The Effect of Pet Therapy and Artist Interactions on Quality of Life in Brain Tumor Patients: A Cross-Section of Art and Medicine in Dialog
Abstract
:1. Introduction
2. Methods
3. Results
3.1. Impact of Pet Therapy on Patients
3.2. Impact of the Portrait Session on Patients
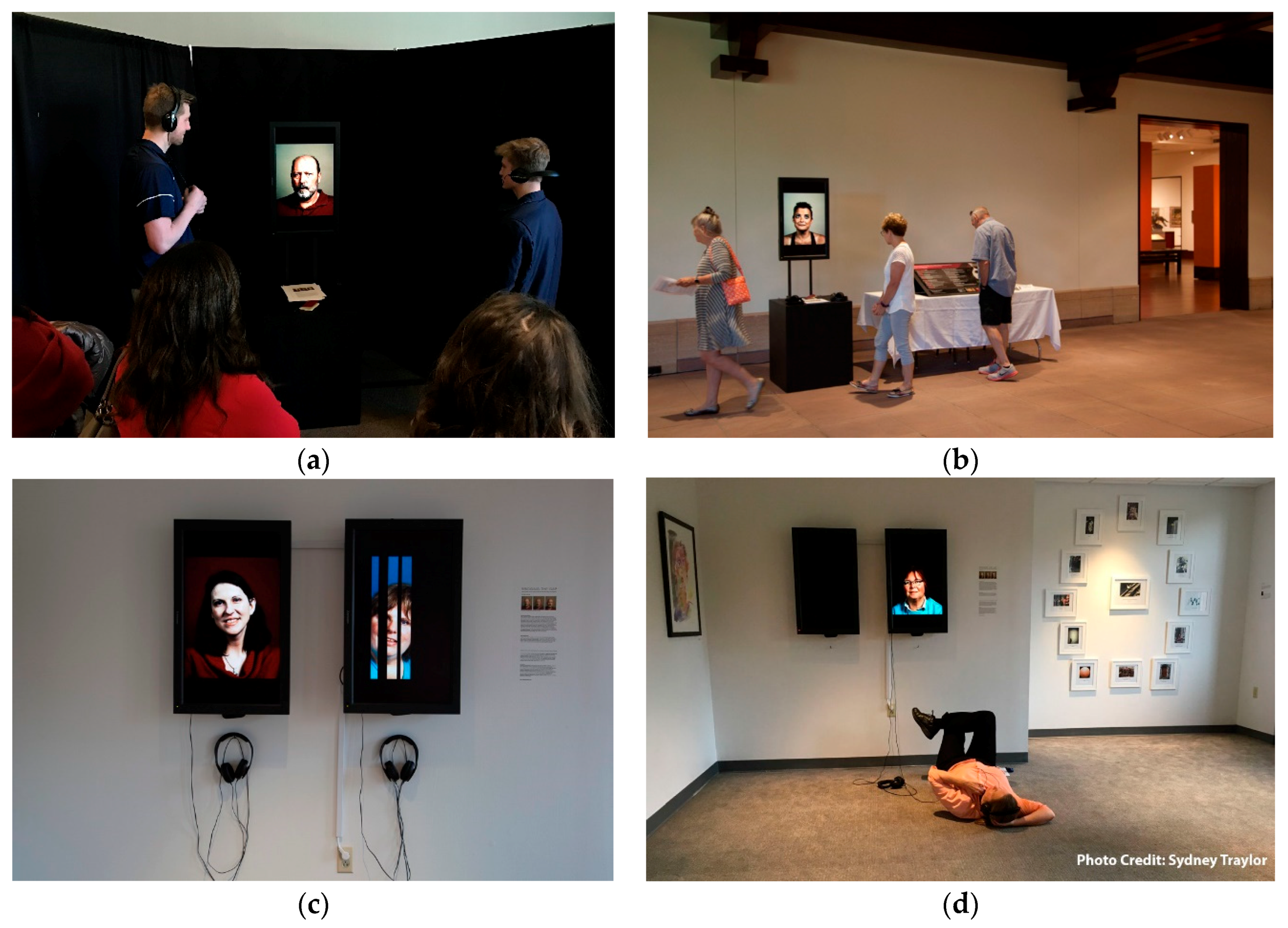
3.3. Impact of the Study on the Community
4. Discussion
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Stupp, R.; Mason, W.P.; van den Bent, M.J.; Weller, M.; Fisher, B.; Taphoorn, M.J.; Belanger, K.; Brandes, A.A.; Marosi, C.; Bogdahn, U.; et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N. Engl. J. Med. 2005, 352, 987–996. [Google Scholar] [CrossRef] [PubMed]
- Stupp, R.; Taillibert, S.; Kanner, A.; Read, W.; Steinberg, D.M.; Lhermitte, B.; Toms, S.; Idbaih, A.; Ahluwalia, M.S.; Fink, K.; et al. Effect of Tumor-Treating Fields Plus Maintenance Temozolomide vs. Maintenance Temozolomide Alone on Survival in Patients With Glioblastoma: A Randomized Clinical Trial. JAMA 2017, 318, 2306–2316. [Google Scholar] [CrossRef] [PubMed]
- Ostrom, Q.T.; Gittleman, H.; Xu, J.; Kromer, C.; Wolinsky, Y.; Kruchko, C.; Barnholtz-Sloan, J.S. CBTRUS Statistical Report: Primary Brain and Other Central Nervous System Tumors Diagnosed in the United States in 2009–2013. Neuro-Oncology 2016, 18, v1–v75. [Google Scholar] [CrossRef] [PubMed]
- Morrison, R.S.; Meier, D.E. Clinical practice. Palliative care. N. Engl. J. Med. 2004, 350, 2582–2590. [Google Scholar] [CrossRef] [PubMed]
- Temel, J.S.; Greer, J.A.; Muzikansky, A.; Gallagher, E.R.; Admane, S.; Jackson, V.A.; Dahlin, C.M.; Blinderman, C.D.; Jacobsen, J.; Pirl, W.F.; et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N. Engl. J. Med. 2010, 363, 733–742. [Google Scholar] [CrossRef] [PubMed]
- Bakitas, M.; Lyons, K.D.; Hegel, M.T.; Balan, S.; Brokaw, F.C.; Seville, J.; Hull, J.G.; Li, Z.; Tosteson, T.D.; Byock, I.R.; et al. Effects of a palliative care intervention on clinical outcomes in patients with advanced cancer: The Project ENABLE II randomized controlled trial. JAMA 2009, 302, 741–749. [Google Scholar] [CrossRef] [PubMed]
- Clayton, P.J. Bipolar affective disorder—Techniques and results of treatment. Am. J. Psychother. 1978, 32, 81–92. [Google Scholar] [PubMed]
- Bottomley, A.; Pe, M.; Sloan, J.; Basch, E.; Bonnetain, F.; Calvert, M.; Campbell, A.; Cleeland, C.; Cocks, K.; Collette, L.; et al. Analysing data from patient-reported outcome and quality of life endpoints for cancer clinical trials: A start in setting international standards. Lancet Oncol. 2016, 17, e510–e514. [Google Scholar] [CrossRef]
- Stuckey, H.L.; Nobel, J. The connection between art, healing, and public health: A review of current literature. Am. J. Public Health 2010, 100, 254–263. [Google Scholar] [CrossRef] [PubMed]
- Hamoen, E.H.; De Rooij, M.; Witjes, J.A.; Barentsz, J.O.; Rovers, M.M. Measuring health-related quality of life in men with prostate cancer: A systematic review of the most used questionnaires and their validity. Urol. Oncol. 2015, 33, 69.e19–69.e28. [Google Scholar] [CrossRef] [PubMed]
