Roots and Shoots: A Pilot Parallel Randomised Controlled Trial Assessing the Feasibility and Acceptability of a Nature-Based Self-Help Intervention for Low Wellbeing
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Sample Size
2.2. Procedure
2.3. Trial Arms
2.3.1. Nature-Based Intervention: Roots and Shoots
2.3.2. Waitlist Control
2.4. Acceptability and Feasibility
2.5. Outcome Measures
2.5.1. The Short Warwick–Edinburgh Mental Wellbeing Scale (SWEMWBS)
2.5.2. Generalised Anxiety Disorder (GAD7)
2.5.3. Patient Health Questionnaire (PHQ8)
2.5.4. Perceived Stress Scale (PSS4)
2.5.5. Ruminative Response Scale (RSS)
2.5.6. Jenkins Sleep Scale (JSS)
2.5.7. Five Facet Mindfulness Questionnaire (FFMQ-15)
2.5.8. Nature Relatedness Scale (NR-6)
2.6. Statistical Analysis
3. Results
3.1. Characteristics of the Participants
3.2. Acceptability and Feasibility
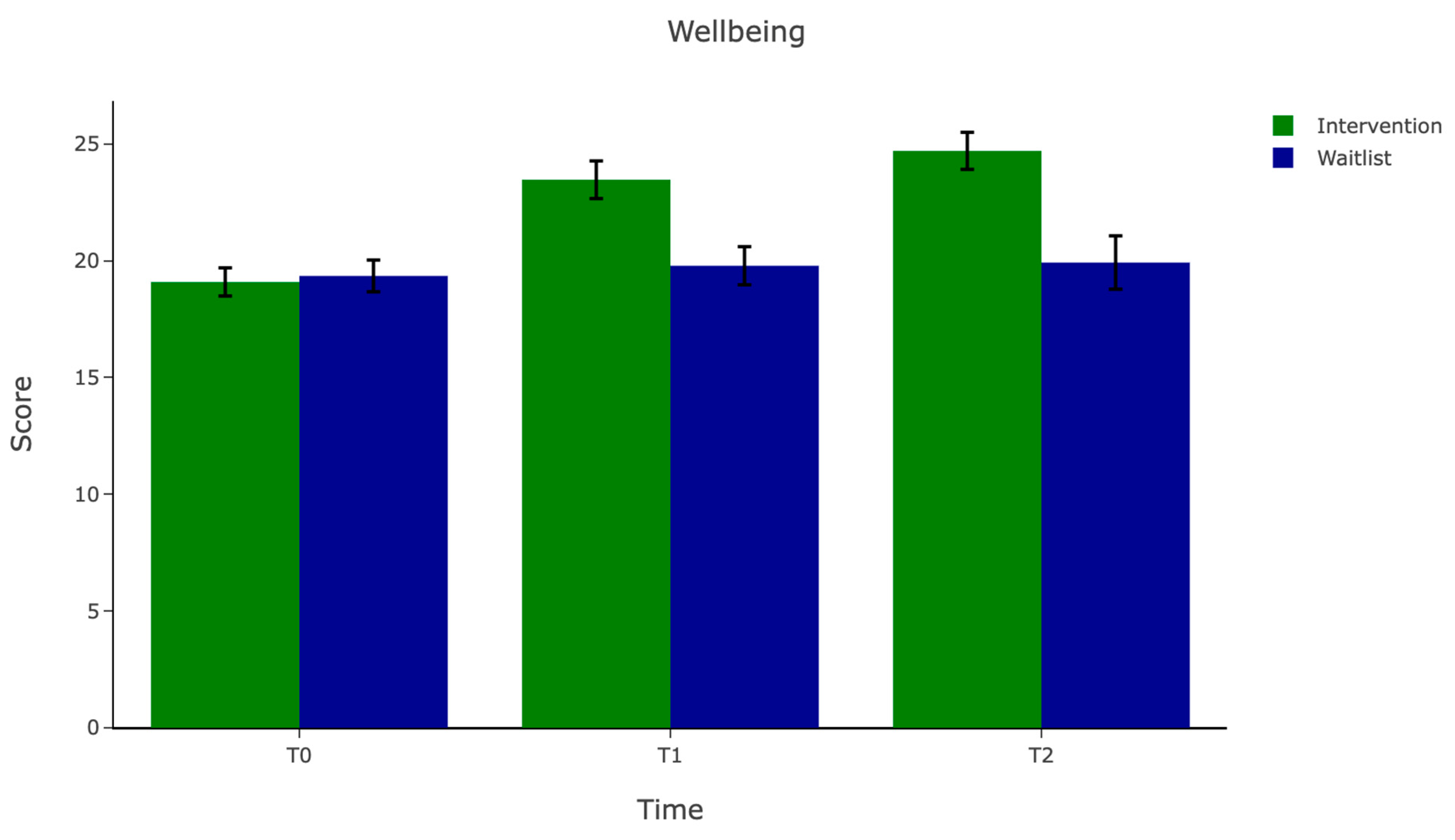
3.3. Quantitative Outcomes
3.4. Preliminary Efficacy on the Primary Outcome
3.5. Reliable Change and Clinically Significant Change
4. Discussion
Clinical Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| NBI | Nature-Based Intervention |
| RCT | Randomised Controlled Trial |
| CSC | Clinically Significant Change |
References
- Ambrey, C. L., & Cartlidge, N. (2017). Do the psychological benefits of greenspace depend on one’s personality? Personality and Individual Differences, 116, 233–239. [Google Scholar] [CrossRef]
- Antonelli, M., Donelli, D., Carlone, L., Maggini, V., Firenzuoli, F., & Bedeschi, E. (2022). Effects of forest bathing (shinrin-yoku) on individual well-being: An umbrella review. International Journal of Environmental Health Research, 32(8), 1842–1867. [Google Scholar] [CrossRef]
- Baer, R., Gu, J., & Strauss, C. (2022). Five facet mindfulness questionnaire (FFMQ). In Handbook of assessment in mindfulness research (pp. 1–23). Springer. [Google Scholar] [CrossRef]
- Bass, M., Dawkin, M., Muncer, S., Vigurs, S., & Bostock, J. (2016). Validation of Warwick-Edinburgh Mental Well-being Scale (WEMWBS) in a population of people using Secondary Care Mental Health Services. Journal of Mental Health, 25(4), 323–329. [Google Scholar] [CrossRef]
- Bot, M., Brouwer, I. A., Roca, M., Kohls, E., Penninx, B. W. J. H., Watkins, E., Van Grootheest, G., Cabout, M., Hegerl, U., Gili, M., Owens, M., & Visser, M. (2019). Effect of multinutrient supplementation and food-related behavioral activation therapy on prevention of major depressive disorder among overweight or obese adults with subsyndromal depressive symptoms: The MooDFOOD randomized clinical trial. JAMA—Journal of the American Medical Association, 321(9), 858–868. [Google Scholar] [CrossRef] [PubMed]
- Bowen, D. J., Kreuter, M., Spring, B., Cofta-Woerpel, L., Linnan, L., Weiner, D., Bakken, S., Kaplan, C. P., Squiers, L., Fabrizio, C., & Fernandez, M. (2009). How we design feasibility studies. American Journal of Preventive Medicine, 36(5), 452–457. [Google Scholar] [CrossRef] [PubMed]
- Bowler, D. E., Buyung-Ali, L. M., Knight, T. M., & Pullin, A. S. (2010). A systematic review of evidence for the added benefits to health of exposure to natural environments. BMC Public Health, 10, 456. [Google Scholar] [CrossRef] [PubMed]
- Bratman, G. N., Anderson, C. B., Berman, M. G., Cochran, B., de Vries, S., Flanders, J., Folke, C., Frumkin, H., Gross, J. J., Hartig, T., Kahn, P. H., Kuo, M., Lawler, J. J., Levin, P. S., Lindahl, T., Meyer-Lindenberg, A., Mitchell, R., Ouyang, Z., Roe, J., … Daily, G. C. (2019). Nature and mental health: An ecosystem service perspective. Science Advances, 5(7), 903–927. [Google Scholar] [CrossRef]
- Bratman, G. N., Olvera-Alvarez, H. A., & Gross, J. J. (2021). The affective benefits of nature exposure. Social and Personality Psychology Compass, 15(8), e12630. [Google Scholar] [CrossRef]
- Browning, M. H. E. M., Shipley, N., McAnirlin, O., Becker, D., Yu, C. P., Hartig, T., & Dzhambov, A. M. (2020). An actual natural setting improves mood better than its virtual counterpart: A meta-analysis of experimental data. Frontiers in Psychology, 11, 2200. [Google Scholar] [CrossRef]
- Budd, M., Iqbal, A., Harding, C., Rees, E., & Bhutani, G. (2021). Mental health promotion and prevention in primary care: What should we be doing vs. what are we actually doing? Mental Health & Prevention, 21, 200195. [Google Scholar] [CrossRef]
