An Integrated Cognitive Remediation and Recovery-Oriented Program for Individuals with Bipolar Disorder Using a Virtual Reality-Based Intervention: 6- and 12-Month Cognitive Outcomes from a Randomized Feasibility Trial
Abstract
1. Introduction
Aim
2. Materials and Methods
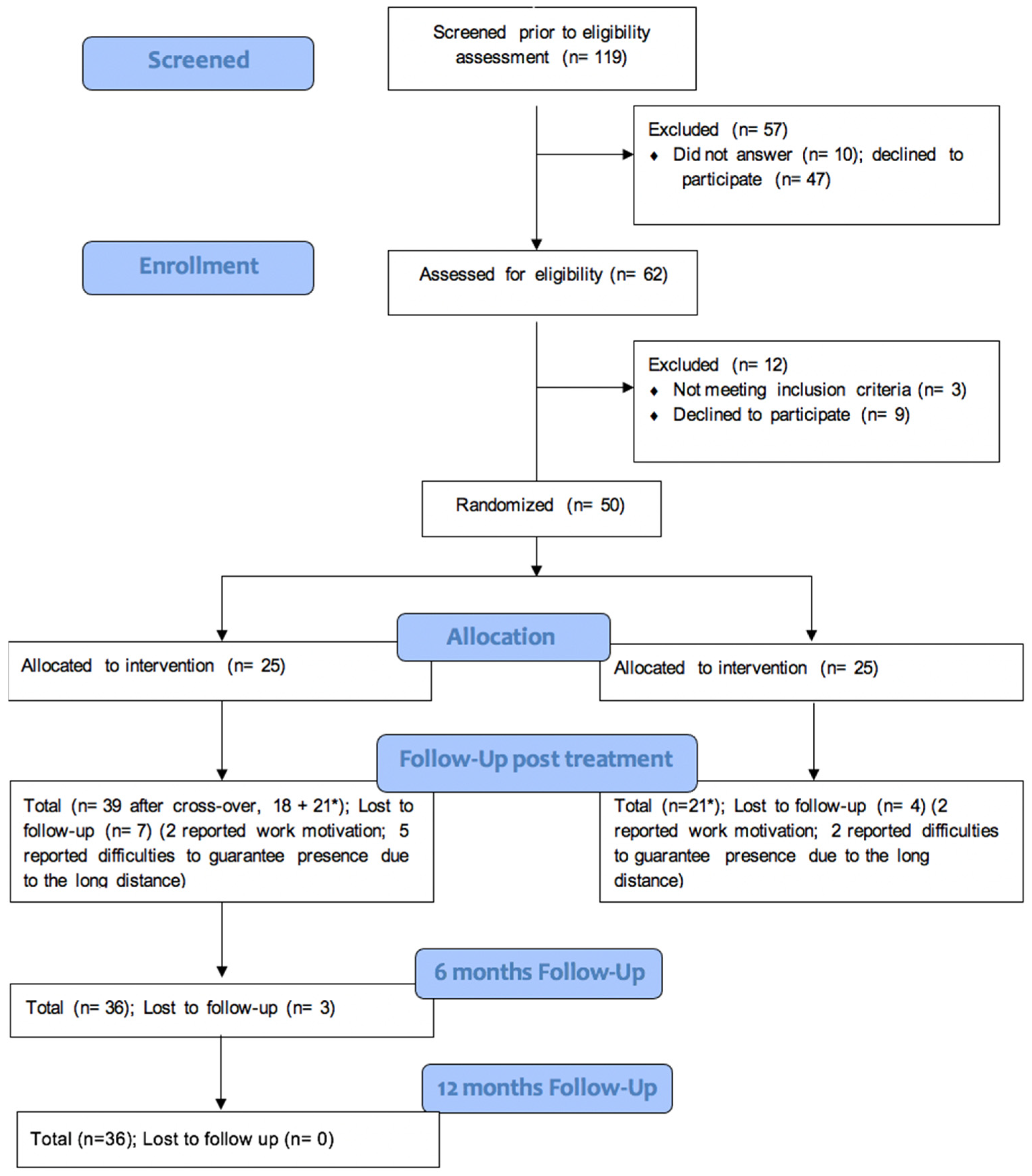
2.1. Study Design
2.2. Participants and Simple Size Considerations
2.3. Outcomes and Data Collection
- -
- Visuospatial function: Rey Figure Test (Caffarra et al., 2002a);
- -
- Attention and immediate recall: Matrix Test (Spinnler & Tognoni, 1987) and Rey’s Words Test (Caltagirone et al., 1995);
- -
- Attention function: Forward Digit Span (Orsini et al., 1987; Bisiacchi et al., 2003) and Trail Making Test, Part A (Spinnler & Tognoni, 1987; Giovagnoli et al., 1996);
- -
- Memory function: Rey’s Words Test Delayed Recall (Caltagirone et al., 1995), Test of the Tale (Carlesimo et al., 2002), and Backward Digit Span (Orsini et al., 1987; Bisiacchi et al., 2003);
- -
- Language function: Phonological and Semantic Verbal Fluency Test, both versions (Carlesimo et al., 2002; Novelli et al., 1986);
- -
- Executive function: Digital Symbol Substitution Test (Amodio et al., 2002, 2008), Trail Making Test, Part B (Amodio et al., 2008), Stroop Test (Caffarra et al., 2002b), Frontal Assessment Battery (FAB) (Dubois et al., 2000), and Cognitive Estimates Test (CET) (Scarpina et al., 2015; Della Sala et al., 2003).
2.4. Intervention
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CR | Cognitive Remediation |
| VR | Virtual Reality |
| BD | Bipolar Disorder |
| CI | Cognitive Impairment |
| CONSORT | Consolidated Standards of Reporting Trial |
| FAB | Frontal Assessment Battery |
| CES | Cognitive Estimates Test |
References
- Abdulatif, M., Mukhtar, A., & Obayah, G. (2015). Pitfalls in reporting sample size calculation in randomized controlled trials published in leading anaesthesia journals: A systematic review. British Journal of Anaesthesia, 115(5), 699–707. [Google Scholar] [CrossRef] [PubMed]
- Amodio, P., Campagna, F., Olianas, S., Iannizzi, P., Mapelli, D., Penzo, M., Angeli, P., & Gatta, A. (2008). Detection of minimal hepatic encephalopathy: Normalization and optimization of the Psychometric Hepatic Encephalopathy Score. A neuropsychological and quantified EEG study. Journal of Hepatology, 49(3), 346–353. [Google Scholar]
- Amodio, P., Wenin, H., Del Piccolo, F., Mapelli, D., Montagnese, S., Pellegrini, A., Musto, C., Gatta, A., & Umiltà, C. (2002). Variability of trail making test, symbol digit test and line trait test in normal people. A normative study taking into account age-dependent decline and sociobiological variables. Aging Clinical and Experimental Research, 14(2), 117–131. [Google Scholar] [CrossRef] [PubMed]
- Bernabei, L., Bersani, F. S., Pompili, E., Chiaie, R. D., Valente, D., Corrado, A., Vergnani, L., Ferracuti, S., Biondi, M., & De’Fornari, M. A. C. (2020). Cognitive remediation for the treatment of neuropsychological disturbances in subjects with euthymic bipolar disorder: Findings from a controlled study. Journal of Affective Disorders, 273, 576–585. [Google Scholar] [CrossRef] [PubMed]
