Abstract
The ongoing public health crisis of substance use among school adolescents and young adults (AYAs) in South Africa is not new in research parlance, amidst the national policy of drug abuse management in schools. In view of no tangible progress to reduce substance use in high schools in the country, we conducted a cross-sectional quantitative study aimed at investigating substance use among adolescents and young adults in the four public high schools selected through multi-stage sampling in rural Mpumalanga province, South Africa. Data on substance use, demographics, household socio-demographics, and related factors were collected via a validated self-administered questionnaire. Hierarchical logistic regression was performed using STATA 18. The study included 402 AYAs aged between 14 and 23 years (18 ± 1 years), and 45% reported substance use in the last twelve months. Alcohol was the most used substance (74%), followed by cigarettes (12%) and cannabis (11%). AYAs used substances out of social influence, curiosity, to find joy, and to eliminate stress, especially in social events, on the streets, and at home, and reported negative physical health outcomes, mainly hallucinations, sleeping disorders, body weakness, and dry mouths. Hierarchical logistic regression showed that the likelihood of substance use was three times in a particular high school (S4) (AOR = 3.93, 95%CI: 1.72–8.99), twice among the grade 12s (AOR = 2.73, 95%CI: 1.46–5.11), over twenty times in the communities with substance availability (AOR = 22.45, 95%CI: 2.75–183.56), almost ten times among AYAs participating in recreational/sports activities (AOR = 9.74, 95%CI: 4.21–22.52), and twice likely to happen in larger households (AOR = 2.96, 95%CI: 1.57–5.58). Prevention and intervention efforts should consider these specific health concerns to develop targeted strategies for mitigating substance use and its adverse consequences in this vulnerable population towards achieving the United Nations’ Sustainable Development Goal Target 3.5, which aims to strengthen the prevention and treatment of substance abuse, including narcotic drug abuse and the harmful use of alcohol.
1. Introduction
Substance use/abuse remains a public health concern worldwide, affecting society on every level with variations in life stages, types, prevalence, and risk factors [1,2,3]. The Centers for Disease Control and Prevention (CDC) refers to substance use as the use of selected substances injected or otherwise absorbed into the body with possible dependence and other detrimental effects [4]. These substances include alcohol (beer, wine, and distilled liquors) and tobacco (cigarettes, vapor-cigarettes, cigars, chewing tobacco, and snuff), which are legal, as well as illegal cannabinoids (marijuana/cannabis/dagga and edible cannabinoids), opioids, cocaine, and hallucinogens. Substance use affects young people aged 10–24 years [5], and the age of onset for substance use is estimated between 13 and 15 years in low- and middle-income countries (LMICs) and under 20 years in Europe, Australia, and North America [6]. Globally, 53% of people aged 15 years and above have ever used substances (mainly alcohol) [1,7]. In sub-Saharan Africa (SSA), 42% of adolescents and young adults (AYAs) use substances, while 33% use alcohol, followed by tobacco use (25%) and cannabis (16%) [1,2]. In the Southern African region, 37% of AYAs use substances, such as alcohol (41%), tobacco (46%), and cannabis (26%) [2]. While, in South Africa, alcohol (22–66%) and tobacco (46%) are the most used substances among school AYAs [3,8,9,10,11], the use of cannabis and other substances has also been documented [12,13,14].
Substance use burdens the educational and social systems and has health and behavioral implications [1,2,7]. The curiosity of AYAs to experiment with substances leads to addiction/dependency [1,10,11,12], and predisposes them to sexual risk behaviors [13,14,15], respiratory conditions, oral pathologies, and decreased physical capacity [15,16]. Others reported negative influences on mental health including psychosocial problems (anxiety and depressive symptoms) and psychological distress [16,17] such as social anxiety, developing psychosis (i.e., hallucinations and paranoia), and schizophrenia (a type of mental illness where people might see or hear things that are not there) [17,18]. Substance use is triggered by wanting to feel good, feel better, and do better, out of curiosity or because others are doing it (i.e., social influence) [9,19]. Among AYAs, reasons are based on seeking new experiences and taking risks, sharing a social experience, or feeling part of a social group, relieving stress, and relieving symptoms of mental health disorders such as anxiety and depression [9,20]. Risk factors associated with substance use are multifaceted, encompassing various domains. These include experiences of childhood trauma [21] as well as demographic and socioeconomic variables [22,23]. Moreover, factors related to educational attainment, engagement in extracurricular activities or part-time employment, financial autonomy, and receiving a childcare grant also play contributory roles [3]. Additionally, psychological attributes such as poor self-control, inadequate parental supervision, parental attitudes, social networks, peer influence, and the presence of certain mental health conditions such as attention-deficit/hyperactivity disorder (ADHD) are implicated [20]. Notably, these risk factors have been observed across multiple African [24,25,26] and South African [9,27,28] contexts, highlighting their broad relevance and potential impact on substance use behaviors.
Studies in South Africa have reported variations in the prevalence of substance use, types, reasons, related effects and complications, and contributing factors in various provinces/regions [3,9,14,16,27,29,30,31,32,33] including the South Africa National Youth Risk Behavior Survey (SANYRBS) [34]. Substance use has reportedly reached epidemic proportions among high school AYAs however, the disproportionality of minimal research by provinces is evident and calls for continuous and translational research, bearing in mind that South Africa has ethnicity and cultural diversity, and pockets of poverty [35]. In South Africa, AYAs are confronted with diverse and context-based social [3,9,36] and health issues [37,38] amidst the burden of disease [39,40]. To date, the SANYRBS remains a comprehensive national baseline survey in South Africa since the implementation of the compulsory education system and contributes significantly to informing the evidence base for future health promotion intervention planning [41], although with limited data on AYAs’ perceptions of substance use and risk factors emerging recently in under-resourced settings in South Africa. One such intervention is the implementation of comprehensive school-based prevention programs that incorporate elements such as education on the risks of substance use, skill-building to resist peer pressure, and fostering positive social norms regarding substance use. Given no tangible progress in reducing substance use among school learners in South Africa, we conducted a cross-sectional quantitative study to investigate substance use among AYAs in public high schools in Mpumalanga, South Africa. If care is not taken, substance use among young people seems likely to persist as one of the public health burdens with implications on health and behavior, as well as burdening the educational and social systems [1]. We envisaged that continuous translational research such as this will add knowledge and inform evidence-based multilevel–multicomponent interventions to minimize the abuse and effects of substances in schools in alignment with the United Nations’ Sustainable Development Goals (SDG) target 3.5. The SDG Target 3.5 aims to strengthen the prevention and treatment of substance abuse, including narcotic drug abuse and harmful use of alcohol. This target is part of the broader SDG 3, which seeks to ensure healthy lives and promote well-being for all at all ages [42].
Moreover, the implementation of school policies and environmental changes can also contribute to substance abuse prevention efforts. This may include enforcing strict policies regarding substance use on school premises, promoting alternative recreational activities, and fostering a supportive and drug-free school environment. Since the legislative frameworks related to substance use differ from country to country, in South Africa, there are age limits for purchasing alcohol and tobacco products, typically ranging from 18 to 21 years old. This is the same as the legality of cannabis, with some countries legalizing its use for medicinal or recreational purposes, while others maintain strict prohibition laws around its use.
Generally, the Socio-Ecological Model provides a comprehensive approach to understanding and addressing the multiple levels of influence on health behaviors and outcomes, and it informs the development of multilevel interventions to promote health and prevent disease [43,44]. Theoretically, risk factors of substance use among AYAs are grouped into three broad categories: personal level influence (genetic susceptibilities, mental health and personality traits, neurological development, and stress reactivity), micro level influences (family influences, school influences, and peer influences) and macro level influences (income and resources, social environment, and physical environment), as reported by the United Nations Office on Drugs and Crime Prevention (UNODC) [45]. The conceptual framework related to the factors investigated in this study is comprehensively presented in Figure 1.
