Improved Socio-Emotional and Behavioral Functioning in Students with Autism Following School-Based Smartglasses Intervention: Multi-Stage Feasibility and Controlled Efficacy Study
Abstract
1. Introduction
2. Addressing Social Communication, Irritability, and ADHD Symptoms through Technology
- Assess the feasibility of the longitudinal use of this technology in real-world classrooms.
- Assess the efficacy of the intervention by measuring irritability, hyperactivity, and social withdrawal, using a validated scale.
- Allow facilitation of the intervention by a range of educators that typically provides behavioral interventions in the classroom, including special education teachers and speech and language therapists (SLTs).
- Provide the intervention longitudinally over two weeks with twice-daily interventions during school days, overcoming prior limitations focusing on outcomes related to a single intervention session.
- Have multiple raters: in this study, every student had pre- and post-intervention ratings completed by a special educator teacher and an SLT.
3. Methodology
3.1 The Technology
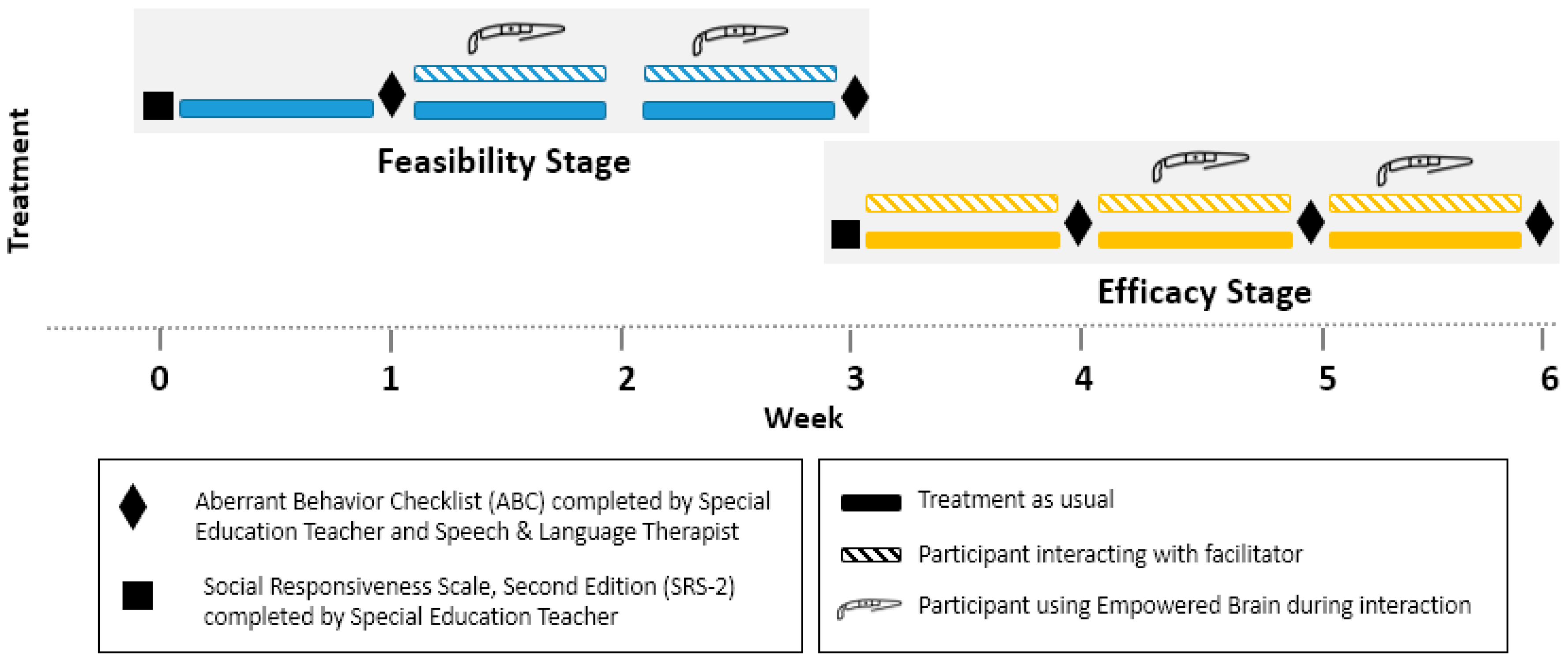
3.2. Study Design
3.3. The Intervention
3.4. The Setting and Participants
3.5. The Control and Intervention Facilitators
3.6. Consent and Institutional Review Board (IRB) Status
4. Results
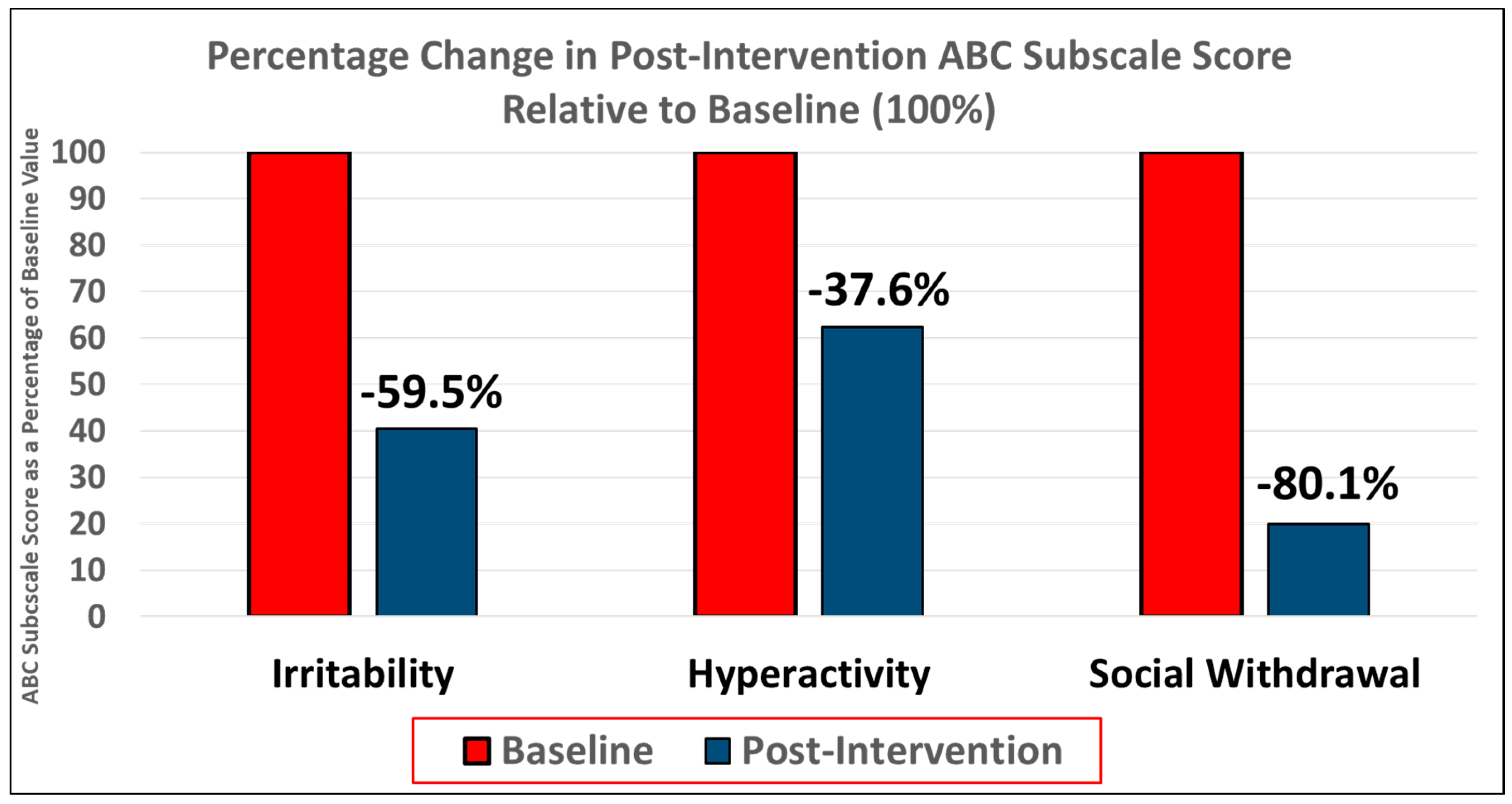
4.1. Feasibility Stage
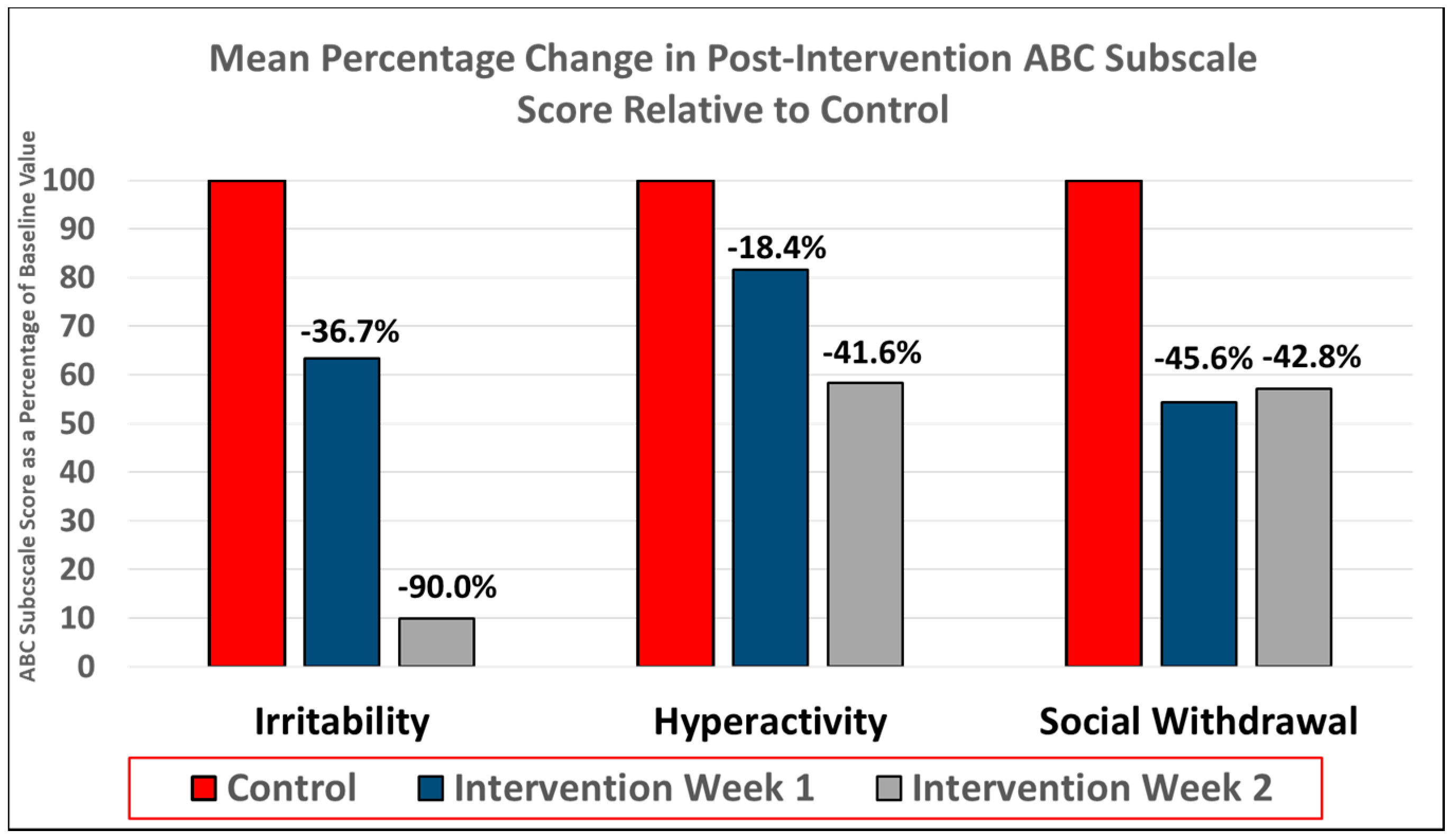
4.2. Controlled Efficacy Stage
4.3. Educator perception of Empowered Brain
5. Discussion
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Association, A.P. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®); American Psychiatric Publishing: Washington, DC, USA, 2013. [Google Scholar]
- Simonoff, E.; Jones, C.R.; Pickles, A.; Happé, F.; Baird, G.; Charman, T. Severe mood problems in adolescents with autism spectrum disorder. J. Child Psychol. Psychiatry 2012, 53, 1157–1166. [Google Scholar] [CrossRef] [PubMed]
- Mansour, R.; Dovi, A.T.; Lane, D.M.; Loveland, K.A.; Pearson, D.A. ADHD severity as it relates to comorbid psychiatric symptomatology in children with Autism Spectrum Disorders (ASD). Res. Dev. Disabil. 2017, 60, 52–64. [Google Scholar] [CrossRef] [PubMed]
- McGuire, K.; Fung, L.K.; Hagopian, L.; Vasa, R.A.; Mahajan, R.; Bernal, P.; Silberman, A.E.; Wolfe, A.; Coury, D.L.; Hardan, A.Y. Irritability and problem behavior in autism spectrum disorder: A practice pathway for pediatric primary care. Pediatrics 2016, 137, S136–S148. [Google Scholar] [CrossRef] [PubMed]
- O’Nions, E.; Happé, F.; Evers, K.; Boonen, H.; Noens, I. How do Parents Manage Irritability, Challenging Behaviour, Non-Compliance and Anxiety in Children with Autism Spectrum Disorders? A Meta-Synthesis. J. Autism Dev. Disord. 2018, 48, 1272–1286. [Google Scholar] [CrossRef] [PubMed]
- Biederman, J.; Monuteaux, M.C.; Doyle, A.E.; Seidman, L.J.; Wilens, T.E.; Ferrero, F.; Morgan, C.L.; Faraone, S.V. Impact of executive function deficits and attention-deficit/hyperactivity disorder (ADHD) on academic outcomes in children. J. Consul. Clin. Psychol. 2004, 72, 757. [Google Scholar] [CrossRef] [PubMed]
- Worley, J.A.; Matson, J.L. Comparing symptoms of autism spectrum disorders using the current DSM-IV-TR diagnostic criteria and the proposed DSM-V diagnostic criteria. Res. Autism Spectr. Disord. 2012, 6, 965–970. [Google Scholar] [CrossRef]
