Abstract
Objective: Emerging adulthood often involves a greater degree of disordered eating behaviors, especially among women. In this psychosocial context, extant evidence suggests that psychological distress is a major contributing factor to disordered eating behaviors. The present cross-sectional study examined whether psychological distress was positively associated with disordered eating behavior in a sample of emerging adult women, and whether difficulty in emotion regulation, self-concealment, or both together, at least partially explained this association. Method: Participants were 723 emerging adult women aged 18 to 25 years old (Mage = 19.5, SDage = 1.6) who were recruited from a four-year public university in Hawaii, USA. Upon the completion of the informed consent procedure, they voluntarily completed an online survey package that included the self-report measures assessing disordered eating behavior, psychological distress, difficulties in emotion regulation, and self-concealment. Results: We found that psychological distress was positively associated with disordered eating behaviors. We also found that both difficulty in emotion regulation and self-concealment partially accounted for the positive association between psychological distress and disordered eating behavior. Discussion: Future research should examine the conceptual and applied implications of these findings further.
1. Introduction
Emerging adulthood, a developmental period spanning from ages 18 to 25 years old (Arnett, 2007), often involves elevated disordered eating behaviors, especially among women (e.g., Arnett et al., 2014; Potterton et al., 2020). In Westernized cultures, disordered eating behaviors often occur in secret and function as a way of coping with difficult thoughts and emotions, such as shame (Goss & Allan, 2009). Disordered eating behaviors that emerging adult women commonly endorse include restricting food intake, binge eating, and purging (Hahn et al., 2022; Jo et al., 2020, 2024; Masuda et al., 2012). In recent years, researchers have examined psychosocial factors that contribute to disordered eating behaviors in this age group (e.g., Fuller-Tyszkiewicz et al., 2022), including psychological distress (Liechty & Lee, 2013; Moore et al., 2014), difficulty in emotion regulation (Gratz & Roemer, 2004), and self-concealment (Larson & Chastain, 1990).
1.1. Psychological Distress and Disordered Eating Behaviors
The link between psychological distress and disordered eating behavior has been integrated into conceptual and applied models of disordered eating concerns for years (e.g., Striegel-Moore & Bulik, 2007). For example, psychological distress in response to difficult life events has been theorized as a major contributing factor for the development and maintenance of disordered eating behaviors within traditional and contemporary cognitive behavioral theories (see Fairburn et al., 2003; Haynos et al., 2016; Wilson et al., 2007). As noted earlier, emerging adulthood is a particularly vulnerable period during which women are at greater risk for disordered eating. Existing research with non-clinical samples of college women and men together (Jo & Yang, 2019; Masuda et al., 2012) and undergraduate college women (Moore et al., 2014) has reported positive associations between psychological distress and disordered eating behavior.
1.2. Difficulty in Emotion Regulation and Self-Concealment as Underlying Mechanisms
Cognitive and behavioral theories of disordered eating concerns emphasize the role of emotion regulation in the development and maintenance of disordered eating behaviors, especially in the context of greater psychological distress (Fairburn et al., 2003; Haynos et al., 2016). These theories postulate that the positive association between psychological distress and disordered eating behaviors is established in part through difficulty in emotion regulation (e.g., Evers et al., 2010). Difficulty in emotion regulation often refers to one’s inability to recognize or manage negative emotions and psychological distress (Gratz & Roemer, 2004) and may include the lack of acceptance of emotional responses, difficulty performing purposeful behavior, difficulty controlling impulses, limited access to strategies for effectively coping with emotions, and difficulty identifying and differentiating emotions (Ritschel et al., 2015). Difficulty in emotion regulation is a transdiagnostic process across a range of eating disorder symptoms and weight concerns (Brockmeyer et al., 2014; Gupta et al., 2008; Lafrance Robinson et al., 2014).
Self-concealment is another construct that reflects an underlying maladaptive regulation process in the context of disordered eating (Chung et al., 2021; Larson et al., 2015; Masuda et al., 2011; Masuda & Latzman, 2012). In applied psychology literature, self-concealment is a general and stable regulation tendency to keep distressing and potentially embarrassing personal information from others (Cramer & Barry, 1999; Larson & Chastain, 1990), and it involves the processes of (a) possessing a distressing personal secret, (b) keeping it from others, and (c) avoiding or feeling apprehensive about self-disclosure (Larson & Chastain, 1990). The process of self-concealment seems to be manifested in both intrapersonal and interpersonal contexts (Larson et al., 2015). Self-concealment is positively associated with both psychological distress (Mendoza et al., 2017, 2018) and disordered eating (Masuda et al., 2018b; Masuda & Latzman, 2012) in young adults (e.g., college women and men).