- Bisiacchi, P. S., Mapelli, D., Mondini, S., & Vestri, A. (2003). Esame neuropsicologico breve, una batteria di test per lo screening neuropsicologico. Raffaello Cortina Editore. [Google Scholar]
- Bortolato, B., Miskowiak, K. W., Köhler, C. A., Vieta, E., & Carvalho, A. F. (2015). Cognitive dysfunction in bipolar disorder and schizophrenia: A systematic review of meta-analyses. Neuropsychiatric Disease and Treatment, 11, 3111–3125. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Caffarra, P., Vezzadini, G., Dieci, F., Zonato, F., & Venneri, A. (2002a). Rey-Osterrieth complex figure: Normative values in an Italian population sample. Neurological Sciences, 22(6), 443–447. [Google Scholar] [CrossRef]
- Caffarra, P., Vezzadini, G., Dieci, F., Zonato, F., & Venneri, A. (2002b). Una versione abbreviata del test di Stroop: Dati normativi nella popolazione italiana. Nuova Rivista di Neurologia, 12, 111–115. [Google Scholar]
- Caltagirone, C., Gainotti, G., Carlesimo, G. A., & Parnetti, L. (1995). Batteria per la valutazione del deterioramento mentale: I. Descrizione di uno strumento di diagnosi neuropsicologica. Archivio di Psicologia, Neurologia e Psichiatria, 14, 109–138. [Google Scholar]
- Carlesimo, G. A., Buccione, I., Fadda, L., Graceffa, A., Mauri, M., Lorusso, S., & Caltagirone, C. (2002). Standardizzazione di due test dimemoria per uso clinico: Breve racconto e figura di rey. Nuova Rivista di Neurologia, 12, 1–13. [Google Scholar]
- Carta, M. G., Kalcev, G., Fornaro, M., Pinna, S., Gonzalez, C. I. A., Nardi, A. E., & Primavera, D. (2023a). Does screening for bipolar disorders identify a “Dysregulation of Mood, Energy, and Social Rhythms Syndrome” (DYMERS)? A heuristic working hypothesis. Journal of Clinical Medicine, 12(15), 5162. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Carta, M. G., Kalcev, G., Scano, A., Gonzalez, C. I. A., Ouali, U., Pinna, S., Carrà, G., Romano, F., Preti, A., Orrù, G., Minerba, L., Cossu, G., Nardi, A. E., & Primavera, D. (2023b). The impact of MDQ positivity on quality of life impairment: Does it support the hypothesis of “Dysregulation of Mood, Energy, and Social Rhythms Syndrome” (DYMERS)? Journal of Public Health Research, 12(4), 22799036231208356. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Carta, M. G., Kalcev, G., Scano, A., Pinna, S., Gonzalez, C. I. A., Nardi, A. E., Orrù, G., & Primavera, D. (2023c). Screening, genetic variants, and bipolar disorders: Can useful hypotheses arise from the sum of partial failures? Clinics and Practice, 13(4), 853–862. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Carta, M. G., Kalcev, G., Scano, A., Primavera, D., Orrù, G., Gureye, O., Cossu, G., & Nardi, A. E. (2022). Is bipolar disorder the consequence of a genetic weakness or not having correctly used a potential adaptive condition? Brain Sciences, 13(1), 16. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Carta, M. G., Ouali, U., Perra, A., Ahmed, A. B. C., Boe, L., Aissa, A., Lorrai, S., Cossu, G., Aresti, A., Preti, A., & Nacef, F. (2021). Living with bipolar disorder in the time of COVID-19: Biorhythms during the severe lockdown in Cagliari, Italy, and the moderate lockdown in Tunis, Tunisia. Frontiers in Psychiatry, 12, 634765. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cella, M., Preti, A., Edwards, C., Dow, T., & Wykes, T. (2017). Cognitive remediation for negative symptoms of schizophrenia: A network meta-analysis. Clinical Psychology Review, 52, 43–51. [Google Scholar] [CrossRef] [PubMed]
- Cella, M., Reeder, C., & Wykes, T. (2015). Lessons learnt? The importance of metacognition and its implications for Cognitive Remediation in schizophrenia. Frontiers in Psychology, 6, 1259. [Google Scholar] [CrossRef] [PubMed] [PubMed Central][Green Version]
- Della Sala, S., MacPherson, S. E., Phillips, L., Sacco, L., & Spinnler, H. (2003). How many camels are there in Italy? Cognitive estimates standardised on the Italian population. Neurological Sciences, 24(1), 10–15. [Google Scholar] [CrossRef]
- Deste, G., Barlati, S., Cacciani, P., DePeri, L., Poli, R., Sacchetti, E., & Vita, A. (2015). Persistence of effectiveness of cognitive remediation interventions in schizophrenia: A 1-year follow-up study. Schizophrenia Research, 161(2–3), 403–406. [Google Scholar] [CrossRef] [PubMed]
- Douglas, K. M., Gallagher, P., Robinson, L. J., Carter, J. D., McIntosh, V. V., Frampton, C. M., Watson, S., Young, A. H., Ferrier, I. N., & Porter, R. J. (2018). Prevalence of cognitive impairment in major depression and bipolar disorder. Bipolar Disorders, 20(3), 260–274. [Google Scholar] [CrossRef] [PubMed]
- Dubois, B., Slachevsky, A., Litvan, I., & Pillon, B. F. A. B. (2000). The FAB: A frontal assessment battery at bedside. Neurology, 55(11), 1621–1626. [Google Scholar] [CrossRef]
- Ehrlich, T. J., Ryan, K. A., Burdick, K. E., Langenecker, S. A., McInnis, M. G., & Marshall, D. F. (2022). Cognitive subgroups and their longitudinal trajectories in bipolar disorder. Acta Psychiatrica Scandinavica, 146(3), 240–250. [Google Scholar] [CrossRef] [PubMed]
- Ehrminger, M., Brunet-Gouet, E., Cannavo, A. S., Aouizerate, B., Cussac, I., Azorin, J. M., Bellivier, F., Bougerol, T., Courtet, P., Dubertret, C., Etain, B., Kahn, J., Leboyer, M., Olié, E., FondaMental Advanced Centers of Expertise in Bipolar Disorders (FACE-BD) Collaborators, Passerieux, C., & Roux, P. (2021). Longitudinal relationships between cognition and functioning over 2 years in euthymic patients with bipolar disorder: A cross-lagged panel model approach with the FACE-BD cohort. The British Journal of Psychiatry, 218(2), 80–87. [Google Scholar] [CrossRef] [PubMed]
- Eldridge, S. M., Chan, C. L., Campbell, M. J., Bond, C. M., Hopewell, S., Thabane, L., & Lancaster, G. A. (2016). CONSORT 2010 statement: Extension to randomised pilot and feasibility trials. BMJ, 355, i5239. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Filser, M., Buchner, A., Fink, G. R., Gold, S. M., & Penner, I. (2023). The manifestation of affective symptoms in multiple sclerosis and discussion of the currently available diagnostic assessment tools. Journal of Neurology, 270(1), 171–207. [Google Scholar] [CrossRef] [PubMed]
