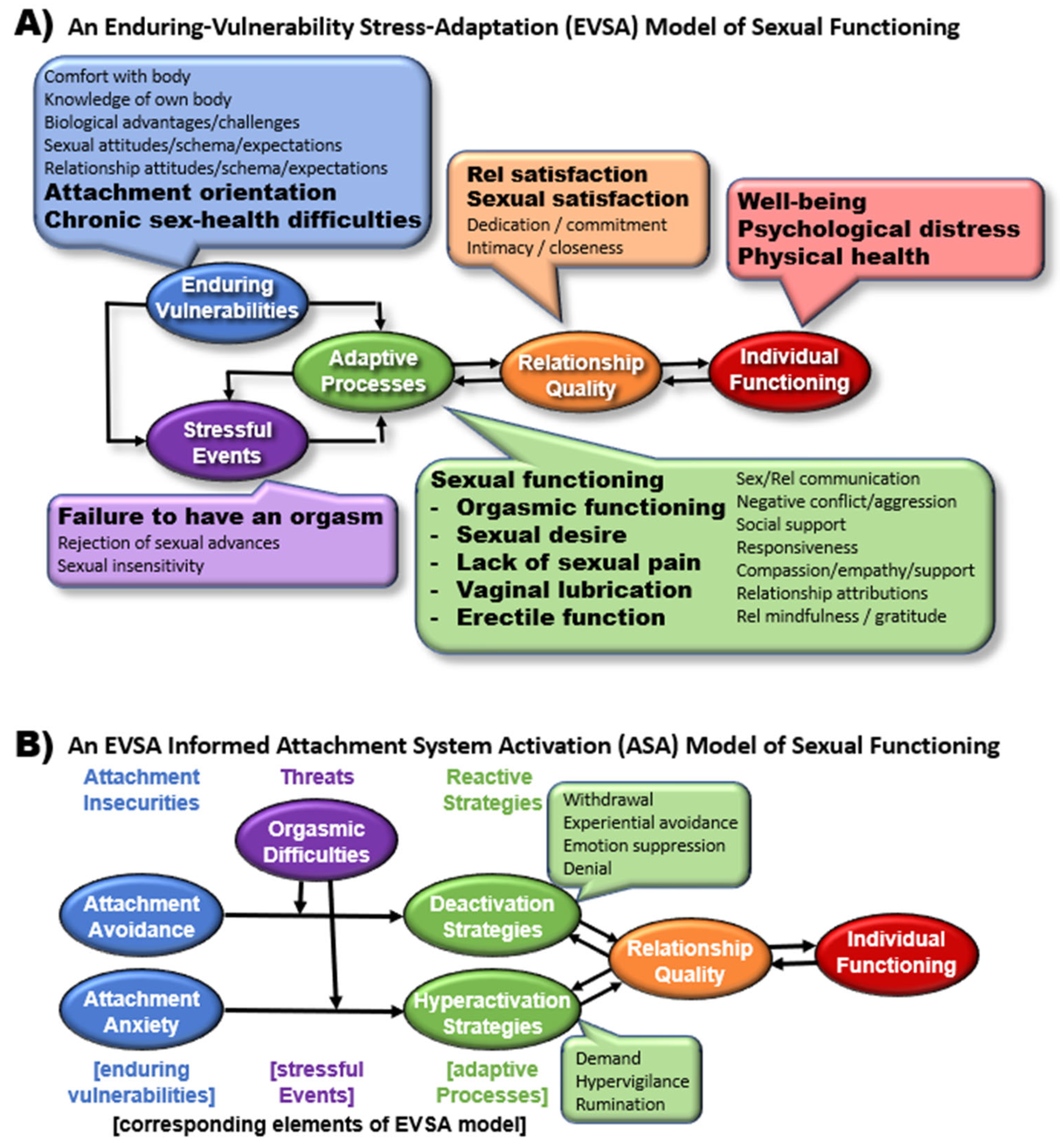
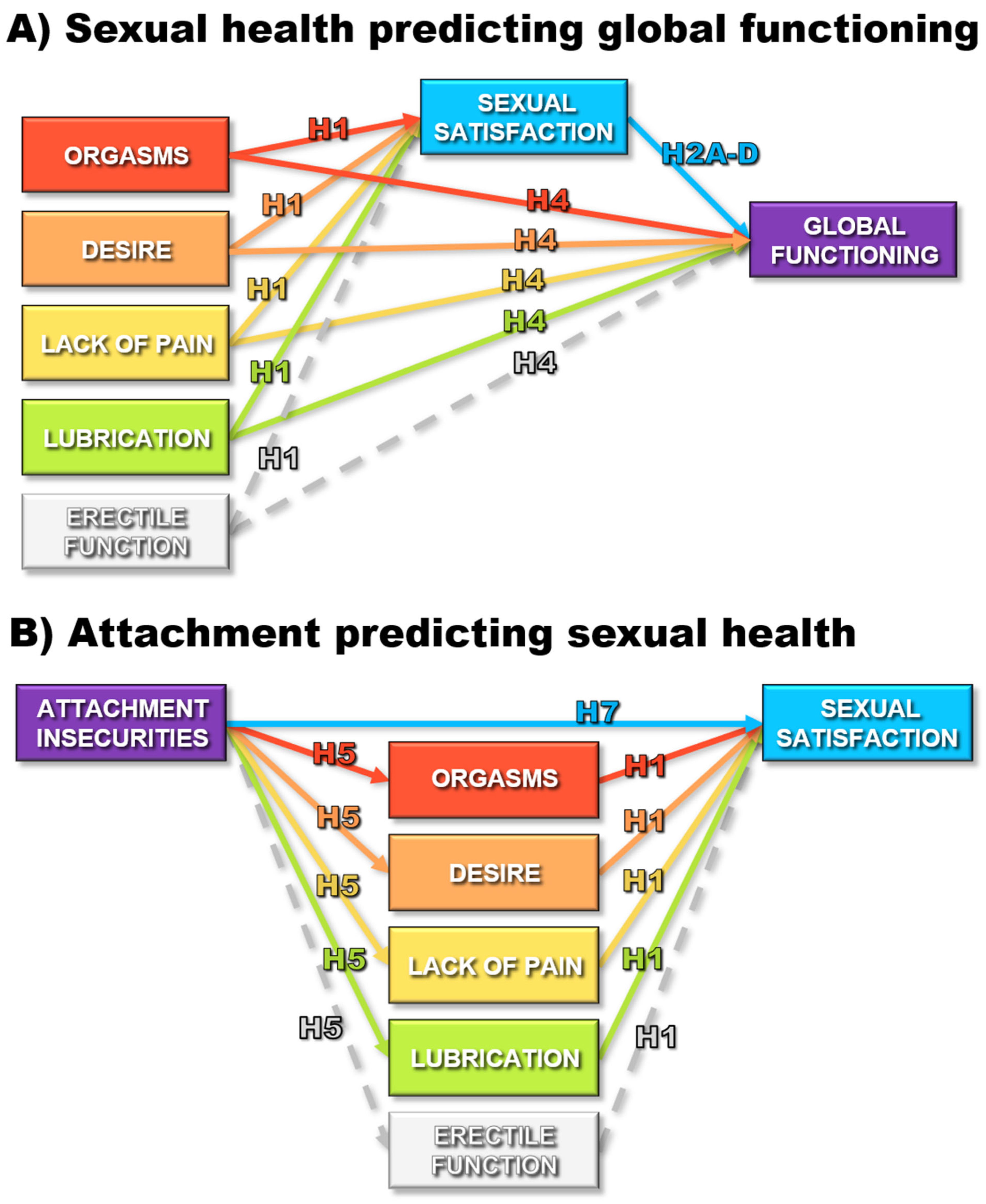
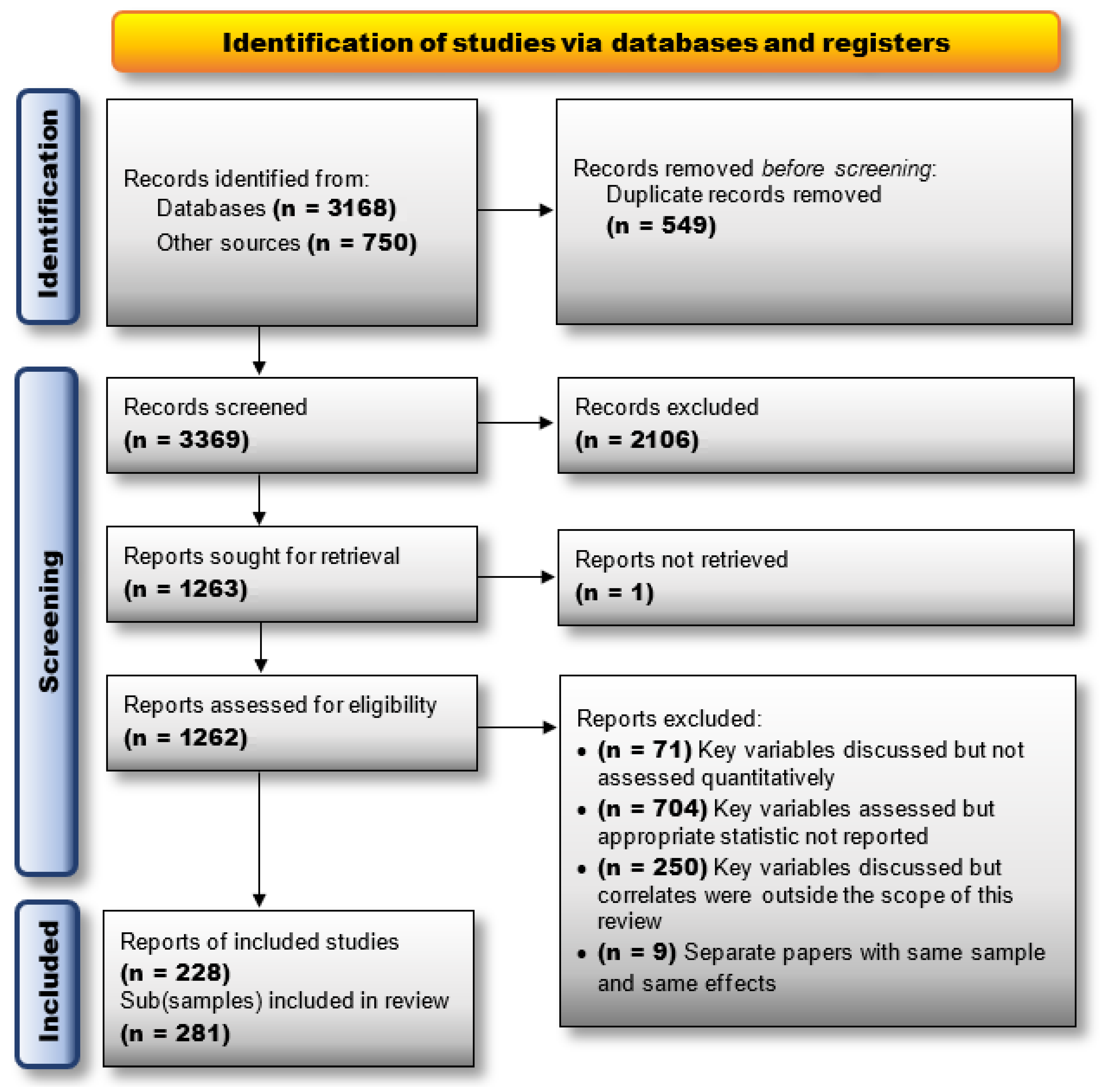
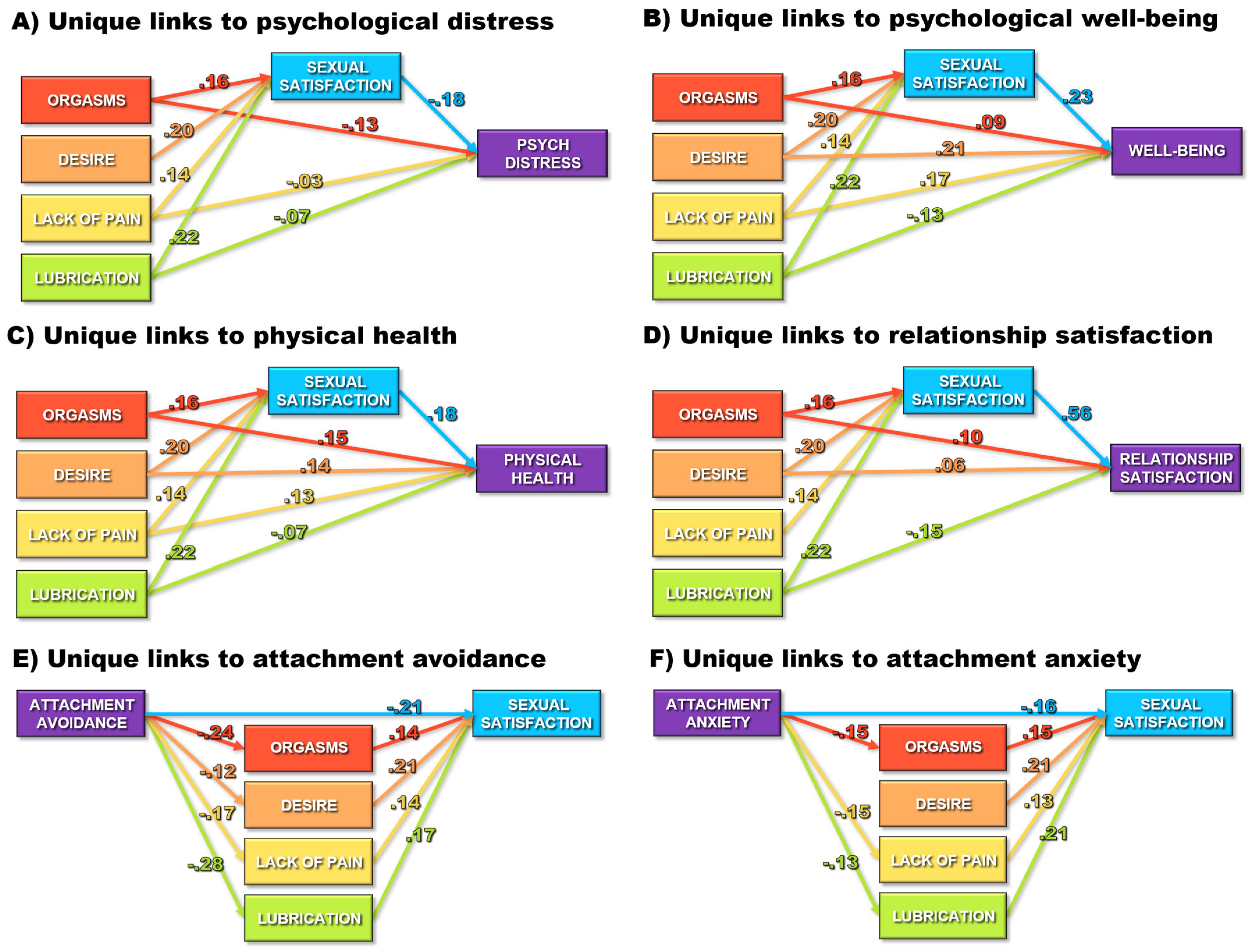
| Category | # Subsamples | Category | # Subsamples | Category/Code | # Subsamples | |
|---|---|---|---|---|---|---|
| Subset (# Reporting) | (# of Effects) | Subset | ||||
| Summary | Clinical population 2 | Country | ||||
| Distinct samples | 281 | Addison’s disease | 1 | Australia | 4 | |
| Unique subjects | 248,021 | Ankylosing spondylitis | 2 | Belgium | 2 | |
| Distinct effects | 1201 | Brain or spinal cord injury | 4 | Brazil | 9 | |
| Publication type | Cancer | 7 | Bulgaria | 1 | ||
| Peer-reviewed article | 260 | Chronic pain | 4 | Canada | 27 | |
| Thesis/dissertation | 21 | Depression &/or anxiety | 9 | Chile | 2 | |
| Publication year | Dialysis | 2 | China/Hong Kong | 10 | ||
| 1971–1990 | 7 | Fertility treatment | 5 | Czech Republic | 5 | |
| 1991–2000 | 10 | Gynecological disorders | 11 | Denmark | 2 | |
| 2001–2010 | 47 | Heart disease/hypertension | 4 | Egypt | 1 | |
| 2011–2020 (February) | 141 | Heroin use | 1 | Finland | 5 | |
| 2020 (February) to 2025 (October) | 76 | Hyperthyroidism | 1 | Germany | 4 | |
| Sex Health 1 | Incontinence | 1 | Greece | 1 | ||
| Sexual Satisfaction | (471) | Lupus | 1 | Hungary | 1 | |
| Orgasm | (474) | Metabolic syndrome | 1 | India | 1 | |
| Desire | (358) | Migraines | 1 | International | 2 | |
| Lack of pain | (184) | Multiple sclerosis | 4 | Iran | 9 | |
| Lubrication | (195) | Nonspecific medical 3 | 2 | Israel | 5 | |
| Erectile function | (51) | Obesity &/or eating disorder | 3 | Italy | 12 | |
| Correlate | Parkinson’s disease | 1 | Japan | 1 | ||
| Psychological distress | (329) | Pre-, post-, &/or menopausal | 8 | Malaysia | 3 | |
| Psychological well-being | (85) | Pregnant &/or postpartum | 9 | Mexico | 1 | |
| Physical health | (58) | PTSD | 1 | Morocco | 1 | |
| Attachment anxiety | (41) | Renal transplant | 1 | Netherlands | 5 | |
| Attachment avoidance | (41) | Rheumatoid arthritis | 1 | Norway | 2 | |
| Relationship satisfaction | (169) | Schizophrenia | 2 | Poland | 7 | |
| Type of population 2 | Sexual abuse | 2 | Portugal | 12 | ||
| College students | 16 | Sexual dysfunction | 12 | Scotland | 1 | |
| Community | 145 | Sjogren’s syndrome | 1 | South Korea | 1 | |
| Clinical | 120 | Sleep apnea | 2 | Spain | 4 | |
| Gender | Stroke | 1 | Sweden | 3 | ||
| Female only study | 183 | Vitamin D3 deficiency | 1 | Switzerland | 3 | |
| Male only study | 60 | Other medical | 6 | Taiwan | 2 | |
| Both genders | 38 | Average age (k = 199) | Turkey | 21 | ||
| Weighted percent female | 75% | Lowest | 14.6 | UK | 5 | |
| Relationship length (k = 41) | Highest | 73.5 | US | 88 | ||
| Lowest | 1.1 | Weighted mean | 37.1 | Other | 18 | |
| Highest | 34.1 | In a relationship (k = 211) | Caucasian | |||
| Weighted mean | 8.0 | Weighted % | 77.1 | Weighted % | 63.80% | |
| Author (Year) | Record Type | N | Country | Subsample | Mean Age | Percent White | Sex Health Dimension(s) | Sex Health Scale(s) | Correlate Dimension | Correlate Scale | # Effects |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Abdel-Hamid and Saleh (2011) | PR | 38 | Egypt | Muslim males w/lifelong delayed ejaculation | 30.8 | 0 | O | IIEF | depressive sxs | SRADM | 1 |
| Abedi et al. (2015) | PR | 228 | Iran | Women w/& w/out abnormal sexual function | 30.4 | 0 | SODPL | FSFI | perceived stress | PSS | 5 |
| Adam et al. (2020) | PR | 65 | Belgium | Women aged 18–58 w/orgasm difficulties | 32.7 | 100 | SO | FSFI | only sex health * | 1 | |
| Aerts et al. (2015) | PR | 84 | Belgium | Women w/endometrial cancer | 63.0 | 100 | O | SSFS | relationship sat | DAS | 1 |
| Alvisi et al. (2014) | PR | 204 | Italy | Women w/& w/out metabolic syndrome | 40.0 | 100 | O | FSFI | depressive sxs | MHQ | 2 |
| Appa et al. (2014) | PR | 1997 | US | Middle-aged women w/multiple medical diagnoses | 60.2 | 36 | SODPL | 1 item | depression diagnosis | medical diagnosis | 5 |
| Artune-Ulkumen et al. (2014) | PR | 177 | Turkey | Women in sexual relationships w/& w/o sexual dysfunction | 32.3 | 0 | SODPL | FSFI | mental health, vitality, physical health | SF-36 | 15 |
| Asselmann et al. (2016) | PR | 149 | Germany | Pregnant women w/& w/o depression | 28.9 | 100 | SODL | MGH | depression diagnosis | CIDI | 4 |
| Assimakopoulos et al. (2006) | PR | 110 | Greece | Healthy women & obese women preparing for bariatric surgery | 34.4 | 100 | SODPL | FSFI | depressive sxs | BDI | 5 |
| Atis et al. (2011) | PR | 80 | Turkey | Women w/& w/o hyperthyroidism | 36.8 | 0 | SODPL | FSFI | depressive sxs | BDI | 5 |
| Aubin et al. (2008) | PR | 72 | US | Men w/chronic pelvic pain syndrome | 40.8 | 66 | O | BSFQ | depressive sxs | CESD | 1 |
| Bakhtiari et al. (2016) | PR | 236 | Iran | Women in fertility treatment | 26.4 | 0 | SOD | DSM-IV | relationship sat | 1 item | 4 |
| Barbara et al. (2016) | PR | 269 | Italy | Women who have given birth 6 mo. ago | 34.4 | 100 | SO | FSFI | only sex health * | 1 | |
| Barrientos and Páez (2006) | PR | 4339 | Chile | Women & men aged 18–69 | 39.7 | 0 | SO | 1 item | only sex health * | 2 | |
| Battaglia et al. (2011) | PR | 87 | Italy | Menstruating women | 28.7 | 100 | O | 1 item | depressive sxs | BDI | 1 |
| Beaber and Werner (2009) | PR | 120 | US | Women in heterosexual & lesbian relationships | 29.4 | 77 | SODPL | FSFI | only sex health * | 16 | |
| Berenguer et al. (2019) | PR | 149 | Portugal | Adult women | 25.0 | 0 | SO | FSFI | only sex health * | 1 | |
| Blair et al. (2018) | PR | 750 | Canada | Women & men in same or opposite sex relationships | 30.0 | 0 | SO | IIEF | only sex health * | 2 | |
| Borissova et al. (2001) | PR | 627 | Bulgaria | Middle-aged pre- & post-menopausal women w/& w/o hormone replacement therapy | 48.0 | 100 | O | 1 item | coping with life | 1 item | 1 |
| Brody and Weiss (2011) | PR | 1570 | Czech Republic | Women & men aged 35–65 in relationships | 48.8 | 100 | SO | 1 item | life sat, relationship sat | LiSat | 6 |
| Burleson et al. (2007) | PR | 58 | US | Middle-aged women | 47.6 | 0 | O | 1 item | Depressive sx, positive affect | 1 item, 7 items | 2 |
| Burri et al. (2015) | PR | 507 | UK | Pre- & post-menopausal twin women | 56.3 | 100 | SODPL | FSFI | relationship sat | 1 item | 14 |