- Asperger, H.; Frith, U.T. ‘Autistic Psychopathy’ in Childhood; Cambridge University Press: Cambridge, UK, 1991. [Google Scholar]
- Kanner, L. Autistic disturbances of affective contact. Nerv. Child 1943, 2, 217–250. [Google Scholar]
- Howlin, P.; Moss, P.; Savage, S.; Rutter, M. Social outcomes in mid-to later adulthood among individuals diagnosed with autism and average nonverbal IQ as children. J. Am. Acad. Child Adolesc. Psychiatry 2013, 52, 572–581. [Google Scholar] [CrossRef] [PubMed]
- Magiati, I.; Tay, X.W.; Howlin, P. Cognitive, language, social and behavioural outcomes in adults with autism spectrum disorders: A systematic review of longitudinal follow-up studies in adulthood. Clin. Psychol. Rev. 2014, 34, 73–86. [Google Scholar] [CrossRef] [PubMed]
- McConnell, S.R. Interventions to facilitate social interaction for young children with autism: Review of available research and recommendations for educational intervention and future research. J. Autism Dev. Disord. 2002, 32, 351–372. [Google Scholar] [CrossRef] [PubMed]
- Pickles, A.; Le Couteur, A.; Leadbitter, K.; Salomone, E.; Cole-Fletcher, R.; Tobin, H.; Gammer, I.; Lowry, J.; Vamvakas, G.; Byford, S. Parent-mediated social communication therapy for young children with autism (PACT): Long-term follow-up of a randomised controlled trial. Lancet 2016, 388, 2501–2509. [Google Scholar] [CrossRef]
- Mayes, S.D.; Calhoun, S.L.; Murray, M.J.; Ahuja, M.; Smith, L.A. Anxiety, depression, and irritability in children with autism relative to other neuropsychiatric disorders and typical development. Res. Autism Spectr. Disord. 2011, 5, 474–485. [Google Scholar] [CrossRef]
- Lecavalier, L. Behavioral and emotional problems in young people with pervasive developmental disorders: Relative prevalence, effects of subject characteristics, and empirical classification. J. Autism Dev. Disord. 2006, 36, 1101–1114. [Google Scholar] [CrossRef] [PubMed]
- Arnold, L.E.; Vitiello, B.; McDougle, C.; Scahill, L.; Shah, B.; Gonzalez, N.M.; Chuang, S.; Davies, M.; Hollway, J.; Aman, M.G. Parent-defined target symptoms respond to risperidone in RUPP autism study: Customer approach to clinical trials. J. Am. Acad. Child Adolesc. Psychiatry 2003, 42, 1443–1450. [Google Scholar] [CrossRef] [PubMed]
- Davis, N.O.; Carter, A.S. Parenting stress in mothers and fathers of toddlers with autism spectrum disorders: Associations with child characteristics. J. Autism Dev. Disord. 2008, 38, 1278. [Google Scholar] [CrossRef] [PubMed]
- Robb, A.S. Managing irritability and aggression in autism spectrum disorders in children and adolescents. Dev. Disabil. Res. Rev. 2010, 16, 258–264. [Google Scholar] [CrossRef] [PubMed]
- Mazefsky, C.A.; White, S.W. Emotion regulation: Concepts & practice in autism spectrum disorder. Child Adolesc. Psychiatr. Clin. N. Am. 2014, 23. [Google Scholar] [CrossRef]
- Richey, J.A.; Damiano, C.R.; Sabatino, A.; Rittenberg, A.; Petty, C.; Bizzell, J.; Voyvodic, J.; Heller, A.S.; Coffman, M.C.; Smoski, M. Neural mechanisms of emotion regulation in autism spectrum disorder. J. Autism Dev. Disord. 2015, 45, 3409–3423. [Google Scholar] [CrossRef] [PubMed]