Finally, difficulty in emotion regulation and self-concealment are interrelated yet distinct processes implicated in disordered eating behavior (Mendoza et al., 2017, 2018). Difficulty in emotion regulation reflects an intrapersonal struggle to manage psychological distress (Gratz & Roemer, 2004), while self-concealment involves maladaptive, secretive regulation across intrapersonal and interpersonal contexts (Larson et al., 2015). Further research should explore how these constructs independently and jointly account for the relationship between psychological distress and disordered eating behavior in emerging adult women.
1.3. Present Study
In this cross-sectional study of emerging adult women, we first examined the positive association between psychological distress and disordered eating behavior. We then tested whether the positive association between psychological distress and disordered eating behavior was established indirectly through difficulty in emotion regulation, self-concealment, or both. We hypothesized that psychological distress would predict disordered eating behavior, and that this relationship would be at least partially explained by emotion regulation difficulties and self-concealment.
2. Method
2.1. Participants
Data were obtained through an online survey administered to 1402 undergraduate students enrolled at a four-year public university in Hawaiʻi, USA. To promote data integrity, the survey included four embedded attention-check items (e.g., “please select option 4 for this item”) distributed evenly throughout the questionnaire. The inclusion criteria were (a) participants who self-identified as women, (b) between 18 and 25 years of age, and (c) fluent in English. Participants presenting with psychotic symptoms were excluded from the study. Based on these parameters, 679 individuals were excluded, resulting in a final analytic sample of 723 women within the specified age range.
2.2. Procedure
This research was approved by the Institutional Review Board affiliated with the senior author’s university. Recruitment took place within psychology courses (e.g., Introduction to Psychology, Research Methods, Developmental Psychology, and Abnormal Psychology) between March 2018 and December 2020. Data collection was conducted through a secure online platform (Sona and Qualtrics), where participants completed the survey anonymously in exchange for course credit. Prior to participation, individuals received information outlining the study’s purpose and procedures and provided informed consent.
2.3. Measures
2.3.1. Demographic Form
A demographic questionnaire was used to capture variables central to the study, including participants’ age, self-identified gender, racial/ethnic background, and sexual identity, alongside other relevant demographic details. Age was treated as a continuous variable, while gender identity was categorized as “man,” “woman,” or “other.” Racial and ethnic identification was classified into nine groups: Native American, Latinx, Asian, Pacific Islander, White, Black, Hawaiian, Other, and Bi-racial/Multicultural (i.e., multiracial). Sexual identity was coded using four categories: heterosexual, homosexual, bisexual, and other.
2.3.2. Disordered Eating Behavior
The Eating Attitudes Test-26 Behavior Subscale (EAT-26-B; Garner et al., 1982; Masuda et al., 2012) comprises nine items drawn from the original EAT-26 instrument, each targeting behavioral components associated with disordered eating. These items reflect behavioral patterns, such as food restriction (e.g., “I avoid eating when I am hungry”), purging behaviors (e.g., “I vomit after I have eaten”), and episodes of binge eating (e.g., “I have gone on eating binges when I feel that I may not be able to stop”). Responses were rated using a 6-point Likert scale, where elevated scores denoted greater engagement in disordered eating behaviors. For the purposes of this study, the nine items were organized into three distinct factors using an item parceling technique (see below). Internal consistency, as measured by Cronbach’s alpha, was 0.82 for the present sample, and the maximal reliability estimate for the EAT-26-B reached 0.87.
2.3.3. Psychological Distress
The Depression Anxiety and Stress Scale, 21-item version (DASS-21; Henry & Crawford, 2005) is a self-administered measure designed to assess psychological distress across three domains: depression, anxiety, and stress. Comprising 21 items, the instrument employs a 4-point Likert scale (ranging from 0 to 3), with higher scores indicating increased levels of distress. Prior studies have supported its convergent and discriminant validity (Lee, 2019). In this investigation, analyses were conducted using the original three-factor structure. Internal consistency for the current sample was high, with a Cronbach’s alpha of 0.93 and a maximal reliability estimate of 0.91.
2.3.4. Difficulty in Emotion Regulation
The Difficulties in Emotion Regulation Scale (DERS; Gratz & Roemer, 2004) is a 36-item self-report instrument developed to assess deficits in emotion regulation. It comprises six theoretically derived subscales: (a) nonacceptance of emotional responses; (b) difficulties engaging in goal-directed behavior; (c) impulse control challenges; (d) lack of emotional awareness; (e) limited access to regulation strategies; and (f) lack of emotional clarity. Items are rated on a 5-point Likert scale ranging from 1 to 5, with elevated scores indicating greater difficulties in emotion regulation. Previous studies have demonstrated strong psychometric support for both the full scale and individual subscales (Gratz & Roemer, 2004). However, consistent with findings reported by Hallion et al. (2018), the current study excluded the Awareness subscale, citing evidence that its removal does not compromise internal consistency and may reflect its distinctiveness as a construct. In the present sample, the remaining five-factor structure yielded a Cronbach’s alpha of 0.92 and a maximal reliability estimate of 0.91.