- Bunce, H. L. I., & Owens, M. (2025). A generational relational model of nature and mental wellbeing: Results of a qualitative analysis. Frontiers in Psychology, 16, 1469507. [Google Scholar] [CrossRef]
- Burger, T., Potgieter, J. C., & Nell, W. (2024). Methods and Environmental conditions typical of nature-based mindfulness practice: A scoping review. Mindfulness, 15(7), 1621–1637. [Google Scholar] [CrossRef]
- Carr, A., Cullen, K., Keeney, C., Canning, C., Mooney, O., Chinseallaigh, E., & O’Dowd, A. (2021). Effectiveness of positive psychology interventions: A systematic review and meta-analysis. Journal of Positive Psychology, 16(6), 749–769. [Google Scholar] [CrossRef]
- Charisi, V., Zafeiroudi, A., Trigonis, I., Tsartsapakis, I., & Kouthouris, C. (2025). The impact of green spaces on workplace creativity: A systematic review of nature-based activities and employee well-being. Sustainability, 17(2), 390. [Google Scholar] [CrossRef]
- Choe, E. Y., Jorgensen, A., & Sheffield, D. (2020). Does a natural environment enhance the effectiveness of Mindfulness-Based Stress Reduction (MBSR)? Examining the mental health and wellbeing, and nature connectedness benefits. Landscape and Urban Planning, 202, 103886. [Google Scholar] [CrossRef]
- Colding, J., Gren, Å., & Barthel, S. (2020). The incremental demise of urban green spaces. Land, 9(5), 162. [Google Scholar] [CrossRef]
- Coles, R. W., & Bussey, S. C. (2000). Urban forest landscapes in the UK—Progressing the social agenda. Landscape and Urban Planning, 52(2–3), 181–188. [Google Scholar] [CrossRef]
- Cooper, A. A., & Conklin, L. R. (2015). Dropout from individual psychotherapy for major depression: A meta-analysis of randomized clinical trials. Clinical Psychology Review, 40, 57–65. [Google Scholar] [CrossRef]
- Coventry, P. A., Brown, J. V. E., Pervin, J., Brabyn, S., Pateman, R., Breedvelt, J., Gilbody, S., Stancliffe, R., McEachan, R., & White, P. C. L. (2021). Nature-based outdoor activities for mental and physical health: Systematic review and meta-analysis. SSM-Population Health, 16, 100934. [Google Scholar] [CrossRef]
- Craig, P., Dieppe, P., Macintyre, S., Michie, S., Nazareth, I., & Petticrew, M. (2013). Developing and evaluating complex interventions: The new Medical Research Council guidance. International Journal of Nursing Studies, 50(5), 587–592. [Google Scholar] [CrossRef]
- Craske, M. G., Dunn, B. D., Meuret, A. E., Rizvi, S. J., & Taylor, C. T. (2024). Positive affect and reward processing in the treatment of depression, anxiety and trauma. Nature Reviews Psychology, 3(10), 665–685. [Google Scholar] [CrossRef]
- Cuthbert, S., Kellas, A., & Page, L. A. (2021). Green care in psychiatry. The British Journal of Psychiatry, 218(2), 73–74. [Google Scholar] [CrossRef]
- Djernis, D., Lerstrup, I., Poulsen, D., Stigsdotter, U., Dahlgaard, J., & O’Toole, M. (2019). A Systematic review and meta-analysis of nature-based mindfulness: Effects of moving mindfulness training into an outdoor natural setting. International Journal of Environmental Research and Public Health, 16(17), 3202. [Google Scholar] [CrossRef] [PubMed]
- Ebert, D. D., & Cuijpers, P. (2018). It is time to invest in the prevention of depression. JAMA Network Open, 1(2), e180335. [Google Scholar] [CrossRef] [PubMed]
- Ekman, R., Fletcher, A., Giota, J., Eriksson, A., Thomas, B., & Bååthe, F. (2022). A flourishing brain in the 21st century: A scoping review of the impact of developing good habits for mind, brain, well-being, and learning. Mind, Brain, and Education, 16(1), 13–23. [Google Scholar] [CrossRef]
- Engemann, K., Pedersen, C. B., Arge, L., Tsirogiannis, C., Mortensen, P. B., & Svenning, J. C. (2019). Residential green space in childhood is associated with lower risk of psychiatric disorders from adolescence into adulthood. Proceedings of the National Academy of Sciences of the United States of America, 116(11), 5188–5193. [Google Scholar] [CrossRef]
- Every-Palmer, S., Grant, M. L., Thabrew, H., Hansby, O., Lawrence, M., Jenkins, M., & Romans, S. (2024). Not heading in the right direction: Five hundred psychiatrists’ views on resourcing, demand, and workforce across New Zealand mental health services. Australian and New Zealand Journal of Psychiatry, 58(1), 82–91. [Google Scholar] [CrossRef]
