Incremental Validity of Trait Impulsivity, Dysfunctional Emotional Regulation, and Affect Lability in the Predictions of Attention Deficit Hyperactivity Disorder and Oppositional Defiant Disorder Symptoms in Adults
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Measures
2.3. Current Symptom Scale [35]
2.4. Short-Urgency-Premeditation-Perseverance-Sensation Seeking- Positive Urgency scale (S-UPPS-P) [36]
2.5. The Affect Liability Scale-18 (ALS-18) [37]
2.6. Difficulties in Emotional Regulation Strategies-36
2.7. Procedure
2.8. Statistical Analysis
3. Results
3.1. Descriptives and Correlations of Study Variables
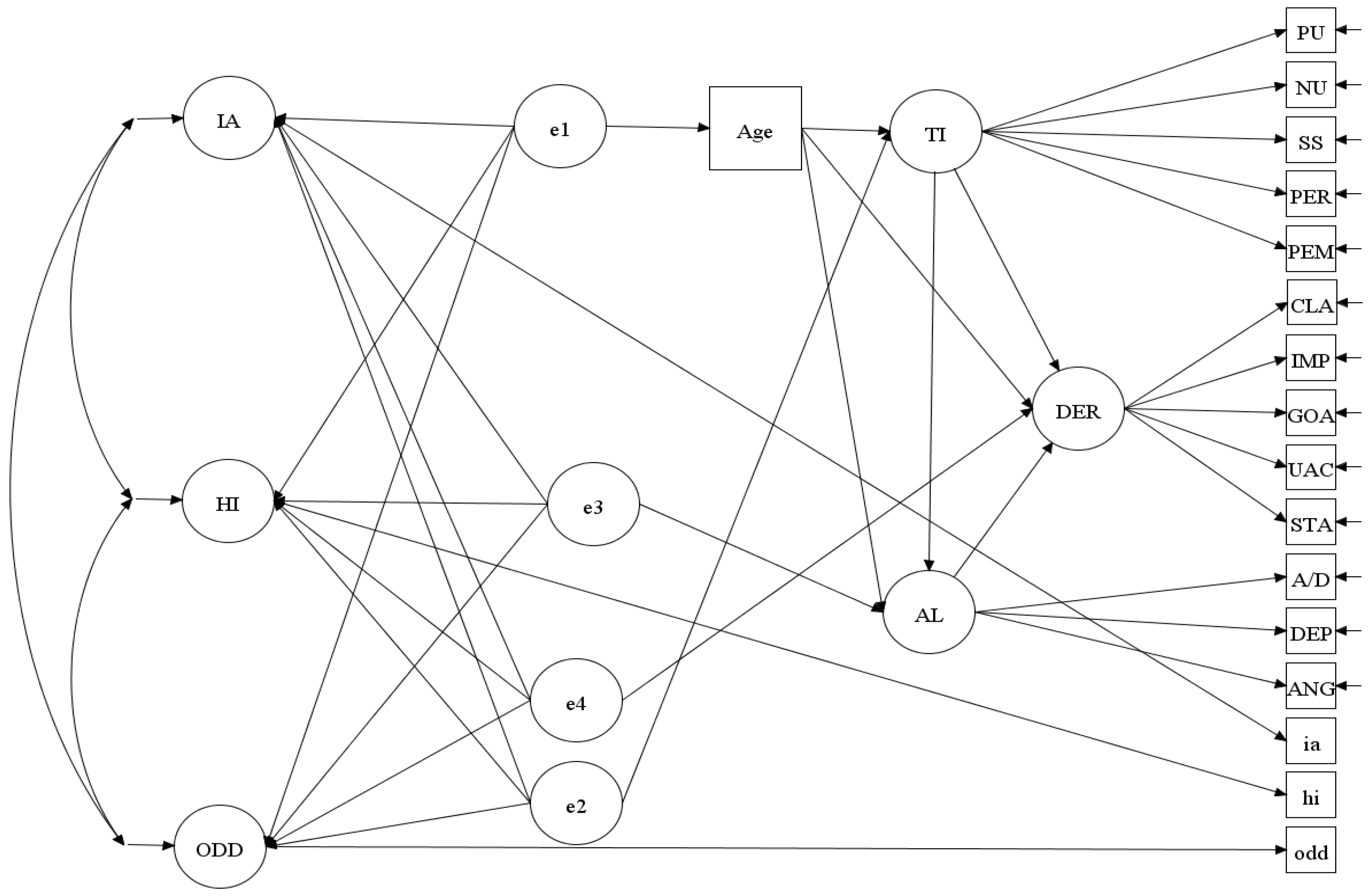
3.2. Factor Structure
3.3. Incremental Validity
3.3.1. Incremental Validity Analysis 1
3.3.2. Incremental Validity Analysis 2
4. Discussion
4.1. Practical Implications for Assessment and Treatment
4.2. Summary and Conclusions
Limitations
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; text revision; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Beauchaine, T.P.; Zisner, A.R.; Sauder, C.L. Trait impulsivity and the externalizing spectrum. Annu. Rev. Clin. Psychol. 2017, 13, 343–368. [Google Scholar] [CrossRef] [PubMed]
- Barkley, R.A.; Fischer, M. The unique contribution of emotional impulsiveness to impairment in major life activities in hyperactive children as adults. J. Am. Acad. Child Adolesc. Psychiatry 2010, 49, 503–513. [Google Scholar] [PubMed]
- Beheshti, A.; Chavanon, M.L.; Schneider, S.; Christiansen, H. ADHD overdiagnosis and the role of patient gender among Iranian psychiatrists. BMC Psychiatry 2021, 21, 514. [Google Scholar] [CrossRef] [PubMed]
- Nigg, J.T.; Goldsmith, H.H.; Sachek, J. Temperament and attention deficit hyperactivity disorder: The development of a multiple pathway model. J. Clin. Child Adolesc. Psychol. 2004, 33, 42–53. [Google Scholar] [CrossRef] [PubMed]
- Retz, W.; Stieglitz, R.D.; Corbisiero, S.; Retz-Junginger, P.; Rösler, M. Emotional dysregulation in adult ADHD: What is the empirical evidence? Expert Rev. Neurother. 2012, 12, 1241–1251. [Google Scholar] [CrossRef] [PubMed]
- Hirsch, O.; Chavanon, M.; Riechmann, E.; Christiansen, H. Emotional dysregulation is a primary symptom in adult Attention-Deficit/Hyperactivity Disorder (ADHD). J. Affect. Disord. 2018, 232, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Skirrow, C.; Asherson, P. Emotional lability, comorbidity and impairment in adults with attention-deficit hyperactivity disorder. J. Affect. Disord. 2013, 147, 80–86. [Google Scholar] [CrossRef] [PubMed]
- Surman, C.B.; Biederman, J.; Spencer, T.; Miller, C.A.; McDermott, K.M.; Faraone, S.V. Understanding deficient emotional self-regulation in adults with attention deficit hyperactivity disorder: A controlled study. ADHD Atten. Deficit Hyperact. Disord. 2013, 5, 273–281. [Google Scholar] [CrossRef] [PubMed]
