Parasomnias in Post-Secondary Students: Prevalence, Distress, and Coping Strategies
Abstract
1. Introduction
1.1. REM and NREM Parasomnias
1.2. Causes and Consequences
1.3. Prevalence
1.4. Present Study
- (1)
- Over 70% of students would report at least one parasomnia during the past year;
- (2)
- Most students would report two or more types of parasomnias;
- (3)
- Nightmare disorder would be the most prevalent parasomnia reported.
- (4)
- Investigating students’ distress levels related to specific parasomnias;
- (5)
- Identifying their coping strategies for each parasomnia;
- (6)
- Exploring the co-occurrence of different parasomnias in this population.
2. Materials and Methods
2.1. Participants
2.2. Measures
2.2.1. Demographics
2.2.2. Munich Parasomnia Screening Questionnaire (MUPS)
2.3. Procedure
3. Results
3.1. One Year Prevalence
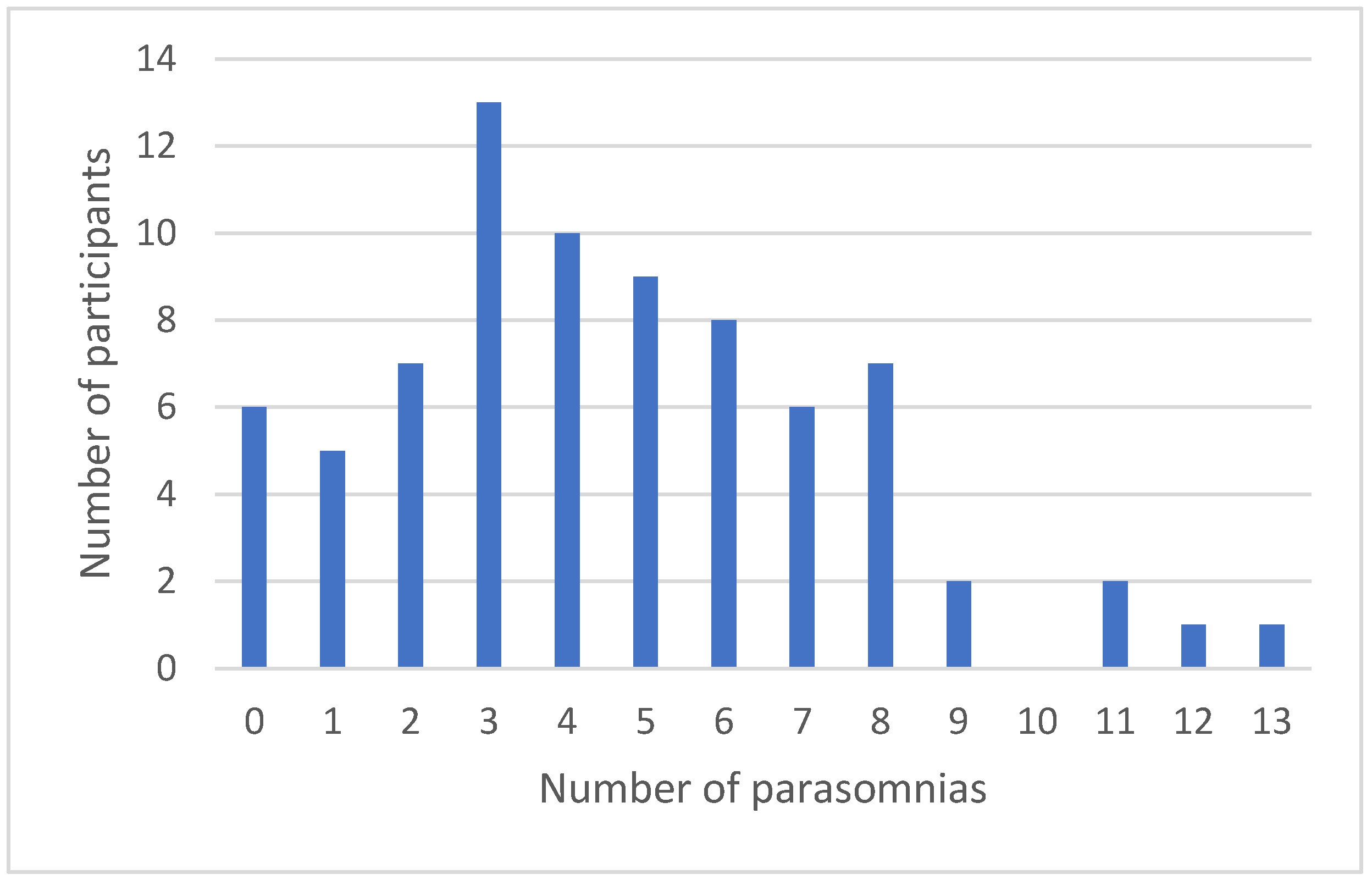
3.2. Number of Parasomnias Experienced
3.3. How Disturbing Is Each Parasomnia?
3.4. Coping Strategies
3.5. Which Parasomnias Tend to Occur Together?
4. Discussion
4.1. Relative Co-Occurrence
4.2. Parasomnia Frequency, Disturbance and Distress Aspects
4.3. How Do Students Cope with Disturbing/Distressing Parasomnias?
4.4. Developmental and Age-Related Considerations
5. Limitations
6. Conclusions and Implications
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Parasomnia Label in Alphabetical Order | MUPS Questionnaire Items and Order of Presentation |
|---|---|
| Confusional arousals | 17. Upon waking, completely confused/difficult orientation/slowed speech |
| Exploding head syndrome | 4. When falling asleep or waking, perceiving a loud bang, a sound similar to a bang (e.g., door bang), or having the sensation of an “explosion in the head.” |
| Hypnagogic/hypnopompic hallucinations | 5. Auditory or visual illusions that accompany falling asleep or waking in a distressing or threatening manner (e.g., hearing sounds or voices, or seeing people or things that are not in the room) |
| Hypnic jerks | 1. Leg or body twitches that occur suddenly and unintentionally when falling asleep, often with the sensation of falling |
| Nightmares | 13. Frightening dreams and nightmares |
| Nocturnal eating | 15. Waking again after falling asleep in order to eat something |
| Nocturnal leg cramps | 7. Night-time cramps in the calves |
| Periodic twitching and kicking while asleep * Periodic leg movements | 6. Repeated involuntary twitching of the legs or kicking during sleep (can only be observed by another person) |