- Fiorillo, A., & Giordano, A. (2022). The biopsychosocial model of schizophrenia and cancer: Unraveling the etiopathogenesis of complex diseases. European Psychiatry, 65(1), 1–5. [Google Scholar] [CrossRef]
- Freeman, D., Lister, R., Waite, F., Yu, L., Slater, M., Dunn, G., & Clark, D. (2019). Automated psychological therapy using virtual reality (VR) for patients with persecutory delusions: Study protocol for a single-blind parallel-group randomised controlled trial (THRIVE). Trials, 20(1), 87. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Freeman, D., Reeve, S., Robinson, A., Ehlers, A., Clark, D., Spanlang, B., & Slater, M. (2017). Virtual reality in the assessment, understanding, and treatment of mental health disorders. Psychological Medicine, 47(14), 2393–2400. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Giannouli, V. (2017). Insomnia-related sleep disruptions, cognition and detailed concurrent anxiety testing during the inter-episode phase of bipolar disorder: A Herculean task or a necessity? Journal of Psychiatric Research, 95, 76–77. [Google Scholar] [CrossRef]
- Giovagnoli, A. R., Del Pesce, M., Mascheroni, S., Simoncelli, M., Laiacona, M., & Capitani, E. (1996). Trail making test: Normative values from 287 normal adult controls. The Italian Journal of Neurological Sciences, 17(4), 305–309. [Google Scholar] [CrossRef]
- Goldberg, Z., Kuslak, B., & Kurtz, M. M. (2023). A meta-analytic investigation of cognitive remediation for mood disorders: Efficacy and the role of study quality, sample and treatment factors. Journal of Affective Disorders, 330, 74–82. [Google Scholar] [CrossRef]
- Huddy, V., Reeder, C., Kontis, D., Wykes, T., & Stahl, D. (2012). The effect of working alliance on adherence and outcome in cognitive remediation therapy. Journal of Nervous & Mental Disease, 200(7), 614–619. [Google Scholar] [CrossRef] [PubMed]
- Kosmidis, M. H., Bozikas, V. P., Giannouli, V., Karavatos, A., & Fokas, K. (2012). Familial comorbidity of bipolar disorder and multiple sclerosis: Genetic susceptibility, coexistence or causal relationship? Behavioural Neurology, 25(4), 341–349. [Google Scholar] [CrossRef] [PubMed]
- Lewandowski, K. E., Sperry, S. H., Cohen, B. M., Norris, L. A., Fitzmaurice, G. M., Ongur, D., & Keshavan, M. S. (2017). Treatment to enhance cognition in bipolar disorder (TREC-BD): Efficacy of a randomized controlled trial of cognitive remediation versus active control. The Journal of Clinical Psychiatry, 78(9), e1242–e1249. [Google Scholar] [CrossRef]
- Lima, F., Rabelo-da-Ponte, F. D., Bücker, J., Czepielewski, L., Hasse-Sousa, M., Telesca, R., Solé, B., Reinares, M., Vieta, E., & Rosa, A. R. (2019). Identifying cognitive subgroups in bipolar disorder: A cluster analysis. Journal of Affective Disorders, 246, 252–261. [Google Scholar] [CrossRef]