- Farrand, P., & Woodford, J. (2013). Impact of support on the effectiveness of written cognitive behavioural self-help: A systematic review and meta-analysis of randomised controlled trials. Clinical Psychology Review, 33(1), 182–195. [Google Scholar] [CrossRef]
- Fava, G. A., Cosci, F., Guidi, J., & Tomba, E. (2017). Well-being therapy in depression: New insights into the role of psychological well-being in the clinical process. Depression and Anxiety, 34(9), 801–808. [Google Scholar] [CrossRef]
- Fincham, G. W., Strauss, C., Montero-Marin, J., & Cavanagh, K. (2023). Effect of breathwork on stress and mental health: A meta-analysis of randomised-controlled trials. Scientific Reports, 13(1). [Google Scholar] [CrossRef] [PubMed]
- Firth, J., Solmi, M., Wootton, R. E., Vancampfort, D., Schuch, F. B., Hoare, E., Gilbody, S., Torous, J., Teasdale, S. B., Jackson, S. E., Smith, L., Eaton, M., Jacka, F. N., Veronese, N., Marx, W., Ashdown-Franks, G., Siskind, D., Sarris, J., Rosenbaum, S., … Stubbs, B. (2020). A meta-review of “lifestyle psychiatry”: The role of exercise, smoking, diet and sleep in the prevention and treatment of mental disorders. World Psychiatry, 19(3), 360–380. [Google Scholar] [CrossRef]
- Fleming, T., Bavin, L., Lucassen, M., Stasiak, K., Hopkins, S., & Merry, S. (2018). Beyond the trial: Systematic review of real-world uptake and engagement with digital self-help interventions for depression, low mood, or anxiety. Journal of Medical Internet Research, 20(6), e199. [Google Scholar] [CrossRef]
- Frumkin, H., Bratman, G. N., Breslow, S. J., Cochran, B., Kahn, P. H., Lawler, J. J., Levin, P. S., Tandon, P. S., Varanasi, U., Wolf, K. L., & Wood, S. A. (2017). Nature contact and human health: A research agenda. Environmental Health Perspectives, 125(7), 075001. [Google Scholar] [CrossRef] [PubMed]
- Gulliver, A., Griffiths, K. M., & Christensen, H. (2010). Perceived barriers and facilitators to mental health help-seeking in young people: A systematic review. BMC Psychiatry, 10, 113. [Google Scholar] [CrossRef] [PubMed]
- Hewis, J. (2023). A salutogenic approach: Changing the paradigm. Journal of Medical Imaging and Radiation Sciences, 54(2), S17–S21. [Google Scholar] [CrossRef] [PubMed]
- Hunter, R. F., Nieuwenhuijsen, M., Fabian, C., Murphy, N., O’Hara, K., Rappe, E., Sallis, J. F., Lambert, E. V., Duenas, O. L. S., Sugiyama, T., & Kahlmeier, S. (2023). Advancing urban green and blue space contributions to public health. The Lancet Public Health, 8(9), e735–e742. [Google Scholar] [CrossRef]
- Huynh, T., & Torquati, J. C. (2019). Examining connection to nature and mindfulness at promoting psychological well-being. Journal of Environmental Psychology, 66, 101370. [Google Scholar] [CrossRef]
- Jacobson, N. S., & Truax, P. (1991). Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology, 59(1), 12–19. [Google Scholar] [CrossRef]
- Jahrami, H., Trabelsi, K., Ghazzawi, H., Ammar, A., Pandi-Perumal, S. R., Saif, Z., & Vitiello, M. V. (2024). Internal consistency and test–retest reliability of the jenkins sleep scale across international versions: A reliability generalization meta-analysis. Current Sleep Medicine Reports, 10(2), 289–300. [Google Scholar] [CrossRef]
- Juhola, J., Arokoski, J. P. A., Ervasti, J., Kivimäki, M., Vahtera, J., Myllyntausta, S., & Saltychev, M. (2021). Internal consistency and factor structure of Jenkins Sleep Scale: Cross-sectional cohort study among 80,000 adults. BMJ Open, 11, 43276. [Google Scholar] [CrossRef]
- Karyotaki, E., Efthimiou, O., Miguel, C., Bermpohl, F. M. G., Furukawa, T. A., Cuijpers, P., Riper, H., Patel, V., Mira, A., Gemmil, A. W., Yeung, A. S., Lange, A., Williams, A. D., Mackinnon, A., Geraedts, A., Van Straten, A., Meyer, B., Björkelund, C., Knaevelsrud, C., … Forsell, Y. (2021). Internet-based cognitive behavioral therapy for depression: A Systematic review and individual patient data network meta-analysis. JAMA Psychiatry, 78(4), 361–371. [Google Scholar] [CrossRef]