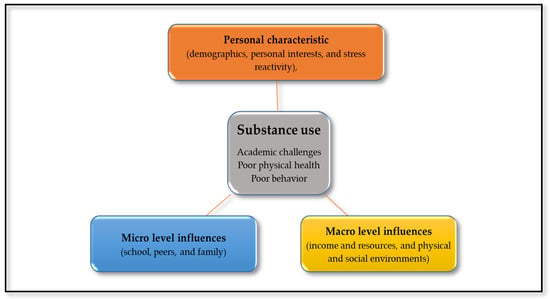
Figure 1.
Adapted Socio-Ecological Model on factors influencing adolescent substance use.
2. Methods
2.1. Study Design, Setting, and Population
This is a cross-sectional and quantitative study conducted between August 2022 and January 2023. The study was conducted in the Dr. JS Moroka municipality situated in Mpumalanga province, South Africa. While several studies have been conducted in other provinces such as Gauteng and Free State Western Cape, Mpumalanga remains less studied regarding substance use and other social issues. We randomly selected the Dr. JS Moroka municipality as the study setting.
Mpumalanga province is found in the north-eastern part of South Africa and is bordered by four out of nine provinces, which are Gauteng, Limpopo, Free State, and KwaZulu-Natal [46]. The Dr. JS Moroka municipality in the Nkangala district is inhabited by 99% black Africans with serious challenges in terms of unemployment, poverty, and inequality. The poverty headcount ratio in South Africa’s national poverty line has been estimated at 56% in 2020 and increased from 40% in 2011 [47]. The gap between the rich and the poor has widened due to unemployment resulting in the income gap, with the wealthiest 20% of South Africans earning almost 68 times more than the poorest 20%. This disparity has serious consequences for social cohesion, as it causes continuous inequality and hinders economic growth [47].
2.2. Sample Size and Sampling Procedure
Using the Cochran formula and taking into consideration an estimated total enrolment figure of approximately 25,000 high school AYAs in this municipality, a 95% confidence interval, and a 5% margin of error, a minimum representative sample was calculated using the Raosoft sample calculator. The calculated minimum representative sample size was 379 participants. Buffered with 10% for possible incomplete or missing data, the total sample size for the study will be 412.
A multi-stage sampling technique was used to select schools, learning grades, classes, and AYAs. First, high schools were selected randomly, and out of the 12 (twelve) schools situated at the Mametlhake and Nokaneng education circuits within the Dr. JS Moroka municipality, four (4) schools were selected. Second, within the selected schools, a simple random sampling of learning grades, classes, and learners was carried out. High schools used in this study previously belonged to the former Bophuthatswana homeland in South Africa and they were called high schools starting with Grade 10 (previously called standard 8), Grade 11 (previously called standard 9), and up to Grade 12 (previously called standard 10). Enrolment numbers by school were as follows: first school (S1) ≈ 659, second school (S2) ≈ 993, third school (S3) ≈ 400, and fourth school (S4) ≈ 555. The sampling plan entailed treating each school as a unit of analysis with a sample size between 90 and 150 to avoid disproportionate sampling. However, a lower sample was obtained in one school due to the reluctance of parents to consent to the participation of their dependencies.
AYAs were recruited during school visits and the principals of schools were provided with letters addressed to the school governing bodies, an ethical certificate from the Sefako Makgatho Health Sciences University Research and Ethics Committee (SMUREC), and a permission letter from the Mpumalanga Department of Education to access high schools in the Mametlhake and Nokaneng education circuits. After obtaining permission to conduct the study in the selected high schools, the research team further liaised with the allocated teacher to facilitate obtaining parental consent for their dependents and identifying AYAs from the grades and classes. Selected AYAs were engaged in the procedure of the study and preparations for data collection.
2.3. Data Collection and Tools
A pre-tested structured self-administered questionnaire was used to collect data on socio-demographic data and substance use. The questionnaire was adapted from similar studies conducted on substance use among school adolescents in South Africa, including the SAYRBS [32,33,48,49]. Data were collected on the demographic data of AYAs such as learning grade, gender, and age, and previous grade performance. Demographic characteristics of participants obtained included, age, sex, school, learning grade, participation in recreational/sports, and religious activities, while their household socio-economic status obtained included parents’/guardians’ marital status, education level, employment status, and household infrastructure. Information on substance use included past and current use (in the last 12 months), age of first use, types, as well as availability, reasons, and related effects. According to the WHO, alcohol consumption in the past 12 months is defined as the proportion of adults (15+ years) in a given population who have consumed any alcohol during the past 12 months, assessed at a given point in time [50].
Before data collection, content, face, and construct validity were checked to ensure the quality of the questionnaire. In content validity, experts in the field ensured the adequacy of the questionnaire to measure the intended constructs [34], while face validity was based on the layout of the questionnaire. The questionnaire was translated from English to a local language (i.e., Setswana) by an independent translator who is conversant in the two languages. A pilot study was conducted to determine the feasibility of the main study. During the pilot study, conducted in one high school that was not part of the main study, research assistants were trained and assessed while assisting the AYAs in filling out the questionnaire. After pretesting the questionnaire, adjustments such as minimal clarity of wording and simplifying the layout and style were performed on the questionnaire. The results from a pilot study informed the feasibility of statistical analysis to ascertain the determinants of substance use and did not form part of the main study.
Thereafter, selected AYAs with parental consent were arranged to gather in their respective schools on the day of data collection. The research team engaged AYAs on the purpose and the procedure of the study, and they were given the opportunity to ask questions. AYAs who were 18 years and above were given consent forms, and those who were below 18 years and had parental consent were requested to give assent to participate in the study. Questionnaires were distributed to adolescents to complete in the presence of the first author and the two research assistants to give assistance when necessary and lasted for 20 to 30 min. During data collection, there were no interruptions to the daily running of the schools, and engagements with adolescents were conducted after school hours. On a rare occasion, we used weekends and school holidays, as per the agreement with parents, permission from the SGB, and ethical clearance from the Mpumalanga Provincial Department of Education (South Africa), with approved timelines to visit all four high schools.
2.4. Statistical Analysis
Data were analyzed using STATA (Intercooled Stata® Version 18). Complete case analysis (CRA) was used to identify participants with missing data during analysis. After checking for data distribution using the Skewness–Kurtosis test for numerical data, descriptive and inferential statistics were computed. Descriptive statistics were used to analyze data on substance use, types, reasons for use, related effects, and risk factors, as well as adolescents’ demographics and households’ socio-demographics (%). Chi-square/Fisher’s exact test was used to compare differences in proportion between two categorical groups. Results are presented as frequencies (n) and percentages (%), Chi-square (χ2) and p-value. Bivariate and multivariable-adjusted logistic regression analyses were used to assess the risk factors of substance use based on factors associated with substance use in the bivariate analysis at p < 0.20. Following that, a stepwise backward elimination procedure was used to eliminate confounders and only factors associated with substance use at p < 0.05 were retained in the final model. Results are presented as crude odds ratios (OR) and adjusted odds ratios (AOR) with a 95% confidence interval (CI) and for all analyses, statistical significance was considered at p < 0.05.