- Miskowiak, K. W., Burdick, K. E., Martinez-Aran, A., Bonnin, C., Bowie, C. R., Carvalho, A. F., Gallagher, P., Lafer, B., López-Jaramillo, C., Sumiyoshi, T., McIntyre, R. S., Schaffer, A., Porter, R. J., Torres, I. J., Yatham, L. N., Young, A. H., Kessing, L. V., & Vieta, E. (2017). Methodological recommendations for cognition trials in bipolar disorder by the International Society for Bipolar Disorders Targeting Cognition Task Force. Bipolar Disorders, 19(8), 614–626. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Novelli, G., Papagno, C., Capitani, E., & Laiacona, M. (1986). Tre test clinici di ricerca e produzione lessicale. Taratura su sogetti normali. Archivio di Psicologia, Neurologia e Psichiatria, 47, 477–506. [Google Scholar]
- Orsini, A., Grossi, D., Capitani, E., Laiacona, M., Papagno, C., & Vallar, G. (1987). Verbal and spatial immediate memory span: Normative data from 1355 adults and 1112 children. The Italian Journal of Neurological Sciences, 8(6), 537–548. [Google Scholar] [CrossRef]
- Ott, C. V., Macoveanu, J., Bowie, C. R., Fisher, P. M., Knudsen, G. M., Kessing, L. V., & Miskowiak, K. W. (2021). Change in prefrontal activity and executive functions after action-based cognitive remediation in bipolar disorder: A randomized controlled trial. Neuropsychopharmacology: Official Publication of the American College of Neuropsychopharmacology, 46(6), 1113–1121. [Google Scholar] [CrossRef]
- Perra, A., De Lorenzo, V., Zaccheddu, R., Locci, A., Piludu, F., Preti, A., Di Natale, L., Galetti, A., Nardi, A. E., Cossu, G., Sancassiani, F., Barbato, S., Cesaretti, O., Kurotshka, P. K., & Carta, M. G. (2022). Cognitive remediation virtual reality tool a tecovery-oriented project for people with bipolar disorder: Protocol of a feasibility randomized clinical trial. Clinical Practice and Epidemiology in Mental Health, 18(1), e174501792208220. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Perra, A., Galetti, A., Zaccheddu, R., Locci, A., Piludu, F., Preti, A., Primavera, D., Di Natale, L., Nardi, A. E., Kurotshka, P. K., Cossu, G., Sancassiani, F., Stella, G., De Lorenzo, V., Zreik, T., & Carta, M. G. (2023a). A recovery-oriented program for people with bipolar disorder through virtual reality-based cognitive remediation: Results of a feasibility randomized clinical trial. Journal of Clinical Medicine, 12(6), 2142. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Perra, A., Riccardo, C. L., De Lorenzo, V., De Marco, E., Di Natale, L., Kurotschka, P. K., Preti, A., & Carta, M. G. (2023b). Fully immersive virtual reality-based cognitive remediation for adults with psychosocial disabilities: A systematic scoping review of methods intervention gaps and meta-analysis of published effectiveness studies. International Journal of Environmental Research and Public Health, 20(2), 1527. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Reeder, C., Huddy, V., Cella, M., Taylor, R., Greenwood, K., Landau, S., & Wykes, T. (2017). A new generation computerised metacognitive cognitive remediation programme for schizophrenia (CIRCuiTS): A randomised controlled trial. Psychological Medicine, 47(15), 2720–2730. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Samamé, C. (2024). When wrong is assumed right: A response to vieta. Psychological Medicine, 54(12), 3567–3568. [Google Scholar] [CrossRef]