- Karyotaki, E., Kleiboer, A., Smit, F., Turner, D. T., Pastor, A. M., Andersson, G., Berger, T., Botella, C., Breton, J. M., Carlbring, P., Christensen, H., De Graaf, E., Griffiths, K., Donker, T., Farrer, L., Huibers, M. J. H., Lenndin, J., Mackinnon, A., Meyer, B., … Cuijpers, P. (2015). Predictors of treatment dropout in self-guided web-based interventions for depression: An ‘individual patient data’ meta-analysis. Psychological Medicine, 45(13), 2717–2726. [Google Scholar] [CrossRef] [PubMed]
- Kassebaum, N. J., Arora, M., Barber, R. M., Brown, J., Carter, A., Casey, D. C., Charlson, F. J., Coates, M. M., Coggeshall, M., Cornaby, L., Dandona, L., Dicker, D. J., Erskine, H. E., Ferrari, A. J., Fitzmaurice, C., Foreman, K., Forouzanfar, M. H., Fullman, N., Goldberg, E. M., … Zuhlke, L. J. (2016). Global, regional, and national disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE), 1990–2015: A systematic analysis for the global burden of disease study 2015. The Lancet, 388(10053), 1603–1658. [Google Scholar] [CrossRef]
- Koivisto, M., & Grassini, S. (2023). Mental imagery of nature induces positive psychological effects. Current Psychology, 42, 30348–30363. [Google Scholar] [CrossRef]
- Kroenke, K., Strine, T. W., Spitzer, R. L., Williams, J. B. W., Berry, J. T., & Mokdad, A. H. (2009). The PHQ-8 as a measure of current depression in the general population. Journal of Affective Disorders, 114(1–3), 163–173. [Google Scholar] [CrossRef]
- Lagnado, A. M., Gilchrist, K., Cvancarova Smastuen, M., & Memon, A. (2017). Is subjective wellbeing associated with depression? A cross-sectional survey in southeast England: Anjum memon. European Journal of Public Health, 27(Suppl. 3). [Google Scholar] [CrossRef]
- Lancaster, G. A. (2015). Pilot and feasibility studies come of age! Pilot and Feasibility Studies, 1(1), 1. [Google Scholar] [CrossRef]
- Liddon, L., Kingerlee, R., & Barry, J. A. (2018). Gender differences in preferences for psychological treatment, coping strategies, and triggers to help-seeking. The British Journal of Clinical Psychology, 57(1), 42–58. [Google Scholar] [CrossRef] [PubMed]
- Ly, K. H., Ly, A. M., & Andersson, G. (2017). A fully automated conversational agent for promoting mental well-being: A pilot RCT using mixed methods. Internet Interventions, 10, 39–46. [Google Scholar] [CrossRef] [PubMed]
- Lynch, L., Long, M., & Moorhead, A. (2018). Young men, help-seeking, and mental health services: Exploring barriers and solutions. American Journal of Men’s Health, 12(1), 138–149. [Google Scholar] [CrossRef]
- Mack, D. E., Vo, K. T., & Wilson, P. M. (2024). The long and short-form warwick-edinburgh mental well-being scale: A Reliability generalization meta-analysis. Journal of Happiness Studies, 25(1–2), 12. [Google Scholar] [CrossRef]
- Mareya, S., Watts, M. C., Zhao, L., & Olasoji, M. (2024). Exploring the stepped care model in delivering primary mental health services—A scoping review. International Journal of Mental Health Nursing, 33(6), 2026–2042. [Google Scholar] [CrossRef]
- Mazzucchelli, T. G., Kane, R. T., & Rees, C. S. (2010). Behavioral activation interventions for well-being: A meta-analysis. Journal of Positive Psychology, 5(2), 105–121. [Google Scholar] [CrossRef] [PubMed]
- McCoy, C. E. (2017). Understanding the intention-to-treat principle in randomized controlled trials. Western Journal of Emergency Medicine, 18(6), 1075. [Google Scholar] [CrossRef] [PubMed]
- McDaid, D., Park, A.-L., Davidson, G., John, A., Knifton, L., Morton, A., & Thorpe, L. (2022). The economic case for investing in the prevention of mental health conditions in the UK. Mental Health Foundation. [Google Scholar]
- McEwan, K., Giles, D., Clarke, F. J., Kotera, Y., Evans, G., Terebenina, O., Minou, L., Teeling, C., Basran, J., Wood, W., & Weil, D. (2021). A pragmatic controlled trial of forest bathing compared with compassionate mind training in the UK: Impacts on self-reported wellbeing and heart rate variability. Sustainability, 13(3), 1380. [Google Scholar] [CrossRef]
- McKenzie, K., Murray, A., & Booth, T. (2013). Do urban environments increase the risk of anxiety, depression and psychosis? An epidemiological study. Journal of Affective Disorders, 150(3), 1019–1024. [Google Scholar] [CrossRef]
- Mental health pressures data analysis. (n.d.). Available online: https://www.bma.org.uk/advice-and-support/nhs-delivery-and-workforce/pressures/mental-health-pressures-data-analysis (accessed on 9 October 2024).
