Perceived Resilience, Meaningful Work, and Mental Health Strain Among Emergency Medicine Clinicians Following a Surge in COVID-19
Abstract
1. Introduction
Literature Review
2. Materials and Methods
2.1. Participants and Procedure
2.2. Measures
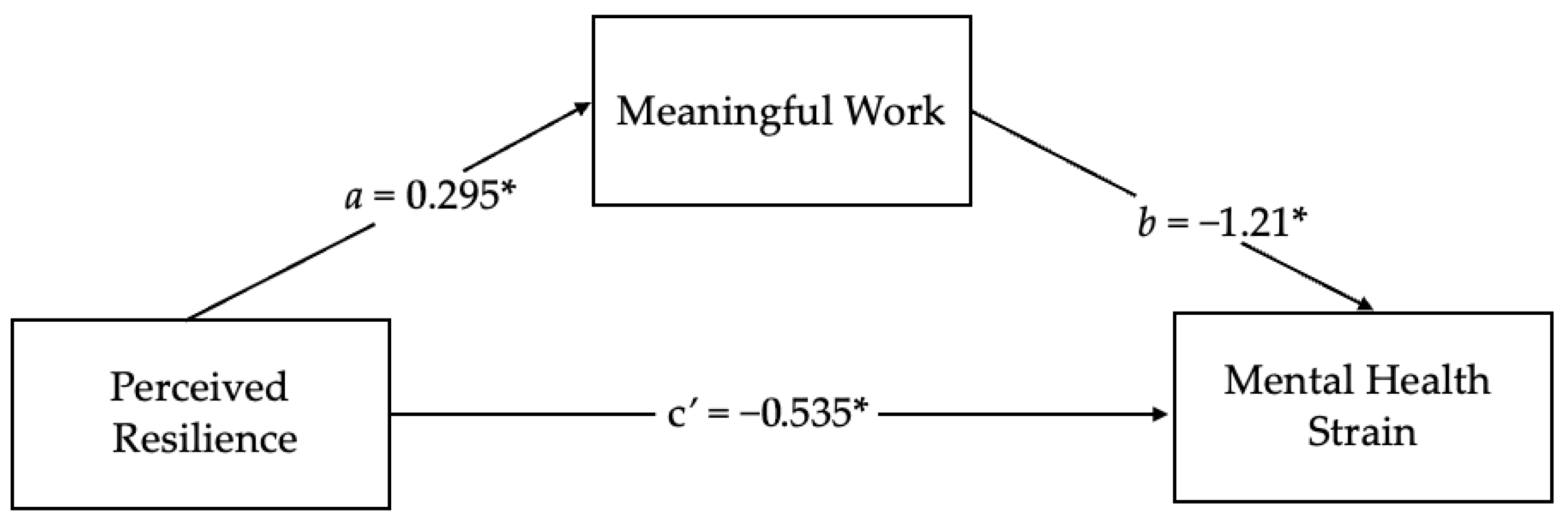
3. Results
4. Discussion
Limitations and Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ahalt, V., Argon, N. T., Ziya, S., Strickler, J., & Mehrotra, A. (2018). Comparison of emergency department crowding scores: A discrete-event simulation approach. Health Care Management Science, 21(1), 144–155. [Google Scholar] [CrossRef]
- Ali, S., Thomson, D., D Graham, T. A., Rickard, S. E., & Stang, A. S. (2017). High stakes and high emotions: Providing safe care in Canadian emergency departments. Open Access Emergency Medicine, 9, 23–26. [Google Scholar] [CrossRef]
- AlQarni, A. M., Elfaki, A., Abdel Wahab, M. M., Aljehani, Y., ALKhunaizi, A. A., Othman, S. A., & AlShamlan, R. A. (2023). Psychological resilience, anxiety, and well-being of health care providers during the COVID-19 pandemic. Journal of Multidisciplinary Healthcare, 16, 1327–1335. [Google Scholar] [CrossRef]
- Arslan, G., & Yıldırım, M. (2021). A longitudinal examination of the association between meaning in life, resilience, and mental well-being in times of coronavirus pandemic [original research]. Frontiers in Psychology, 12, 645597. Available online: https://www.frontiersin.org/journals/psychology/articles/10.3389/fpsyg.2021.645597 (accessed on 1 October 2025). [CrossRef] [PubMed]
- Bozdağ, F., & Ergün, N. (2021). Psychological resilience of healthcare professionals during COVID-19 pandemic. Psychological Reports, 124(6), 2567–2586. [Google Scholar] [CrossRef]
- Britt, T., Adler, A., & Fynes, J. (2021). Perceived resilience and social connection as predictors of adjustment following occupational adversity. Journal of Occupational Health Psychology, 26, 339–349. [Google Scholar] [CrossRef]
- Britt, T., Shen, W., Sinclair, R., Grossman, M., & Klieger, D. (2016). How much do we really know about employee resilience? Industrial and Organizational Psychology, 9, 378–404. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. (2024, September 22). COVID data tracker. U.S. Department of Health and Human Services, CDC. Available online: https://covid.cdc.gov/covid-data-tracker (accessed on 1 October 2025).