- Cavanagh, M.; Quinn, D.; Duncan, D.; Graham, T.; Balbuena, L. Oppositional defiant disorder is better conceptualized as a disorder of emotional regulation. J. Atten. Disord. 2017, 21, 381–389. [Google Scholar] [CrossRef]
- Martel, M.M.; Von Eye, A.; Nigg, J. Developmental differences in structure of attention-deficit/hyperactivity disorder (ADHD) between childhood and adulthood. Int. J. Behav. Dev. 2012, 36, 279–292. [Google Scholar] [CrossRef]
- Mitchison, G.M.; Njardvik, U. Prevalence and gender differences of ODD, anxiety, and depression in a sample of children with ADHD. J. Atten. Disord. 2019, 23, 1339–1345. [Google Scholar] [CrossRef] [PubMed]
- Shaw, P.; Stringaris, A.; Nigg, J.; Leibenluft, E. Emotion dysregulation in attention deficit hyperactivity disorder. Am. J. Psychiatry 2014, 171, 276–293. [Google Scholar] [CrossRef] [PubMed]
- Beauchaine, T.P.; McNulty, T. Comorbidities and continuities as ontogenic processes: Toward a developmental spectrum model of externalizing psychopathology. Dev. Psychopathol. 2013, 25 Pt 2, 1505–1528. [Google Scholar] [CrossRef] [PubMed]
- Hart, E.L.; Lahey, B.B.; Loeber, R.; Applegate, B.; Frick, P.J. Developmental change in attention-deficit hyperactivity disorder in boys: A four-year longitudinal study. J. Abnorm. Child Psychol. 1995, 23, 729–749. [Google Scholar] [CrossRef] [PubMed]
- Beauchaine, T.P.; Hinshaw, S.P.; Pang, K.L. Comorbidity of attention-deficit/hyperactivity disorder and early-onset conduct disorder: Biological, environmental, and developmental mechanisms. Clin. Psychol. Sci. Pract. 2010, 17, 327. [Google Scholar] [CrossRef]
- Beauchaine, T.P.; Constantino, J.N. Redefining the endophenotype concept to accommodate transdiagnostic vulnerabilities and etiological complexity. Biomark. Med. 2017, 11, 769–780. [Google Scholar] [CrossRef] [PubMed]
- Thompson, R.A. Emotion regulation: A theme in search of definition. Monogr. Soc. Res. Child Dev. 1994, 59, 25–52. [Google Scholar] [CrossRef] [PubMed]
- Graziano, P.A.; Garcia, A. Attention-deficit hyperactivity disorder and children’s emotion dysregulation: A meta-analysis. Clin. Psychol. Rev. 2016, 46, 106–123. [Google Scholar] [CrossRef] [PubMed]
- Corbisiero, S.; Stieglitz, R.D.; Retz, W.; Rösler, M. Is emotional dysregulation part of the psychopathology of ADHD in adults? ADHD Atten. Deficit Hyperact. Disord. 2013, 5, 83–92. [Google Scholar] [CrossRef]
- Liu, Y.; Millsap, R.E.; West, S.G.; Tein, J.Y.; Tanaka, R.; Grimm, K.J. Testing measurement invariance in longitudinal data with ordered-categorical measures. Psychol. Methods 2017, 22, 486. [Google Scholar] [CrossRef]
- Merwood, A.; Chen, W.; Rijsdijk, F.; Skirrow, C.; Larsson, H.; Thapar, A.; Kuntsi, J.; Asherson, P. Genetic associations between the symptoms of attention-deficit/hyperactivity disorder and emotional lability in child and adolescent twins. J. Am. Acad. Child Adolesc. Psychiatry 2014, 53, 209–220. [Google Scholar] [CrossRef] [PubMed]