2.5. Ethics Statement
This study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving human subjects were approved by the Sefako Makgatho Health Sciences University Research and Ethics Committee (SMUREC) (SMUREC/H/137/2022: PG). Further permission was sought from the Mpumalanga Provincial Department of Education (South Africa) to access schools in the municipality. Following that, permission was sought from the schools’ principals and governing bodies of the selected high schools. Post receiving permission from the schools, written consent was requested from the parents before engaging students, as described in the recruitment of learners. Additionally, during data collection, written informed consent was obtained from adolescents who were aged 18 years, and assent from adolescents who were aged below 18 years.
3. Results
3.1. Prevalence of Substance Use and the Types of Substances
Ten questionnaires had missing data of over 10%, especially on the primary outcome, and were excluded during data analysis. The final sample of 402 AYAs was obtained, and their mean age was 18 ± 1 years ranging from 14 to 23 years. Almost half (45%, 95%CI: 40–50%) of them reported using one or more substances in the last twelve months, and most, 92% (95%CI: 87–95%), started using substances before the age of 18 years. Alcohol was the most used substance (74%), followed by cigarette (12%) and cannabis (11%) use, and other substances such as nyaope (i.e., a form of black tar heroin, sometimes mixed with other substances). Results are presented as frequencies (N) and proportions (%) in Table 1.

Table 1.
Prevalence of substance use and the types.
3.2. Demographic Characteristics of Adolescents and Guardians
In Table 2, the Chi-square test was used to compare demographic characteristics between AYAs who use substances and the non-users. The sample included 162 (40%) boys and 240 (60%) girls. Adolescents were divided into two groups: younger (<18 years) and older (≥18 years). Sample sizes by schools were 93 (23%) in the first school (S1); 133 (33%) in the second school (S2); 131 (33%) in the third school (S3); and 45 (11%) in school number 4 (S4) with the lowest participation of adolescents. AYAs were distributed across grade 10 (n = 90), grade 11 (n = 85), and grade 12 (n = 227). Only 13% of AYAs reported participation in both recreational activities/sports and religious activities. Significant differences of substance use were observed by school (p ≤ 0.0001) and participation in recreational/sports activities (p ≤ 0.0001).

Table 2.
Comparison of demographics among substance non-users and users.
Chi-square/Fisher’s exact tests showed significant differences of substance use with parents’/guardians’ marital status, household size, water access, electricity use, and type of toilet. Most parents/guardians of AYAs had grade 12 education, were married (84%), unemployed (52%), lived in larger households (85%), and with a monthly income below R5000 (85%). Poor sanitation and infrastructure were observed by the use of pit toilets (95%), while electricity and water access were reported in 90% of households in Table 3.

Table 3.
Comparison of guardians’ socio-demographics among substance non-users and users.
3.3. Availability, Reasons, and Related Effects of Substance Use
Table 4 shows availability, reasons, and related effects of substance use. Over two-thirds of AYAs reported availability of alcohol outlets near schools (70%) and in the communities (70%). Substance use among AYAs was common at social events (i.e., parties/social occasions) (47%), streets and homes (43%), and less common at the recreational/sports platforms (10%) with minimal participation in sports/recreational activities (13%). About two-thirds of AYAs (60%) were aware of substance use complications, and at some point, while using substances, they reported experiencing excitement/euphoria (28%), nausea (17%), aggressiveness (16%), lack of respect (15%), and lack of studying (10%). Also, at the time of the study, AYAs reported episodes of hallucinations, sleeping disorders, body weakness, and dry mouths due to substance use.

Table 4.
Availability, reasons, and related effects of substance use.
3.4. Risk Factors for Substance Use
Table 5 shows the association of substance use and risk factors. In univariable logistic regressions (crude odds ratio (COR)), substance use was associated with age, attending a particular high school, learning grade, participation in recreational/sports activities, and parents’/guardians’ marital status, and household size (p ≤ 0.25). After controlling for potential confounders (i.e., age, sex, age of first use, and guardians’ employment status and household income), the final hierarchical logistic regression showed significant associations of substance use with attending a particular high school (S4) (AOR = 3.93, 95%CI: 1.72–8.99), learning grade 12 (AOR = 2.73, 95%CI: 1.46–5.11), substance availability in communities (AOR = 22.45, 95%CI: 2.75–183.56), participating in recreational/sports activities (AOR = 9.74, 95%CI: 4.21–22.52), and living in larger households (AOR = 2.96, 95%CI:1.57–5.58).

Table 5.
Risk factors for substance use.
4. Discussion
The concern about the ongoing substance use among young people accompanied by negative social and health outcomes can never be overemphasized. For this reason, we investigated substance use among school adolescents and young adults (AYAs) in rural public high schools in the Dr. JS Moroka municipality in Mpumalanga, South Africa. Almost half of AYAs in this study reported current use of a substance, like reports in other studies [3,9,14,16,27]. The prevalence of substance use among AYAs varies in SSA [2,51], attributed to several factors including socio-environmental, liberal attitudes and practices, social norms, lack of effective substance enforcement, lack of effective implementation of laws, as well as access and availability of these substances [2,51]. AYAs who participated in the current study started substance use while they were below 18 years of age [52,53], which has previously been reported in South Africa, despite the National Liquor Act prohibiting alcohol sale to individuals younger than 18 years of age [9,54]. Initiation of substance use in early adolescence age (age ≤ 13 years) has serious public health implications and consequences such as poor performance at school, dropout, developing alcohol addiction/dependence, experiencing mental and social harm, and cardiovascular diseases later in adulthood [55,56]. Our results show that 45% of school AYAs were currently using substances at the time of the study, suggesting an ongoing public health problem predisposing them to social, behavioral, and health issues.
Over two-thirds of AYAs reported alcohol (beer, cider, and wine) as a common substance used, followed by cigarette smoking and cannabis. According to the WHO [57], beer, wine, and spirits are mostly consumed in SSA and vary by geographical differences and population groups. In South Africa [3,9,14,27,31,32,58], alcohol use is common, the same as in most SSA countries [2,51,59], Europe [60], and the USA [61,62]. Cigarette smoking and cannabis were less likely used after alcohol use, same as in previous South African studies [14,28,31,63,64] and other countries like Ethiopia [65] and Ghana [66]. Furthermore, the availability of alcohol outlets near most schools and the presence of various substances in the communities have been reported in our study, like in other local studies [58,67,68] and in other countries [69,70,71]. Also, easy access to alcohol, cigarette, and cannabis substances, also observed in this study, has been implicated as the main contributing factor to the use of various types of substances [14,31,32]. Stringent measures to halt the availability of substances around schools and communities, as well as easy access, should be put in place. Such measures that could be implemented may include firstly, community policing and surveillance by involving regular patrols, targeted operations, and collaboration with local authorities to identify and address areas of high substance availability. Secondly, community engagement and awareness campaigns by fostering community involvement in substance abuse prevention efforts through educational campaigns, community forums, and neighborhood watch programs. Thirdly, supporting alternative outdoor activities that provide opportunities for AYAs to participate in positive recreational, cultural, and educational activities as alternatives to substance use. This could include expanding access to sports programs, arts and music classes, after-school clubs, and community events that promote healthy lifestyles and social connections.