| REM sleep behavior disorder | 21. Have you ever actually done what you dreamt (e.g., gesticulating or lashing about)? |
| Rhythmic leg movements while falling asleep | 2. While falling asleep or while half asleep, rhythmic and rapid leg movements that can also occur intentionally |
| * Rhythmic feet movements | |
| Rhythmic movement disorder | 3. Rhythmic and repeated movements of the head or body when falling asleep or during night-time wake periods, e.g., nodding, rocking or swaying yourself to sleep |
| Sleep enuresis | 12. Wetting oneself during sleep |
| Sleep paralysis | 18. Waking with a paralysis of the whole body (not including eyes and breathing) that can last for several seconds |
| Sleep-related abnormal choking/suffocating | 10. Choking or suffocating during sleep, or waking with the feeling of choking or suffocating |
| * Sleep-related abnormal swallowing | |
| Sleep-related bruxism | 8. Teeth grinding during the night |
| Sleep-related eating | 16. While asleep, eating something or preparing a meal that can have unusual or inedible ingredients (e.g., ice-cream and cheese, washing-up liquid instead of butter) |
| Sleep-related groaning | 11. Loud and repeated sighing and moaning during sleep |
| Sleep talking | 9. Talking during sleep |
| Sleep terrors | 14. Waking with severe anxiety and, possibly, screaming, with no recollection of a dream |
| Sleep walking | 19. Sleepwalking or sitting up while still asleep without leaving the bed |
| Violent behavior | 20. Have you ever thrashed around, hitting or kicking? |
Appendix B

Appendix C
References
- Singh, S.; Kaur, H.; Shivank, S.; Imran, K. Parasomnias: A comprehensive review. Cureus 2018, 10, e3807. [Google Scholar] [CrossRef] [PubMed]
- Irfan, M.; Schenck, C.H.; Howell, M.J. NonREM disorders of arousal and related parasomnias: An updated review. Neurotherapeutics 2021, 18, 124–139. [Google Scholar] [CrossRef] [PubMed]
- American Academy of Sleep Medicine. ICSD-3 (International Classification of Sleep Disorders—Third Edition); American Academy of Sleep Medicine: Darien, IL, USA, 2014. [Google Scholar]
- Fulda, S.; Hornyak, M.; Müller, K.; Cerny, L.; Beitinger, P.A.; Wetter, T.C. Development and validation of the Munich Parasomnia Screening (MUPS): A questionnaire for parasomnias and nocturnal behaviors. Somnologie 2008, 12, 56–65. [Google Scholar] [CrossRef]