- Moreno-Agostino, D., Wu, Y. T., Daskalopoulou, C., Hasan, M. T., Huisman, M., & Prina, M. (2021). Global trends in the prevalence and incidence of depression:a systematic review and meta-analysis. Journal of Affective Disorders, 281, 235–243. [Google Scholar] [CrossRef]
- Nisbet, E. K., & Zelenski, J. M. (2013). The NR-6: A new brief measure of nature relatedness. Frontiers in Psychology, 4, 813. [Google Scholar] [CrossRef]
- Owens, M., & Bunce, H. (2023). The effect of brief exposure to virtual nature on mental wellbeing in adolescents. Scientific Reports, 13(1), 119. [Google Scholar] [CrossRef]
- Owens, M., & Bunce, H. L. I. (2022). The potential for outdoor nature-based interventions in the treatment and prevention of depression. Frontiers in Psychology, 13, 740210. [Google Scholar] [CrossRef]
- Owens, M., Leivang, R., & Bunce, H. (2024). Nature-based guided imagery and meditation significantly enhance mental well-being and reduce depressive symptoms: A randomized experiment. Ecopsychology, 17(1), 27–41. [Google Scholar] [CrossRef]
- Petrocchi, N., Ottaviani, C., Cheli, S., Matos, M., Baldi, B., Basran, J. K., & Gilbert, P. (2023). The impact of compassion-focused therapy on positive and negative mental health outcomes: Results of a series of meta-analyses. Clinical Psychology: Science and Practice, 31(2), 230. [Google Scholar] [CrossRef]
- Petrunoff, N., Yao, J., Sia, A., Ng, A., Ramiah, A., Wong, M., Han, J., Tai, B. C., Uijtdewilligen, L., & Müller-Riemenschneider, F. (2021). Activity in nature mediates a park prescription intervention’s effects on physical activity, park use and quality of life: A mixed-methods process evaluation. BMC Public Health, 21(1), 204. [Google Scholar] [CrossRef]
- Piotrowski, M. C., Lunsford, J., & Gaynes, B. N. (2021). Lifestyle psychiatry for depression and anxiety: Beyond diet and exercise. Lifestyle Medicine, 2(1), e21. [Google Scholar] [CrossRef]
- Plummer, F., Manea, L., Trepel, D., & McMillan, D. (2016). Screening for anxiety disorders with the GAD-7 and GAD-2: A systematic review and diagnostic metaanalysis. General Hospital Psychiatry, 39, 24–31. [Google Scholar] [CrossRef]
- Powell, L., Vasiliou, V., & Thompson, A. (2023). An ACT self-help intervention for adults with a visible difference in appearance: A pilot feasibility and acceptability randomized controlled study. Body Image, 47, 101637. [Google Scholar] [CrossRef] [PubMed]
- Pozzar, R., Hammer, M. J., Underhill-Blazey, M., Wright, A. A., Tulsky, J. A., Hong, F., Gundersen, D. A., & Berry, D. L. (2020). Threats of bots and other bad actors to data quality following research participant recruitment through social media: Cross-sectional questionnaire. Journal of Medical Internet Research, 22(10), e23021. [Google Scholar] [CrossRef] [PubMed]
- Pretty, J., & Barton, J. (2020). Nature-based interventions and mind–body interventions: Saving public health costs whilst increasing life satisfaction and happiness. International Journal of Environmental Research and Public Health, 17(21), 7769. [Google Scholar] [CrossRef]
- Pruessner, L., Timm, C., Barnow, S., Rubel, J. A., Lalk, C., & Hartmann, S. (2024). Effectiveness of a web-based cognitive behavioral self-help intervention for binge eating disorder: A randomized clinical trial. JAMA Network Open, 7(5), e2411127. [Google Scholar] [CrossRef]
- Rosa, C. D., Larson, L. R., Collado, S., & Profice, C. C. (2021). Forest therapy can prevent and treat depression: Evidence from meta-analyses. Urban Forestry and Urban Greening, 57, 126943. [Google Scholar] [CrossRef]
- Sagar-Ouriaghli, I., Brown, J. S. L., Tailor, V., & Godfrey, E. (2020). Engaging male students with mental health support: A qualitative focus group study. BMC Public Health, 20(1), 1159. [Google Scholar] [CrossRef] [PubMed]
- Sarris, J., Thomson, R., Hargraves, F., Eaton, M., de Manincor, M., Veronese, N., Solmi, M., Stubbs, B., Yung, A. R., & Firth, J. (2020). Multiple lifestyle factors and depressed mood: A cross-sectional and longitudinal analysis of the UK Biobank (N = 84,860). BMC Medicine, 18(1), 354. [Google Scholar] [CrossRef]
- Seidler, Z. E., Dawes, A. J., Rice, S. M., Oliffe, J. L., & Dhillon, H. M. (2016). The role of masculinity in men’s help-seeking for depression: A systematic review. Clinical Psychology Review, 49, 106–118. [Google Scholar] [CrossRef]
- Shafran, R., Egan, S. J., de Valle, M., Davey, E., Carlbring, P., Creswell, C., & Wade, T. D. (2024). A guide for self-help guides: Best practice implementation. Cognitive Behaviour Therapy, 53(5), 561–575. [Google Scholar] [CrossRef]
- Shah, N., Cader, M., Andrews, B., McCabe, R., & Stewart-Brown, S. L. (2021). Short Warwick-Edinburgh Mental Well-being Scale (SWEMWBS): Performance in a clinical sample in relation to PHQ-9 and GAD-7. Health and Quality of Life Outcomes, 19(1), 260. [Google Scholar] [CrossRef]
- Shanahan, D. F., Astell-Burt, T., Barber, E. A., Brymer, E., Cox, D. T. C., Dean, J., Depledge, M., Fuller, R. A., Hartig, T., Irvine, K. N., Jones, A., Kikillus, H., Lovell, R., Mitchell, R., Niemelä, J., Nieuwenhuijsen, M., Pretty, J., Townsend, M., Van Heezik, Y., … Gaston, K. J. (2019). Nature-based interventions for improving health and wellbeing: The purpose, the people and the outcomes. Sports, 7, 141. [Google Scholar] [CrossRef]
- Shidhaye, R. (2023). Global priorities for improving access to mental health services for adolescents in the post-pandemic world. Current Opinion in Psychology, 53, 101661. [Google Scholar] [CrossRef] [PubMed]