- Weiss, J.A.; Thomson, K.; Burnham Riosa, P.; Albaum, C.; Chan, V.; Maughan, A.; Tablon, P.; Black, K. A randomized waitlist-controlled trial of cognitive behavior therapy to improve emotion regulation in children with autism. J. Child Psychol. Psychiatry 2018. [Google Scholar] [CrossRef] [PubMed]
- Owen, R.; Sikich, L.; Marcus, R.N.; Corey-Lisle, P.; Manos, G.; McQuade, R.D.; Carson, W.H.; Findling, R.L. Aripiprazole in the treatment of irritability in children and adolescents with autistic disorder. Pediatrics 2009, 124, 1533–1540. [Google Scholar] [CrossRef] [PubMed]
- McCracken, J.T.; McGough, J.; Shah, B.; Cronin, P.; Hong, D.; Aman, M.G.; Arnold, L.E.; Lindsay, R.; Nash, P.; Hollway, J. Risperidone in children with autism and serious behavioral problems. N. Engl. J. Med. 2002, 347, 314–321. [Google Scholar] [CrossRef] [PubMed]
- Hellings, J.A.; Zarcone, J.R.; Crandall, K.; Wallace, D.; Schroeder, S.R. Weight gain in a controlled study of risperidone in children, adolescents and adults with mental retardation and autism. J. Child Adolesc. Psychopharmacol. 2001, 11, 229–238. [Google Scholar] [CrossRef] [PubMed]
- Anderson, G.M.; Scahill, L.; McCracken, J.T.; McDougle, C.J.; Aman, M.G.; Tierney, E.; Arnold, L.E.; Martin, A.; Katsovich, L.; Posey, D.J. Effects of short-and long-term risperidone treatment on prolactin levels in children with autism. Biol. Psychiatry 2007, 61, 545–550. [Google Scholar] [CrossRef] [PubMed]
- Hampshire, P.K.; Butera, G.D.; Bellini, S. Self-management and parents as interventionists to improve homework independence in students with autism spectrum disorders. Prev. Sch. Fail. Altern. Educ. Child. Youth 2016, 60, 22–34. [Google Scholar] [CrossRef]
- Neely-Barnes, S.L.; Hall, H.R.; Roberts, R.J.; Graff, J.C. Parenting a child with an autism spectrum disorder: Public perceptions and parental conceptualizations. J. Fam. Soc. Work 2011, 14, 208–225. [Google Scholar] [CrossRef]
- Larson, E. Caregiving and autism: How does children’s propensity for routinization influence participation in family activities? OTJR Occup. Particip. Health 2006, 26, 69–79. [Google Scholar] [CrossRef]
- Johnson, N.L.; Bekhet, A.; Robinson, K.; Rodriguez, D. Attributed meanings and strategies to prevent challenging behaviors of hospitalized children with autism: Two perspectives. J. Pediat. Health Care 2014, 28, 386–393. [Google Scholar] [CrossRef] [PubMed]
- Bagatell, N. The routines and occupations of families with adolescents with autism spectrum disorders. Focus Autism Dev. Disabil. 2016, 31, 49–59. [Google Scholar] [CrossRef]
- Fettig, A.; Schultz, T.R.; Sreckovic, M.A. Effects of coaching on the implementation of functional assessment–based parent intervention in reducing challenging behaviors. J. Posit. Behav. Interv. 2015, 17, 170–180. [Google Scholar] [CrossRef]
- McEvoy, R.E.; Rogers, S.J.; Pennington, B.F. Executive function and social communication deficits in young autistic children. J. Child Psychol. Psychiatry 1993, 34, 563–578. [Google Scholar] [CrossRef] [PubMed]
- McClintock, K.; Hall, S.; Oliver, C. Risk markers associated with challenging behaviours in people with intellectual disabilities: A meta-analytic study. J. Intellect. Disabil. Res. 2003, 47, 405–416. [Google Scholar] [CrossRef] [PubMed]