| Burri et al. (2013) | PR | 866 | UK | Monozygotic twin women discordant for sexual dysfunction | 55.0 | 100 | SODPL | FSFI | relationship sat | 1 item | 5 |
| Cagnacci et al. (2020) | PR | 518 | Italy | Sexually active women aged 40–55 at gynecological clinics | 49.4 | 100 | SO | FSFI | only sex health * | 1 | |
| Canat et al. (2016) | PR | 108 | Turkey | Women aged 22–51 w/vitamin D3 deficiency | 34.9 | 0 | SODPL | FSFI | depressive sx | BDI | 5 |
| Carmen (2014) | MT | 145 | US | Adult women | 25.8 | 0 | SODPL | FSFI | only sex health * | 10 | |
| Carrobles et al. (2011) | PR | 157 | Spain | College women aged 20–45 | 22.8 | 0 | SO | 3 items | mental health | WHO-5 | 3 |
| Castellini et al. (2010) | PR | 309 | Italy | Obese & not obese women w/& w/o Binge ED | 39.1 | 100 | SODPL | FSFI | depressive sx | BDI | 15 |
| Ceyhan et al. (2019) | PR | 102 | Turkey | Married women in treatment for hypertension | 55.1 | 0 | SOD | ASEX | relationship sat | MAT | 3 |
| S. Chang et al. (2012) | PR | 555 | Taiwan | Pregnant women | 33.0 | 0 | SODPL | FSFI | depressive sx | CESD | 5 |
| S. R. Chang et al. (2019) | PR | 1026 | Taiwan | Women aged 40–65 | 48.5 | 0 | SODPL | FSFI | mental health, physical health | SF-12, SF-12 | 10 |
| Cheng et al. (2007) | PR | 160 | China | Sexually active men aged 50+ from a primary care treatment center | 55.0 | 0 | SOE | IIEF | depressive sx | GDS | 3 |
| Chivers et al. (2011) | PR | 57 | Canada | Post-partum women w/& w/o depression | 34.3 | 0 | SODPL | FSFI | depressive sxs | EPDS | 5 |
| D. L. Cohen and Belsky (2008) | PR | 323 | UK | Adult women | 24.4 | 70 | O | 4 items | attachment | ECR | 2 |
| K. Conroy (2018) | MT | 158 | US | Women w/gynecologic or breast cancer | 57.7 | 92 | SO | DSFI; 1 item | depressive sxs, relationship sat | CESD, single item? | 3 |
| Constantine (2017) | DD | 531 | US | Adult women | 27.0 | 78 | SO | ISS, 1 item | psychological sxs, attachment, relationship sat | BSI, ECR, RAS | 7 |
| Costa and Brody (2007) | PR | 30 | Portugal | Women currently in sexual relationships | 25.8 | 0 | SO | 1 item | relationship sat | PRQC | 2 |
| Costa and Brody (2011) | PR | 70 | Scotland | College sexually experienced women | 25.7 | 100 | O | 1 item | attachment | ECR | 2 |
| Costa et al. (2016) | PR | 116 | Portugal | Adult women & men | 24.9 | 0 | SO | 1 item | only sex health * | 2 | |
| Dashti et al. (2016) | PR | 16 | Malaysia | Women aged 28–48 w/PCOS | 33.4 | 0 | SODPL | FSFI | depressive sxs | DASS-21 | 5 |
| Davidson and Hoffman (1986) | PR | 206 | US | Married undergrad & graduate women | 28.1 | 0 | SO | 1 item | only sex health * | 1 | |
| de Jong (2016) | DD | 220 | US & Canada | Couples w/o current sexual, medical, or psychiatric diagnoses or treatments | 26.5 | 86 | SO | 2 items | only sex health * | 1 | |
| de Lucena and Abdo (2014) | PR | 96 | Brazil | Women attending routine gynecology checkup | 38.5 | 0 | SOD | FSQ | anxiety sxs | BAI | 3 |
| de Oliveira Ferro et al. (2019) | PR | 46 | Brazil | Men aged 18–60 w/spinal cord injury | 34.0 | 0 | SO | IIEF | only sex health * | 2 | |
| Demir et al. (2013) | PR | 23 | Turkey | Women w/ankylosing spondylitis | 39.3 | 0 | SODPL | FSFI | depressive sxs, vitality, physical health | BDI, SF-36, SF-36 | 15 |
| Denes (2012) | PR | 200 | US | Undergrad women & men from U of California, Santa Barbara | 19.6 | 59 | O | 1 item | relationship sat | MOQ | 1 |
| Denes (2018) | PR | 206 | US | Female & male college students | 19.3 | 68 | O | 1 item | relationship sat | MOQ | 2 |
| Dèttore et al. (2013) | PR | 130 | Italy | Women w/& w/out anxiety diagnoses | 29.5 | 100 | SODPL | FSFI | anxiety sxs | STAI | 10 |
| Dissiz (2018) | PR | 57 | Turkey | Women heroin users | 26.2 | 0 | SODPL | FSFI | depressive sxs | BDI | 7 |
| Dogan et al. (2017) | PR | 142 | Turkey | Women w/& w/o migraines | 34.0 | 0 | OL | FSFI | depressive sxs | BDI | 2 |
| Duits et al. (2009) | PR | 19 | Netherlands | Men w/history of strokes | 58.8 | 100 | SODE | IIEF | depressive sxs | SCL | 4 |
| Dunkley et al. (2016) | PR | 576 | Canada | Undergrad women from U of British Columbia | 20.8 | 37 | SODPL | FSFI | attachment | ECR | 10 |
| Dunn et al. (1999) | PR | 613 | UK | Women aged 18–75 | 50.0 | 0 | OL | 1 item, 1 item | depressive sxs, marital difficulties | HAD, 1 item | 4 |
| Dyar et al. (2020) | PR | 279 | US | Sexual and gender minority individuals assigned female at birth who had been in sexual or romantic relationships within the last 6 mo. | 21.2 | 19 | SO | 3 items, 2 items | relationship sat | RAS | 3 |
| Eaton et al. (2017) | PR | 70 | US | Women w/gynecologic cancer | 53.0 | 80 | OP | WSIDI | depressive sxs | PHQ | 2 |
| Eichel et al. (1988) | PR | 86 | US | Men & women who had or had not learned & practiced the coital alignment technique | 41.1 | 0 | SO | 1 item | only sex health * | 1 | |
| Ellero (2019) | MT | 330 | International | Portuguese or English speaking, sexually active women & men | 28.4 | 0 | SOD | 1 item | only sex health * | 4 | |
| Ellsworth and Bailey (2013) | PR | 112 | US | Female undergraduate students in relationships | 18.8 | 0 | O | 1 item | relationship sat | RAS | 1 |
| Fabre and Smith (2012) | PR | 281 | US | Women w/depression | 38.3 | 88 | OD | CSFQ | depressive sxs | HAMD | 2 |
| Fabre et al. (2013) | PR | 326 | US | Men w/major or atypical depression | 39.5 | 80 | OD | DISF | depressive sxs | HAMD | 2 |
| Fan et al. (2007) | PR | 64 | US | Women & men w/schizophrenia in outpatient treatment | 43.5 | 70 | SOD | CSFQ | depressive sxs, quality of life | HAMD, QOL | 12 |
| Forbes et al. (2016) | PR | 336 | Australia | Sexually active women aged 19–65 | 29.5 | 100 | SO | FSFI | depressive sxs, | DASS | 2 |
| Frederick et al. (2017) | PR | 38747 | US | Heterosexual women & men in a relationship for at least 3 years | 39.4 | 87 | SO | 1 item | only sex health * | 4 | |
| Gallup et al. (2014) | PR | 54 | US | Heterosexual undergrad women in sexual relationships | 19.0 | 0 | SO | 1 item | only sex health * | 1 | |
| Gracia et al. (2007) | PR | 311 | US | Women enrolled in the Penn Ovarian Aging Study | 48.0 | 51 | SODL | FSFI | anxiety sxs | ZAI | 4 |
| Gewirtz-Meydan (2017) | PR | 256 | Israel | Heterosexual couples (dyads) | 34.4 | 87 | SOD | ISS, ISBI | only sex health * | 6 | |