- Sateia, M.J. International classification of sleep disorders-third edition: Highlights and modifications. Chest 2014, 146, 1387–1394. [Google Scholar] [CrossRef]
- Stieglitz, S.; Heppner, H.J.; Netzer, N. Abnormal things happening during sleep: Parasomnias. Z. Gerontol. Geriatr. 2020, 53, 119–122. [Google Scholar] [CrossRef]
- Bruni, O.; Miano, S. Parasomnias. In Pediatric Sleep Medicine: Mechanisms and Comprehensive Guide to Clinical Evaluation and Management; Gozal, D., Kheirandish-Gozal, L., Eds.; Springer: Cham, Switzerland, 2021; pp. 415–429. [Google Scholar] [CrossRef]
- Fleetham, J.A.; Fleming, J.A.E. Parasomnias. Can. Med. Assoc. J. 2014, 186, E273–E280. [Google Scholar] [CrossRef] [PubMed]
- Ariza-Serrano, J.; Santana-Vargas, D.; Millan-Rosas, G.; Santana-Miranda, R.; Rosenthal, L.; Poblano, A. Parasomnias related to shift work disorder among medical residents during the first year of training in Mexico. Sleep Biol. Rhythm. 2023, 21, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Matsui, K.; Komada, Y.; Nishimura, K.; Kuriyama, K.; Inoue, Y. Prevalence and associated factors of nocturnal eating behavior and sleep-related eating disorder-like behavior in Japanese young adults: Results of an internet survey using Munich parasomnia screening. J. Clin. Med. 2020, 9, 1243. [Google Scholar] [CrossRef]
- Alshahrani, S.M.; Albrahim, R.A.; Abukhlaled, J.K.; Aloufi, L.H.; Aldharman, S.S.; Albrahim, R.; Aloufi, L. Parasomnias and associated factors among university students: A Cross-sectional study in Saudi Arabia. Cureus 2023, 15, e48722. [Google Scholar] [CrossRef]
- Loddo, G.; Lopez, R.; Cilea, R.; Dauvilliers, Y.; Provini, F. Disorders of arousal in adults: New diagnostic tools for clinical practice. Sleep Sci. Pract. 2019, 3, 5. [Google Scholar] [CrossRef]
- Oluwole, O.S.A. Lifetime prevalence and incidence of parasomnias in a population of young adult Nigerians. J. Neurol. 2010, 257, 1141–1147. [Google Scholar] [CrossRef] [PubMed]
- Kirwan, E.; Fortune, D.G. Exploding head syndrome, chronotype, parasomnias and mental health in young adults. J. Sleep Res. 2021, 30, e13044. [Google Scholar] [CrossRef] [PubMed]
- Heinzer, R. (Centre d’investigation et de recherche sur le sommeil (CIRS), CHUV, BH 06, 1011 Lausanne, Switzerland), personal communication, 26 June 2023.
- McGill IT Services. LimeSurvey 3: User Guide to Creating Surveys; McGill University: Montreal, QC, Canada, 2020; Available online: https://webforms.mcgill.ca/KB-downloads/LimeSurvey/limesurvey-v3-userguide.pdf (accessed on 20 July 2024).