The current study further showed that AYAs predominantly engaged in substance use during social events, on the streets, and in their homes, with fewer instances reported at recreational or sports platforms. This highlights the significant role of environmental contexts in shaping substance use behaviors within this demographic. These findings align with existing studies that underscore the impact of social settings on AYAs’ substance use [72,73,74]. Social events, streets, and homes often serve as venues for social interactions and peer influences, contributing to the increased likelihood of substance use initiation and engagement in these settings [43,75]. The prevalence of substance use at social events indicates the influence of peer dynamics and socialization processes on AYAs’ substance use behaviors. Peer influence has been identified as a potent factor in the initiation and maintenance of substance use during adolescence [43,76]. The prominence of substance use on streets and in homes further emphasizes the significance of familial and community environments in influencing AYAs’ engagement with substances. Family dynamics, including parental attitudes and behaviors, may contribute to the normalization or acceptance of substance use within the home environment, thereby influencing adolescents’ perceptions and behaviors [77,78]. Therefore, the availability and accessibility of substances on streets may expose AYAs to increased opportunities for experimentation.
Similarly, the comparatively higher likelihood of substance use at recreational/sports platforms suggests that these settings may be conducive to substance use among AYAs. Researchers have highlighted the influence of recreational habits, particularly in the weekend night-life context, on drug use [79]. Veliz and colleagues [80] also emphasized that the type of sports participation can influence substance use, with high-contact sports associated with higher odds of substance use. Nevertheless, recreational and sports activities often provide structured and supervised environments, which may act as protective factors against substance use initiation [72,73]. As such, we believe that the presence of positive role models, organized activities, and a focus on skill development in these settings may help to reduce the likelihood of engaging in substance use in this community.
Reasons/motivations for substance use were diverse among AYAs and cited as seeking joy, curiosity, eliminating stress, and succumbing to social influences from family and friends. These motivational factors align with previous research that has identified similar drivers for substance use in AYAs [81,82]. Researchers have reported that learners are prone to substance use due to various reasons, like academic and peer pressure, the appeal of popularity and identification, readily available pocket money, and relatively easy accessibility of several substances [83,84]. Further, AYAs are vulnerable to substance use either due to peer pressure from their friends and family or because of being lonely. Therefore, this multifaceted nature of motivations underscores the complexity of addressing substance use behaviors within this demographic. However, these behaviors should be discouraged since they may affect the academic performance and physical growth of AYAs, and therefore a need for social resistance training skills for one not to succumb to pressure is required [85]. Therefore, in this setting, it would be important to equip AYAs with skills and strategies to resist peer pressure and make healthy choices regarding substance use. To mention a few examples, school-based prevention programs could integrate substance use prevention modules into the school curriculum, focusing on building refusal skills, assertiveness, and decision-making abilities. Secondly, peer support groups could be established within schools or communities where AYAs can connect with peers who share similar values and goals regarding substance use avoidance. Peer mentors can provide guidance, support, and encouragement to resist peer pressure and make positive choices.
Regarding risk factors, substance use was significantly associated with attending a particular high school, being in learning grade 12, substance availability in communities, participating in recreational/sports activities, living in larger households, as well as several socio-demographic variables such as parents’/guardians’ marital status and infrastructure and sanitation issues on bivariate analysis. These findings are similar to other studies in South Africa [3,27,31,58,86] and other countries [85,87]. However, inconsistent determinants of substance use among AYAs by age, sex, setting, learning grade, and school attended have been reported [3,27,53,88], mostly attributed to the differences in alcohol drinking patterns [27]. In this case, AYAs who are in grade 12 were likely to use substances in this study, compared to those in grades 10 and 11. According to the Youth Research Unit (YRU), most learners who use drugs are in grade 12, and this is attributed to peer pressure and the desire to be socially accepted amidst stress relief and recreational purposes [89].
Episodes of lack of studying, lack of respect, and aggressiveness were reported in this study. In particular, substance use has been associated with aggression, influencing the course and risks of substance-use disorders among AYAs [90]. Previous research has reported that AYAs who use substances encounter social harms, such as physical fights and injury/accidents [9] in addition to repeating a grade, absenteeism, missing school, dropout, and low academic performance [3,91,92,93,94]. Some AYAs reported experiencing complications with hallucinations, sleeping disorders, body weakness, and dry mouths, which reveals the need for understanding of the impact of substance use on the physical and mental well-being of this population. This is because hallucinations are perceptual disturbances that can significantly impair cognitive function and reality perception [95], such that previous studies have linked hallucinatory experiences to substance use, particularly in the context of hallucinogenic substances [96,97]. The reported complications in this study align with the existing literature that underscores the potential psychological repercussions of substance use among AYAs [95,96,97,98]. Our study further noted sleeping disorders as another complication. Disruptions in sleep patterns can have detrimental effects on overall health and well-being, particularly in a developmental stage where adequate sleep is crucial [99]. Substance use has been consistently associated with sleep disturbances among adolescents and young adults [100,101]. As such, our findings reinforce the existing literature by highlighting the prevalence of sleeping disorders as a potential consequence of substance use among AYAs.
Over two decades ago, the South African government intended to secure schools as safe and disciplined learning environments to enhance quality education, and as a result, published the National Policy of Drug Abuse Management in Schools guidelines to manage substance use in school environments [39]. To date, no progress related to this policy to address substance use has been recorded, as attested by colleagues [39]. There are several successful school-based programs reported in Australia (School Health and Alcohol Harm Reduction Project (SHAHRP)) [102], the United States of America (Project ALERT [103] and ALERT Plus [104]), and Europe (the Unplugged program) [105]. These programs have shown promising results in enhancing the reduction of substance use among youth [106], mainly because they incorporate skills training aimed at changing attitudes, promoting social and emotional abilities, critical thinking, and problem-solving compared to traditional intervention programs focusing on changing attitudes and perceptions on substance use and increasing awareness about the negative effects of peer pressure [106]. Therefore, these programs might also be relevant in our context considering that AYAs are an important target group for substance use prevention and interventions and intensified efforts to address this crisis must be on a school level.
Our results should be considered with some limitations. The cross-sectional design used allowed for reporting on the inferences rather than causality. The use of four high schools in the area, although selected randomly, limits generalizing the results, mainly because the study was limited to black AYAs in rural high schools. We did not control for the number of different high schools as the unit of analysis, and as a result, did not account for the potential clustering effect, where students from the same high school are likely to be more like each other compared to students from different schools. This clustering can lead to alpha inflation, making the results appear more significant than they might be if the school-level variance were properly controlled. In addition to prevalence, types, and reasons/motivations, this study reports on proximal determinants of substance use rather than distal determinants, which could have been elaborated on based on the pricing and marketing of substances. Social desirability, response, and recall biases might have been introduced during data collection originating from AYAs self-reporting substance use, types, and reasons. Most importantly, although we validated a tool used in this study and tested for reliability, the use of standardized tools such as the Alcohol Use Disorders Identification Test could have provided conclusive results and must be adopted in future studies. However, the prevalence, types, reasons, and risk factors correspond with local studies, although with varying magnitudes and intensities of relationships. Finally, this study did not investigate how and where AYAs obtain substances, and this information could provide insights into effective enforcement strategies to curb availability. Understanding the sources of substances can inform targeted interventions to disrupt supply chains and prevent access to illicit drugs. To address this gap, future research could incorporate qualitative methods such as interviews or focus groups to explore AYAs’ experiences with obtaining substances, including their interactions with dealers, peers, or online platforms. Additionally, collaborating with law enforcement agencies to gather data on drug trafficking patterns and areas of high substance availability could further inform enforcement efforts. By elucidating the pathways through which AYAs access substances, policymakers and stakeholders can develop more targeted and effective strategies to reduce availability and mitigate the harms associated with substance use among this vulnerable population. The use of frameworks emphasizes that individuals are embedded within multiple systems and that the interaction between these systems influences their health and well-being.