| Gewirtz-Meydan and Finzi-Dottan (2018) | PR | 256 | Israel | Married or cohabitating couples, together 3+ yrs & co-parenting 1+ children (dyads) | 34.4 | 0 | SOD | ISS, 3 items | attachment | ECR | 12 |
| Gomes and Nobre (2012) | PR | 1363 | Portugal | Sexually active men w/& w/o erectile dysfunction | 37.7 | 0 | SODE | IIEF | only sex health * | 6 | |
| Goodman (2011) | DD | 1576 | US | Adult women & men collected online | 32.0 | 79 | O | 1 item | attachment, relationship sat | ECR, PRQC | 3 |
| Granata et al. (2013) | PR | 12 | Italy | Men aged 21–59 w/Addison’s disease | 40.5 | 100 | SOD | IIEF | only sex health * | 2 | |
| Grose (2016) | DD | 430 | US | Heterosexual undergrad women w/a sex partner in the last year | 19.9 | 38 | SO | MSSCQ-S, FSFI | only sex health * | 2 | |
| Gunst et al. (2017) | PR | 2173 | Finland | Twin women | 25.5 | 100 | SODPL | FSFI | only sex health * | 10 | |
| Guo et al. (2004) | PR | 13498 | China | Newlywed women & men in Shanghai (dyads) | 27.8 | 0 | SO | 1 item | relationship sat | 1 item | 4 |
| Gutsche and Burri (2017) | PR | 159 | Switzerland | Adult women | 31.8 | 100 | SODPL | FSFI | relationship sat, | RAS | 15 |
| Haavio-Mannila and Kontula (1997) | PR | 2250 | Finland | Women & men aged 18–74 | 42.2 | 100 | SO | 2 items | only sex health * | 2 | |
| Harte and Meston (2012) | PR | 1207 | US | Undergrad sexually active men using & not using ED meds | 21.9 | 73 | SODE | IIEF | only sex health * | 6 | |
| Hassan et al. (2008) | PR | 354 | Turkey | Men w/erectile dysfunction | 37.9 | 0 | SO | IIEF | only sex health * | 1 | |
| Hazewinkel et al. (2012) | PR | 76 | Netherlands | Women w/history of vulvar cancer & radiotherapy | 68.0 | 100 | SOD | FSFI | physical health | SF-36 | 3 |
| Hevesi et al. (2017) | PR | 508 | Hungary | Undergrad women & patients w/endometriosis or PCOS | 27.9 | 100 | SODPL | FSFI | only sex health * | 10 | |
| Hevesi et al. (2020) | PR | 1843 | US & Hungary | Adult women | 28.8 | 0 | SO | 1 item | relationship sat | 1 item | 2 |
| Horton (1982) | DD | 99 | US | Women in relationships | 27.5 | 97 | SO | SII 1 item | only sex health * | 1 | |
| Hoyer et al. (2009) | PR | 451 | Germany | CBT outpatients w/anxiety or depression diagnosis | 36.0 | 100 | SODLE | MGH | only sex health * | 9 | |
| Hurlbert et al. (1993) | PR | 98 | US | Fort Hood, TX military wives | 26.7 | 68 | SOD | ISS, 1 item | only sex health * | 3 | |
| Hwang et al. (2019) | PR | 32 | South Korea | Women w/& w/o stress urinary incontinence | 41.7 | 0 | SO | FSFI | only sex health * | 1 | |
| Jensen et al. (2004) | PR | 75 | Denmark | Gynecological cancer patients (cervical, endometrial, ovarian) aged 28–77 | 58.0 | 100 | SOL | SVQ | only sex health * | 2 | |
| Jones et al. (2018) | PR | 284 | US | Heterosexual couples (dyads) | 32.4 | 90 | SO | NSSS-S, 1 item | only sex health * | 2 | |
| Kahn (2001) | DD | 104 | US | Married women aged 25–40 | 31.7 | 0 | SO | ISS, 1 item | only sex health * | 1 | |
| Kalmbach and Pillai (2014) | PR | 136 | US | Adult women | 20.7 | 82 | OP | FSDS-R | depressive sxs | CESD | 2 |
| Kalmbach et al. (2012) | PR | 1258 | US | Undergrad women & men from Kent State U w/depression &/or anxiety | 19.6 | 0 | SODPLE | FSFI/MSFI, PFSF | general distress | MASQ | 3 |
| Kalmbach et al. (2015) | PR | 171 | US | College women free of antidepressants | 20.1 | 81 | ODL | FSFI | depressive sxs | CESD | 22 |
| Kalmbach et al. (2019) | PR | 150 | US | Postmenopausal women w/chronic insomnia | 56.4 | 52 | SODPL | FSFI | depressive sxs | BDI | 5 |
| Karabulutlu et al. (2011) | PR | 33 | Turkey | Women getting hemodialysis | 41.0 | 0 | SODPL | FSFI | depressive sxs | BDI | 5 |
| Kelley and Gidycz (2017) | PR | 501 | US | Undergrad women from Ohio U w/& w/o history of sexual assault | 18.9 | 88 | ODPL | FSFI | depressive sxs | TSC-D | 10 |
| Keskin et al. (2019) | PR | 225 | Turkey | Dialysis patients | 43.0 | 0 | SOE | GRISS | depressive sxs | BSI | 3 |
| Khajehei et al. (2015) | PR | 295 | Australia | Postpartum women | 29.7 | 0 | SO | FSFI | depressive sxs, relationship sat | PHQ, RAS | 3 |
| Khnaba et al. (2016) | PR | 60 | Morocco | Women w/rheumatoid arthritis | 45.2 | 0 | SODPL | FSFI | depressive sxs, vitality, physical health | HADS-D, SF-36, SF-36 | 15 |
| Klapilová et al. (2015) | PR | 170 | Czech Republic | Heterosexual couples (dyads) | 27.1 | 100 | SO | 1 item | relationship sat | DAS | 4 |
| Kračun et al. (2019) | PR | 200 | Israel | Women aged 21–44 attending antenatal classes | 30.5 | 0 | SODPL | FSFI | relationship sat | EMS | 10 |
| Kreuter et al. (1998) | PR | 84 | Sweden | Women & men post traumatic brain injury | 40.0 | 100 | SO | SIS, 1 item | only sex health * | 4 | |
| Leeners et al. (2014) | PR | 299 | Switzerland | Adult women | 50.0 | 100 | O | 1 item | depressive sxs | SCL | 1 |
| Leonhardt et al. (2018) | PR | 3366 | US | Heterosexual newlywed couples (dyads) | 28.6 | 62 | SO | GRISS, 1 item | relationship sat | CSI | 4 |
| Lew-Starowicz and Rola (2014) | PR | 204 | Poland | Women & men w/multiple sclerosis | 50.3 | 100 | SODPLE | SFQ | depressive sxs | BDI | 9 |
| Llaneza et al. (2011) | PR | 117 | Spain | Post-menopausal women | 57.0 | 0 | OD | CSFQ | depressive sxs | CESD | 2 |
| Madewell (2013) | DD | 243 | US | Undergrad women from Oklahoma State U | 19.6 | 69 | SODP | GSF | only sex health * | 6 | |
| Maes (2017) | DD | 92 | US | Men enrolled in Osher Lifelong Learning Institute at U of Nevada, Las Vegas | 73.5 | 89 | SOE | MSHQ | perceived stress | PSSI | 3 |
| Masmoudi et al. (2018) | PR | 52 | Tunisia | Women aged 27–57 w/& w/out multiple sclerosis | 37.7 | 0 | SODPL | FSFI | depressive sxs | BDI | 5 |
| McNicoll et al. (2017) | PR | 137 | Canada | Women reporting pain during sex | 32.2 | 0 | SO | FSFI | only sex health * | 1 | |
| Meadow (1982) | DD | 95 | US | Arizona married female community college students | 38.5 | 0 | SO | SIS | relationship sat | MAT | 3 |
| Mendes et al. (2008) | PR | 90 | Brazil | Men w/spinal cord injury—retroactive pre-injury report | 33.5 | 0 | SODE | 1 item | only sex health * | 3 | |
| Mernone et al. (2019) | PR | 93 | Switzerland | Women aged 40–73 | 52.5 | 100 | SODPL | FSFI | life sat, relationship sat | SWLS, RAS | 10 |
| Monga et al. (1998) | PR | 82 | US | Women &men aged 29–74 in treatment for chronic pain | 49.9 | 67 | O | DISF | depressive sxs | CESD | 1 |