- Singh, V., Kumar, A., & Gupta, S. (2022). Mental health prevention and promotion—A narrative review. Frontiers in Psychiatry, 13, 898009. [Google Scholar] [CrossRef]
- Spitzer, R. L., Kroenke, K., Williams, J. B. W., & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097. [Google Scholar] [CrossRef]
- Stenhoff, A., Steadman, L., Nevitt, S., Benson, L., & White, R. G. (2020). Acceptance and commitment therapy and subjective wellbeing: A systematic review and meta-analyses of randomised controlled trials in adults. Journal of Contextual Behavioral Science, 18, 256–272. [Google Scholar] [CrossRef]
- Stigsdotter, U. K., Corazon, S. S., Sidenius, U., Nyed, P. K., Larsen, H. B., & Fjorback, L. O. (2018). Efficacy of nature-based therapy for individuals with stress-related illnesses: Randomised controlled trial. The British Journal of Psychiatry, 213(1), 404–411. [Google Scholar] [CrossRef]
- Tennant, R., Hiller, L., Fishwick, R., Platt, S., Joseph, S., Weich, S., Parkinson, J., Secker, J., & Stewart-Brown, S. (2007). The Warwick-Dinburgh mental well-being scale (WEMWBS): Development and UK validation. Health and Quality of Life Outcomes, 5, 63. [Google Scholar] [CrossRef]
- Thornicroft, G., Chatterji, S., Evans-Lacko, S., Gruber, M., Sampson, N., Aguilar-Gaxiola, S., Al-Hamzawi, A., Alonso, J., Andrade, L., Borges, G., Bruffaerts, R., Bunting, B., De Almeida, J. M. C., Florescu, S., De Girolamo, G., Gureje, O., Haro, J. M., He, Y., Hinkov, H., … Kessler, R. C. (2017). Undertreatment of people with major depressive disorder in 21 countries. The British Journal of Psychiatry, 210(2), 119–124. [Google Scholar] [CrossRef]
- Tong, L., Panagiotopoulou, O. M., Cuijpers, P., & Karyotaki, E. (2024). The effectiveness of self-guided interventions in adults with depressive symptoms: A systematic review and meta-analysis. EBioMedicine, 105, 105208. [Google Scholar] [CrossRef] [PubMed]
- Treynor, W., Gonzalez, R., & Nolen-Hoeksema, S. (2003). Rumination reconsidered: A psychometric analysis. Cognitive Therapy and Research, 27(3), 247–259. [Google Scholar] [CrossRef]
- Tursi, M. F. D. S., Baes, C. V. W., Camacho, F. R. D. B., Tofoli, S. M. D. C., & Juruena, M. F. (2013). Effectiveness of psychoeducation for depression: A systematic review. Australian & New Zealand Journal of Psychiatry, 47(11), 1019–1031. [Google Scholar] [CrossRef]
- van Agteren, J., Iasiello, M., Lo, L., Bartholomaeus, J., Kopsaftis, Z., Carey, M., & Kyrios, M. (2021). A systematic review and meta-analysis of psychological interventions to improve mental wellbeing. Nature Human Behaviour, 5(5), 631–652. [Google Scholar] [CrossRef] [PubMed]
- van der Wal, J. M., van Borkulo, C. D., Deserno, M. K., Breedvelt, J. J. F., Lees, M., Lokman, J. C., Borsboom, D., Denys, D., van Holst, R. J., Smidt, M. P., Stronks, K., Lucassen, P. J., van Weert, J. C. M., Sloot, P. M. A., Bockting, C. L., & Wiers, R. W. (2021). Advancing urban mental health research: From complexity science to actionable targets for intervention. The Lancet Psychiatry, 8(11), 991–1000. [Google Scholar] [CrossRef] [PubMed]
- Van Der Watt, A. S. J., Odendaal, W., Louw, K., & Seedat, S. (2020). Distant mood monitoring for depressive and bipolar disorders: A systematic review. BMC Psychiatry, 20(1), 383. [Google Scholar] [CrossRef]
- Vigo, D., Haro, J. M., Hwang, I., Aguilar-Gaxiola, S., Alonso, J., Borges, G., Bruffaerts, R., Caldas-De-Almeida, J. M., De Girolamo, G., Florescu, S., Gureje, O., Karam, E., Karam, G., Kovess-Masfety, V., Lee, S., Navarro-Mateu, F., Ojagbemi, A., Posada-Villa, J., Sampson, N. A., … Kessler, R. C. (2022). Towards measuring effective treatment coverage: Critical bottlenecks in quality- and user-adjusted coverage for major depressive disorder. Psychological Medicine, 52(10), 1. [Google Scholar] [CrossRef]
- Walters, S. J., Dos Anjos Henriques-Cadby, I. B., Bortolami, O., Flight, L., Hind, D., Jacques, R. M., Knox, C., Nadin, B., Rothwell, J., Surtees, M., & Julious, S. A. (2017). Recruitment and retention of participants in randomised controlled trials: A review of trials funded and published by the United Kingdom health technology assessment programme. BMJ Open, 7(3), e015276. [Google Scholar] [CrossRef] [PubMed]
- Warttig, S. L., Forshaw, M. J., South, J., & White, A. K. (2013). New, normative, English-sample data for the short form perceived stress scale (PSS-4). Journal of Health Psychology, 18(12), 1617–1628. [Google Scholar] [CrossRef]
- Wendt, D., & Shafer, K. (2016). Gender and attitudes about mental health help seeking: Results from national data. Health & Social Work, 41(1), e20–e28. [Google Scholar] [CrossRef]
- Whitehead, A. L., Julious, S. A., Cooper, C. L., & Campbell, M. J. (2016). Estimating the sample size for a pilot randomised trial to minimise the overall trial sample size for the external pilot and main trial for a continuous outcome variable. Statistical Methods in Medical Research, 25(3), 1057–1073. [Google Scholar] [CrossRef]
- Wood, A. M., & Joseph, S. (2010). The absence of positive psychological (eudemonic) well-being as a risk factor for depression: A ten year cohort study. Journal of Affective Disorders, 122(3), 213–217. [Google Scholar] [CrossRef]
- World Health Organisation. (2017). Depression and other common mental disorders: Global health estimates. World Health Organisation. Available online: https://apps.who.int/iris/bitstream/handle/10665/254610/WHO-MSD-MER-2017.2-eng.pdf (accessed on 13 May 2025).