- Chuang, C.-H., Tseng, P.-C., Lin, C.-Y., Lin, K.-H., & Chen, Y.-Y. (2016). Burnout in the intensive care unit professionals: A systematic review. Medicine, 95(50), e5629. [Google Scholar] [CrossRef] [PubMed]
- Curtin, M., Richards, H. L., & Fortune, D. G. (2022). Resilience among health care workers while working during a pandemic: A systematic review and meta synthesis of qualitative studies. Clinical Psychology Review, 95, 102173. [Google Scholar] [CrossRef]
- Drutchas, A., Rusch, R., & Leiter, R. (2024). The palliative story exchange: An innovative storytelling intervention to build community, foster shared meaning, and improve sustainability. Palliative and Supportive Care, 22(6), 2069–2076. [Google Scholar] [CrossRef] [PubMed]
- Dyrbye, L. N., Satele, D., Sloan, J., & Shanafelt, T. D. (2013). Utility of a brief screening tool to identify physicians in distress. Journal of General Internal Medicine, 28(3), 421–427. [Google Scholar] [CrossRef]
- Foster, K., Shakespeare-Finch, J., Shochet, I., Maybery, D., Bui, M. V., Steele, M., & Roche, M. (2024). Psychological distress, well-being, resilience, posttraumatic growth, and turnover intention of mental health nurses during COVID-19: A cross-sectional study. International Journal of Mental Health Nursing, 33(5), 1543–1552. [Google Scholar] [CrossRef] [PubMed]
- Fredrickson, B. L. (2001). The role of positive emotions in positive psychology. The broaden-and-build theory of positive emotions. The American Psychologist, 56(3), 218–226. [Google Scholar] [CrossRef] [PubMed]
- Gloria, C. T., & Steinhardt, M. A. (2016). Relationships among positive emotions, coping, resilience and mental health. Stress Health, 32, 145–156. [Google Scholar] [CrossRef] [PubMed]
- Hayes, A. F. (2022). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach (Vol. 3). The Guilford Press. [Google Scholar]
- Hollinger-Smith, L. M., O’Lynn, C., & Groenwald, S. (2021). The importance of meaningful faculty recognition in creating a healthy academic work environment: A mixed-methods study. Nursing Education Perspectives, 42(5), 297–303. [Google Scholar] [CrossRef]
- Horowitz, C. R., Suchman, A. L., Branch, W. T., & Frankel, R. M. (2003). What do doctors find meaningful about their work? Annals of Internal Medicine, 138(9), 772–775. [Google Scholar] [CrossRef]
- Jachmann, A., Loser, A., Mettler, A., Exadaktylos, A., Müller, M., & Klingberg, K. (2025). Burnout, depression, and stress in emergency department nurses and physicians and the impact on private and work life: A systematic review. Journal of the American College of Emergency Physicians Open, 6(2), 100046. [Google Scholar] [CrossRef]
- Kennett, P., & Lomas, T. (2015). Making meaning through mentoring: Mentors finding fulfilment at work through self-determination and self-reflection. International Journal of Evidence Based Coaching and Mentoring, 13, 29–44. [Google Scholar]
- Killgore, W. D. S. D. S., Cloonan, S. A., Taylor, E. C., Persich, M. R., & Dailey, N. S. (2021). Sleep and resilience during the COVID-19 pandemic. In F. Gabrielli, & F. Irtelli (Eds.), Anxiety, uncertainty, and resilience during the pandemic period—Anthropological and psychological perspectives. IntechOpen. [Google Scholar] [CrossRef]