2.3.5. Self-Concealment
The Self-Concealment Scale (SCS; Larson & Chastain, 1990) is a 10-item self-report measure designed to assess the extent to which individuals habitually withhold personally distressing information. Each item is rated on a 5-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree), with higher scores indicating greater levels of self-concealment. Previous research has demonstrated sound psychometric properties for the scale (Masuda et al., 2018a). Although originally conceptualized as a unidimensional measure, the present study employed an item parceling strategy to group the 10 items into three parcels for analytical purposes. Internal consistency was high, with a Cronbach’s alpha of 0.91 and a maximal reliability coefficient of 0.92.
2.4. Data Analyses
All statistical procedures were conducted using R software, version 4.1.2 (R Core Team, 2013). Descriptive statistics and Pearson correlation coefficients were computed to summarize and explore relationships among study variables. To assess normality assumptions, the absolute values of skewness and kurtosis were evaluated, with thresholds of 2 and 7, respectively, in accordance with guidelines by West et al. (1995).
Subsequently, following the two-step methodology outlined by Anderson and Gerbing (1988), both the measurement and structural models were evaluated sequentially. Model fit was assessed using three widely accepted indices: the root mean square error of approximation (RMSEA), the comparative fit index (CFI), and the Tucker–Lewis index (TLI). Consistent with established benchmarks, model fit was deemed adequate when RMSEA values were below 0.08 (Browne & Cudeck, 1992), and both CFI (Bentler, 1990) and TLI (Bentler & Bonett, 1980) exceeded 0.90. After confirming a satisfactory fit for both models, path coefficients and overall model fit were compared between full and partial mediation models. A competing model strategy was employed, as previous literature has limited evidence to support whether the relationship between psychological distress and disordered eating behaviors was partially or fully mediated by difficulty in emotion regulation and self-concealment. By setting the partially mediated model as the research model and the fully mediated model as the competitive model, an attempt was made to search for a more accurate and parsimonious model. Structural Equation Modeling (SEM) analyses were conducted using the lavaan package in R (Rosseel, 2012).
To test the study’s hypotheses, bootstrapping procedures were employed to evaluate the statistical significance of indirect effects. This approach involved generating 5000 resampled datasets through random sampling with replacement from the original data. Indirect effects were considered statistically significant at the 0.05 level when the 95% confidence interval did not include zero (Bollen & Stine, 1992).
As outlined earlier, item parceling was applied to the EAT-26-B and SCS scales, consistent with practices in SEM (Matsunaga, 2008). This technique involves aggregating item scores, either by summation or averaging, to reduce the total number of measured variables and enhance model fit. Although parceling introduces potential bias, such effects are generally minimal and can be statistically adjusted. In alignment with the balancing approach proposed by Little et al. (2013), items were grouped based on factor loading magnitudes to ensure relative equivalence within each parcel. To assess reliability, both composite reliability (e.g., Cronbach’s alpha) and maximal reliability (Coefficient H; Raykov et al., 2016) were calculated. Maximal reliability was included given its capacity to more accurately reflect the reliability of latent constructs as measured by their indicators. A threshold of 0.70 or greater is generally considered acceptable for maximal reliability estimates in empirical research. These calculations were conducted using the semPlot package in R (Epskamp, 2015).
3. Results
3.1. Demographics
As summarized in Table 1, the mean age of the retained sample was 19.5 years (SD = 1.6). The cohort was demographically diverse: 34.9% identified as Asian; 26.7% as Non-Hispanic White; 23.9% as Multiracial; 6.6% as Latinx; 3.5% as Hawaiian; 1.8% as Pacific Islander; 1.4% as Non-Hispanic Black; 0.6% as Other; and 0.5% as Native American. The racial and ethnic distribution of the final sample closely mirrored that of the broader student population at the host institution.

Table 1.
Demographic background.
3.2. Measurement Model
Descriptive statistics, including means, standard deviations, skewness, kurtosis, and inter-variable correlations, were computed for all study variables and are presented in Table 2. The assumption of normality was met for all variables, as the observed skewness and kurtosis values fell within acceptable thresholds.

Table 2.
Means, standard deviation, and correlations of study variables.
Prior to proceeding with structural model evaluation, a measurement model was evaluated for psychological distress, disordered eating behavior, difficulty in emotion regulation, and self-concealment. As shown in Table 3, the measurement model demonstrated a satisfactory fit to the data (χ2 = 232.263; df = 71; TLI = 0.968; CFI = 0.975; RMSEA = 0.056). The standardized factor loadings for the indicators were statistically significant at the 0.001 level and ranged from 0.83 to 0.92 for psychological distress, 0.67 to 0.91 for disordered eating behavior, 0.56 to 0.92 for emotion regulation difficulties, and 0.88 to 0.90 for self-concealment.