| Morales et al. (2013) | PR | 65 | Spain | Women w/lupus | 39.0 | 0 | SODPL | FSFI | depressive sxs, vitality, physical health | SCL, SF-36, SF-36 | 15 |
| Moshfeghy et al. (2020) | PR | 100 | Iran | Sexually active married women w/& w/out recurrent vulvovaginal candidiasis | 31.5 | 0 | SODPL | FSFI | depressive sxs | DASS-21 | 5 |
| Najafabady et al. (2011) | PR | 1200 | Iran | Reproductive aged women | 29.9 | 0 | SO | FSFI | anxiety | --- | 2 |
| Nascimento et al. (2015) | PR | 157 | Brazil | Hypertensive women | 56.4 | 0 | SODPL | FSFI | depressive sxs | HADS-D | 15 |
| Norhayati and Azman Yacob (2017) | PR | 321 | Malaysia | Women w/& w/out severe delivery complications | 30.2 | 0 | SO | FSFI | only sex health * | 1 | |
| Onem et al. (2008) | PR | 26 | Turkey | Patients w/obstructive sleep apnea-hypopnea | 45.8 | 0 | SODPL | FSFI | depressive sxs | BDI | 5 |
| E. A. Opperman et al. (2013) | PR | 85 | Canada | Undergrad women in relationship | 20.8 | 100 | SODPL | FSFI | only sex health * | 10 | |
| Özcan et al. (2015) | PR | 89 | Turkey | Adults w/Parkinson’s disease | 67.7 | 0 | ODLE | ASEX | depressive sxs | HAMD | 4 |
| Özdemir et al. (2007) | PR | 98 | Turkey | Women & men w/renal transplants | 36.1 | 0 | OD | ASEX | depressive sxs | BDI | 3 |
| Pakpour et al. (2015) | PR | 131 | Iran | Peri-menopausal women at a health center | 55.8 | 0 | SODPL | FSFI | stress, relationship sat | --- | 20 |
| Papini et al. (2013) | PR | 44 | Italy | College women aged 21–47 | 26.1 | 100 | SODPL | FSFI | depressive sxs | SCL | 5 |
| Parish et al. (2007) | PR | 2411 | China | Sexually active women & men aged 20–64 in long-term relationships | 40.4 | 0 | SO | 1 item | only sex health * | 2 | |
| Pascoal et al. (2018) | PR | 248 | Portugal | Women & men in heterosexual couples | 29.5 | 0 | SODLE | GMSEX, FSFI | only sex health * | 12 | |
| C. Peixoto et al. (2019) | PR | 36 | Brazil | Postmenopausal women aged 45–65 at a climacteric clinic | 55.4 | 0 | SODPL | FSFI | mental health, vitality, physical health | SF-36 | 15 |
| Philippsohn and Hartmann (2009) | PR | 102 | Germany | Adult women | 36.7 | 100 | SO | 4 items, 1 item | only sex health * | 1 | |
| Pinney et al. (1987) | PR | 275 | US | College aged sexually active heterosexual women | 20.5 | 97 | SO | PSSI, 1 item | only sex health * | 1 | |
| Pinsky (2016) | MT | 248 | US | Male combat veterans w/PTSD aged over 18 | --- | 85 | SODE | IIEF | attachment | ECR | 19 |
| Powers (2012) | DD | 835 | US | Undergrad sexually active women from U of North Texas | 21.2 | 60 | O | 1 item | depressive sxs | QIDS | 1 |
| Randolph (2002) | DD | 63 | US | Women w/endometriosis & suffering from chronic pelvic pain | 33.3 | 87 | OD | DISF | depressive sxs | CESD | 3 |
| R. Rosen et al. (2000) | PR | 259 | US | Women w/& w/o sexual arousal disorder | 40.1 | 76 | SODPL | FSFI | only sex health * | 20 | |
| N. O. Rosen et al. (2019) | PR | 193 | Canada | Women w/sexual arousal disorder & their male partners (dyads) | 31.2 | 86 | SO | FSFI | depressive sxs, relationship sat | BDI, CSI | 10 |
| Rottmann et al. (2017) | PR | 574 | Denmark | Heterosexual, sexually active couples dealing w/breast cancer (dyads) | 55.8 | 100 | SO | PROMIS | only sex health * | 2 | |
| Rowland and Kolba (2019) | PR | 2068 | US & Hungary | Adult women | 29.1 | 0 | O | 1 item | relationship sat | 1 item | 1 |
| Rowland et al. (2018) | PR | 2304 | US & Hungary | Adult women | 28.8 | 0 | SO | 1 item | depression diagnosis; relationship sat | 1 item each | 3 |
| Sakinci et al. (2016) | PR | 159 | Turkey | Sexually active women at routine gynecology visits | 33.7 | 0 | SODPL | FSFI | depressive sxs | BDI | 15 |
| Sariyildiz et al. (2013) | PR | 70 | Turkey | Men aged 20–50 w/ankylosing spondylitis | 36.4 | 0 | SODE | IIEF | depressive sxs | HADS-D | 4 |
| Sarti et al. (2010) | PR | 2087 | Italy | Women at menopausal clinics | 54.0 | 100 | O | 1 item | mental health, physical health | SF-12 | 2 |
| Scott et al. (2018) | PR | 206 | US | Women in lesbian couples | 33.7 | 73 | SO | 1 item | only sex health * | 1 | |
| Seldin et al. (2002) | PR | 493 | US | Adult women | 31.0 | 0 | O | 1 item | mental adjustment | 1 item | 1 |
| Shifren et al. (2008) | PR | 31581 | US | Women from a nationally representative sample | 49.5 | 81 | O | 3 items | depressive sxs | CSFQ | 1 |
| Skoczyński et al. (2019) | PR | 129 | Poland | Men aged 31–76 w/& w/out obstructive sleep apnea | 57.9 | 100 | SO | IIEF | depressive sxs, relationship sat | HADS-D | 5 |
| Speer et al. (2005) | PR | 55 | US | Women aged 41–69 surviving breast cancer | 53.4 | 100 | SOD | FSFI | relationship distress | MSI-R | 5 |
| Stephenson and Meston (2010) | PR | 319 | US | Women in sexually active heterosexual relationships w/& w/o sexual arousal disorder | 22.8 | 63 | SODPL | FSFI | relationship sat | DAS | 28 |
| Stephenson et al. (2012) | PR | 176 | US | Women w/& w/out history of childhood sexual abuse | 33.3 | 71 | SODPL | SSS-W, FSFI | only sex health * | 10 | |
| Stoeber and Harvey (2016) | PR | 289 | UK | College women & internet users aged 17–69 | 23.5 | 73 | SO | FSFI | only sex health * | 1 | |
| Takahashi et al. (2011) | PR | 126 | Japan | Women in partnered relationships | 38.1 | 0 | SODPL | FSFI | only sex health * | 10 | |
| Tao and Brody (2011) | PR | 158 | China | Women & men industrial workers | 40.2 | 0 | SO | MSQ, 1 item | only sex health * | 1 | |
| Tavares et al. (2017) | PR | 926 | Portugal | Sexually active heterosexual premenopausal women | 25.2 | 0 | O | 1 item | depressive sxs, positive affect, relationship sat | PANAS | 3 |
| Thakurdesai & Sawant (2018) | PR | 116 | India | Men w/& w/o depression | 32.4 | 0 | SODE | IIEF | depressive sxs | BDI | 4 |
| Therrien and Brotto (2016) | PR | 255 | Canada | Women w/sexual dysfunction | --- | 82 | O | FSFI | depressive sxs, relationship sat | BDI, 1 item | 2 |
| Tracy and Junginger (2007) | PR | 350 | US | Lesbian women | 35.5 | 86 | SODPL | FSFI | psychological sxs, relationship sat | BSI, DAS | 20 |
| Træen (2007) | PR | 42 | Norway | Heart disease patients | 58.8 | 0 | SOD | 1 item | only sex health * | 3 | |
| Tuinman et al. (2010) | PR | 93 | Netherlands | Testicular cancer patients | 29.4 | 100 | OE | IIEF | depressive sxs | CESD | 2 |
| Tutino et al. (2017) | PR | 311 | Canada | College women aged 17–38 | 19.2 | 81 | ODPL | FSFI | depressive sxs | DASS | 10 |