- Sobanski, E.; Banaschewski, T.; Asherson, P.; Buitelaar, J.; Chen, W.; Franke, B.; Holtmann, M.; Krumm, B.; Sergeant, J.; Sonuga-Barke, E.; et al. Emotional lability in children and adolescents with attention deficit/hyperactivity disorder (ADHD): Clinical correlates and familial prevalence. J. Child Psychol. Psychiatry 2010, 51, 915–923. [Google Scholar] [CrossRef]
- Gross, J.J. The emerging field of emotion regulation: An integrative review. Rev. Gen. Psychol. 1998, 2, 271–299. [Google Scholar] [CrossRef]
- Chen, S.; Bonanno, G.A. Components of emotion regulation flexibility: Linking latent profiles to depressive and anxious symptoms. Clin. Psychol. Sci. 2021, 9, 236–251. [Google Scholar] [CrossRef]
- Jiang, W.; Li, Y.; Du, Y.; Fan, J. Emotional regulation and executive function deficits in unmedicated Chinese children with oppositional defiant disorder. Psychiatry Investig. 2016, 13, 277. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; He, T.; Hinshaw, S.; Chi, P.; Lin, X. Longitudinal relationship between oppositional defiant disorder symptoms and attention-deficit/hyperactivity disorder symptoms in Chinese children: Insights from cross-lagged panel network analyses. Eur. Child Adolesc. Psychiatry 2023, 1–14. [Google Scholar] [CrossRef]
- Marwaha, S.; He, Z.; Broome, M.; Singh, S.P.; Scott, J.; Eyden, J.; Wolke, D. How is affective instability defined and measured? A systematic review. Psychol. Med. 2014, 44, 1793–1808. [Google Scholar] [CrossRef]
- Johnston, O.G.; Derella, O.J.; Burke, J.D. Identification of oppositional defiant disorder in young adult college students. J. Psychopathol. Behav. Assess. 2018, 40, 563–572. [Google Scholar] [CrossRef]
- Barry, T.D.; Marcus, D.K.; Barry, C.T.; Coccaro, E.F. The latent structure of oppositional defiant disorder in children and adults. J. Psychiatr. Res. 2013, 47, 1932–1939. [Google Scholar] [CrossRef]
- Harpold, T.; Biederman, J.; Gignac, M.; Hammerness, P.; Surman, C.; Potter, A.; Mick, E. Is oppositional defiant disorder a meaningful diagnosis in adults? Results from a large sample of adults with ADHD. J. Nerv. Ment. Dis. 2007, 195, 601–605. [Google Scholar] [CrossRef]
- Nock, M.K.; Kazdin, A.E.; Hiripi, E.; Kessler, R.C. Lifetime prevalence, correlates, and persistence of oppositional defiant disorder: Results from the National Comorbidity Survey Replication. J. Child Psychol. Psychiatry 2007, 48, 703–713. [Google Scholar] [CrossRef] [PubMed]
- Feng, Y.; Hancock, G.R. Model-based incremental validity. Psychol. Methods 2022, 27, 1039. [Google Scholar] [CrossRef] [PubMed]
- Soper, D. A-Priori Sample Size Calculator for Structural Equation Models [Software]. 2022. Available online: https://www.danielsoper.com/statcalc/ (accessed on 20 October 2022).