- Samamé, C., Durante, P., Cattaneo, B., Aprahamian, I., & Strejilevich, S. (2023). Efficacy of cognitive remediation in bipolar disorder: Systematic review and meta-analysis of randomized controlled trials. Psychological Medicine, 53(12), 5361–5373. [Google Scholar] [CrossRef] [PubMed]
- Saxena, A., Paredes-Echeverri, S., Michaelis, R., Popkirov, S., & Perez, D. L. (2022). Using the biopsychosocial model to guide patient-centered neurological treatments. Seminars in Neurology, 42(02), 080–087. [Google Scholar] [CrossRef]
- Scarpina, F., D’Aniello, G. E., Mauro, A., Castelnuovo, G., & MacPherson, S. E. (2015). How many segments are there in an orange: Normative data for the new Cognitive Estimation Task in an Italian population. Neurological Sciences, 36(10), 1889–1895. [Google Scholar] [CrossRef] [PubMed]
- Skivington, K., Matthews, L., Simpson, S. A., Craig, P., Baird, J., Blazeby, J. M., Boyd, K. A., Craig, N., French, D. P., McIntosh, E., Petticrew, M., Rycroft-Malone, J., White, M., & Moore, L. (2021). A new framework for developing and evaluating complex interventions: Update of Medical Research Council guidance. BMJ, 374, n2061. [Google Scholar] [CrossRef]
- Spinnler, H., & Tognoni, G. (1987). Standardizzazione e taratura italiana di test neuropsicologici. Italian Journal of Neurological Sciences, 6, 21–120. [Google Scholar]
- Strawbridge, R., Tsapekos, D., Hodsoll, J., Mantingh, T., Yalin, N., McCrone, P., Boadu, J., Macritchie, K., Cella, M., Reeder, C., Fish, J., Wykes, T., & Young, A. H. (2021). Cognitive remediation therapy for patients with bipolar disorder: A randomised proof-of-concept trial. Bipolar Disorders, 23(2), 196–208. [Google Scholar] [CrossRef]
- Torrent, C., Bonnin, C. D. M., Martínez-Arán, A., Valle, J., Amann, B. L., González-Pinto, A., Crespo, J. M., Ibáñez, Á., Garcia-Portilla, M. P., Tabarés-Seisdedos, R., Arango, C., Colom, F., Solé, B., Pacchiarotti, I., Rosa, A. R., Ayuso-Mateos, J. L., Anaya, C., Fernández, P., Landín-Romero, R., … Vieta, E. (2013). Efficacy of functional remediation in bipolar disorder: A multicenter randomized controlled study. The American Journal of Psychiatry, 170(8), 852–859. [Google Scholar] [CrossRef]
- Tsapekos, D., Strawbridge, R., Cella, M., Young, A. H., & Wykes, T. (2023). Does cognitive improvement translate into functional changes? Exploring the transfer mechanisms of cognitive remediation therapy for euthymic people with bipolar disorder. Psychological Medicine, 53(3), 936–944. [Google Scholar] [CrossRef] [PubMed]
- Tsapekos, D., Strawbridge, R., Wykes, T., Young, A. H., & Cella, M. (2022). Cognitive remediation for people with bipolar disorder: The contribution of session attendance and therapy components to cognitive and functional outcomes. Journal of Psychiatric Research, 152, 144–151. [Google Scholar] [CrossRef] [PubMed]