- Kurtz, P.F.; Boelter, E.W.; Jarmolowicz, D.P.; Chin, M.D.; Hagopian, L.P. An analysis of functional communication training as an empirically supported treatment for problem behavior displayed by individuals with intellectual disabilities. Res. Dev. Disabil. 2011, 32, 2935–2942. [Google Scholar] [CrossRef] [PubMed]
- Simonoff, E.; Pickles, A.; Charman, T.; Chandler, S.; Loucas, T.; Baird, G. Psychiatric disorders in children with autism spectrum disorders: Prevalence, comorbidity, and associated factors in a population-derived sample. J. Am. Acad. Child Adolesc. Psychiatry 2008, 47, 921–929. [Google Scholar] [CrossRef] [PubMed]
- Loe, I.M.; Feldman, H.M. Academic and educational outcomes of children with ADHD. J. Pediatr. Psychol. 2007, 32, 643–654. [Google Scholar] [CrossRef] [PubMed]
- Bussing, R.; Porter, P.; Zima, B.T.; Mason, D.; Garvan, C.; Reid, R. Academic outcome trajectories of students with ADHD: Does exceptional education status matter? J. Emot. Behav. Disord. 2012, 20, 131–143. [Google Scholar] [CrossRef]
- Gadow, K.D.; DeVincent, C.J.; Schneider, J. Comparative study of children with ADHD only, autism spectrum disorder+ ADHD, and chronic multiple tic disorder+ ADHD. J. Atten. Disord. 2009, 12, 474–485. [Google Scholar] [CrossRef] [PubMed]
- Guttmann-Steinmetz, S.; Gadow, K.D.; DeVincent, C.J. Oppositional defiant and conduct disorder behaviors in boys with autism spectrum disorder with and without attention-deficit hyperactivity disorder versus several comparison samples. J. Autism Dev. Disord. 2009, 39, 976–985. [Google Scholar] [CrossRef] [PubMed]
- Colombi, C.; Ghaziuddin, M. Neuropsychological Characteristics of Children with Mixed Autism and ADHD. Autism Res. Treat. 2017, 2017, 5781781. [Google Scholar] [CrossRef] [PubMed]
- Sikora, D.M.; Vora, P.; Coury, D.L.; Rosenberg, D. Attention-deficit/hyperactivity disorder symptoms, adaptive functioning, and quality of life in children with autism spectrum disorder. Pediatrics 2012, 130, S91–S97. [Google Scholar] [CrossRef] [PubMed]
- Joshi, G.; Faraone, S.V.; Wozniak, J.; Tarko, L.; Fried, R.; Galdo, M.; Furtak, S.L.; Biederman, J. Symptom Profile of ADHD in Youth With High-Functioning Autism Spectrum Disorder: A Comparative Study in Psychiatrically Referred Populations. J. Atten. Disord. 2017, 21, 846–855. [Google Scholar] [CrossRef] [PubMed]
- Autism, N. Randomized, controlled, crossover trial of methylphenidate in pervasive developmental disorders with hyperactivity. Arch. Gen. Psychiatry 2005, 62, 1266–1274. [Google Scholar]
- Erickson, C.A.; Posey, D.J.; Stigler, K.A.; Mullett, J.; Katschke, A.R.; McDougle, C.J. A retrospective study of memantine in children and adolescents with pervasive developmental disorders. Psychopharmacology 2007, 191, 141. [Google Scholar] [CrossRef] [PubMed]
- Grynszpan, O.; Weiss, P.L.; Perez-Diaz, F.; Gal, E. Innovative technology-based interventions for autism spectrum disorders: A meta-analysis. Autism 2014, 18, 346–361. [Google Scholar] [CrossRef] [PubMed]
- Gresham, F.M.; Elliott, S.N. The relationship between adaptive behavior and social skills: Issues in definition and assessment. J. Spec. Educ. 1987, 21, 167–181. [Google Scholar] [CrossRef]