- Jorgensen, M.; Qin, Y.; Vasseur, A.; Zlotea, B.; Liao, H. Coping Strategies for Parasomnias [Coding Manual]; Adaptech Research Network: Montreal, QC, Canada, 2024; Available online: https://adaptech.org/wp-content/uploads/Latest-DraftCodingManualFebruary282024FINAL-1.xlsx (accessed on 20 July 2024).
- Holland, K. Causes of Bed-Wetting in Adults and How to Treat It. Healthline, 26 October 2018. Available online: https://www.healthline.com/health/adult-bed-wetting (accessed on 20 July 2024).
- Pacheco, D.; Troung, K. REM Sleep Behavior Disorder. Sleep Foundation, 18 July 2023. Available online: https://www.sleepfoundation.org/parasomnias/rem-sleep-behavior-disorder (accessed on 20 July 2024).
- de Martin Truzzi, G.; Frange, C.; Santos Coelho, F.M. Parasomnias. In Sleep Medicine and Physical Therapy; Frange, C., Coelho, F.M.S., Eds.; Springer: Berlin/Heidelberg, Germany, 2022; pp. 239–244. [Google Scholar] [CrossRef]
- Nevsimalova, S.; Prihodova, I.; Kemlink, D.; Skibova, J. Childhood parasomnia—A disorder of sleep maturation? Eur. J. Paediatr. Neurol. 2013, 17, 615–619. [Google Scholar] [CrossRef]
- Montplaisir, J.; Zadra, A.; Nielsen, T.; Petit, D. Parasomnias. In Sleep Disorders Medicine; Chokroverty, S., Ed.; Springer: New York, NY, USA, 2017; pp. 1087–1113. [Google Scholar] [CrossRef]
- Stefani, A.; Högl, B. Diagnostic criteria, differential diagnosis, and treatment of minor motor activity and less well-known movement disorders of sleep. Curr. Treat. Options Neurol. 2019, 21, 1. [Google Scholar] [CrossRef]
- Li, S.X.; Zhang, B.; Li, A.M.; Wing, Y.K. Prevalence and correlates of frequent nightmares: A community-based 2-phase study. Sleep 2010, 33, 774–780. [Google Scholar] [CrossRef] [PubMed]
- Nadorff, M.R.; Nadorff, D.K.; Germain, A. Nightmares: Under-reported, undetected, and therefore untreated. J. Clin. Sleep Med. 2015, 11, 747–750. [Google Scholar] [CrossRef]
- Libman, E.; Fichten, C.; Creti, L.; Bailes, S. Parasomnias and Other Negative Sleep Related Phenomena among Post-Secondary Students with and without Disabilities [Invited Speakers]. In Proceedings of the Psychosocial Rounds at the Jewish General Hospital, Montreal, QC, Canada, 5 September 2023. [Google Scholar]
- Khan, I.; Slowik, J.M. Exploding Head Syndrome. Europe PMC 12 December 2022. Available online: https://europepmc.org/article/nbk/nbk560817 (accessed on 20 July 2024).
- Nakayama, M.; Nakano, N.; Mihara, T.; Arima, S.; Sato, S.; Kabaya, K.; Suzuki, M.; Kitahara, T. Two cases of exploding head syndrome documented by polysomnography that improved after treatment. J. Clin. Sleep Med. 2021, 17, 103–106. [Google Scholar] [CrossRef]
- Puledda, F.; Moreno-Ajona, D.; Goadsby, P.J. Exploding head syndrome (a.k.a episodic cranial sensory shock) responds to single-pulse transcranial magnetic stimulation. Eur. J. Neurol. 2021, 28, 1432–1433. [Google Scholar] [CrossRef]
- Whitney, R.; Weiss, S.K. Sleep-related movement disorders: Hypnic jerks. Curr. Sleep Med. Rep. 2018, 4, 19–27. [Google Scholar] [CrossRef]
- Kumar, R.; Ali, S.N.; Saha, S.; Bhattacharjee, S. SSRI induced hypnic jerks: A case series. Indian J. Psychiatry 2023, 65, 785–788. [Google Scholar] [CrossRef]
- Summer, J.; DeBanto, J. Hypnic Jerks. Sleep Foundation, 1 August 2023. Available online: https://www.sleepfoundation.org/parasomnias/hypnic-jerks (accessed on 20 July 2024).