- Vissers, P.A.; Thong, M.S.; Pouwer, F.; Zanders, M.M.; Coebergh, J.W.; van de Poll-Franse, L.V. The impact of comorbidity on Health-Related Quality of Life among cancer survivors: Analyses of data from the PROFILES registry. J. Cancer Surviv. 2013, 7, 602–613. [Google Scholar] [CrossRef] [PubMed]
- Sanders, C.; Egger, M.; Donovan, J.; Tallon, D.; Frankel, S. Reporting on quality of life in randomised controlled trials: Bibliographic study. BMJ 1998, 317, 1191–1194. [Google Scholar] [CrossRef] [PubMed]
- Bottomley, A. The cancer patient and quality of life. Oncologist 2002, 7, 120–125. [Google Scholar] [CrossRef] [PubMed]
- Karimi, M.; Brazier, J. Health, Health-Related Quality of Life, and Quality of Life: What is the Difference? Pharmacoeconomics 2016, 34, 645–649. [Google Scholar] [CrossRef] [PubMed]
- Romero, M.; Vivas-Consuelo, D.; Alvis-Guzman, N. Is Health Related Quality of Life (HRQoL) a valid indicator for health systems evaluation? SpringerPlus 2013, 2, 664. [Google Scholar] [CrossRef] [PubMed]
- Post, M.W. Definitions of quality of life: What has happened and how to move on. Top. Spinal Cord Inj. Rehabil. 2014, 20, 167–180. [Google Scholar] [CrossRef] [PubMed]
- Musoro, Z.J.; Hamel, J.F.; Ediebah, D.E.; Cocks, K.; King, M.T.; Groenvold, M.; Sprangers, M.A.G.; Brandberg, Y.; Velikova, G.; Maringwa, J.; et al. Establishing anchor-based minimally important differences (MID) with the EORTC quality-of-life measures: A meta-analysis protocol. BMJ Open 2018, 8, e019117. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.H.; Li, L.; Kochen, M.M. A systematic review: How to choose appropriate health-related quality of life (HRQOL) measures in routine general practice? J. Zhejiang Univ. Sci. B 2005, 6, 936–940. [Google Scholar] [CrossRef] [PubMed]
- Higginson, I.J.; Carr, A.J. Measuring quality of life: Using quality of life measures in the clinical setting. BMJ 2001, 322, 1297–1300. [Google Scholar] [CrossRef] [PubMed]
- Ramnarayan, P.; Kapoor, R.R.; Coren, M.; Nanduri, V.; Tomlinson, A.L.; Taylor, P.M.; Wyatt, J.C.; Britto, J.F. Measuring the impact of diagnostic decision support on the quality of clinical decision making: Development of a reliable and valid composite score. J. Am. Med. Inform. Assoc. 2003, 10, 563–572. [Google Scholar] [CrossRef] [PubMed]
- Deshpande, P.R.; Rajan, S.; Sudeepthi, B.L.; Abdul Nazir, C.P. Patient-reported outcomes: A new era in clinical research. Perspect. Clin. Res. 2011, 2, 137–144. [Google Scholar] [CrossRef] [PubMed]
- Fries, J.F.; Bruce, B.; Cella, D. The promise of PROMIS: Using item response theory to improve assessment of patient-reported outcomes. Clin. Exp. Rheumatol. 2005, 23, S53–S57. [Google Scholar] [PubMed]
- Black, N. Patient reported outcome measures could help transform healthcare. BMJ 2013, 346, f167. [Google Scholar] [CrossRef] [PubMed]