| Uddenberg (1974) | PR | 94 | Sweden | Pregnant women & their mothers | 100 | SO | 1 item | only sex health * | 1 | ||
| van den Brink et al. (2016) | PR | 399 | Netherlands | Undergrad women | 21.7 | 100 | SODPL | FSFI | attachment | ECR | 13 |
| van Nimwegen et al. (2015) | PR | 85 | Netherlands | Women w/& w/out Sjogren’s syndrome | 45.4 | 100 | SO | FSFI | depressive sxs | HADS-D | 2 |
| Villeda Sandoval et al. (2014) | PR | 200 | Mexico | Young adult women from Mexico City | 26.3 | 0 | O | FSFI | depression diagnosis | 1 item | 1 |
| Waite and Joyner (2001) | PR | 2195 | US | Women & men in national sample | 36.8 | 87 | SO | 1 item | relationship sat | 2 items | 4 |
| Wallace and Barbach (1974) | PR | 15 | US | Treatment of preorgasmic women | 27.5 | 88 | SO | 1 item | only sex health * | 1 | |
| Weiss and Brody (2011) | PR | 720 | Czech Republic | Women in relationships aged 35–65 | 47.6 | 100 | SO | 1 item | life sat, relationship sat | 1 item each | 3 |
| Witting et al. (2008b) | PR | 2081 | Finland | Women aged 33–43 | 37.5 | 100 | SODPL | FSFI | only sex health * | 10 | |
| Witting et al. (2008a) | PR | 2081 | Finland | Pregnant women, & women w/children | 37.5 | 100 | SOD | FSFI | relationship sat | PRQC | 5 |
| Wongsomboon et al. (2020) | PR | 1315 | US | Women reporting committed or casual sex | 23.7 | 0 | SO | SSS-W, FSFI | only sex health * | 2 | |
| Yangin et al. (2008) | PR | 300 | Turkey | Menopausal women | 53.6 | 100 | SODPL | FSFI | depressive sxs | BDI | 5 |
| Yanikkerem et al. (2016) | PR | 298 | Turkey | Pregnant married women | 27.5 | 0 | SO | GRISS | relationship sat | MAS | 3 |
| Yela et al. (2018) | PR | 80 | Brazil | Women w/premature ovarian insufficiency | 38.4 | 0 | SODPL | FSFI | mental health, physical health | WHOQoL | 10 |
| Yeoh et al. (2014) | PR | 269 | Malaysia | Married heterosexual couples in fertility treatments (dyads) | 33.2 | 0 | SODPLE | FSFI | only sex health * | 16 | |
| Young et al. (1998) | PR | 797 | US | Married women | --- | 0 | SO | 3 items, 1 item | relationship sat | 1 item | 3 |
| Zhang et al. (2015) | PR | 1518 | China | Married women | 38.9 | 0 | SODPL | 1 item | life sat, relationship sat | 1 item each | 11 |
| Zhou (1993) | PR | 1789 | China | Adult women | 37.2 | 0 | SO | 1 item | only sex health * | 1 item | 1 |
| ARTICLES PUBLISHED SINCE FEB-2020 | |||||||||||
| Lipinski and Beck (2022) | PR | 148 | US | Sexually active female undergraduate survivors of sexual violence | 22.4 | 43 | SOD | SSS-W, FSFI | only sex health * | 3 | |
| Girouard et al. (2021) | PR | 1036 | Canada | Sexually active high school students from Quebec | 14.6 | SOD | GMSEX, ASEX | only sex health * | 3 | ||
| Jolink et al. (2025) | PR | 158 | US | Individuals in romantic relationships ≥ 6 mo. | 24.7 | 75 | SO | GMSEX, 1 item | only sex health * | 1 | |
| Leavitt et al. (2021) | PR | 3314 | US | Sexually active adults in rom. relationships ≥ 2 yr. | 34.3 | 77 | SO | GMSEX, 1 item | relationship sat | CSI-4 | 6 |
| Abedi et al. (2020) | PR | 460 | Iran | Sexually active middle-aged empty-nester women | 51.7 | 0 | SODPL | LSS, FSFI | depressive sx | UCLA | 20 |
| Mangas et al. (2024) | PR | 104 (208) | Spain & Latin Am countries | Same-sex Spanish-Hispanic-Latin couples together ≥ 3 mo. | 28.0 | 0 | SO | GMSEX, ORS | relationship sat | GMREL | 6 |
| Pollard and Rogge (2022) | PR | 1241 | US | Sexually active adults in rom. relationships | 34.0 | 82 | SD | QSI-6, 4-items | depressive sxs, relationship sat | PHQ-9, CSI-8 | 9 |
| Denes et al. (2020) | PR | 319 | US | University adults in sexual relationships | 19.0 | 62 | O | 1 item | relationship sat | MOQ | 1 |
| Wei et al. (2022) | PR | 2028 | Hong Kong | Heterosexual couples | 32.0 | 0 | SODPLE | LSS, FSFI | only sex health * | 16 | |
| Busby et al. (2022) | PR | US | Adults in committed relationships ≥ 2 yr. | --- | 78 | SO | PN-RQ(mod), 1 item | relationship sat | PN-RQ | 3 | |
| Cinek et al. (2025) | PR | 112 | Turkey | Women with breast cancer and healthy controls | 52.5 | SODPL | FSFI | depressive sx | HAMD | 5 | |
| Lafortune et al. (2023) | PR | 2854 | Canada | Québécois adults from community & sex clinic | 38.1 | S | GMSEX | depressive sxs, relationship sat | K-6, DAS-4 | 4 | |
| van de Grift et al. (2020) | PR | 63 | Netherlands | Women undergoing breast reconstruction post-mastectomy | 45.0 | SL | FSFI | only sex health * | 1 | ||
| Wiśniewski and Zabłocka-Żytka (2021) | PR | 81 | Poland | Women with connective tissue diseases | 33.7 | SODPL | FSFI | depressive sxs, relationship sat, life sat, phys health | HADS-M, PERMA-Profiler | 20 | |
| Amiri et al. (2021) | PR | 185 (370) | Canada | Mixed-sex Québécois couples seeking reproductive services for infertility | 32.7 | 92 | SODPL | FSFI, IIEF | life sat, phys health, relationship sat | FertiQoL | 24 |
| A. B. Smith et al. (2022) | PR | 24 | US | Men post-myocardial infarction | 62.5 | 96 | SODE | MSFI | only sex health * | 6 | |
| Karaçin and Küçükşahin (2025) | PR | 217 | Turkey | Women who completed treatment for early-stage breast cancer | 45.0 | SODPL | FSFI | depressive sx | HADS-D | 15 | |
| Gaither et al. (2024) | PR | 1084 | US | Men engaging in receptive anal sex in the last 6 mo. | 32.0 | 70 | SODE | ASFI | depressive sx | BSI | 10 |
| Macia et al. (2025) | PR | 155 | Senegal | Sexually active women living in Dakar | 34.0 | 0 | SO | 2 single items | only sex health * | 1 | |
| Winter et al. (2020) | PR | 243 | US | Adults who have hooked up in the last month via an app | 26.8 | 80 | SODPLE | FSFI, MSHQ | only sex health * | 11 | |
| Gérard et al. (2025) | PR | 91 | Canada | Québécois cis-gender adults living with spinal cord injuries | 40.8 | SO | GMSEX, FSDS-DAO | depressive sx | BDI-II | 3 | |
| Busch et al. (2025) | PR | 215 | US | Undergraduate students in relationships ≥ 4 mo. | 23.0 | 41 | SD | NSSS-S, SDS | relationship sat | CSI | 3 |
| de Oliveira et al. (2025) | PR | 1153 | Portugal | Women in cohabiting monogamous relationships ≥ 1 yr. | 31.6 | SD | NSSS-S, SDI-2 | relationship sat | GMREL | 3 | |
| Thompson et al. (2024) | PR | 619 | US | Adults in relationships ≥ 6 mo. recruited from Mturk | 38.0 | 79 | S | NSSS | attachment | ECR | 3 |
| Boudreau et al. (2024) | PR | 97 (194) | Canada | Québécois mixed-sex couples undergoing fertility treatment | 31.8 | S | FSFI, IIEF | attachment | ECR-12 | 4 | |