5. Conclusions
This study highlights current substance use among school AYAs. Alcohol was the most common substance used, followed by cigarette and cannabis use. Availability of alcohol outlets near their schools and various substances in the communities were reported. Further results showed that AYAs used substances out of social influence, curiosity, to find joy, and eliminate stress, especially in social events, on the streets, and at home. They also reported experiencing negative physical health outcomes due to substance use, mainly hallucinations, sleeping disorders, body weakness, and dry mouths. In the final model, risk factors for substance use were attending a particular high school, being in grade 12, availability in communities, participating in recreational/sports activities, and living in larger households. These findings advocate for prevention and intervention efforts that should consider these specific health concerns to develop targeted strategies for mitigating substance use and its adverse consequences in this vulnerable population.
Our conclusion underscores the importance of tailored prevention and intervention initiatives to address the specific health challenges faced by HIV-positive individuals with substance use disorders, to achieve the United Nations’ Sustainable Development Goals (SDGs) Target 3.5. SDG Target 3.5 aims to strengthen the prevention and treatment of substance abuse, including narcotic drug abuse and harmful use of alcohol. To effectively curb substance use in the municipality where the high schools are located, the first step should involve conducting a comprehensive needs assessment and situational analysis to understand the specific factors contributing to substance use among learners. This assessment should involve collaboration with local stakeholders, including schools, healthcare providers, law enforcement agencies, and community organizations. Additionally, it is crucial to prioritize evidence-based prevention strategies such as education and awareness campaigns, peer support programs, access to mental health and substance use services, and enforcement of policies to restrict access to substances.
Adapting some of the programs mentioned previously, such as the SHAHRP [102], Project ALERT [103], ALERT Plus [104], and the Unplugged program [105], might also assist in our case due to the reported promising results in enhancing the reduction of substance use among youth [106], and the incorporation of skills-training to change attitudes, promote social and emotional abilities, critical thinking, and problem-solving [106].
Author Contributions
Conceptualization, T.G.M., P.M. and M.M.; methodology, T.G.M., P.M. and M.M.; supervision, P.M. and M.M.; formal analysis, P.M. and N.T.; validation, M.M. and O.A.-Y.; investigation, T.G.M. and P.M.; project administration, T.G.M.; resources, T.G.M.; writing—original draft preparation, T.G.M., P.M., M.M., N.T., M.D.S., T.K.M. and O.A.-Y.; writing—review and editing, P.M., M.M., M.D.S., T.K.M. and O.A.-Y. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study received ethical clearance from the Sefako Makgatho Health Sciences University Research and Ethics Committee (SMUREC) (SMUREC/H/137/2022: PG) on the 2nd of June 2022. Permissions were obtained from the Department of Education (Mpumalanga Province, South Africa). Further permissions were obtained from the schools’ principals and governing bodies, and parents.
Informed Consent Statement
Written informed consent was obtained from parents of school AYAs in addition to their consent and assent as participants. Prior to data collection, AYAs were informed that participation is voluntary, and it will have no effect on their academic status.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- WHO. Global Status Report on Alcohol and Health; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Ogundipe, O.; Amoo, E.; Adeloye, D.; Olawole-Isaac, A. Substance use among adolescents in sub-Saharan Africa: A systematic review and meta-analysis. S. Afr. J. Child Health 2018, 12, 79–83. [Google Scholar] [CrossRef]
- Mmereki, B.; Mathibe, M.; Cele, L.; Modjadji, P. Risk factors for alcohol use among adolescents: The context of township high schools in Tshwane, South Africa. Front. Public Health 2022, 10, 969053. [Google Scholar] [CrossRef] [PubMed]
- CDC. Substance Use. Centers for Disease Control and Prevention. 2023. Available online: https://en.wikipedia.org/wiki/Centers_for_Disease_Control_and_Prevention (accessed on 26 January 2024).
- WHO. Adolescents and Young Adults Health Key Facts; World Health Organization: Geneva, Switzerland, 2021; Available online: https://www.who.int/news-room/fact-sheets/detail/adolescents-health-risks-and-solutions (accessed on 18 February 2024).
- Dykes, G.; Casker, R. Adolescents and substance abuse: The effects of substance abuse on parents and siblings. Int. J. Adolesc. Youth 2021, 26, 224–237. [Google Scholar] [CrossRef]
- Francis, J.M.; Weiss, H.A.; Mshana, G.; Baisley, K.; Grosskurth, H.; Kapiga, S.H. The Epidemiology of Alcohol Use and Alcohol Use Disorders among Young People in Northern Tanzania. PLoS ONE 2015, 10, e0140041. [Google Scholar] [CrossRef] [PubMed]
- Maserumule, O.M.; Skaal, L.; Sithole, S.L. Alcohol use among high school learners in rural areas of Limpopo province. S. Afr. J. Psychiatry 2019, 25, 1–6. [Google Scholar] [CrossRef]
- Mathibe, M.; Cele, L.; Modjadji, P. Alcohol Use among High School Learners in the Peri-Urban Areas, South Africa: A Descriptive Study on Accessibility, Motivations and Effects. Children 2022, 9, 1342. [Google Scholar] [CrossRef] [PubMed]
- Ramsoomar, L.; Morojele, N.K.; Norris, S.A. Alcohol use in early and late adolescence among the birth to twenty cohort in Soweto, South Africa. Glob. Health Action 2013, 6, 19274. [Google Scholar] [CrossRef] [PubMed]
- Morojele, N.K.; Brook, J.S.; Brook, D.W. Tobacco and alcohol use among adolescents in South Africa: Shared and unshared risks. J. Child Adolesc. Ment. Health 2016, 28, 139–152. [Google Scholar] [CrossRef] [PubMed]
- Manu, E.; Douglas, M.; Ntsaba, M.J.; Makaula, B.; Tarkang, E.E. Protective Behavioural Mechanisms against Cannabis Use among Adolescents in Cannabis-Growing Settings of South Africa: Insights into Adolescent Cannabis Use Prevention. Tob. Use Insights 2022, 15, 1179173x221146040. [Google Scholar] [CrossRef]
- Khine, A.A.; Mokwena, K.E. Drug interaction s in the constituents of street drug mixture“Nyaope”in South Africa: A mini-review. Afr. J. Drug Alcohol Stud. 2016, 15, 91–101. [Google Scholar]
- Mohale, D.; Mokwena, K.E. Substance use amongst high school learners in the south of Johannesburg: Is this the new norm? S. Afr. Fam. Pract. Off. J. S. Afr. Acad. Fam. Pract./Prim. Care 2020, 62, e1–e6. [Google Scholar] [CrossRef] [PubMed]
- Nogueira, K.T.; da Silva, C.M.F.M. Tabagismo em adolescentes numa escola da rede pública do estado do Rio de Janeiro. Adolesc. E Saude 2004, 1, 6–10. [Google Scholar]
- Ayo-Yusuf, O.A.; Van Den Borne, B.; Reddy, P.S.; Van Wyk, P.J.; Severson, H.H. Longitudinal Association of Smoking-Related Attitude to Oral Health with Adolescents’ Smoking Onset. J. Public Health Dent. 2009, 69, 29–33. [Google Scholar] [CrossRef]
- National Academies of Sciences Engineering and Medicine. The Health Efects of Cannabis and Cannabinoids: Current State of Evidence and Recommendations for Research; National Academies of Sciences Engineering and Medicine: Washington, DC, USA, 2017. [Google Scholar]
- Volkow, N.D.; Swanson, J.M.; Evins, A.E.; DeLisi, L.E.; Meier, M.H.; Gonzalez, R.; Bloomfield, M.A.; Curran, H.V.; Baler, R. Effects of Cannabis Use on Human Behavior, Including Cognition, Motivation, and Psychosis: A Review. JAMA Psychiatry 2016, 73, 292–297. [Google Scholar] [CrossRef]
- NIDA. Drugs, Brains, and Behavior: The Science of Addiction. 2008. Available online: https://www.drugsandalcohol.ie/13597/8/NIDA_Drugs_Brains_Behavior.pdf (accessed on 10 March 2022).