- Forsberg, H.H.; Nelson, E.C.; Reid, R.; Grossman, D.; Mastanduno, M.P.; Weiss, L.T.; Fisher, E.S.; Weinstein, J.N. Using patient-reported outcomes in routine practice: Three novel use cases and implications. J. Ambul. Care Manag. 2015, 38, 188–195. [Google Scholar] [CrossRef] [PubMed]
- Lavallee, D.C.; Chenok, K.E.; Love, R.M.; Petersen, C.; Holve, E.; Segal, C.D.; Franklin, P.D. Incorporating Patient-Reported Outcomes into Health Care to Engage Patients and Enhance Care. Health Aff. 2016, 35, 575–582. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, T.S. Measuring clinical benefit: Use of patient-reported outcomes (PRO) in primary brain tumor clinical trials. Curr. Oncol. Rep. 2013, 15, 27–32. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, T.S.; Gilbert, M.R. Patient reported endpoints for measuring clinical benefit in (high grade glioma) primary brain tumor patients. Curr. Treat. Options Oncol. 2014, 15, 519–528. [Google Scholar] [CrossRef] [PubMed]
- Klein, M.; Taphoorn, M.J.; Heimans, J.J.; van der Ploeg, H.M.; Vandertop, W.P.; Smit, E.F.; Leenstra, S.; Tulleken, C.A.; Boogerd, W.; Belderbos, J.S.; et al. Neurobehavioral status and health-related quality of life in newly diagnosed high-grade glioma patients. J. Clin. Oncol. 2001, 19, 4037–4047. [Google Scholar] [CrossRef] [PubMed]
- Brown, P.D.; Ballman, K.V.; Rummans, T.A.; Maurer, M.J.; Sloan, J.A.; Boeve, B.F.; Gupta, L.; Tang-Wai, D.F.; Arusell, R.M.; Clark, M.M.; et al. Prospective study of quality of life in adults with newly diagnosed high-grade gliomas. J. Neuro-Oncol. 2006, 76, 283–291. [Google Scholar] [CrossRef] [PubMed]
- Dirven, L.; Reijneveld, J.C.; Aaronson, N.K.; Bottomley, A.; Uitdehaag, B.M.; Taphoorn, M.J. Health-related quality of life in patients with brain tumors: Limitations and additional outcome measures. Curr. Neurol. Neurosci. Rep. 2013, 13, 359. [Google Scholar] [CrossRef] [PubMed]
- Liu, R.; Page, M.; Solheim, K.; Fox, S.; Chang, S.M. Quality of life in adults with brain tumors: Current knowledge and future directions. Neuro-Oncology 2009, 11, 330–339. [Google Scholar] [CrossRef] [PubMed]
- Osoba, D.; Brada, M.; Prados, M.D.; Yung, W.K. Effect of disease burden on health-related quality of life in patients with malignant gliomas. Neuro-Oncology 2000, 2, 221–228. [Google Scholar] [CrossRef] [PubMed]
- Brown, P.D.; Decker, P.A.; Rummans, T.A.; Clark, M.M.; Frost, M.H.; Ballman, K.V.; Arusell, R.M.; Buckner, J.C. A prospective study of quality of life in adults with newly diagnosed high-grade gliomas: Comparison of patient and caregiver ratings of quality of life. Am. J. Clin. Oncol. 2008, 31, 163–168. [Google Scholar] [CrossRef] [PubMed]
- Wellisch, D.K.; Kaleita, T.A.; Freeman, D.; Cloughesy, T.; Goldman, J. Predicting major depression in brain tumor patients. Psycho-Oncology 2002, 11, 230–238. [Google Scholar] [CrossRef] [PubMed]