- Barkley, R.A.; Murphy, K.R. Attention-Deficit Hyperactivity Disorder: A Clinical Workbook, 2nd ed.; Guilford Press: New York, NY, USA, 1998. [Google Scholar]
- Cyders, M.A.; Littlefield, A.K.; Coffey, S.; Karyadi, K.A. Examination of a short English version of the UPPS-P Impulsive Behavior Scale. Addict. Behav. 2014, 39, 1372–1376. [Google Scholar] [CrossRef] [PubMed]
- Oliver, M. N & Simons, J.S. The affective lability scales: Development of a short-form measure. Personal. Individ. Differ. 2004, 37, 1279–1288. [Google Scholar] [CrossRef]
- Harvey, P.D.; Greenberg, B.R.; Serper, M.R. The affective lability scales: Development, reliability, and validity. J. Clin. Psychol. 1989, 45, 786–793. [Google Scholar] [CrossRef] [PubMed]
- Gratz, K.L.; Roemer, L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. J. Psychopathol. Behav. Assess. 2004, 26, 41–54. [Google Scholar] [CrossRef]
- Fowler, J.C.; Charak, R.; Elhai, J.D.; Allen, J.G.; Frueh, B.C.; Oldham, J.M. Construct validity and factor structure of the difficulties in emotion regulation scale among adults with severe mental illness. J. Psychiatr. Res. 2014, 58, 175–180. [Google Scholar] [CrossRef] [PubMed]
- Osborne, T.L.; Michonski, J.; Sayrs, J.; Welch, S.S.; Anderson, L.K. Factor structure of the difficulties in emotion regulation scale (DERS) in adult outpatients receiving dialectical behavior therapy (DBT). J. Psychopathol. Behav. Assess. 2017, 39, 355–371. [Google Scholar] [CrossRef]
- Mislevy, R.J.; Beaton, A.E.; Kaplan, B.; Sheehan, K.M. Estimating population characteristics from sparse matrix samples of item responses. J. Educ. Meas. 1992, 29, 133–161. [Google Scholar] [CrossRef]
- Hu, L.T.; Bentler, P.M. Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychol. Methods 1998, 3, 424. [Google Scholar] [CrossRef]
- Schermelleh-Engel, K.; Moosbrugger, H.; Müller, H. Evaluating the fit of structural equation models: Tests of significance and descriptive goodness-of-fit measures. Methods Psychol. Res. Online 2003, 8, 23–74. [Google Scholar]
- Hu, L.T.; Bentler, P. M Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. Multidiscip. J. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Brown, T.A. Confirmatory Factor Analysis for Applied Research, 2nd ed.; Guilford Press: New York, NY, USA, 2015. [Google Scholar]
- Giromini, L.; Ales, F.; de Campora, G.; Zennaro, A.; Pignolo, C. Developing age and gender adjusted normative reference values for the Difficulties in Emotion Regulation Scale (DERS). J. Psychopathol. Behav. Assess. 2017, 39, 705–714. [Google Scholar] [CrossRef]
- Miguel, F.K.; Giromini, L.; Colombarolli, M.S.; Zuanazzi, A.C.; Zennaro, A. A Brazilian investigation of the 36-and 16-item difficulties in emotion regulation scales. J. Clin. Psychol. 2017, 73, 1146–1159. [Google Scholar] [CrossRef] [PubMed]
- Orgeta, V. Specificity of age differences in emotion regulation. Aging Ment. Health 2009, 13, 818–826. [Google Scholar] [CrossRef] [PubMed]
- Hervás, G.; Jódar, R. Adaptación al castellano de la Escala de Dificultades en la Regulación Emocional. Clínica y Salud 2008, 19, 139–156. [Google Scholar]