Table 3.
Confirmatory factor analysis of research model.
3.3. Structural Model
Since the above-mentioned measurement model adequately explained the latent variable, the structural model that explained the relationship between latent factors was examined. The result indicated that both partially mediated model (χ2 = 318.669; df = 111; TLI = 0.956; CFI = 0.968; RMSEA = 0.051) and fully mediated model (χ2 = 323.012; df = 112; TLI = 0.956; CFI = 0.967; RMSEA = 0.051) were good fit to the data. The chi-square difference test was employed to compare the model fit of two models, and a significant difference was identified (Δχ2 = 4.343; Δdf = 1; p < 0.05). If the chi-square difference is significant, the larger model with more freely estimated parameters fits the data better than the smaller model in which the parameters in question are fixed. Therefore, as shown in Figure 1, a partially mediated model was adopted as the final model.
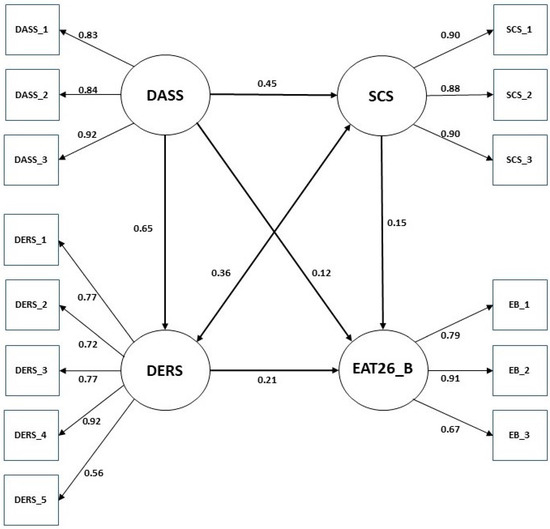
Figure 1.
Partial mediation model between psychological distress and disordered eating behavior. Note: EAT26-B, the Eating Attitudes Test-26-Behavior Subscale; DASS, the Depression, Anxiety, and Stress Scale; DERS, the Difficulties in Emotion Regulation Scale; SCS, the Self Concealment Scale.
3.4. Significance Test of Indirect Effects
A bootstrap procedure was performed to examine whether the indirect effect of psychological distress on disordered eating behavior via difficulty in emotion regulation and self-concealment was significant in the final model. We found the indirect effect of psychological distress on disordered eating behaviors through difficulty in emotion regulation and self-concealment (Table 4). The direct effect of psychological distress on disordered eating behaviors was also significant (β = 0.12, p = 0.05), which confirmed that the difficulty in emotion regulation and self-concealment partially mediates the effect of psychological distress. The direct effects of psychological distress on difficulty in emotion regulation and self-concealment were β = 0.65 (p < 0.01) and β = 0.45 (p < 0.01), respectively. The direct effect of difficulty in emotion regulation (β = 0.21, p < 0.01) and self-concealment (β = 0.15, p < 0.01) on disordered eating behaviors was also significant. The indirect effect between psychological distress and disordered eating behavior via difficulty in emotion regulation was β = 0.14 (p < 0.01), and the indirect effect via self-concealment was β = 0.07 (p < 0.01).

Table 4.
Parameter estimate of partial mediation model.
4. Discussion
Emerging adulthood is often marked by exposure to numerous life stressors (Arnett et al., 2014), which may heighten vulnerability to disordered eating behaviors (e.g., Masuda et al., 2018a; Potterton et al., 2020; Simone et al., 2022), and eating disorders continue to be more prevalent in women than men (Marie et al., 2019). This cross-sectional study investigated the relationship between psychological distress and disordered eating behaviors in a sample of emerging adult women, as well as the extent to which difficulty in emotion regulation and self-concealment mediated this association. Consistent with the study’s hypotheses, psychological distress was significantly correlated with disordered eating behavior. Further, both difficulty in emotion regulation and self-concealment were found to partially mediate the association between psychological distress and disordered eating behavior, suggesting their contributory roles in this linkage.
Conceptually, our results indicate that difficulty in emotion regulation and self-concealment function as interconnected yet distinct pathways that underlie the link between psychological distress and disordered eating behavior. These findings add to the growing research emphasizing the covert and maladaptive nature of disordered eating patterns (e.g., Goss & Allan, 2009; Masuda et al., 2011; Masuda & Latzman, 2012). More specifically, the present study demonstrated that psychological distress was positively associated with disordered eating in emerging adult women, and this relationship was indirectly accounted for by both impaired emotion regulation and tendencies toward self-concealment. Clinically, there is a pressing need to improve treatment outcomes for eating disorders, as current response rates remain modest; approximately 50% for binge eating disorder (Hilbert, 2023) and 40–45% for bulimia nervosa (Monteleone et al., 2022). Our findings indicate that interventions targeting both emotion regulation difficulties and self-concealment may offer particular benefit for women in this age group.