- Baker, J.T.; Germine, L.T.; Ressler, K.J.; Rauch, S.L.; Carlezon, J.W. Digital devices and continuous telemetry: Opportunities for aligning psychiatry and neuroscience. Neuropsychopharmacology 2018. [Google Scholar] [CrossRef] [PubMed]
- Tobar-Muñoz, H.; Fabregat, R.; Baldiris, S. Augmented reality game-based learning for mathematics skills training in inclusive contexts. Inf. Educ. Comun. 2015, 21, 39–51. [Google Scholar]
- Escobedo, L.; Nguyen, D.H.; Boyd, L.; Hirano, S.; Rangel, A.; Garcia-Rosas, D.; Tentori, M.; Hayes, G. MOSOCO: A mobile assistive tool to support children with autism practicing social skills in real-life situations. In Proceedings of the SIGCHI Conference on Human Factors in Computing Systems, Austin, TX, USA, 5–10 May 2012; pp. 2589–2598. [Google Scholar]
- Chen, C.-H.; Lee, I.-J.; Lin, L.-Y. Augmented reality-based self-facial modeling to promote the emotional expression and social skills of adolescents with autism spectrum disorders. Res. Dev. Disabil. 2015, 36, 396–403. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.-H.; Lee, I.-J.; Lin, L.-Y. Augmented reality-based video-modeling storybook of nonverbal facial cues for children with autism spectrum disorder to improve their perceptions and judgments of facial expressions and emotions. Comput. Hum. Behav. 2016, 55, 477–485. [Google Scholar] [CrossRef]
- Cunha, P.; Brandão, J.; Vasconcelos, J.; Soares, F.; Carvalho, V. Augmented reality for cognitive and social skills improvement in children with ASD. In Proceedings of the 2016 13th International Conference on Remote Engineering and Virtual Instrumentation (REV), Madrid, Spain, 24–26 February 2016; pp. 334–335. [Google Scholar]
- Escobedo, L.; Tentori, M.; Quintana, E.; Favela, J.; Garcia-Rosas, D. Using augmented reality to help children with autism stay focused. IEEE Pervasive Comput. 2014, 13, 38–46. [Google Scholar] [CrossRef]
- Liu, R.; Salisbury, J.P.; Vahabzadeh, A.; Sahin, N.T. Feasibility of an Autism-Focused Augmented Reality Smartglasses System for Social Communication and Behavioral Coaching. Front. Pediatr. 2017, 5, 145. [Google Scholar] [CrossRef] [PubMed]
- Keshav, N.U.; Salisbury, J.P.; Vahabzadeh, A.; Sahin, N.T. Social Communication Coaching Smartglasses: Well Tolerated in a Diverse Sample of Children and Adults With Autism. JMIR mHealth uHealth 2017, 5, e140. [Google Scholar] [CrossRef] [PubMed]
- Sahin, N.T.; Keshav, N.U.; Salisbury, J.P.; Vahabzadeh, A. Second Version of Google Glass as a Wearable Socio-Affective Aid: Positive School Desirability, High Usability, and Theoretical Framework in a Sample of Children with Autism. JMIR Hum. Factors 2018, 5, e1. [Google Scholar] [CrossRef] [PubMed]
- Sahin, N.T.; Keshav, N.U.; Salisbury, J.P.; Vahabzadeh, A. Safety and Lack of Negative Effects of Wearable Augmented-Reality Social Communication Aid for Children and Adults with Autism. bioRxiv 2017. [Google Scholar] [CrossRef]
- Vahabzadeh, A.; Keshav, N.U.; Salisbury, J.P.; Sahin, N.T. Improvement of Attention-Deficit/Hyperactivity Disorder Symptoms in School-Aged Children, Adolescents, and Young Adults With Autism via a Digital Smartglasses-Based Socioemotional Coaching Aid: Short-Term, Uncontrolled Pilot Study. JMIR Ment. Health 2018, 5, e25. [Google Scholar] [CrossRef] [PubMed]