- Xu, Y., Pace, S., Kim, J., Iachini, A., King, L. B., Harrison, T., Dehart, D., Levkoff, S. E., Browne, T. A., Lewis, A. A., Kunz, G. M., Reitmeier, M., Utter, R. K., & Simone, M. (2022). Threats to online surveys: Recognizing, detecting, and preventing survey bots. Social Work Research, 46(4), 343–350. [Google Scholar] [CrossRef]
- Yao, W., Zhang, X., & Gong, Q. (2021). The effect of exposure to the natural environment on stress reduction: A meta-analysis. Urban Forestry and Urban Greening, 57, 126932. [Google Scholar] [CrossRef]
- Zhang, D., Lee, E. K. P., Mak, E. C. W., Ho, C. Y., & Wong, S. Y. S. (2021). Mindfulness-based interventions: An overall review. British Medical Bulletin, 138(1), 41–57. [Google Scholar] [CrossRef] [PubMed]


| VARIABLE | Intervention Group (n = 22) | Waitlist Group (n = 20) | p Value |
|---|---|---|---|
| Age, n (%) | 0.41 | ||
| 18–24 | 3 (13.64) | 5 (25.00) | |
| 25–34 | 4 (18.18) | 2 (10.00) | |
| 35–44 | 6 (27.27) | 8 (40.00) | |
| 45–54 | 8 (36.36) | 3 (15.00) | |
| 55–64 | 1 (4.54) | 2 (10.00) | |
| Gender, n (%) | 0.16 | ||
| Female | 21 (95.50) | 15 (75.00) | |
| Male | 1 (4.5) | 4 (20.00) | |
| Non-binary/third gender | 0 (0.00) | 1 (5.00) | |
| Ethnicity, n (%) | 0.37 | ||
| White | 21 (95.45) | 19 (95.00) | |
| Asian | 1 (4.55) | 0 (0.00) | |
| Prefer not to say | 0 (0.00) | 1 (5.00) | |
| Ses, n (%) | 0.30 | ||
| High | 0 (0.00) | 2 (10.00) | |
| Middle | 14 (63.64) | 12 (60.00) | |
| Low | 5 (22.73) | 2 (10.00) | |
| Prefer not to say | 1 (4.55) | 2 (10.00) | |
| No response | 2 (9.10) | 2 (10.00) | 0.80 |
| Strongly Disagree n (%) | Disagree n (%) | Neutral n (%) | Agree n (%) | Strongly Agree n (%) | |
|---|---|---|---|---|---|
| Overall, I enjoyed doing the Roots and Shoots programme | |||||
| 0 (0.00) | 0 (0.00) | 0 (0.00) | 10 (58.82) | 7 (41.18) | |
| I would come back and use the Roots and Shoots guidebook again in the future | |||||
| 0 (0.00) | 0 (0.00) | 1 (5.88) | 8 (47.06) | 8 (47.06) | |
| The Roots and Shoots programme was helpful in improving my wellbeing | |||||
| 0 (0.00) | 0 (0.00) | 2 (11.76) | 10 (58.82) | 5 (29.41) | |
| I would recommend the Roots and Shoots programme to a friend | |||||
| 1 (5.88) | 0 (0.00) | 0 (0.00) | 9 (52.94) | 7 (41.18) | |
| The information in the guidebook was helpful | |||||
| 0 (0.00) | 0 (0.00) | 1 (5.88) | 11 (64.71) | 5 (29.41) | |
| The habit wheel was helpful | |||||
| 0 (0.00) | 0 (0.00) | 4 (23.53) | 8 (47.06) | 5 (29.41) | |
| The habit and mood tracker was helpful | |||||
| 1 (5.88) | 0 (0.00) | 2 (11.76) | 7 (41.18) | 7 (41.18) | |
| The expressive writing tool was helpful | |||||
| 0 (0.00) | 3 (17.65) | 3 (17.65) | 7 (41.18) | 4 (23.53) | |
| The coping tool was helpful | |||||
| 1 (5.88) | 0 (0.00) | 4 (23.53) | 10 (58.82) | 2 (11.76) | |
| The honeycomb challenge was helpful | |||||
| 0 (0.00) | (0.00) | 8 (47.06) | 6 (35.29) | 3 (17.65) | |
| I found the nature videos helpful | |||||
| 0 (0.00) | 0 (0.00) | 5 (29.41) | 9 (52.94) | 3 (17.65) | |
| I found the meditations helpful | |||||
| 0 (0.00) | 1 (5.88) | 6 (35.29) | 8 (47.06) | 2 (11.76) | |
| I found the breathing exercises helpful | |||||
| 0 (0.00) | 0 (0.00) | 3 (17.65) | 8 (47.06) | 6 (35.29) | |
| Measure | T0 | T0 Difference by Arm | T1 | Change from Baseline (T0–T1) | T1 Effect Size Between Group | T2 | Change from Baseline (T0–T2) | T2 Effect Size Between Group |