- Levy, S. Drug and Substance Use in Adolescents. MDS Manualscom. 2022. Available online: https://www.msdmanuals.com/en-in/professional/pediatrics/problems-in-adolescents/drug-and-substance-use-in-adolescents (accessed on 10 March 2022).
- Kiburi, S.K.; Molebatsi, K.; Obondo, A.; Kuria, M.W. Adverse childhood experiences among patients with substance use disorders at a referral psychiatric hospital in Kenya. BMC Psychiatry 2018, 18, 197. [Google Scholar] [CrossRef]
- Muchiri, B.W.; Dos Santos, M.M. Family management risk and protective factors for adolescent substance use in South Africa. Subst. Abus. Treat. Prev. Policy 2018, 13, 1–10. [Google Scholar] [CrossRef]
- Oshodi, O.Y.; Aina, O.F.; Onajole, A.T. Substance use among secondary school students in an urban setting in Nigeria: Prevalence and associated factors. Afr. J. Psychiatry 2010, 13, 52–57. [Google Scholar] [CrossRef] [PubMed]
- Birhanu, A.M.; Bisetegn, T.A.; Woldeyohannes, S.M. High prevalence of substance use and associated factors among high school adolescents in Woreta Town, Northwest Ethiopia: Multi-domain factor analysis. BMC Public Health 2014, 14, 1186. [Google Scholar] [CrossRef] [PubMed]
- Jere, D.L.; Norr, K.F.; Bell, C.C.; Corte, C.; Dancy, B.L.; Kaponda, C.P.; Levy, J.A. Substance Use and Risky Sexual Behaviors among Young Men Working at a Rural Roadside Market in Malawi. J. Assoc. Nurses AIDS Care 2017, 28, 250–265. [Google Scholar] [CrossRef] [PubMed]
- Ogunsola, O.O.; Fatusi, A.O. Risk and protective factors for adolescent substance use: A comparative study of secondary school students in rural and urban areas of Osun State, Nigeria. Int. J. Adolesc. Med. Health 2016, 29, 20150096. [Google Scholar] [CrossRef]
- Chauke, T.M.; van der Heever, H.; Hoque, M.E. Alcohol use amongst learners in rural high school in South Africa. Afr. J. Prim. Health Care Fam. Med. 2015, 7, e1–e6. [Google Scholar] [CrossRef] [PubMed]
- Morojele, N.; Parry, C.; Brook, J. Substance abuse and the young: Taking action. MRC Res. Brief 2009, 6, 1–4. [Google Scholar]
- Carney, T.; Myers, B.J.; Louw, J.; Lombard, C.; Flisher, A.J. The relationship between substance use and delinquency among high-school students in Cape Town, South Africa. J. Adolesc. 2013, 36, 447–455. [Google Scholar] [CrossRef] [PubMed]
- Gordon, K.; Kutywayo, A.; Frade, S.; Naidoo, N.; Mullick, S. Socio-demographic and social support factors related to substance use in South African in-school adolescents: Insights from the Girls Achieve Power (GAP Year) trial in three peri-urban settings. Gates Open Res. 2021, 5, 154. [Google Scholar] [CrossRef] [PubMed]
- Mokwena, K.; Sindane, P. Cigarette smoking and alcohol intake among high school learners in Pretoria, South Africa. Psychol. Educ. J. 2020, 57, 531–536. [Google Scholar]
- Mokwena, K.E.; Setshego, N.J. Substance abuse among high school learners in a rural education district in the Free State province, South Africa. S. Afr. Fam. Pract. 2021, 63, e1–e6. [Google Scholar] [CrossRef] [PubMed]
- Tshitangano, T.G.; Tosin, O.H. Substance use amongst secondary school students in a rural setting in South Africa: Prevalence and possible contributing factors. Afr. J. Prim. Health Care Fam. Med. 2016, 8, e1–e6. [Google Scholar] [CrossRef] [PubMed]
- Shilubane, H.N.; Ruiter, R.A.C.; van den Borne, B.; Sewpaul, R.; James, S.; Reddy, P.S. Suicide and related health risk behaviours among school learners in South Africa: Results from the 2002 and 2008 national youth risk behaviour surveys. BMC Public Health 2013, 13, 926. [Google Scholar] [CrossRef] [PubMed]
- Van Scheepers, C.L.W. Ethnicity, cultural diversity and poverty in South Africa: Archaeological perspectives from iron age Palestine. Old Testam. Essays 2010, 23, 161–177. [Google Scholar]
- Mathabela, B.; Madiba, S.; Modjadji, P. Exploring Barriers to Accessing Sexual and Reproductive Health Services among Adolescents and Young People with Physical Disabilities in South Africa. Int. J. Environ. Res. Public Health 2024, 21, 199. [Google Scholar] [CrossRef]
- Debeila, S.; Modjadji, P.; Madiba, S. High prevalence of overall overweight/obesity and abdominal obesity amongst adolescents: An emerging nutritional problem in rural high schools in Limpopo Province, South Africa. Afr. J. Prim. Health Care Fam. Med. 2021, 13, 1–9. [Google Scholar] [CrossRef]
- Mengwai, K.; Madiba, S.; Modjadji, P. Low Disclosure Rates to Sexual Partners and Unsafe Sexual Practices of Youth Recently Diagnosed with HIV; Implications for HIV Prevention Interventions in South Africa. Healthcare 2020, 8, 253. [Google Scholar] [CrossRef]
- Mkhwanazi, T.W.; Modjadji, P.; Mokgalaboni, K.; Madiba, S.; Roomaney, R.A. Multimorbidity, Treatment, and Determinants among Chronic Patients Attending Primary Health Facilities in Tshwane, South Africa. Diseases 2023, 11, 129. [Google Scholar] [CrossRef]
- Modjadji, P. Communicable and non-communicable diseases coexisting in South Africa. Lancet Glob. Health 2021, 9, e889–e890. [Google Scholar] [CrossRef] [PubMed]
- Bhana, R. Youth Risk Behaviour. Health Systems Trust. 2003. Available online: https://www.hst.org.za/publications/South%20African%20Health%20Reviews/15%20-%20Chapter%209.pdf (accessed on 23 February 2024).
- WHO. SDG Target 3.5 Substance Abuse; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- Manu, E.; Douglas, M.; Ayanore, M. Socio-ecological influences of adolescence marijuana use initiation: Qualitative evidence from two illicit marijuana-growing communities in South Africa. S. Afr. J. Psychiatry 2020, 26, 1–11. [Google Scholar] [CrossRef]
- Scarneo, S.E.; Kerr, Z.Y.; Kroshus, E.; Register-Mihalik, J.K.; Hosokawa, Y.; Stearns, R.L.; DiStefano, L.J.; Casa, D.J. The Socioecological Framework: A Multifaceted Approach to Preventing Sport-Related Deaths in High School Sports. J. Athl. Train. 2019, 54, 356–360. [Google Scholar] [CrossRef] [PubMed]
- UnitedNations. United Nations Office on Drugs and Crime. Drugs and Age: Drugs and Associated Issues among Young People and Older People. United Nations. 2018. Available online: https://www.unodc.org/wdr2018/prelaunch/WDR18_Booklet_4_YOUTH.pdf (accessed on 7 February 2024).