- Valmaggia, L. (2017). The use of virtual reality in psychosis research and treatment. World Psychiatry, 16(3), 246–247. [Google Scholar] [CrossRef]
- Vieta, E., Berk, M., Schulze, T. G., Carvalho, A. F., Suppes, T., Calabrese, J. R., Gao, K., Miskowiak, K. W., & Grande, I. (2018). Bipolar disorders. Nature Reviews Disease Primers, 4(1), 18008. [Google Scholar] [CrossRef] [PubMed]
- Vinogradov, S., Fisher, M., & de Villers-Sidani, E. (2012). Cognitive training for impaired neural systems in neuropsychiatric illness. Neuropsychopharmacology, 37(1), 43–76. [Google Scholar] [CrossRef]
- Vita, A., Barlati, S., Ceraso, A., Nibbio, G., Ariu, C., Deste, G., & Wykes, T. (2021). Effectiveness, core elements, and moderators of response of cognitive remediation for schizophrenia: A systematic review and meta-analysis of randomized clinical trials. JAMA Psychiatry, 78(8), 848–858. [Google Scholar] [CrossRef]
- Whiteford, H. A., Degenhardt, L., Rehm, J., Baxter, A. J., Ferrari, A. J., Erskine, H. E., Charlson, F. J., Norman, R. E., Flaxman, A. D., Johns, N., Burstein, R., Murray, C. J., & Vos, T. (2013). Global burden of disease attributable to mental and substance use disorders: Findings from the Global Burden of Disease Study 2010. The Lancet, 382(9904), 1575–1586. [Google Scholar] [CrossRef] [PubMed]
- World Medical Association. (2013). World medical association declaration of helsinki: Ethical principles for medical research involving human subjects. JAMA, 310(20), 2191–2194. [Google Scholar] [CrossRef] [PubMed]
- Wykes, T., Huddy, V., Cellard, C., McGurk, S. R., & Czobor, P. (2011). A meta-analysis of cognitive remediation for schizophrenia: Methodology and effect sizes. American Journal of Psychiatry, 168(5), 472–485. [Google Scholar] [CrossRef]
- Zhu, X., Fan, H., Zou, Y., Tan, Y., Yang, F., Wang, Z., Zhao, Y., Fan, F., Reeder, C., Zhou, D., Tan, S., & Wykes, T. (2022). Computerized or manual? Long term effects of cognitive remediation on schizophrenia. Schizophrenia Research, 239, 47–54. [Google Scholar] [CrossRef] [PubMed]
| VR/CR GROUP (N = 36) | ||||
|---|---|---|---|---|
| Test | T0 | T1 | T2 | T3 |
| Fig. Rey Immediate (Vis. Sp.) | 29.04 ± 8.60 | 30.68 ± 6.88 | 28.11 ± 9.13 | 28.83 ± 8.73 |
| Matrix (Attent.) | 1.94 ± 1.37 | 2.36 ± 1.47 | 1.94 ± 1.41 | 1.88 ± 1.40 |
| Digit Span Forward (Attent.) | 2.86 ± 1.47 | 2.75 ± 1.50 | 2.66 ± 1.53 | 2.75 ± 1.46 |
| Rey’s Words Immediate (Attent.) | 2.38 ± 1.62 | 3.02 ± 1.50 | 2.66 ± 1.80 | 2.72 ± 1.75 |
| TMT-A (Attent.) | 2.88 ± 1.21 | 3.02 ± 1.42 | 3.11 ± 1.18 | 3.16 ± 1.20 |
| Rey’s Words Delayed (Memory) | 2.25 ± 1.57 | 2.89 ± 1.55 | 2.70 ± 1.72 | 2.75 ± 1.67 |
| Digit Span Backward (Memory) | 1.97 ± 1.64 | 2.16 ± 1.68 | 2.15 ± 1.52 | 2.61 ± 1.49 |
| Test of Tale (Memory) | 2.16 ± 1.44 | 2.77 ± 1.17 | 2.25 ± 1.15 | 2.52 ± 1.18 |
| Verbal Phonological Test (Leng.) | 2.63 ± 1.43 | 3.05 ± 1.28 | 3.13 ± 1.37 | 3.11 ± 1.42 |
| Verbal Semantic Test (Leng.) | 2.63 ± 1.31 | 3.22 ± 1.14 | 2.97 ± 1.34 | 2.97 ± 1.34 |