- Keshav, N.; Vahabzadeh, A.; Abdus-Sabur, R.; Huey, K.; Salisbury, J.; Liu, R.; Sahin, N. Longitudinal Socio-Emotional Learning Intervention for Autism via Smartglasses: Qualitative School Teacher Descriptions of Practicality, Usability, and Efficacy in General and Special Education Classroom Settings. Educ. Sci. 2018, 8, 107. [Google Scholar] [CrossRef]
- Sahin, N.T.; Abdus-Sabur, R.; Keshav, N.U.; Liu, R.; Salisbury, J.P.; Vahabzadeh, A. Case Study of a Digital Augmented Reality Intervention for Autism in School Classrooms: Associated with Improved Social Communication, Cognition, and Motivation as rated by Educators and Parents. Front. Educ. 2018, 3, 57. [Google Scholar] [CrossRef]
- Kinsella, B.G.; Chow, S.; Kushki, A. Evaluating the usability of a wearable social skills training technology for children with autism spectrum disorder. Front. Robot. AI 2017, 4, 31. [Google Scholar]
- Daniels, J.; Schwartz, J.N.; Voss, C.; Haber, N.; Fazel, A.; Kline, A.; Washington, P.; Feinstein, C.; Winograd, T.; Wall, D.P. Exploratory study examining the at-home feasibility of a wearable tool for social-affective learning in children with autism. npj Digit. Med. 2018, 1, 32. [Google Scholar] [CrossRef]
- Aman, M.G.; Singh, N.N.; Stewart, A.W.; Field, C.J. The aberrant behavior checklist: A behavior rating scale for the assessment of treatment effects. Am. J. Ment. Defic. 1985, 89, 485–491. [Google Scholar] [PubMed]
- Aman, M.G.; Singh, N.N.; Stewart, A.W.; Field, C.J. Psychometric characteristics of the aberrant behavior checklist. Am. J. Ment. Defic. 1985, 89, 492–502. [Google Scholar] [PubMed]
- Shea, S.; Turgay, A.; Carroll, A.; Schulz, M.; Orlik, H.; Smith, I.; Dunbar, F. Risperidone in the treatment of disruptive behavioral symptoms in children with autistic and other pervasive developmental disorders. Pediatrics 2004, 114, e634–e641. [Google Scholar] [CrossRef] [PubMed]
- Hellings, J.A.; Zarcone, J.R.; Reese, R.M.; Valdovinos, M.G.; Marquis, J.G.; Fleming, K.K.; Schroeder, S.R. A crossover study of risperidone in children, adolescents and adults with mental retardation. J. Autism Dev. Disord. 2006, 36, 401–411. [Google Scholar] [CrossRef] [PubMed]
- Marcus, R.N.; Owen, R.; Kamen, L.; Manos, G.; McQuade, R.D.; Carson, W.H.; Aman, M.G. A placebo-controlled, fixed-dose study of aripiprazole in children and adolescents with irritability associated with autistic disorder. J. Am. Acad. Child Adolesc. Psychiatry 2009, 48, 1110–1119. [Google Scholar] [CrossRef] [PubMed]
- Elbe, D.; Lalani, Z. Review of the pharmacotherapy of irritability of autism. J. Can. Acad. Child Adolesc. Psychiatry 2012, 21, 130. [Google Scholar] [PubMed]
- Arnold, L.E.; Aman, M.G.; Cook, A.M.; Witwer, A.N.; Hall, K.L.; Thompson, S.; Ramadan, Y. Atomoxetine for hyperactivity in autism spectrum disorders: Placebo-controlled crossover pilot trial. J. Am. Acad. Child Adolesc. Psychiatry 2006, 45, 1196–1205. [Google Scholar] [CrossRef] [PubMed]
- Bent, S.; Hendren, R.L.; Zandi, T.; Law, K.; Choi, J.-E.; Widjaja, F.; Kalb, L.; Nestle, J.; Law, P. Internet-based, randomized, controlled trial of omega-3 fatty acids for hyperactivity in autism. J. Am. Acad. Child Adolesc. Psychiatry 2014, 53, 658–666. [Google Scholar] [CrossRef] [PubMed]