Importantly, the present findings also indicate that the association between psychological distress and disordered eating behavior is not fully explained by difficulty in emotion regulation or self-concealment. This suggests the involvement of additional psychosocial factors, particularly among emerging adult women and potentially across other demographic groups. Such alternative contributing factors may include perfectionism, social anxiety, self-esteem challenges, and developmental stressors uniquely characteristic of emerging adulthood (Fuller-Tyszkiewicz et al., 2022; McCabe et al., 2019). Continued research in this domain holds meaningful clinical and theoretical relevance, offering potential avenues for refining interventions and prevention strategies aimed at disordered eating in this developmental group of women.
Furthermore, although it falls outside the scope of the current study, it is important to acknowledge the bidirectional nature of the association between psychological distress and disordered eating behavior. Disordered eating behaviors have been shown to intensify psychological distress over time, leading to heightened symptoms of anxiety, depression, and emotional dysregulation (Blinder et al., 2006; Patrick et al., 2011). This reciprocal dynamic suggests that disordered eating not only stems from psychological challenges but may also perpetuate them.
5. Limitations
Several limitations of the present study should be acknowledged. First, the sample consisted exclusively of emerging adult women enrolled at a public university in Hawaiʻi, which may constrain the generalizability of findings to other cultural and geographic contexts. Nonetheless, a notable strength of the study is the racial and ethnic diversity represented within the sample. Second, the findings are inherently tied to the specific instruments utilized (Haynes et al., 2018), and alternative measures of psychological distress, disordered eating behavior, difficulty in emotion regulation, and self-concealment may yield different outcomes. Nevertheless, the selected instruments are widely recognized and frequently employed within psychological research. Additionally, by applying SEM, the study examined associations at the latent construct level, offering deeper insight into the underlying mechanisms. Third, given that this study employed a cross-sectional design, it was not possible to investigate the temporal or causal dynamics among key variables as proposed in the conceptual mediation framework. To clarify the roles of difficulty in emotion regulation and self-concealment within the interplay of psychological distress and disordered eating behavior, future investigations should adopt longitudinal methodologies or intervention-based approaches. Finally, a portion of the sample was collected after the onset of the COVID-19 pandemic. Considering the well-documented effects of the pandemic on psychological distress and eating behaviors (e.g., Chan & Chiu, 2022; Ramalho et al., 2022), additional research is warranted to assess the generalizability of these findings.
6. Conclusions
The present investigation contributes meaningfully to the growing body of literature on disordered eating behaviors among emerging adult women and highlights important pathways linking psychological distress to disordered eating behaviors. By identifying difficulty in emotion regulation and self-concealment as partial mediators, the study offers insight into the psychological processes that may underlie maladaptive eating patterns in this population. These findings not only extend theoretical understanding but also underscore potential targets for prevention and clinical intervention efforts tailored to emerging adults.
Author Contributions
D.J. conducted literature review, discussed study questions with A.M. (senior author), conducted statistical analyses, drafted and revised the manuscript. M.L.H. conducted literature review and assisted in manuscript preparation (i.e., writing the first and subsequent drafts). A.M. supervised D.J. in study design and research questions and assisted in manuscript preparation (i.e., writing the first and subsequent drafts). All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board at University of Hawaiʻi (protocol code 2017-00421/2018-00244 and 27 November 2017).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Anderson, J. C., & Gerbing, D. W. (1988). Structural equation modeling in practice: A review and recommended two-step approach. Psychological Bulletin, 103(3), 411. [Google Scholar] [CrossRef]