- Lips-Wiersma, M., & Wright, S. (2012). Measuring the meaning of meaningful work: Development and validation of the comprehensive meaningful work scale (CMWS). Group & Organization Management, 37(5), 655–685. [Google Scholar] [CrossRef]
- Liu, Y., Hou, T., Gu, H., Wen, J., Shao, X., Xie, Y., Deng, W., & Dong, W. (2022). Resilience and anxiety among healthcare workers during the spread of the SARS-CoV-2 delta variant: A moderated mediation model [original research]. Frontiers in Psychiatry, 13, 804538. Available online: https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2022.804538 (accessed on 1 October 2025). [CrossRef]
- McKenna, J. (2024, January 26). Medscape physician burnout & depression report 2024: ‘We have much work to do’. Medscape. Available online: https://www.medscape.com/slideshow/2024-lifestyle-burnout-6016865#3 (accessed on 1 October 2025).
- Montani, F., Boudrias, J. S., & Pigeon, M. (2017). Employee recognition, meaningfulness and behavioural involvement: Test of a moderated mediation model. The International Journal of Human Resource Management, 31(3), 356–384. [Google Scholar] [CrossRef]
- Morales-Solis, J. C., Chen, J., May, D. R., & Schwoerer, C. E. (2022). Resiliency and meaningfulness in work: A job crafting perspective. International Journal of Organizational Analysis, 31(6), 2581–2594. [Google Scholar] [CrossRef]
- Munn, L., Liu, T., Swick, M., Rose, R., Broyhill, B., New, L., & Gibbs, M. (2021). Original research: Well-being and resilience among health care workers during the COVID-19 pandemic: A cross-sectional study. AJN, American Journal of Nursing, 121(8), 24–34. [Google Scholar] [CrossRef]
- Panagioti, M., Panagopoulou, E., Bower, P., Lewith, G., Kontopantelis, E., Chew-Graham, C., Dawson, S., van Marwijk, H., Geraghty, K., & Esmail, A. (2017). Controlled interventions to reduce burnout in physicians: A systematic review and meta-analysis. JAMA Internal Medicine, 177(2), 195–205. [Google Scholar] [CrossRef]
- Pavlish, C., & Hunt, R. (2012). An exploratory study about meaningful work in acute care nursing. Nursing Forum, 47(2), 113–122. [Google Scholar] [CrossRef] [PubMed]
- Podsakoff, P. M., MacKenzie, S. B., Lee, J. Y., & Podsakoff, N. P. (2003). Common method biases in behavioral research: A critical review of the literature and recommended remedies. The Journal of Applied Psychology, 88(5), 879–903. [Google Scholar] [CrossRef]
- Preti, E., Di Mattei, V., Perego, G., Ferrari, F., Mazzetti, M., Taranto, P., Di Pierro, R., Madeddu, F., & Calati, R. (2020). The psychological impact of epidemic and pandemic outbreaks on healthcare workers: Rapid review of the evidence. Current Psychiatry Reports, 22(8), 43. [Google Scholar] [CrossRef] [PubMed]
- Rohland, B., Kruse, G., & Rohrer, J. (2004). Validation of a single-item measure of burnout against the Maslach Burnout Inventory among physicians. Stress and Health, 20, 75–79. [Google Scholar] [CrossRef]
- Ryan, R. M., & Deci, E. L. (2000). Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. The American Psychologist, 55(1), 68–78. [Google Scholar] [CrossRef] [PubMed]
- Saladino, V., Algeri, D., & Auriemma, V. (2020). The psychological and social impact of covid-19: New perspectives of well-being. Frontiers in Psychology, 11, 577684. [Google Scholar] [CrossRef]