- Britannica. Mpumalanga Province, South Africa. 2023. Available online: https://www.britannica.com/place/Mpumalanga (accessed on 16 June 2023).
- Isla, J. The Impact of Unemployment on Poverty in South Africa: Uemployment. Oddysey. 2023. Available online: https://www.theodysseyonline.com/the-impact-of-unemployment-on-poverty-in-south-africa/particle-1 (accessed on 20 February 2024).
- Ghuman, S.; Meyer-Weitz, A.; Knight, S. Prevalence patterns and predictors of alcohol use and abuse among secondary school students in southern KwaZulu-Natal, South Africa: Demographic factors and the influence of parents and peers. S. Afr. Fam. Pract. 2012, 54, 132–138. [Google Scholar] [CrossRef]
- Khuzwayo, N.; Taylor, M.; Connolly, C. Changing youth behaviour in South Africa. Health SA = SA Gesondheid 2020, 25, 1031. [Google Scholar] [CrossRef]
- WHO. Alcohol, Consumers, Past 12 Months; World Haelth Organization: Geneve, Switzerland, 2024; Available online: https://www.who.int/data/gho/indicator-metadata-registry/imr-details/2325 (accessed on 12 January 2024).
- Kugbey, N. Prevalence and correlates of substance use among school-going adolescents (11–18 years) in eight Sub-Saharan Africa countries. Subst. Abus. Treat. Prev. Policy 2023, 18, 44. [Google Scholar] [CrossRef]
- Reddy, S.; Panday, S.; Swart, D.; Jinabhai, C.; Amosun, S.; James, S.; Monyeki, K.; Stevens, G.; Morejele, N.; Kambaran, N. Umthenthe Uhlaba Usamila–The South African Youth Risk Behaviour Survey 2002; South African Medical Research Council: Cape Town, South Africa, 2003; Volume 20. [Google Scholar]
- Reddy, S.P.; James, S.; Sewpaul, R.; Sifunda, S.; Ellahebokus, A.; Kambaran, N.S.; Omardien, R.G. Umthente Uhlaba Usamila: The 3rd South African National Youth Risk Behaviour Survey 2011; South African Medical Research Council: Cape Town, South Africa, 2013. [Google Scholar]
- Department of Tradeand Industry. Final Liquor Policy Paper National Liquor Policy Review. 2016. Available online: https://www.gov.za/sites/default/files/gcis_document/201609/40321gon1208.pdf (accessed on 1 June 2023).
- Benţea, C.-C. Motivations for alcohol use in late adolescence and educational strategies of intervention. Procedia-Soc. Behav. Sci. 2014, 128, 186–191. [Google Scholar] [CrossRef]
- Whiteford, H.A.; Degenhardt, L.; Rehm, J.; Baxter, A.J.; Ferrari, A.J.; Erskine, H.E.; Charlson, F.J.; Norman, R.E.; Flaxman, A.D.; Johns, N. Global burden of disease attributable to mental and substance use disorders: Findings from the Global Burden of Disease Study 2010. Lancet 2013, 382, 1575–1586. [Google Scholar] [CrossRef] [PubMed]
- WHO. Global Strategy to Reduce the Harmful Use of Alcohol; The World Health Organization: Switerland, Geneva, 2010. [Google Scholar]
- Onya, H.; Tessera, A.; Myers, B.; Flisher, A. Adolescent alcohol use in rural South African high schools: Original. Afr. J. Psychiatry 2012, 15, 352–357. [Google Scholar] [CrossRef] [PubMed]
- Onaolapo, O.J.; Olofinnade, A.T.; Ojo, F.O.; Adeleye, O.; Falade, J.; Onaolapo, A.Y. Substance use and substance use disorders in Africa: An epidemiological approach to the review of existing literature. World J. Psychiatry 2022, 12, 1268–1286. [Google Scholar] [CrossRef] [PubMed]
- Hibell, B.; Guttormsson, U.; Ahlström, S.; Balakireva, O.; Kokkevi, T.B.A.; Kraus, L. The 2011 ESPAD Report: Substance Use among Students in 36 European Countries; EPSAD: Stockholm, Sweden, 2012. [Google Scholar]
- Eaton, D.K.; Kann, L.; Kinchen, S.; Shanklin, S.; Flint, K.H.; Hawkins, J.; Harris, W.A.; Lowry, R.; McManus, T.; Chyen, D.; et al. Youth risk behavior surveillance—United States, 2011. Morb. Mortal. Wkly. Rep. Surveill. Summ. 2012, 61, 1–162. [Google Scholar]
- Johnston, L.D.; O’Malley, P.M.; Miech, R.A.; Bachman, J.G.; Schulenberg, J.E. Overview: Key Findings on Adolescent Drug Use, 1975–2014; Institute for Social Research, The University of Michigan: Ann Arbor, MI, USA, 2015. [Google Scholar]
- Flisher, A.J.; Townsend, L.; Chikobvu, P.; Lombard, C.F.; King, G. Substance use and psychosocial predictors of high school dropout in Cape Town, South Africa. J. Res. Adolesc. 2010, 20, 237–255. [Google Scholar] [CrossRef]
- Moodley, S.V.; Matjila, M.J.; Moosa, M. Epidemiology of substance use among secondary school learners in Atteridgeville, Gauteng. S. Afr. J. Psychiatry 2012, 18, 2–7. [Google Scholar] [CrossRef]
- Dida, N.; Kassa, Y.; Sirak, T.; Zerga, E.; Dessalegn, T. Substance use and associated factors among preparatory school students in Bale Zone, Oromia Regional State, Southeast Ethiopia. Harm Reduct. J. 2014, 11, 21. [Google Scholar] [CrossRef]
- Osei-Bonsu, E.; Appiah, P.K.; Norman, I.D.; Asalu, G.A.; Kweku, M.; Ahiabor, S.Y.; Takramah, W.K.; Duut, A.B.; Ntow, G.E.; Boadu, S. Prevalence of alcohol consumption and factors influencing alcohol use among the youth in Tokorni-Hohoe, Volta region of Ghana. Sci. J. Public Health 2017, 5, 205–214. [Google Scholar] [CrossRef]
- Letsela, L.; Weiner, R.; Gafos, M.; Fritz, K. Alcohol Availability, Marketing, and Sexual Health Risk Amongst Urban and Rural Youth in South Africa. AIDS Behav. 2019, 23, 175–189. [Google Scholar] [CrossRef]
- Rabotata, E.; Makhubele, J.; Mafa, P. Accessibility of alcohol as a risk factor contributing towards alcohol abuse amongst the youth of a selected rural community in Limpopo Province, South Africa. Tech. Soc. Sci. J. 2021, 25, 715–721. [Google Scholar] [CrossRef]
- Frank, R.; Makhubele, J.; Ananias, J.; Svinurai, A.; Winnie, M.; Tiberia, H.; Ilonga, N.; Freeman, R.; Mafa, P.; Matlakala, F.; et al. Non-Governmental Organisations Personnel, Social Workers and Religious Leaders’ Perspectives on the Risk Factors of Alcohol Abuse amongst the Youth: The Case of the Northern Region of the Republic of Namibia. Glob. J. Health Sci. 2019, 11, 55. [Google Scholar] [CrossRef]
- Martins, J.G.; Guimarães, M.O.; Jorge, K.O.; Silva, C.J.P.; Ferreira, R.C.; Pordeus, I.A.; Kawachi, I.; Zarzar, P. Binge drinking, alcohol outlet density and associated factors: A multilevel analysis among adolescents in Belo Horizonte, Minas Gerais State, Brazil. Cad. Saude Publica 2019, 36, e00052119. [Google Scholar] [CrossRef] [PubMed]