| Meston et al. (2024) | PR | 268 | US | Sexually active men in committed heterosexual relationships | 37.3 | 71 | SODE | SSS, IIEF | relationship sat | CSI | 4 |
| Beaulieu et al. (2023) | PR | 145 (290) | Canada | Québécois mixed-sex couples | 31.3 | 94 | S | GMSEX | relationship sat | DAS-4 | 2 |
| Kfoury et al. (2023) | PR | 317 | Lebanon | Sexually active women with (n = 65) and without (n = 252) endometriosis | 29.5 | S | SSS-W | depressive sx & relationship sat | DASS, CSI | 2 | |
| Józefacka et al. (2023) | PR | 237 | Poland | Undergraduate students in heterosexual relationships ≥ 1 mo. | 20.1 | S | SSQ | relationship sat | CSI-32 | 2 | |
| Dion et al. (2023) | PR | 2754 | Canada | Québécois university employees (43%) and students (57%) | 37.2 | S | 1 item | depressive sx & relationship sat | PHQ-4, DAS-4 | 2 | |
| Busby et al. (2023) | PR | 1605 | US | Adults from Mturk in romantic relationships ≥ 2 yr. | 34.9 | 75 | S | GMSEX | relationship sat & attachment | CSI-4, ECR | 3 |
| Ramos Costa et al. (2023) | PR | 79 | Brazilian Amazon | Young adults (aged 18 to 35) from Quilombola communities (descended from African slaves) | 23.6 | 1.3 | SODPLE | FSFI, IIEF | physical health & life satisfaction | WHOQoL | 34 |
| Feder (2023) | DD | 46,874 | ISS: 43 countries | Women respondents in the International Sex Survey (ISS) | 32.4 | SD | GMSEX, SDI-2 | only sex health * | 1 | ||
| Karakose et al. (2023) | PR | 102 (204) | Turkey | Heterosexual married couples | 30.1 | S | NSSS | depressive sx | DASS-21 | 2 | |
| Ogallar-Blanco et al. (2022) | PR | 1080 | Spain | Women (aged 18 to 55) born in Spain or living in Spain ≥ 1 yr. | 24.5 | SO | NSSS, 1 item | only sex health * | 1 | ||
| McKay et al. (2022) | PR | 61 (122) | Australia | Women (aged 18 to 47) with endometriosis and their partners | 30.7 | S | NSSS | relationship sat | CSI-16 | 2 | |
| J. M. Strizzi et al. (2022) | PR | 4148 | Norway | National population study of adults | 46.5 | S | 1 item | relationship sat | 1 item | 1 | |
| Uhlich et al. (2022) | PR | 179 (358) | Iran | Heterosexual cohabiting married couples | 37.0 | S | 1 item | relationship sat | 1 CSI item | 2 | |
| Lopes (2022) | MT | 282 | Portugal | Sexually active (in previous month) heterosexual adults | 28.9 | SODPLE | FSFI, IIEF | depressive sx | EADS-21 | 9 | |
| Wójcik & Rogowska (2022) | PR | 440 | Poland | Sexually active, childless adults aged 18 to 40 | 24.3 | S | SSQ | life satisfaction | SWLS | 1 | |
| Péloquin et al. (2022) | PR | 274 (548) | Canada | Mixed-sex Québécois couples seeking relationship therapy | 42.0 | S | GMSEX | attachment | ECR | 4 | |
| Lafortune et al. (2022) | PR | 543 | Canada | French-Canadian community adults | 36.2 | S | GMSEX | attachment | ECR | 2 | |
| Attaky et al. (2022) | PR | 100 (200) | Saudi Arabia | Heterosexual Arabic married couples (half seeking treatment for sexual or marital problems) | 33.4 | S | ISS | relationship sat & attachment | DAS-4, ECR-R | 6 | |
| Kamrava et al. (2021) | PR | 170 | Iran | Married and sexually active patients with PTOD (n = 55) and healthy controls (n = 115) | 38.4 | S | SSSW | depressive sx & relationship sat | BDI, ENRICH | 2 | |
| A. A. Conroy et al. (2021) | PR | 211 (422) | Malawi | Heterosexual couples with at least one partner living with HIV | 40.5 | 0 | S | CSSS | relationship sat | 1 CSI item | 1 |
| Peters and Meltzer (2021) | PR | 102 (204) | US | Newlywed couples living in Northern Florida | 30.9 | 76 | S | ISS | relationship sat | QMI, SMD, KMSS | 1 |
| Gesselman et al. (2021) | PR | 88 | US | People with epilepsy currently in relationships and on medication to control seizures | 32.1 | 83 | S | GMSEX | relationship sat, well-being | GMREL, AESMI | 2 |
| Cruz and Caringal-Go (2021) | PR | 442 | Philippines | Heterosexual Christian adults in relationships | 38.0 | SD | GMSEX, 1 item | relationship sat | GMREL | 3 | |
| Park et al. (2021) | PR | 3890 | US & Germany | Never married and divorced individuals who were currently single | 39.9 | 77 | S | 1 item | life satisfaction | 1 item | 3 |
| Charbonneau-Lefebvre et al. (2021) | PR | 125 (250) | Canada | Sexually active couples seeking treatment for Provoked VestibuloDynia (PVD) | 28.1 | 73 | S | GMSEX | relationship sat & attachment | CSI-32 & ECR-R | 6 |
| Smedley et al. (2021) | PR | 1627 (3254) | US | Mixed-sex couples from the CREATE study | 30.9 | 53 | S | RELATE | relationship sat & attachment | CSI-4 & ECR-R | 6 |
| do Rosário Ramos Nunes Bacalhau et al. (2020) | PR | 113 | Portugal | Women having completed treatment for cervical cancer | 48.0 | S | ISS | relationship sat & attachment | DAS-14 & ECR | 3 | |
| Fleishman et al. (2020) | PR | 265 | US & Canada | 60–75 yo. adults in same-sex relationships | 65.3 | 82 | S | ISS | relationship sat | CSI-32 | 1 |
| N. O. Rosen et al. (2020) | PR | 171 | Canada | Women in relationships who were 18–25 weeks pregnant with their first child | 29.8 | 85 | S | GMSEX | relationship sat | CSI-4 | 1 |
| Calvillo et al. (2020) | PR | 820 | Spain & Latin Am countries | Spanish-speaking adults in same-sex relationships ≥ 3 mo. | 29.1 | S | MGH-SFQ | relationship sat & attachment | GMREL & ECR-S | 6 | |
| Merwin and Rosen (2020) | PR | 303 | US & Canada | Sexually active adults in cohabiting romantic relationships | 35.9 | S | GMSEX | relationship sat | PRQC | 1 | |
| Category of Results | SM Rel-Prob | Funnel Plot Asym Z | Trim and Fill Adj. Est. | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Correlate Variable | |||||||||||
| Sexual Health Variables | k | N | r | SE | 95% CI | Q | I2 | r | k | ||
| Sexual health links to correlates | |||||||||||
| Psychological distress | |||||||||||
| Sexual satisfaction | 69 | 17,234 | −.276 **** | .022 | [−.318, −.233] | 4449.05 **** | 91.27 | .99 | 1.84 | ||
| Orgasms | 97 | 58,706 | −.250 **** | .022 | [−.294, −.207] | 13,035.00 **** | 97.46 | 3.04 | 1.33 | ||
| Desire | 64 | 13,722 | −.167 **** | .031 | [−.228, −.105] | 4077.37 **** | 94.54 | 3.20 | −.12 | ||
| Lack of pain | 42 | 8575 | −.183 **** | .047 | [−.275, −.090] | 3230.86 **** | 96.71 | 6.17 | .22 | ||
| Lubrication | 46 | 9090 | −.239 *** | .033 | [−.304, −.174] | 1678.95 **** | 92.78 | 4.19 | 1.35 | ||
| Erectile function | 11 | 2127 | −.148 *** | .046 | [−.238, −.059] | 24.95 ** | 68.74 | .92 | −1.95 | ||
| Psychological well-being | |||||||||||