- Arnett, J. J. (2007). Emerging adulthood: What is it, and what is it good for? Child Development Perspectives, 1(2), 68–73. [Google Scholar] [CrossRef]
- Arnett, J. J., Žukauskienė, R., & Sugimura, K. (2014). The new life stage of emerging adulthood at ages 18–29 years: Implications for mental health. The Lancet Psychiatry, 1(7), 569–576. [Google Scholar] [CrossRef]
- Bentler, P. M. (1990). Comparative fit indexes in structural models. Psychological Bulletin, 107(2), 238–246. [Google Scholar] [CrossRef] [PubMed]
- Bentler, P. M., & Bonett, D. G. (1980). Significance tests and goodness of fit in the analysis of covariance structures. Psychological Bulletin, 88(3), 588. [Google Scholar] [CrossRef]
- Blinder, B. J., Cumella, E. J., & Sanathara, V. A. (2006). Psychiatric comorbidities of female inpatients with eating disorders. Psychosomatic Medicine, 68(3), 454–462. [Google Scholar] [CrossRef]
- Bollen, K. A., & Stine, R. A. (1992). Bootstrapping goodness-of-fit measures in structural equation models. Sociological Methods & Research, 21(2), 205–229. [Google Scholar]
- Brockmeyer, T., Skunde, M., Wu, M., Bresslein, E., Rudofsky, G., Herzog, W., & Friederich, H.-C. (2014). Difficulties in emotion regulation across the spectrum of eating disorders. Comprehensive Psychiatry, 55(3), 565–571. [Google Scholar] [CrossRef]
- Browne, M. W., & Cudeck, R. (1992). Alternative ways of assessing model fit. Sociological Methods & Research, 21(2), 230–258. [Google Scholar] [CrossRef]
- Chan, C. Y., & Chiu, C. Y. (2022). Disordered eating behaviors and psychological health during the COVID-19 pandemic. Psychology, Health & Medicine, 27(1), 249–256. [Google Scholar]
- Chung, M. C., Ye, Z., Wang, N., & Thomas, J. (2021). Linking posttraumatic stress disorder with eating disorders among Emirati university female students: The role of self-concealment. Current Psychology, 41, 8975–8984. [Google Scholar] [CrossRef]
- Cramer, K. M., & Barry, J. E. (1999). Psychometric properties and confirmatory factor analysis of the self-concealment scale. Personality and Individual Differences, 27(4), 629–637. [Google Scholar] [CrossRef]
- Epskamp, S. (2015). semPlot: Unified visualizations of structural equation models. Structural Equation Modeling: A Multidisciplinary Journal, 22(3), 474–483. [Google Scholar]
- Evers, C., Marijn Stok, F., & de Ridder, D. T. D. (2010). Feeding your feelings: Emotion regulation strategies and emotional eating. Personality and Social Psychology Bulletin, 36(6), 792–804. [Google Scholar] [CrossRef]
- Fairburn, C. G., Cooper, Z., & Shafran, R. (2003). Cognitive behaviour therapy for eating disorders: A ‘transdiagnostic’ theory and treatment. Behaviour Research and Therapy, 41(5), 509–528. [Google Scholar] [CrossRef] [PubMed]
- Fuller-Tyszkiewicz, M., Rodgers, R. F., Maïano, C., Mellor, D., Sicilia, A., Markey, C. H., Aimé, A., Dion, J., Pietrabissa, G., Lo Coco, G., Caltabiano, M. L., Strodl, E., Alcaraz-Ibánez, M., Bégin, C., Blackburn, M.-È., Castelnuovo, G., Granero-Gallegos, A., Gullo, S., Hayami-Chisuwa, N., … McCabe, M. (2022). Testing of a model for risk factors for eating disorders and higher weight among emerging adults: Baseline evaluation. Body Image, 40, 322–339. [Google Scholar] [CrossRef] [PubMed]
- Garner, D. M., Olmsted, M. P., Bohr, Y., & Garfinkel, P. E. (1982). The eating attitudes test: Psychometric features and clinical correlates. Psychological Medicine: A Journal of Research in Psychiatry and the Allied Sciences, 12(4), 871–878. [Google Scholar] [CrossRef]
- Goss, K., & Allan, S. (2009). Shame, pride and eating disorders. Clinical Psychology & Psychotherapy, 16(4), 303–316. [Google Scholar] [CrossRef] [PubMed]
- Gratz, K. L., & Roemer, L. (2004). Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment, 26(1), 41–54. [Google Scholar] [CrossRef]
- Gupta, S., Zachary Rosenthal, M., Mancini, A. D., Cheavens, J. S., & Lynch, T. R. (2008). Emotion regulation skills mediate the effects of shame on eating disorder symptoms in women. Eating Disorders, 16(5), 405–417. [Google Scholar] [CrossRef]
- Hahn, S. L., Hazzard, V. M., Loth, K. A., Larson, N., Klein, L., & Neumark-Sztainer, D. (2022). Using apps to self-monitor diet and physical activity is linked to greater use of disordered eating behaviors among emerging adults. Preventive Medicine, 155, 106967. [Google Scholar] [CrossRef]
- Hallion, L. S., Steinman, S. A., Tolin, D. F., & Diefenbach, G. J. (2018). Psychometric properties of the difficulties in emotion regulation scale (DERS) and its short forms in adults with emotional disorders. Frontiers in Psychology, 9, 539. [Google Scholar] [CrossRef]