- Yui, K.; Koshiba, M.; Nakamura, S.; Kobayashi, Y. Effects of large doses of arachidonic acid added to docosahexaenoic acid on social impairment in individuals with autism spectrum disorders: A double-blind, placebo-controlled, randomized trial. J. Clin. Psychopharmacol. 2012, 32, 200–206. [Google Scholar] [CrossRef] [PubMed]
- King, B.H.; Wright, D.M.; Handen, B.L.; Sikich, L.; Zimmerman, A.W.; McMahon, W.; Cantwell, E.; Davanzo, P.A.; Dourish, C.T.; Dykens, E.M. Double-blind, placebo-controlled study of amantadine hydrochloride in the treatment of children with autistic disorder. J. Am. Acad. Child Adolesc. Psychiatry 2001, 40, 658–665. [Google Scholar] [CrossRef] [PubMed]
- Salisbury, J.P.; Keshav, N.U.; Sossong, A.D.; Sahin, N.T. Concussion Assessment With Smartglasses: Validation Study of Balance Measurement Toward a Lightweight, Multimodal, Field-Ready Platform. JMIR mHealth uHealth 2018, 6, e15. [Google Scholar] [CrossRef] [PubMed]
- Farr, W.; Male, I.; Green, D.; Morris, C.; Gage, H.; Bailey, S.; Speller, S.; Colville, V.; Jackson, M.; Bremner, S. Current issues and challenges in research on virtual reality therapy for children with neurodisability. In Proceedings of the 11th International Conference in Disability, Virtual Reality and Associated Technologies, Los Angeles, CA, USA, 20–22 September 2016; pp. 9–26. [Google Scholar]
- Horner, R.H.; Carr, E.G.; Halle, J.; McGee, G.; Odom, S.; Wolery, M. The use of single-subject research to identify evidence-based practice in special education. Except. Child. 2005, 71, 165–179. [Google Scholar] [CrossRef]
- Kratochwill, T.R.; Levin, J.R. Enhancing the scientific credibility of single-case intervention research: Randomization to the rescue. Psychol. Methods 2010, 15, 124. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.D. Single-case experimental designs: A systematic review of published research and current standards. Psychol. Methods 2012, 17, 510. [Google Scholar] [CrossRef] [PubMed]
- Robey, R.R.; Schultz, M.C.; Crawford, A.B.; Sinner, C.A. Single-subject clinical-outcome research: Designs, data, effect sizes, and analyses. Aphasiology 1999, 13, 445–473. [Google Scholar] [CrossRef]
- Borckardt, J.J.; Nash, M.R.; Murphy, M.D.; Moore, M.; Shaw, D.; O’neil, P. Clinical practice as natural laboratory for psychotherapy research: A guide to case-based time-series analysis. Am. Psychol. 2008, 63, 77. [Google Scholar] [CrossRef] [PubMed]
- Zaczynski, M. Efficacy Before Novelty: Establishing Design Guidelines in Interactive Gaming for Rehabilitation and Training; Carleton University: Ottawa, ON, Canada, 2013. [Google Scholar]
- Constantino, J.N.; Gruber, C.P. Social Responsiveness Scale (SRS); Western Psychological Services: Torrance, CA, USA, 2012. [Google Scholar]

| No. of Multisite IRB * Approved Programs | 2 (2016 and 2017) |
|---|---|
| Current Number of Research Sites | 8+ |
| Demonstrated Feasibility | Liu et al. [54] |
| High Usability | Sahin et al. [56] Keshav et al. [59] |
| High Desirability | Sahin et al. [56] |
| High Tolerability | Keshav et al. [55] |
| Safety Study | Sahin et al. [57] |
| Improvement in Social Communication | Sahin et al. [60] Keshav et al. [59] Liu et al. [54] |
| Improvement in ADHD **-related symptoms | Vahabzadeh et al. [58] Liu et al. [54] |
| Demonstration of Positive Teacher Perception | Keshav et al. [59] |