| Substit. Digit Symbol (Ex. Fun.) | 35.9 ± 13.97 | 38.55 ± 11.89 | 37.81 ± 14.45 | 38.56 ± 14.71 |
| TMT-B (Ex. Fun.) | 2.91 ± 1.29 | 3.02 ± 1.20 | 3.08 ± 1.36 | 3.02 ± 1.34 |
| Stroop Test Time (Ex. Fun.) | 2.61 ± 1.60 | 2.94 ± 1.45 | 2.83 ± 1.59 | 2.75 ± 1.61 |
| FAB (Ex. Fun.) | 15.0 ± 3.20 | 15.58 ± 2.66 | 15.27 ± 2.95 | 15.30 ± 2.92 |
| Cognitive Estimation Test (Ex. Fun.) | 1.94 ± 1.47 | 2.80 ± 1.09 | 1.88 ± 1.36 | 1.88 ± 1.34 |
| Test | χ² | p |
|---|---|---|
| Fig. Rey Immediate (Vis. Sp.) | 10.61 | 0.01 |
| Matrix (Attent.) | 5.15 | 0.16 |
| Digit Span Forward (Attent.) | 0.12 | 0.98 |
| Rey’s Words Immediate (Attent.) | 6.12 | 0.10 |
| TMT-A (Attent.) | 2.77 | 0.42 |
| Ray’s Words Delayed (Memory) | 7.10 | 0.06 |
| Digit Span Backward (Memory) | 4.50 | 0.21 |
| Test of Tale (Memory) | 3.68 | 0.29 |
| Verbal Phonological Test (Language) | 9.10 | 0.02 |
| Verbal Semantic Test (Language) | 9.22 | 0.02 |
| Substit. Digit Symbol (Ex. Fun.) | 0.66 | 0.88 |
| TMT-B (Ex. Fun.) | 2.20 | 0.53 |
| Stroop Test Time (Ex. Fun.) | 1.35 | 0.71 |
| FAB (Ex. Fun.) | 1.09 | 0.77 |
| Cognitive Estimation Test (Ex. Fun.) | 16.47 | 0.00 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Perra, A.; Carta, M.G.; Primavera, D.; Cossu, G.; Locci, A.; Zaccheddu, R.; Piludu, F.; Galetti, A.; Preti, A.; De Lorenzo, V.; et al. An Integrated Cognitive Remediation and Recovery-Oriented Program for Individuals with Bipolar Disorder Using a Virtual Reality-Based Intervention: 6- and 12-Month Cognitive Outcomes from a Randomized Feasibility Trial. Behav. Sci. 2025, 15, 452. https://doi.org/10.3390/bs15040452
Perra A, Carta MG, Primavera D, Cossu G, Locci A, Zaccheddu R, Piludu F, Galetti A, Preti A, De Lorenzo V, et al. An Integrated Cognitive Remediation and Recovery-Oriented Program for Individuals with Bipolar Disorder Using a Virtual Reality-Based Intervention: 6- and 12-Month Cognitive Outcomes from a Randomized Feasibility Trial. Behavioral Sciences. 2025; 15(4):452. https://doi.org/10.3390/bs15040452
Chicago/Turabian StylePerra, Alessandra, Mauro Giovanni Carta, Diego Primavera, Giulia Cossu, Aurora Locci, Rosanna Zaccheddu, Federica Piludu, Alessia Galetti, Antonio Preti, Valerio De Lorenzo, and et al. 2025. "An Integrated Cognitive Remediation and Recovery-Oriented Program for Individuals with Bipolar Disorder Using a Virtual Reality-Based Intervention: 6- and 12-Month Cognitive Outcomes from a Randomized Feasibility Trial" Behavioral Sciences 15, no. 4: 452. https://doi.org/10.3390/bs15040452
APA StylePerra, A., Carta, M. G., Primavera, D., Cossu, G., Locci, A., Zaccheddu, R., Piludu, F., Galetti, A., Preti, A., De Lorenzo, V., Di Natale, L., Machado, S., Nardi, A. E., & Sancassiani, F. (2025). An Integrated Cognitive Remediation and Recovery-Oriented Program for Individuals with Bipolar Disorder Using a Virtual Reality-Based Intervention: 6- and 12-Month Cognitive Outcomes from a Randomized Feasibility Trial. Behavioral Sciences, 15(4), 452. https://doi.org/10.3390/bs15040452