- Haynes, S. N., Kaholokula, J. K. A., & Tanaka-Matsumi, J. (2018). Psychometric foundations of psychological assessment with diverse cultures: What are the concepts, methods, and evidence? In Cultural competence in applied psychology (pp. 441–472). Springer. [Google Scholar]
- Haynos, A. F., Forman, E. M., Butryn, M. L., & Lillis, J. (2016). Mindfulness and acceptance in for treating eating disorders and weight concerns: Evidence-based interventions. Context Press/New Harbinger Publications. [Google Scholar]
- Henry, J. D., & Crawford, J. R. (2005). The short-form version of the depression anxiety stress scales (DASS-21): Construct validity and normative data in a large non-clinical sample. British Journal of Clinical Psychology, 44(2), 227–239. [Google Scholar] [CrossRef] [PubMed]
- Hilbert, A. (2023). Psychological and medical treatments for binge-eating disorder: A research update. Physiology & Behavior, 269, 114267. [Google Scholar] [CrossRef] [PubMed]
- Jo, D., Goh, P. K., Lin, S. L., Spencer, S. D., & Masuda, A. (2024). Bridging eating disorder symptoms and psychological flexibility and inflexibility in racially diverse emerging adult women: A network analysis. Journal of Contextual Behavioral Science, 32, 100766. [Google Scholar] [CrossRef]
- Jo, D., Spencer, S. D., & Masuda, A. (2020). Mindfulness attenuates the positive association between disordered eating cognition and disordered eating behavior in a sample of college women. Current Psychology, 41, 4536–4544. [Google Scholar] [CrossRef]
- Jo, D., & Yang, E. (2019). The role of present moment awareness and cognitive fusion with food craving in the relationship between depression and binge eating. Journal of Contextual Behavioral Science, 13, 126–133. [Google Scholar] [CrossRef]
- Lafrance Robinson, A., Kosmerly, S., Mansfield-Green, S., & Lafrance, G. (2014). Disordered eating behaviours in an undergraduate sample: Associations among gender, body mass index, and difficulties in emotion regulation. Canadian Journal of Behavioural Science/Revue Canadienne Des Sciences Du Comportement, 46(3), 320–326. [Google Scholar] [CrossRef]
- Larson, D. G., & Chastain, R. L. (1990). Self-concealment: Conceptualization, measurement, and health implications. Journal of Social and Clinical Psychology, 9(4), 439–455. [Google Scholar] [CrossRef]
- Larson, D. G., Chastain, R. L., Hoyt, W. T., & Ayzenberg, R. (2015). Self-concealment: Integrative review and working model. Journal of Social and Clinical Psychology, 34(8), 705–729. [Google Scholar] [CrossRef]
- Lee, D. (2019). The convergent, discriminant, and nomological validity of the depression anxiety stress scales-21 (DASS-21). Journal of Affective Disorders, 259, 136–142. [Google Scholar] [CrossRef]
- Liechty, J. M., & Lee, M.-J. (2013). Longitudinal predictors of dieting and disordered eating among young adults in the U.S. International Journal of Eating Disorders, 46(8), 790–800. [Google Scholar] [CrossRef]
- Little, T. D., Rhemtulla, M., Gibson, K., & Schoemann, A. M. (2013). Why the items versus parcels controversy needn’t be one. Psychological Methods, 18(3), 285. [Google Scholar] [CrossRef]
- Marie, G., Pierre, D., Gregory, L., & Pierre, T. M. (2019). Prevalence of eating disorders over the 2000–2018 period: A systematic literature review. The American Journal of Clinical Nutrition, 109(5), 1402–1413. [Google Scholar] [CrossRef]
- Masuda, A., Boone, M. S., & Timko, C. A. (2011). The role of psychological flexibility in the relationship between self-concealment and disordered eating symptoms. Eating Behaviors, 12(2), 131–135. [Google Scholar] [CrossRef]
- Masuda, A., Latner, J. D., Barlie, J. P., & Sargent, K. (2018a). Understanding self-concealment within a framework of eating disorder cognitions and body image flexibility: Conceptual and applied implications. Eating Behaviors, 30, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Masuda, A., & Latzman, R. D. (2012). Psychological flexibility and self-concealment as predictors of disordered eating symptoms. Journal of Contextual Behavioral Science, 1(1–2), 49–54. [Google Scholar] [CrossRef]
- Masuda, A., Marshall, R. D., & Latner, J. D. (2018b). Mindfulness as a moderator of the association between eating disorder cognition and eating disorder behavior among a non-clinical sample of female college students: A role of ethnicity. Frontiers in Psychology, 9, 700. [Google Scholar] [CrossRef] [PubMed]
- Masuda, A., Price, M., & Latzman, R. D. (2012). Mindfulness moderates the relationship between disordered eating cognitions and disordered eating behaviors in a non-clinical college sample. Journal of Psychopathology and Behavioral Assessment, 34(1), 107–115. [Google Scholar] [CrossRef] [PubMed]