- Mainio, A.; Hakko, H.; Niemela, A.; Koivukangas, J.; Rasanen, P. Depression and functional outcome in patients with brain tumors: A population-based 1-year follow-up study. J. Neurosurg. 2005, 103, 841–847. [Google Scholar] [CrossRef] [PubMed]
- Arnold, S.D.; Forman, L.M.; Brigidi, B.D.; Carter, K.E.; Schweitzer, H.A.; Quinn, H.E.; Guill, A.B.; Herndon, J.E., 2nd; Raynor, R.H. Evaluation and characterization of generalized anxiety and depression in patients with primary brain tumors. Neuro-Oncology 2008, 10, 171–181. [Google Scholar] [CrossRef] [PubMed]
- Mainio, A.; Tuunanen, S.; Hakko, H.; Niemela, A.; Koivukangas, J.; Rasanen, P. Decreased quality of life and depression as predictors for shorter survival among patients with low-grade gliomas: A follow-up from 1990 to 2003. Eur. Arch. Psychiatry Clin. Neurosci. 2006, 256, 516–521. [Google Scholar] [CrossRef] [PubMed]
- Mainio, A.; Hakko, H.; Timonen, M.; Niemela, A.; Koivukangas, J.; Rasanen, P. Depression in relation to survival among neurosurgical patients with a primary brain tumor: A 5-year follow-up study. Neurosurgery 2005, 56, 1234–1241; discussion 1241–1232. [Google Scholar] [CrossRef] [PubMed]
- Pelletier, G.; Verhoef, M.J.; Khatri, N.; Hagen, N. Quality of life in brain tumor patients: The relative contributions of depression, fatigue, emotional distress, and existential issues. J. Neuro-Oncology 2002, 57, 41–49. [Google Scholar] [CrossRef]
- Marcus, D.A. The science behind animal-assisted therapy. Curr. Pain Headache Rep. 2013, 17, 322. [Google Scholar] [CrossRef] [PubMed]
- Marcus, D.A.; Bernstein, C.D.; Constantin, J.M.; Kunkel, F.A.; Breuer, P.; Hanlon, R.B. Impact of animal-assisted therapy for outpatients with fibromyalgia. Pain Med. 2013, 14, 43–51. [Google Scholar] [CrossRef] [PubMed]
- Engelman, S.R. Palliative care and use of animal-assisted therapy. Omega-J. Death Dying 2013, 67, 63–67. [Google Scholar] [CrossRef] [PubMed]
- Mani, I.; Weese, J.S. Pet Therapy: Enhancing Patient Care Through Time with Animals. Am. Fam. Physician 2016, 94, 737–740. [Google Scholar] [PubMed]
- Fleishman, S.B.; Homel, P.; Chen, M.R.; Rosenwald, V.; Abolencia, V.; Gerber, J.; Nadesan, S. Beneficial effects of animal-assisted visits on quality of life during multimodal radiation-chemotherapy regimens. J. Commun. Support Oncol. 2015, 13, 22–26. [Google Scholar] [CrossRef] [PubMed]
- White, J.H.; Quinn, M.; Garland, S.; Dirkse, D.; Wiebe, P.; Hermann, M.; Carlson, L.E. Animal-Assisted Therapy and Counseling Support for Women With Breast Cancer: An Exploration of Patient’s Perceptions. Integr. Cancer Ther. 2015, 14, 460–467. [Google Scholar] [CrossRef] [PubMed]
- Marcus, D.A.; Blazek-O’Neill, B.; Kopar, J.L. Symptom reduction identified after offering animal-assisted activity at a cancer infusion center. Am. J. Hosp. Palliat. Care 2014, 31, 420–421. [Google Scholar] [CrossRef] [PubMed]
- Lynch, C.E.; Magann, E.F.; Barringer, S.N.; Ounpraseuth, S.T.; Eastham, D.G.; Lewis, S.D.; Stowe, Z.N. Pet therapy program for antepartum high-risk pregnancies: A pilot study. J. Perinatol. 2014, 34, 816–818. [Google Scholar] [CrossRef] [PubMed]