| Sexual satisfaction | 22 | 6719 | .343 **** | .042 | [.260, .425] | 1041.04 **** | 93.52 | .22 | −1.697 | ||
| Orgasms | 23 | 9420 | .239 **** | .041 | [.159, .320] | 601.83 **** | 94.04 | .32 | −1.52 | ||
| Desire | 15 | 3502 | .320 **** | .070 | [.184, .457] | 354.57 **** | 97.11 | 2.85 | −2.83 ** | .335 **** | 16 |
| Lack of pain | 12 | 3399 | .268 **** | .067 | [.137, .399] | 215.11 **** | 94.30 | 10.88 | −3.26 *** | .336 **** | 15 |
| Lubrication | 12 | 3399 | .196 ** | .063 | [.072, .319] | 258.63 | 90.94 | 2.23 | −.72 | ||
| Erectile function | 0 | 0 | |||||||||
| Physical health | |||||||||||
| Sexual satisfaction | 12 | 1997 | .311 **** | .077 | [.159, .462] | 464.55 **** | 92.30 | 1.52 | −2.90 ** | .387 *** | 15 |
| Orgasms | 14 | 4160 | .278 **** | .066 | [.149, .406] | 705.08 **** | 95.00 | .09 | −1.52 | ||
| Desire | 13 | 2073 | .270 **** | .068 | [.137, .404] | 365.65 **** | 89.62 | 1.50 | −2.35 * | .323 **** | 15 |
| Lack of pain | 9 | 1588 | .249 **** | .073 | [.106, .392] | 87.50 **** | 82.16 | 11.09 | −2.44 * | .304 **** | 11 |
| Lubrication | 9 | 1588 | .221 * | .093 | [.039, .402] | 146.89 **** | 89.77 | 1.63 | −2.02 * | .221 * | 9 |
| Erectile function | 1 | 39 | |||||||||
| Attachment anxiety | |||||||||||
| Sexual satisfaction | 22 | 10,156 | −.237 **** | .048 | [−.331, −.142] | 4575.31 **** | 97.86 | .96 | 2.38 * | −.336 **** | 30 |
| Orgasms | 9 | 3979 | −.149 **** | .022 | [−.193, −.105] | 13.26 | 40.04 | .91 | −2.58 ** | −.127 **** | 12 |
| Desire | 5 | 1479 | −.043 | .046 | [−.133, .048] | 9.43 | 59.61 | .86 | −1.9 | ||
| Attachment anxiety | |||||||||||
| Lack of pain | 2 | 975 | −.145 **** | .031 | [−.207, −.083] | .89 | .00 | .75 | |||
| Lubrication | 2 | 975 | −.128 **** | .032 | [−.190, −.067] | .22 | .00 | .75 | |||
| Erectile function | 1 | 248 | |||||||||
| Attachment avoidance | |||||||||||
| Sexual satisfaction | 22 | 10,156 | −.339 **** | .034 | [−.405, −.272] | 237.89 **** | 93.38 | .89 | 3.51 *** | −.339 **** | 22 |
| Orgasms | 9 | 3979 | −.241 **** | .029 | [−.270, −.158] | 24.02 ** | 63.99 | .91 | −.19 | ||
| Desire | 5 | 1479 | −.124 ** | .046 | [−.213, −.034] | 9.71 * | 64.27 | .86 | 2.03 * | −.124 * | 5 |
| Lack of pain | 2 | 975 | −.165 **** | .040 | [−.243, −.088] | 1.58 | 36.82 | .75 | |||
| Lubrication | 2 | 975 | −.279 **** | .070 | [−.416, −.412] | 5.56 * | 82.02 | .75 | |||
| Erectile function | 1 | 248 | |||||||||
| Relationship satisfaction | |||||||||||
| Sexual satisfaction | 62 | 69,328 | .554 **** | .020 | [.516, .592] | 4372.45 **** | 97.83 | .02 | −4.91 **** | .589 **** | 27 |
| Orgasms | 60 | 47,311 | .267 **** | .026 | [.216, .317] | 7075.88 **** | 97.55 | .23 | −1.37 | ||
| Desire | 21 | 10,312 | .248 **** | .043 | [.164, .331] | 1158.65 **** | 95.78 | 1.16 | −1.49 | ||
| Lack of pain | 11 | 3976 | .183 *** | .053 | [.079, .287] | 51.96 **** | 88.48 | 1.18 | .38 | ||
| Lubrication | 14 | 6973 | .187 *** | .038 | [.114, .261] | 90.39 **** | 88.23 | .99 | .14 | ||
| Erectile function | 1 | 248 | |||||||||
| Links among sexual health dimensions | |||||||||||
| Sexual satisfaction correlating with | |||||||||||
| Orgasms | 138 | 113,079 | .398 *** | .019 | [.361, .435] | 24,581.54 **** | 98.59 | .17 | −1.99 * | .444 **** | 156 |
| Desire | 56 | 70,791 | .382 *** | .029 | [.325, .440] | 15,921.34 **** | 98.84 | .22 | −2.30 * | .467 **** | 70 |
| Lack of pain | 26 | 11,834 | .375 **** | .053 | [.271, .480] | 3540.22 **** | 98.85 | .31 | −2.67 ** | .426 **** | 29 |
| Lubrication | 29 | 12,318 | .462 **** | .043 | [.379, .546] | 1995.12 **** | 97.38 | .05 | −3.41 *** | .542 **** | 36 |
| Erectile function | 13 | 6315 | .400 **** | .045 | [.313, .488] | 193.87 **** | 92.94 | .43 | 1.36 | ||
| Orgasms correlating with | |||||||||||
| Desire | 56 | 21,958 | .339 **** | .027 | [.287, .392] | 3555.92 **** | 96.32 | .25 | −3.19 ** | .416 **** | 71 |
| Lack of pain | 27 | 11,128 | .357 *** | .055 | [.249, .465] | 3675.84 **** | 98.65 | .21 | −1.26 | ||
| Lubrication | 24 | 11,504 | .531 **** | .046 | [.441, .621] | 2268.09 **** | 99.12 | .08 | −4.57 **** | .531 **** | 28 |
| Erectile function | 13 | 6541 | .527 **** | .032 | [.465, .589] | 139.90 **** | 90.87 | .07 | −.75 | ||
| Desire correlating with | |||||||||||
| Lack of pain | 28 | 11,240 | .265 **** | .039 | [.189, .342] | 3568.58 **** | 96.58 | .45 | −2.46 * | .348 **** | 36 |
| Lubrication | 28 | 11,804 | .393 **** | .034 | [.326, .460] | 1929.99 **** | 96.04 | .03 | −3.60 *** | .464 **** | 37 |
| Erectile function | 11 | 6183 | .343 **** | .058 | [.230, .456] | 298.79 **** | 96.06 | 1.04 | −1.33 | ||
| Lack of pain correlating with | |||||||||||
| Lubrication | 25 | 10,422 | .555 **** | .037 | [.482, .628] | 1447.75 **** | 97.89 | .04 | −3.17 ** | .588 **** | 28 |
| MODEL | 99% CIs | MODEL | 99% CIs | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Correlate Being Predicted | Correlate Being Predicted | ||||||||
| Predictors | β | p | LL | UL | Predictors | β | p | LL | UL |
| PSYCH DISTRESS MODEL | WELL-BEING MODEL | ||||||||
| SexH → psychological distress | SexH → well-being | ||||||||
| Sexual satisfaction | −.175 | <.001 | −.209 | −.142 | Sexual satisfaction | .225 | <.001 | .165 | .285 |
| Orgasms | −.127 | <.001 | −.161 | −.093 | Orgasms | .087 | <.001 | .026 | .148 |
| Desire | −.024 | .054 | −.055 | .008 | Desire | .211 | <.001 | .154 | .268 |
| Lack of pain | −.030 | .025 | −.064 | .004 | Lack of pain | .169 | <.001 | .108 | .231 |
| Lubrication | −.065 | <.001 | −.103 | −.026 | Lubrication | −.131 | <.001 | −.201 | −.061 |
| SexH → sex satisfaction | SexH → sex satisfaction | ||||||||
| Orgasms | .163 | <.001 | .134 | .193 | Orgasms | .163 | <.001 | .107 | .219 |
| Desire | .204 | <.001 | .177 | .231 | Desire | .204 | <.001 | .152 | .256 |
| Lack of pain | .143 | <.001 | .113 | .173 | Lack of pain | .143 | <.001 | .086 | .199 |
| Lubrication | .216 | <.001 | .182 | .250 | Lubrication | .216 | <.001 | .152 | .280 |
| Indirect paths | Indirect paths | ||||||||
| Orgasm → SexSat → Distress | −.029 | −.036 | −.021 | Orgasm → SexSat → Well-being | .037 | .021 | .053 | ||
| Desire → SexSat → Distress | −.036 | −.044 | −.027 | Desire → SexSat → Well-being | .046 | .029 | .063 | ||
| L-pain → SexSat → Distress | −.025 | −.032 | −.018 | L-pain → SexSat → Well-being | .032 | .017 | .047 | ||