- Matsunaga, M. (2008). Item parceling in structural equation modeling: A primer. Communication Methods and Measures, 2(4), 260–293. [Google Scholar] [CrossRef]
- McCabe, M., Tatangelo, G., Watson, B., Fuller-Tyszkiewicz, M., Rodgers, R. F., Aimé, A., Mellor, D., Granero-Gallegos, A., Strodl, E., Caltabiano, M., Camacho, A. S., Castelnuovo, G., Coco, G. L., Grogan, S., Probst, M., Dion, J., Maïano, C., Manzoni, G., Begin, C., … Ricciardelli, L. (2019). Development and testing of a model for risk and protective factors for eating disorders and higher weight among emerging adults: A study protocol. Body Image, 31, 139–149. [Google Scholar] [CrossRef]
- Mendoza, H., Goodnight, B. L., Caporino, N. E., & Masuda, A. (2017). Psychological distress among Latina/o college students: The roles of self-concealment and psychological inflexibility. Current Psychology. Advance online publication. [Google Scholar] [CrossRef]
- Mendoza, H., Tully, E. C., Goodnight, B., Gray, J., & Masuda, A. (2018). The indirect effect of self-concealment on distress through psychological inflexibility in Asian American, black American, and white American college students. Personality and Individual Differences, 126, 93–98. [Google Scholar] [CrossRef]
- Monteleone, A. M., Pellegrino, F., Croatto, G., Carfagno, M., Hilbert, A., Treasure, J., Wade, T., Bulik, C. M., Zipfel, S., Hay, P., Schmidt, U., Castellini, G., Favaro, A., Fernandez-Aranda, F., Shin, J. I., Voderholzer, U., Ricca, V., Moretti, D., Busatta, D., … Solmi, M. (2022). Treatment of eating disorders: A systematic meta-review of meta-analyses and network meta-analyses. Neuroscience & Biobehavioral Reviews, 142, 104857. [Google Scholar] [CrossRef]
- Moore, M., Masuda, A., Hill, M. L., & Goodnight, B. L. (2014). Body image flexibility moderates the association between disordered eating cognition and disordered eating behavior in a non-clinical sample of women: A cross-sectional investigation. Eating Behaviors, 15(4), 664–669. [Google Scholar] [CrossRef] [PubMed]
- Patrick, J. H., Stahl, S. T., & Sundaram, M. (2011). Disordered eating and psychological distress among adults. The International Journal of Aging and Human Development, 73(3), 209–226. [Google Scholar] [CrossRef]
- Potterton, R., Richards, K., Allen, K., & Schmidt, U. (2020). Eating disorders during emerging adulthood: A systematic scoping review. Frontiers in Psychology, 10, 3062. [Google Scholar] [CrossRef] [PubMed]
- Ramalho, S. M., Trovisqueira, A., de Lourdes, M., Gonçalves, S., Ribeiro, I., Vaz, A. R., Machado, P. P. P., & Conceição, E. (2022). The impact of COVID-19 lockdown on disordered eating behaviors: The mediation role of psychological distress. Eating and Weight Disorders-Studies on Anorexia, Bulimia and Obesity, 27(1), 179–188. [Google Scholar] [CrossRef] [PubMed]
- Raykov, T., Gabler, S., & Dimitrov, D. M. (2016). Maximal reliability and composite reliability: Examining their difference for multicomponent measuring instruments using latent variable modeling. Structural Equation Modeling: A Multidisciplinary Journal, 23(3), 384–391. [Google Scholar] [CrossRef]
- R Core Team. (2013). R: A language and environment for statistical computing. Foundation for Statistical Computing. [Google Scholar]
- Ritschel, L. A., Tone, E. B., Schoemann, A. M., & Lim, N. E. (2015). Psychometric properties of the difficulties in emotion regulation scale across demographic groups. Psychological Assessment, 27(3), 944–954. [Google Scholar] [CrossRef]
- Rosseel, Y. (2012). lavaan: An R package for structural equation modeling. Journal of Statistical Software, 48, 1–36. [Google Scholar] [CrossRef]
- Simone, M., Telke, S., Anderson, L. M., Eisenberg, M., & Neumark-Sztainer, D. (2022). Ethnic/racial and gender differences in disordered eating behavior prevalence trajectories among women and men from adolescence into adulthood. Social Science & Medicine, 294, 114720. [Google Scholar] [CrossRef] [PubMed]
- Striegel-Moore, R. H., & Bulik, C. M. (2007). Risk factors for eating disorders. American Psychologist, 62(3), 181–198. [Google Scholar] [CrossRef] [PubMed]
- West, S. G., Finch, J. F., & Curran, P. J. (1995). Structural equation models with nonnormal variables: Problems and remedies. In R. H. Hoyle (Ed.), Structural equation modeling: Concepts, issues, and applications (pp. 56–75). Thousand Oaks. [Google Scholar]
- Wilson, G. T., Grilo, C. M., & Vitousek, K. M. (2007). Psychological treatment of eating disorders. American Psychologist, 62(3), 199–216. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).