- Mitsopoulou, E.; Kafetsios, K.; Karademas, E.; Papastefanakis, E.; Simos, P.G. The Greek version of the Difficulties in Emotion Regulation Scale: Testing the factor structure, reliability and validity in an adult community sample. J. Psychopathol. Behav. Assess. 2013, 35, 123–131. [Google Scholar] [CrossRef]
- Rugancı, R.N.; Gençöz, T. Psychometric properties of a Turkish version of the Difficulties in Emotion Regulation Scale. J. Clin. Psychol. 2010, 66, 442–455. [Google Scholar] [CrossRef]
- Barkley, R.A. A Handbook for Diagnosis and Treatment; Guilford Publications: New York, NY, USA, 2006; pp. 3–75. [Google Scholar]
- Barkley, R.A. Recent longitudinal studies of childhood attention-deficit/hyperactivity disorder: Important themes and questions for further research. J. Abnorm. Psychol. 2016, 125, 248–255. [Google Scholar] [CrossRef]
- Winstanley, C.A.; Eagle, D.M.; Robbins, T.W. Behavioral models of impulsivity in relation to ADHD: Translation between clinical and preclinical studies. Clin. Psychol. Rev. 2006, 26, 379–395. [Google Scholar] [CrossRef]
- Cludius, B.; Mennin, D.; Ehring, T. Emotion regulation as a transdiagnostic process. Emotion 2020, 20, 37–42. [Google Scholar] [CrossRef] [PubMed]
- Moriarity, D.P.; Grehl, M.M.; Walsh, R.F.L.; Roos, L.G.; Slavich, G.M.; Alloy, L.B. A systematic review of associations between emotion regulation characteristics and inflammation. Neurosci. Biobehav. Rev. 2023, 150, 105162. [Google Scholar] [CrossRef] [PubMed]
- Petruso, F.; Giff, A.E.; Milano, B.A.; De Rossi, M.M.; Saccaro, L.F. Inflammation and emotion regulation: A narrative review of evidence and mechanisms in emotion dysregulation disorders. Neuronal Signal. 2023, 7, NS20220077. [Google Scholar] [CrossRef] [PubMed]
- Hayes, S.C.; Wilson, K.G.; Gifford, E.V.; Follette, V.M.; Strosahl, K. Experiential avoidance and behavioral disorders: A functional dimensional approach to diagnosis and treatment. J. Consult. Clin. Psychol. 1996, 64, 1152. [Google Scholar] [CrossRef] [PubMed]
- Hallion, L.S.; Steinman, S.A.; Tolin, D.F.; Diefenbach, G.J. Psychometric properties of the Difficulties in Emotion Regulation Scale (DERS) and its short forms in adults with emotional disorders. Front. Psychol. 2018, 9, 539. [Google Scholar] [CrossRef] [PubMed]
- Saccaro, L.F.; Giff, A.; De Rossi, M.M.; Piguet, C. Interventions targeting emotion regulation: A systematic umbrella review. J. Psychiatr. Res. 2024, 174, 263–274. [Google Scholar] [CrossRef] [PubMed]
- Brummer, L.; Stopa, L.; Bucks, R. The influence of age on emotion regulation strategies and psychological distress. Behav. Cogn. Psychother. 2014, 42, 668–681. [Google Scholar] [CrossRef] [PubMed]
- Kwon, H.; Yoon, K.L.; Joormann, J.; Kwon, J.H. Cultural and gender differences in emotion regulation: Relation to depression. Cogn. Emot. 2013, 27, 769–782. [Google Scholar] [CrossRef] [PubMed]
- Nolen-Hoeksema, S. Emotion regulation and psychopathology: The role of gender. Annu. Rev. Clin. Psychol. 2012, 8, 161–187. [Google Scholar] [CrossRef]