| Lube → SexSat → Distress | −.038 | −.047 | −.029 | Lube → SexSat → Well-being | .049 | .029 | .068 | ||
| PHYSICAL HEALTH MODEL | REL SATISFACTION MODEL | ||||||||
| SexH → perceived health | SexH → rel satisfaction | ||||||||
| Sexual satisfaction | .181 | <.001 | .107 | .255 | Sexual satisfaction | .559 | <.001 | .518 | .599 |
| Orgasms | .148 | <.001 | .073 | .223 | Orgasms | .104 | <.001 | .063 | .145 |
| Desire | .144 | <.001 | .074 | .214 | Desire | .058 | <.001 | .019 | .096 |
| Lack of pain | .129 | <.001 | .053 | .204 | Lack of pain | .005 | .734 | −.036 | .047 |
| Lubrication | −.069 | .039 | −.155 | .017 | Lubrication | −.152 | <.001 | −.199 | −.105 |
| SexH → sex satisfaction | SexH → sex satisfaction | ||||||||
| Orgasms | .163 | <.001 | .095 | .231 | Orgasms | .163 | <.001 | .122 | .205 |
| Desire | .204 | <.001 | .142 | .266 | Desire | .204 | <.001 | .166 | .242 |
| Lack of pain | .143 | <.001 | .075 | .211 | Lack of pain | .143 | <.001 | .101 | .185 |
| Lubrication | .216 | <.001 | .139 | .293 | Lubrication | .216 | <.001 | .169 | .263 |
| Indirect paths | Indirect paths | ||||||||
| Orgasm → SexSat → Health | .030 | .012 | .047 | Orgasm → SexSat → RelSat | .091 | .067 | .115 | ||
| Desire → SexSat → Health | .037 | .018 | .056 | Desire → SexSat → RelSat | .114 | .091 | .137 | ||
| L-pain → SexSat → Health | .026 | .010 | .042 | L-pain → SexSat → RelSat | .080 | .056 | .104 | ||
| Lube → SexSat → Health | .039 | .018 | .060 | Lube → SexSat → RelSat | .121 | .093 | .148 | ||
| ATTCH AVOIDANCE MODEL | ATTCH ANXIETY MODEL | ||||||||
| Avoid & SexH → Sex sat | Attch anxiety → SexH | ||||||||
| Attch avoidance | −.209 | <.001 | −.280 | −.139 | Sexual satisfaction | −.161 | <.001 | −.230 | −.092 |
| Orgasms | .136 | <.001 | .055 | .217 | Orgasms | .146 | <.001 | .064 | .228 |
| Desire | .205 | <.001 | .130 | .279 | Desire | .209 | <.001 | .134 | .284 |
| Lack of pain | .142 | <.001 | .061 | .223 | Lack of pain | .127 | <.001 | .045 | .209 |
| Lubrication | .172 | <.001 | .079 | .265 | Lubrication | .212 | <.001 | .119 | .304 |
| Attch avoidance → SexH | SexH → sex satisfaction | ||||||||
| Orgasms | −.241 | <.001 | −.321 | −.161 | Orgasms | −.149 | <.001 | −.231 | −.067 |
| Desire | −.124 | <.001 | −.206 | −.042 | Desire | −.043 | .179 | −.125 | .039 |
| Lack of pain | −.165 | <.001 | −.246 | −.084 | Lack of pain | −.145 | <.001 | −.227 | −.063 |
| Lubrication | −.279 | <.001 | −.358 | −.200 | Lubrication | −.128 | <.001 | −.210 | −.046 |
| Indirect paths | Indirect paths | ||||||||
| Avoid → Orgasm → SexSat | −.033 | −.055 | −.010 | Anxiety → Orgasm → SexSat | −.022 | −.039 | −.005 | ||
| Avoid → Desire → SexSat | −.025 | −.044 | −.006 | Anxiety → Desire → SexSat | −.009 | −.027 | .009 | ||
| Avoid → L-pain → SexSat | −.023 | −.041 | −.006 | Anxiety → L-pain → SexSat | −.018 | −.034 | −.003 | ||
| Avoid → Lube → SexSat | −.048 | −.077 | −.019 | Anxiety → Lube → SexSat | −.027 | −.048 | −.006 | ||
| Sexual Health Indicator | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Correlate Being Predicted | Sexual Satisfaction | Orgasms | Desire | Lack of Pain | Lubrication | |||||
| Moderators Tested | Estimate | p | Estimate | p | Estimate | p | Estimate | p | Estimate | p |
| Predicting sexual satisfaction | ||||||||||
| intercept | --- | --- | .391 | <.0001 | .382 | <.0001 | .438 | <.0001 | .536 | <.0001 |
| Male contrast | --- | --- | −.162 | <.0001 | −.048 | .479 | ||||
| Age (centered at 38.9 years) | --- | --- | .001 | .464 | .006 | .032 | .012 | .019 | .006 | .171 |
| Clinical population contrast | --- | --- | .130 | .001 | .051 | .406 | −.028 | .801 | .003 | .972 |
| Peer-reviewed contrast | --- | --- | −.037 | .527 | .134 | .214 | −.184 | .360 | −.388 | .087 |
| Predicting psychological distress | ||||||||||
| intercept | −.311 | <.0001 | −.237 | <.0001 | −.133 | .026 | −.264 | .004 | −.280 | <.0001 |
| Male contrast | .013 | .816 | .059 | .290 | .040 | .641 | --- | --- | --- | --- |
| Age (centered at 38.9 years) | −.001 | .560 | −.006 | .002 | −.002 | .481 | .001 | .897 | −.004 | .116 |
| Clinical population contrast | .068 | .207 | .014 | .773 | −.066 | .404 | .182 | .127 | .169 | .020 |
| Peer-reviewed contrast | −.009 | .925 | −.083 | .322 | .084 | .584 | −.165 | .597 | −.259 | .228 |
| Predicting psychological well-being | ||||||||||
| intercept | .349 | <.0001 | .191 | .001 | .374 | <.0001 | .336 | .001 | .080 | .408 |
| Male contrast | −.199 | .118 | −.164 | .223 | −.177 | .411 | --- | --- | --- | --- |
| Age (centered at 38.9 years) | .006 | .096 | .003 | .544 | .008 | .334 | .005 | .535 | .009 | .240 |
| Clinical population contrast | −.040 | .618 | .043 | .618 | −.173 | .219 | −.153 | .265 | .181 | .171 |
| Predicting relationship satisfaction | ||||||||||
| intercept | .581 | <.0001 | .253 | <.0001 | .219 | .004 | .124 | .046 | .122 | .006 |
| Male contrast | .047 | .325 | −.062 | .331 | −.042 | .835 | --- | --- | --- | --- |
| Age (centered at 38.9 yrs) | −.001 | .640 | .001 | .668 | .003 | .450 | .008 | .025 | .001 | .846 |
| Clinical population contrast | −.031 | .463 | .049 | .384 | .028 | .778 | .075 | .421 | .143 | .040 |
| Peer-reviewed contrast | −.152 | .089 | .015 | .872 | .066 | .815 | --- | --- | --- | --- |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pollard, A.E.; Cero, I.; Rogge, R.D. Conceptual Frameworks Linking Sexual Health to Physical, Mental, and Interpersonal Well-Being: A Comprehensive Systematic Review and Meta-Analysis. Behav. Sci. 2025, 15, 1636. https://doi.org/10.3390/bs15121636
Pollard AE, Cero I, Rogge RD. Conceptual Frameworks Linking Sexual Health to Physical, Mental, and Interpersonal Well-Being: A Comprehensive Systematic Review and Meta-Analysis. Behavioral Sciences. 2025; 15(12):1636. https://doi.org/10.3390/bs15121636
Chicago/Turabian StylePollard, Agnieszka E., Ian Cero, and Ronald D. Rogge. 2025. "Conceptual Frameworks Linking Sexual Health to Physical, Mental, and Interpersonal Well-Being: A Comprehensive Systematic Review and Meta-Analysis" Behavioral Sciences 15, no. 12: 1636. https://doi.org/10.3390/bs15121636
APA StylePollard, A. E., Cero, I., & Rogge, R. D. (2025). Conceptual Frameworks Linking Sexual Health to Physical, Mental, and Interpersonal Well-Being: A Comprehensive Systematic Review and Meta-Analysis. Behavioral Sciences, 15(12), 1636. https://doi.org/10.3390/bs15121636