|---|---|---|---|---|---|---|---|---|
| Mean (sd) | Hedges’ g (CI) | Mean (sd) | Hedges’ g (CI) | Mean (sd) | Hedges’ g (CI) | |||
| SWEMWBS | ||||||||
| Intervention | 19.09 (2.83) | −0.09 (−0.68 to 0.51) | 23.25 (3.16) | 4.16 | 1.08 (0.42 to 1.73) | 24.36 (3.02) | 5.27 | 1.24 (0.57 to 1.91) |
| Waitlist | 19.35 (3.03) | 20.30 (3.93) | 0.95 | 20.92 (4.08) | 1.52 | |||
| GAD | ||||||||
| Intervention | 9.40 (4.63) | 0.05 (−0.55 to 0.64) | 6.93 (3.92) | −2.47 | −0.45 (−1.07 to 0.17) | 5.46 (3.31) | −3.94 | −0.54 (−1.16 to 0.08) |
| Waitlist | 9.20 (3.91) | 8.71 (4.73) | −0.49 | 7.63 (3.27) | −1.57 | |||
| PHQ | ||||||||
| Intervention | 10.39 (4.64) | 0.02 (−0.58 to 0.61) | 8.42 (5.03) | −1.97 | −0.23 (−0.84 to 0.38) | 7.25 (4.38) | −3.14 | −0.48 (−1.10 to 0.14) |
| Waitlist | 10.30 (4.40) | 9.38 (4.48) | −0.92 | 9.38 (4.61) | −0.92 | |||
| PSS | ||||||||
| Intervention | 9.09 (1.93) | 0.17 (−0.43 to 0.76) | 7.36 (1.84) | −1.73 | −0.78 (−1.41 to −0.14) | 6.36 (1.77) | −2.73 | −0.67 (−1.30 to −0.04) |
| Waitlist | 8.73 (2.30) | 8.67 (1.73) | −0.06 | 7.45 (2.28) | −1.28 | |||
| RRS | ||||||||
| Intervention | 12.07 (2.95) | −0.22 (−0.82 to 0.37) | 11.52 (3.12) | −0.55 | −0.07 (−0.68 to 0.54) | 9.72 (3.31) | −2.35 | −0.56 (−1.19 to 0.06) |
| Waitlist | 12.76 (3.14) | 12.43 (3.28) | −0.33 | 12.16 (2.93) | −0.60 | |||
| JSS | ||||||||
| Intervention | 11.75 (4.88) | −0.14 (−0.73 to 0.46) | 11.95 (4.23) | 0.20 | 0.24 (−0.37 to 0.85) | 9.42 (4.68) | −2.33 | −0.17 (−0.78 to 0.45) |
| Waitlist | 12.44 (5.08) | 11.43 (5.39) | −1.01 | 10.95 (5.60) | −1.49 | |||
| FFMQ | ||||||||
| Intervention | 34.79 (5.76) | 0.19 (−0.41 to 0.78) | 35.32 (4.73) | 0.53 | 0.12 (−0.49 to 0.73) | 39.98 (5.50) | 5.19 | 0.70 (0.07 to 1.33) |
| Waitlist | 33.56 (7.02) | 33.33 (6.70) | −0.23 | 34.16 (7.00) | 0.60 | |||
| NR6 | ||||||||
| Intervention | 3.95 (0.78) | −0.30 (−0.90 to 0.29) | 4.11 (0.63) | 0.16 | 0.26 (−0.35 to 0.88) | 4.46 (0.50) | 0.51 | 0.61 (−0.02 to 1.23) |
| Waitlist | 4.18 (0.70) | 4.14 (0.89) | −0.04 | 4.23 (0.70) | 0.05 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Owens, M.; Houghton, C.; Beattie, P.; Bunce, H.L.I. Roots and Shoots: A Pilot Parallel Randomised Controlled Trial Assessing the Feasibility and Acceptability of a Nature-Based Self-Help Intervention for Low Wellbeing. Behav. Sci. 2025, 15, 1096. https://doi.org/10.3390/bs15081096
Owens M, Houghton C, Beattie P, Bunce HLI. Roots and Shoots: A Pilot Parallel Randomised Controlled Trial Assessing the Feasibility and Acceptability of a Nature-Based Self-Help Intervention for Low Wellbeing. Behavioral Sciences. 2025; 15(8):1096. https://doi.org/10.3390/bs15081096
Chicago/Turabian StyleOwens, Matthew, Chloe Houghton, Paige Beattie, and Hannah L. I. Bunce. 2025. "Roots and Shoots: A Pilot Parallel Randomised Controlled Trial Assessing the Feasibility and Acceptability of a Nature-Based Self-Help Intervention for Low Wellbeing" Behavioral Sciences 15, no. 8: 1096. https://doi.org/10.3390/bs15081096
APA StyleOwens, M., Houghton, C., Beattie, P., & Bunce, H. L. I. (2025). Roots and Shoots: A Pilot Parallel Randomised Controlled Trial Assessing the Feasibility and Acceptability of a Nature-Based Self-Help Intervention for Low Wellbeing. Behavioral Sciences, 15(8), 1096. https://doi.org/10.3390/bs15081096