- Sheppes, G.; Suri, G.; Gross, J.J. Emotion regulation and psychopathology. Annu. Rev. Clin. Psychol. 2015, 11, 379–405. [Google Scholar] [CrossRef]
| Model | MLRχ2 (df) | CFI | TLI | RMSEA (90% CI) | SRMR |
|---|---|---|---|---|---|
| 1-Factor | 638.736 (65) | 0.794 | 0.753 | 0.130 (0.121–0.139) | 0.076 |
| 3-Factor | 369.675 (62) | 0.889 | 0.861 | 0.097 (0.088–0.107) | 0.062 |
| Age | TI | DER | AL | ||
|---|---|---|---|---|---|
| IA | β (SE); z | −0.104 (0.045); 2.311 | 0.667 (0.041); 16.268 | 0.277 (0.051); 5.431 | 0.040 (0.049); 0.816 |
| R2 (95% CI) | 0.011 (−0.01/0.028) | 0.445 (0.382/0.508) | 0.077 (0.034/0.120) | 0.001 (−0.004/0.006 | |
| HI | β (SE); z | −0.014 (0.045); 0.311 | 0.548 (0.043); 12.744 | 0.309 (0.051); 6.059 | −0.066 (0.050); 1.320 |
| R2 (95% CI) | 0.000 (−0.000/0.001) | 0.300 (0.2370/0.365) | 0.095 (0.048/0.142) | 0.004 (−0.001/0.015) | |
| ODD | β (SE); z | −0.217 (0.037); 5.865 | 0.573 (0.039) 14.692 | 0.338 (0.047); 7.191 | 0.020 (0.041); 0.488 |
| R2 (95% CI) | 0.047 (0.012/0.089) | 0.328 (0.263/0.393) | 0.114 (0.063/0.165) | 0.000 (−0.002/0.002) |
| Age | TI | AL | DER | ||
|---|---|---|---|---|---|
| IA | β (SE); z | −0.104 (0.045); 2.311 | 0.667 (0.041); 16.268 | 0.208 (0.043); 4.84 | 0.188 (0.047); 4.00 |
| R2 (95% CI) | 0.011 (−0.01/0.028) | 0.445(0.382/0.508) | 0.043 (0.009/0.077) | 0.035 (0.004/0.066) | |
| HI | β (SE); z | −0.014 (0.045); 0.311 | 0.548 (0.043); 12.744 | 0.146 (0.055); 2.655 | 0.280 (0.048); 5.833 |
| R2 (95% CI) | 0.000 (−0.000/0.001) | 0.300 (0.237/0.365) | 0.021 (−0.003/0.045) | 0.078 (0.034/0.122) | |
| ODD | β (SE); z | −0.217 (0.037); 5.865 | 0.573 (0.039) 14.692 | 0.230 (0.049); 4.694 | 0.248 (0.042); 5.905 |
| R2 (95% CI) | 0.047 (0.012/0.089) | 0.328 (0.263/0.393) | 0.053 (0.016/0.090) | 0.062 (0.022/0.102) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gomez, R.; Houghton, S.J. Incremental Validity of Trait Impulsivity, Dysfunctional Emotional Regulation, and Affect Lability in the Predictions of Attention Deficit Hyperactivity Disorder and Oppositional Defiant Disorder Symptoms in Adults. Behav. Sci. 2024, 14, 598. https://doi.org/10.3390/bs14070598
Gomez R, Houghton SJ. Incremental Validity of Trait Impulsivity, Dysfunctional Emotional Regulation, and Affect Lability in the Predictions of Attention Deficit Hyperactivity Disorder and Oppositional Defiant Disorder Symptoms in Adults. Behavioral Sciences. 2024; 14(7):598. https://doi.org/10.3390/bs14070598
Chicago/Turabian StyleGomez, Rapson, and Stephen J Houghton. 2024. "Incremental Validity of Trait Impulsivity, Dysfunctional Emotional Regulation, and Affect Lability in the Predictions of Attention Deficit Hyperactivity Disorder and Oppositional Defiant Disorder Symptoms in Adults" Behavioral Sciences 14, no. 7: 598. https://doi.org/10.3390/bs14070598
APA StyleGomez, R., & Houghton, S. J. (2024). Incremental Validity of Trait Impulsivity, Dysfunctional Emotional Regulation, and Affect Lability in the Predictions of Attention Deficit Hyperactivity Disorder and Oppositional Defiant Disorder Symptoms in Adults. Behavioral Sciences, 14(7), 598. https://doi.org/10.3390/bs14070598