- Saladino, V., Auriemma, V., & Campinoti, V. (2022). Healthcare professionals, post-traumatic stress disorder, and COVID-19: A review of the literature. Frontiers in Psychiatry, 12, 795221. [Google Scholar] [CrossRef]
- Shi, X., Xie, P., Zhou, Z., Zhao, Y., Luo, K., Liu, G., & Han, X. (2025). Work experiences, burnout, and psychological distress of frontline health professionals during the COVID-19 omicron epidemic: A multicenter cross-sectional study in Southern China. Human Resources for Health, 23(1), 62. [Google Scholar] [CrossRef] [PubMed]
- Smith, B. W., Dalen, J., Wiggins, K., Tooley, E., Christopher, P., & Bernard, J. (2008). The brief resilience scale: Assessing the ability to bounce back. International Journal of Behavioral Medicine, 15(3), 194–200. [Google Scholar] [CrossRef]
- Steger, M. F., Dik, B. J., & Duffy, R. D. (2012). Measuring meaningful work: The work and meaning inventory (WAMI). Journal of Career Assessment, 20(3), 322–337. [Google Scholar] [CrossRef]
- Sun, P., Wang, M., Song, T., Wu, Y., Luo, J., Chen, L., & Yan, L. (2021). The psychological impact of COVID-19 pandemic on health care workers: A systematic review and meta-analysis [systematic review]. Frontiers in Psychology, 12, 626547. Available online: https://www.frontiersin.org/journals/psychology/articles/10.3389/fpsyg.2021.626547 (accessed on 1 October 2025). [CrossRef]
- Tugade, M. M., & Fredrickson, B. L. (2004). Resilient individuals use positive emotions to bounce back from negative emotional experiences. Journal of Personality and Social Psychology, 86(2), 320–333. [Google Scholar] [CrossRef]
- van Mol, M. M. C., Kompanje, E. J. O., Benoit, D. D., Bakker, J., & Nijkamp, M. D. (2015). The prevalence of compassion fatigue and burnout among healthcare professionals in intensive care units: A systematic review. PLoS ONE, 10(8), e0136955. [Google Scholar] [CrossRef]
- Weiss, S. J., Derlet, R., Arndahl, J., Ernst, A. A., Richards, J., Fernández-Frankelton, M., Schwab, R., Stair, T. O., Vicellio, P., Levy, D., Brautigan, M., Johnson, A., & Nick, T. G. (2004). Estimating the degree of emergency department overcrowding in academic medical centers: Results of the national ED overcrowding study (NEDOCS). Academic Emergency Medicine, 11, 38–50. [Google Scholar] [CrossRef]
- Wiig, S., Aase, K., Billett, S., Canfield, C., Røise, O., Njå, O., Guise, V., Haraldseid-Driftland, C., Ree, E., Anderson, J. E., Macrae, C., & on behalf of the RiH-Team. (2020). Defining the boundaries and operational concepts of resilience in the resilience in healthcare research program. BMC Health Services Research, 20(1), 330. [Google Scholar] [CrossRef]
- Windle, G., Bennett, K. M., & Noyes, J. (2011). A methodological review of resilience measurement scales. Health and Quality of Life Outcomes, 9(1), 1–18. [Google Scholar] [CrossRef] [PubMed]
- Yıldırım, M., Arslan, G., & Özaslan, A. (2022). Perceived risk and mental health problems among healthcare professionals during COVID-19 pandemic: Exploring the mediating effects of resilience and coronavirus fear. International Journal of Mental Health and Addiction, 20(2), 1035–1045. [Google Scholar] [CrossRef] [PubMed]
- Yong, E. (2022, January 7). Hospitals are in serious trouble. The Atlantic Website. Available online: https://www.theatlantic.com/health/archive/2022/01/omicron-mild-hospital-strain-health-care-workers/621193/ (accessed on 23 November 2025).