| Rater | ABC Subscale | Baseline | Post-Intervention |
|---|---|---|---|
| Special Education Teacher Rater | Irritability | 21 | 10 |
| Lethargy | 1 | 0 | |
| Stereotypy | 4 | 1 | |
| Hyperactivity | 11 | 6 | |
| Inappropriate Speech | 0 | 0 | |
| Speech and Language Therapist Rater | Irritability | 9 | 3 |
| Lethargy | 7 | 3 | |
| Stereotypy | 0 | 0 | |
| Hyperactivity | 7 | 7 | |
| Inappropriate Speech | 1 | 0 |
| Rater | ABC Subscale | Baseline | Post-Intervention |
|---|---|---|---|
| Special Education Teacher Rater | Irritability | 10 | 0 |
| Lethargy | 11 | 1 | |
| Stereotypy | 7 | 2 | |
| Hyperactivity | 13 | 4 | |
| Inappropriate Speech | 4 | 4 | |
| Speech and Language Therapist Rater | Irritability | 13 | 3 |
| Lethargy | 18 | 5 | |
| Stereotypy | 0 | 1 | |
| Hyperactivity | 14 | 9 | |
| Inappropriate. Speech | 2 | 2 |
| Rater | ABC Subscale | Time Point | ||
|---|---|---|---|---|
| Control Week | Intervention Week 1 | Intervention Week 2 | ||
| Special Education Teacher Rater | Irritability | 5 | 1 | 2 |
| Lethargy | 2 | 0 | 2 | |
| Stereotypy | 1 | 1 | 1 | |
| Hyperactivity | 42 | 28 | 20 | |
| Inappropriate Speech | 2 | 2 | 1 | |
| Speech and Language Therapist Rater | Irritability | 1 | 1 | 0 |
| Lethargy | 5 | 4 | 2 | |
| Stereotypy | 1 | 0 | 0 | |
| Hyperactivity | 23 | 14 | 12 | |
| Inappropriate Speech | 1 | 1 | 0 | |
| Rater | ABC Subscale | Time Point | ||
|---|---|---|---|---|
| Control Week | Intervention Week 1 | Intervention Week 2 | ||
| Special Education Teacher Rater | Irritability | 3 | 1 | 0 |
| Lethargy | 17 | 10 | 9 | |
| Stereotypy | 10 | 5 | 4 | |
| Hyperactivity | 27 | 19 | 13 | |
| Inappropriate Speech | 3 | 2 | 2 | |
| Speech and Language Therapist Rater | Irritability | 2 | 2 | 0 |
| Lethargy | 14 | 11 | 5 | |
| Stereotypy | 1 | 2 | 0 | |
| Hyperactivity | 7 | 9 | 6 | |
| Inappropriate Speech | 3 | 2 | 1 | |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vahabzadeh, A.; Keshav, N.U.; Abdus-Sabur, R.; Huey, K.; Liu, R.; Sahin, N.T. Improved Socio-Emotional and Behavioral Functioning in Students with Autism Following School-Based Smartglasses Intervention: Multi-Stage Feasibility and Controlled Efficacy Study. Behav. Sci. 2018, 8, 85. https://doi.org/10.3390/bs8100085
Vahabzadeh A, Keshav NU, Abdus-Sabur R, Huey K, Liu R, Sahin NT. Improved Socio-Emotional and Behavioral Functioning in Students with Autism Following School-Based Smartglasses Intervention: Multi-Stage Feasibility and Controlled Efficacy Study. Behavioral Sciences. 2018; 8(10):85. https://doi.org/10.3390/bs8100085
Chicago/Turabian StyleVahabzadeh, Arshya, Neha U. Keshav, Rafiq Abdus-Sabur, Krystal Huey, Runpeng Liu, and Ned T. Sahin. 2018. "Improved Socio-Emotional and Behavioral Functioning in Students with Autism Following School-Based Smartglasses Intervention: Multi-Stage Feasibility and Controlled Efficacy Study" Behavioral Sciences 8, no. 10: 85. https://doi.org/10.3390/bs8100085
APA StyleVahabzadeh, A., Keshav, N. U., Abdus-Sabur, R., Huey, K., Liu, R., & Sahin, N. T. (2018). Improved Socio-Emotional and Behavioral Functioning in Students with Autism Following School-Based Smartglasses Intervention: Multi-Stage Feasibility and Controlled Efficacy Study. Behavioral Sciences, 8(10), 85. https://doi.org/10.3390/bs8100085