- Cleveland Clinic. Nightmare Disorder. 21 November 2022. Available online: https://my.clevelandclinic.org/health/diseases/24464-nightmare-disorder (accessed on 20 July 2024).
- Gieselmann, H.; Aoudia, M.A.; Carr, M.; Germain, A.; Gorzka, R.; Holzinger, B.; Kleim, B.; Krakow, B.; Kunze, A.E.; Lancee, J.; et al. Aetiology and treatment of nightmare disorder: State of the art and future perspectives. J. Sleep Res. 2019, 28, e12820. [Google Scholar] [CrossRef] [PubMed]
- Cho, J.; Lee, J.H.; Hong, S.C. Sleep-related eating disorder and nocturnal eating syndrome. Sleep Med. Res. 2020, 11, 65–69. [Google Scholar] [CrossRef]
- McMillen, M. Nocturnal Leg Cramps. WebMD. 3 March 2022. Available online: https://www.webmd.com/sleep-disorders/leg-cramps (accessed on 20 July 2024).
- Akhavizadegan, H.; Locke, J.A.; Stothers, L.; Kavanagh, A. A comprehensive review of adult enuresis. Can. J. Urol. 2019, 13, 282–287. [Google Scholar] [CrossRef]
- Cleveland Clinic. Sleep Paralysis. 18 October 2021. Available online: https://my.clevelandclinic.org/health/diseases/21974-sleep-paralysis (accessed on 20 July 2024).
- Sharpless, B.A. A clinician’s guide to recurrent isolated sleep paralysis. Neuropsychiatr. Dis. Treat. 2016, 12, 1761–1767. [Google Scholar] [CrossRef] [PubMed]
- Suni, E.; Dimitriu, A. Sleep Talking. Sleep Foundation, 18 July 2023. Available online: https://www.sleepfoundation.org/parasomnias/sleep-talking (accessed on 20 July 2024).
- Foxx, R. Fighting Fright: How Adults Can Manage Night Terrors. Doctors Health Press. 3 November 2015. Available online: https://www.doctorshealthpress.com/fighting-fright-how-adults-can-manage-night-terrors/ (accessed on 20 July 2024).
- Turan, H.S.; Gündüz, N.; Polat, A.; Tural, U. Treatment approach to sleep terror: Two case reports. Noro. Psikiyatr. Ars. 2015, 52, 204–206. [Google Scholar] [CrossRef][Green Version]
- Higuera, V. Choking on Saliva Causes and Treatments. Healthline, 8 March 2019. Available online: https://www.healthline.com/health/choking-on-saliva (accessed on 20 July 2024).
- Suni, E.; Truong, K. How to Stop Grinding Teeth: Effective Prevention Strategies. Sleep Foundation, 16 January 2024. Available online: https://www.sleepfoundation.org/bruxism/tips (accessed on 20 July 2024).