- Calcaterra, V.; Veggiotti, P.; Palestrini, C.; De Giorgis, V.; Raschetti, R.; Tumminelli, M.; Mencherini, S.; Papotti, F.; Klersy, C.; Albertini, R.; et al. Post-operative benefits of animal-assisted therapy in pediatric surgery: A randomised study. PLoS ONE 2015, 10, e0125813. [Google Scholar] [CrossRef] [PubMed]
- Munoz Lasa, S.; Maximo Bocanegra, N.; Valero Alcaide, R.; Atin Arratibel, M.A.; Varela Donoso, E.; Ferriero, G. Animal assisted interventions in neurorehabilitation: A review of the most recent literature. Neurologia 2015, 30, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Vrbanac, Z.; Zecevic, I.; Ljubic, M.; Belic, M.; Stanin, D.; Bottegaro, N.B.; Jurkic, G.; Skrlin, B.; Bedrica, L.; Zubcic, D. Animal assisted therapy and perception of loneliness in geriatric nursing home residents. Coll. Antropol. 2013, 37, 973–976. [Google Scholar] [PubMed]
- Holt, N.J. Using the experience-sampling method to examine the psychological mechanisms by which participatory art improves wellbeing. Perspect. Public Health 2018, 138, 55–65. [Google Scholar] [CrossRef] [PubMed]
- Baikie, K.A.; Geerligs, L.; Wilhelm, K. Expressive writing and positive writing for participants with mood disorders: An online randomized controlled trial. J. Affect. Disord. 2012, 136, 310–319. [Google Scholar] [CrossRef] [PubMed]
- Noice, T.; Noice, H.; Kramer, A.F. Participatory arts for older adults: A review of benefits and challenges. Gerontologist 2014, 54, 741–753. [Google Scholar] [CrossRef] [PubMed]
- Mohatt, N.V.; Hunter, B.A.; Matlin, S.L.; Golden, J.; Evans, A.C.; Tebes, J.K. From recovery-oriented care to public health: Case studies of participatory public art as a pathway to wellness for persons with behavioral health challenges. J. Psychosoc. Rehabil. Ment. Health 2015, 2, 9–18. [Google Scholar] [CrossRef] [PubMed]



© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Petranek, S.; Pencek, J.; Dey, M. The Effect of Pet Therapy and Artist Interactions on Quality of Life in Brain Tumor Patients: A Cross-Section of Art and Medicine in Dialog. Behav. Sci. 2018, 8, 43. https://doi.org/10.3390/bs8050043
Petranek S, Pencek J, Dey M. The Effect of Pet Therapy and Artist Interactions on Quality of Life in Brain Tumor Patients: A Cross-Section of Art and Medicine in Dialog. Behavioral Sciences. 2018; 8(5):43. https://doi.org/10.3390/bs8050043
Chicago/Turabian StylePetranek, Stefan, Jennifer Pencek, and Mahua Dey. 2018. "The Effect of Pet Therapy and Artist Interactions on Quality of Life in Brain Tumor Patients: A Cross-Section of Art and Medicine in Dialog" Behavioral Sciences 8, no. 5: 43. https://doi.org/10.3390/bs8050043
APA StylePetranek, S., Pencek, J., & Dey, M. (2018). The Effect of Pet Therapy and Artist Interactions on Quality of Life in Brain Tumor Patients: A Cross-Section of Art and Medicine in Dialog. Behavioral Sciences, 8(5), 43. https://doi.org/10.3390/bs8050043