- Zheng, D., Marbut, A. R., Zhang, J., & O’Keefe, L. C. (2022). The contribution of psychological resilience and job meaningfulness to well-being of working cancer survivors. Workplace Health & Safety, 70(10), 468–478. [Google Scholar] [CrossRef] [PubMed]

| Sample Characteristics | n | % | M | SD |
|---|---|---|---|---|
| Gender | ||||
| Male | 129 | 65.5% | ||
| Female | 68 | 34.5% | ||
| Professional Role | ||||
| Advanced Practice Clinicians | 18 | 9.1% | ||
| Attending | 71 | 36% | ||
| Resident | 14 | 7.1% | ||
| Registered Nurses | 94 | 47.7% | ||
| Race | ||||
| Asian | 7 | 3.6% | ||
| Black or African American | 7 | 3.6% | ||
| Hispanic or Latino | 3 | 1.5% | ||
| Two or More Races | 10 | 5.1% | ||
| White | 170 | 86.3% | ||
| Age | 38.65 | 11.48 |
| Variables | M | SD | 1 | 2 | 3 | ||
|---|---|---|---|---|---|---|---|
| Time 1 | |||||||
| 1. Brief Resilience | 3.60 | 0.60 | - | ||||
| 2. Meaningful Work | 3.65 | 0.61 | 0.29 | *** | - | ||
| Time 2 | |||||||
| 3. Mental Health Strain | 2.32 | 1.84 | −0.29 | *** | −0.46 | *** | - |
| Predictor | b | SE b | β | t | p |
|---|---|---|---|---|---|
| Step 1 | |||||
| Constant | 5.76 | 0.77 | - | 7.49 | <0.001 |
| Role: APC | 0.07 | 0.45 | 0.01 | 0.16 | 0.87 |
| Role: Attending | −0.42 | 0.30 | −0.11 | −1.41 | 0.16 |
| Role: Resident | −0.91 | 0.52 | −0.13 | −1.75 | 0.08 |
| Gender: Male | 0.47 | 0.29 | 0.12 | 1.63 | 0.10 |
| Month: January | −0.30 | 0.64 | −0.03 | −0.47 | 0.64 |
| Month: December | 0.59 | 0.32 | 0.13 | 1.86 | 0.06 |
| Step 2 | |||||
| Perceived Resilience | −0.97 | 0.21 | −0.32 | −4.66 | <0.001 |
| Step 3 | |||||
| Perceived Resilience | −0.60 | 0.21 | −0.20 | −2.92 | 0.004 |
| Meaningful Work | −1.15 | 0.21 | −0.38 | −5.60 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Vosika, E.C.; Britt, T.W.; McCallus, R.L.; Shuffler, M.; Hirsh, E. Perceived Resilience, Meaningful Work, and Mental Health Strain Among Emergency Medicine Clinicians Following a Surge in COVID-19. Behav. Sci. 2026, 16, 10. https://doi.org/10.3390/bs16010010
Vosika EC, Britt TW, McCallus RL, Shuffler M, Hirsh E. Perceived Resilience, Meaningful Work, and Mental Health Strain Among Emergency Medicine Clinicians Following a Surge in COVID-19. Behavioral Sciences. 2026; 16(1):10. https://doi.org/10.3390/bs16010010
Chicago/Turabian StyleVosika, Emma C., Thomas W. Britt, Riley L. McCallus, Marissa Shuffler, and Emily Hirsh. 2026. "Perceived Resilience, Meaningful Work, and Mental Health Strain Among Emergency Medicine Clinicians Following a Surge in COVID-19" Behavioral Sciences 16, no. 1: 10. https://doi.org/10.3390/bs16010010
APA StyleVosika, E. C., Britt, T. W., McCallus, R. L., Shuffler, M., & Hirsh, E. (2026). Perceived Resilience, Meaningful Work, and Mental Health Strain Among Emergency Medicine Clinicians Following a Surge in COVID-19. Behavioral Sciences, 16(1), 10. https://doi.org/10.3390/bs16010010