| Name of Parasomnia | Description |
|---|---|
| Confusional arousals | Partial awakenings during slow-wave (stage 3) sleep. The individual is confused, disoriented to time and space. |
| Sleepwalking | Ambulatory behavior during slow wave (stage 3) sleep. |
| Sleep-related eating | Recurrent episodes of involuntary binge eating after partial awakening from sleep. |
| Sleep talking | Speaking aloud during slow wave (stage 3) sleep. |
| Sleep terrors | Episodes of intense fear, accompanied by increased autonomic nervous system activity. |
| Name of Parasomnia | Description |
|---|---|
| Nightmares | Repeated occurrence of frightening dreams that lead to awakening. |
| REM sleep behavior disorder | Vivid dreaming (often frightening) without the usual accompanying reduced muscle tone that results in behavioral acting out of the dream content. |
| Sleep paralysis | REM-based reduced skeletal muscle tone perseverates into wakefulness, resulting in the inability of the affected person to move or speak during wakefulness. |
| Name of Parasomnia | Description |
|---|---|
| Exploding head syndrome | Sudden loud noise in the head that occurs during wake-sleep transitions or while awakening in the middle of the night. |
| Sleep enuresis | Involuntary release of urine while sleeping. |
| Sleep-related abnormal choking/suffocating | Swallowing with aspiration during sleep. |
| 1 Parasomnia Label | 2 REM/NREM | 3 Our Data: % with the Parasomnialiwenn = 77 | 3 Kirwan & Fortune [14] % with the Parasomnia |
|---|---|---|---|
| Confusional arousals | NREM | 19% | 30% |
| Exploding head syndrome | Either | 16% | 16% |
| Hypnagogic/hypnopompic hallucinations | Transition | 21% | 41% |
| Hypnic jerks | NREM | 53% | 79% |
| Nightmares | REM | 82% | 74% |
| Nocturnal eating | NREM | 18% | 33% |
| Nocturnal leg cramps | Either | 32% | 44% |
| Periodic twitching and kicking while asleep | NREM | 25% | 28% |
| REM sleep behavior disorder | REM | 14% | 16% |
| Rhythmic leg movements while falling asleep | Transition | 25% | 38% |
| Rhythmic movement disorder | NREM | 13% | 19% |
| Sleep enuresis | Either | 5% | 2% |
| Sleep paralysis | REM | 14% | 15% |
| Sleep-related abnormal choking/suffocating | NREM | 5% | 10% |
| Sleep-related bruxism | Either | 34% | 27% |
| Sleep-related eating | NREM | 0% | 2% |
| Sleep-related groaning | Either | 17% | 26% |
| Sleep talking | NREM | 38% | 58% |
| Sleep terrors | NREM | 17% | 30% |
| Sleep walking | NREM | 4% | 9% |
| Violent behavior | NREM | 8% | 11% |
| Parasomnia Label | Number of Participants Reporting Parasomnia | 1 How Often Do You Have This Parasomnia (Mean: Very Rarely = 2 to Very Often = 6) | How Disturbing/Distressing Was This? | |
|---|---|---|---|---|
| 2 Number of Participants | 3 Mean Disturbance 1–10 | |||
| Confusional arousals | 15 | 3 | 9 | 3.56 |
| Exploding head syndrome | 12 | 3 | 6 | 5.50 |
| Hypnagogic/hypnopompic hallucinations | 16 | 4 | 5 | 4.80 |
| Hypnic jerks | 41 | 3 | 26 | 3.42 |
| Nightmares | 63 | 3 | 41 | 5.56 |
| Nocturnal eating | 14 | 3 | 7 | 4.14 |
| Nocturnal leg cramps | 25 | 4 | 14 | 6.50 |
| Periodic twitching and kicking while asleep | 19 | 3 | 11 | 2.82 |
| REM sleep behavior disorder | 11 | 2 | 4 | 5.25 |
| Rhythmic leg movements while falling asleep | 19 | 3 | 10 | 3.00 |
| Rhythmic movement disorder | 10 | 3 | 7 | 1.86 |
| Sleep enuresis | 4 | 3 | 1 | 8.00 |
| Sleep paralysis | 11 | 3 | 6 | 7.50 |
| Sleep-related abnormal choking/suffocating | 4 | 3 | 3 | 7.33 |
| Sleep-related bruxism | 26 | 3 | 18 | 4.22 |
| Sleep-related eating | 0 | 0 | 0 | 0.00 |
| Sleep-related groaning | 13 | 3 | 5 | 1.40 |
| Sleep talking | 29 | 3 | 13 | 1.69 |
| Sleep terrors | 13 | 3 | 5 | 7.40 |
| Sleepwalking | 3 | 3 | 2 | 1.50 |
| Violent behavior | 6 | 3 | 2 | 2.00 |
| Categories | Examples of Codes |
|---|---|
| Preventative interventions | “Changed the type of content I was looking at before going to sleep.” “Put physical barriers (i.e., cushions or pillows) to prevent me from falling from my bed.” |
| Distraction/shifting focus | “Listen/watch videos to help me feel better.” “I will text my friends.” |
| Grounding strategies | “Take a minute before going back to sleep–breathe, drink some water, calm down.” “So I just try to stay calm in my mind until I muster enough energy to force my body to wake up.” |
| Physical manipulation of body/exercise | “Moved my legs for several minutes until I felt circulation.” “I will straighten my calf and pull my big toe hard.” |
| Other strategies | “I tried to think why I was having unsettling dreams and made a cognitive effort to understand my feelings that were not fully in my conscious awareness.” “I sometimes share my dreams with family or friends.” |
| Coping Responses by a Participant | |||||||
|---|---|---|---|---|---|---|---|
| 1 Parasomnia Labels | Preventative Interventions | Distraction/Shifting Focus | Grounding Strategies | Physical Manipulation of Body/Exercise | Other Strategies | 2 Total Number of Participants Using These Coping Responses | 3 Reported They Did Nothing |
| Confusional arousals | 1 | 4 | 5 | ||||
| Exploding head syndrome | 1 | 1 | 2 | 4 | 1 | ||
| Hypnagogic/hypnopompic hallucinations | 1 | 1 | 3 | ||||
| Hypnic jerks | 2 | 1 | 3 | 16 | |||
| Nightmares | 4 | 5 | 6 | 4 | 19 | 11 | |
| Nocturnal eating | 2 | 4 | 2 | 8 | 2 | ||
| Nocturnal leg cramps | 6 | 6 | 4 | ||||
| Periodic twitching and kicking while asleep | 1 | 1 | 4 | ||||
| REM sleep behavior disorder | 1 | 1 | 1 | ||||
| Rhythmic leg movements while falling asleep | 0 | 3 | |||||
| Rhythmic movement disorder | 1 | 1 | 2 | 2 | |||
| 4 Sleep enuresis | |||||||
| Sleep paralysis | 3 | 2 | 1 | 6 | 2 | ||
| Sleep-related abnormal choking/suffocating | 1 | 1 | |||||
| Sleep-related bruxism | 7 | 2 | 3 | 12 | 6 | ||
| 4 Sleep-related eating | |||||||
| Sleep-related groaning | 0 | 1 | |||||
| Sleep talking | 0 | 4 | |||||
| Sleep terrors | 1 | 1 | 2 | ||||
| Sleep walking | 0 | 1 | |||||
| Violent behavior | 1 | 1 | |||||
| Total number of codes | 19 | 8 | 23 | 12 | 10 | 72 | 61 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fichten, C.S.; Libman, E.; Bailes, S.; Jorgensen, M.; Havel, A.; Qin, Y.; Creti, L.; Liao, H.; Zlotea, B.; Vo, C.; et al. Parasomnias in Post-Secondary Students: Prevalence, Distress, and Coping Strategies. Behav. Sci. 2024, 14, 646. https://doi.org/10.3390/bs14080646
Fichten CS, Libman E, Bailes S, Jorgensen M, Havel A, Qin Y, Creti L, Liao H, Zlotea B, Vo C, et al. Parasomnias in Post-Secondary Students: Prevalence, Distress, and Coping Strategies. Behavioral Sciences. 2024; 14(8):646. https://doi.org/10.3390/bs14080646
Chicago/Turabian StyleFichten, Catherine S., Eva Libman, Sally Bailes, Mary Jorgensen, Alice Havel, Yuxuan Qin, Laura Creti, Huanan Liao, Bianca Zlotea, Christine Vo, and et al. 2024. "Parasomnias in Post-Secondary Students: Prevalence, Distress, and Coping Strategies" Behavioral Sciences 14, no. 8: 646. https://doi.org/10.3390/bs14080646
APA StyleFichten, C. S., Libman, E., Bailes, S., Jorgensen, M., Havel, A., Qin, Y., Creti, L., Liao, H., Zlotea, B., Vo, C., Budd, J., Vasseur, A., Pierre-Sindor, T., & Costin, G. (2024). Parasomnias in Post-Secondary Students: Prevalence, Distress, and Coping Strategies. Behavioral Sciences, 14(8), 646. https://doi.org/10.3390/bs14080646