- Slaunwhite, A.K.; McEachern, J.; Ronis, S.T.; Peters, P.A. Alcohol distribution reforms and school proximity to liquor sales outlets in New Brunswick. Can. J. Public Health 2017, 108, e488–e496. [Google Scholar] [CrossRef] [PubMed]
- Dunn, M.S. Association between physical activity and substance use behaviors among high school students participating in the 2009 Youth Risk Behavior Survey. Psychol. Rep. 2014, 114, 675–685. [Google Scholar] [CrossRef] [PubMed]
- Glasser, N.J.; Jameson, J.C.; Tung, E.L.; Lindau, S.T.; Pollack, H.A. Associations of Adolescent School Social Networks, Gender Norms, and Adolescent-to-Young Adult Changes in Male Gender Expression with Young Adult Substance Use. J. Adolesc. Health 2024, 74, 755–763. [Google Scholar] [CrossRef] [PubMed]
- Kaufman, M.R.; Bazell, A.T.; Collaco, A.; Sedoc, J. “This show hits really close to home on so many levels”: An analysis of Reddit comments about HBO’s Euphoria to understand viewers’ experiences of and reactions to substance use and mental illness. Drug Alcohol Depend. 2021, 220, 108468. [Google Scholar] [CrossRef] [PubMed]
- Nath, A.; Choudhari, S.G.; Dakhode, S.U.; Rannaware, A.; Gaidhane, A.M. Substance Abuse Amongst Adolescents: An Issue of Public Health Significance. Cureus 2022, 14, e31193. [Google Scholar] [CrossRef] [PubMed]
- Grigsby, T.J.; Forster, M.; Soto, D.W.; Unger, J.B. Changes in the strength of peer influence and cultural factors on substance use initiation between late adolescence and emerging adulthood in a Hispanic sample. J. Ethn. Subst. Abus. 2017, 16, 137–154. [Google Scholar] [CrossRef]
- Booth, J.M.; Shaw, D.S. Examining Parental Monitoring, Neighborhood Peer Anti-social Behavior, and Neighborhood Social Cohesion and Control as a Pathway to Adolescent Substance Use. J. Child Fam. Stud. 2023, 32, 626–639. [Google Scholar] [CrossRef]
- McLaughlin, A.; Campbell, A.; McColgan, M. Adolescent Substance Use in the Context of the Family: A Qualitative Study of Young People’s Views on Parent-Child Attachments, Parenting Style and Parental Substance Use. Subst. Use Misuse 2016, 51, 1846–1855. [Google Scholar] [CrossRef]
- Calafat, A.; Gómez, C.; Juan, M.; Becona, E. Recreational nightlife: Risk and protective factors for drug misuse among young Europeans in recreational environments. Drugs: Educ. Prev. Policy 2009, 15, 189–200. [Google Scholar] [CrossRef]
- Veliz, P.T.; Boyd, C.J.; McCabe, S.E. Competitive sport involvement and substance use among adolescents: A nationwide study. Subst. Use Misuse 2015, 50, 156–165. [Google Scholar] [CrossRef] [PubMed]
- Mahsoon, A.N.; Almashat, L.; Alsubaui, N.; Hindi, S.; Alharbi, S.; Yaghmour, S.; Sharif, L. Socio-Demographics of Initial Substance Use Exposure and Its Relation to Progression: A Cross-Sectional Study in Saudi Arabia. Cureus 2023, 15, e42795. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Chen, C.; Abdullah, A.S.; Liu, L.; Sharma, M.; Li, Y.; Zhao, Y. Smoking related attitudes, motives, and behaviors of male secondary school students in an urban setting of China. SpringerPlus 2016, 5, 2021. [Google Scholar] [CrossRef] [PubMed]
- Mahanta, B.; Mohapatra, P.K.; Phukan, N.; Mahanta, J. Alcohol use among school-going adolescent boys and girls in an industrial town of Assam, India. Indian J. Psychiatry 2016, 58, 157–163. [Google Scholar] [CrossRef] [PubMed]
- Sivapuram, M.S.; Nagarathna, R.; Anand, A.; Patil, S.; Singh, A.; Nagendra, H.R. Prevalence of Alcohol and Tobacco Use in India and Implications for COVID-19—Niyantrita Madhumeha Bharata Study Projections. J. Med. Life 2020, 13, 499–509. [Google Scholar] [CrossRef] [PubMed]
- El Ansari, W.; Stock, C.; Mills, C. Is alcohol consumption associated with poor academic achievement in university students? Int. J. Prev. Med. 2013, 4, 1175–1188. [Google Scholar]
- CDC. Making the Connection: Alcohol Behaviors and Academic Grades. Centers for Disease Control and Prevention. 2019. Available online: https://www.cdc.gov/healthyyouth/health_and_academics/pdf/DASHfactsheetAlcohol.pdf (accessed on 26 January 2024).
- WHO. Substance Use among Young People in Urban Environments; World Health Organization: Geneva, Switzerland, 2005. [Google Scholar]
- Tanner-Smith, E.E.; Nichols, L.M.; Loan, C.M.; Finch, A.J.; Moberg, D.P. Recovery High School Attendance Effects on Student Delinquency and Substance Use: The Moderating Role of Social Problem Solving Styles. Prev. Sci. Off. J. Soc. Prev. Res. 2020, 21, 1104–1113. [Google Scholar] [CrossRef]
- Biz Community. BMR Youth Research Unit on Gauteng Youth’s High Drug, Alcohol Use. 2012. Available online: https://www.bizcommunity.com/Article/196/347/74114.html (accessed on 8 March 2024).
- Bukstein, O.G. Aggression, Violence, and Substance Abuse in Adolescents. Child Adolesc. Psychiatr. Clin. N. Am. 1996, 5, 93–109. [Google Scholar] [CrossRef]
- Bray, J.W.; Zarkin, G.A.; Ringwalt, C.; Qi, J. The relationship between marijuana initiation and dropping out of high school. Health Econ. 2000, 9, 9–18. [Google Scholar] [CrossRef]
- Brook, J.S.; Stimmel, M.A.; Zhang, C.; Brook, D.W. The association between earlier marijuana use and subsequent academic achievement and health problems: A longitudinal study. Am. J. Addict. 2008, 17, 155–160. [Google Scholar] [CrossRef]
- Bugbee, B.A.; Beck, K.H.; Fryer, C.S.; Arria, A.M. Substance Use, Academic Performance, and Academic Engagement among High School Seniors. J. Sch. Health 2019, 89, 145–156. [Google Scholar] [CrossRef] [PubMed]
- Homel, J.; Thompson, K.; Leadbeater, B. Trajectories of marijuana use in youth ages 15–25: Implications for postsecondary education experiences. J. Stud. Alcohol Drugs 2014, 75, 674–683. [Google Scholar] [CrossRef]
- Powers, A.R.; Kelley, M.; Corlett, P.R. Hallucinations as Top-Down Effects on Perception. Biol. Psychiatry Cogn. Neurosci. Neuroimaging 2016, 1, 393–400. [Google Scholar] [CrossRef] [PubMed]
- Shalit, N.; Rehm, J.; Lev-Ran, S. Epidemiology of hallucinogen use in the U.S. results from the National epidemiologic survey on alcohol and related conditions III. Addict. Behav. 2018, 89, 35–43. [Google Scholar] [CrossRef]
- Walsh, Z.; Hendricks, P.S.; Smith, S.; Kosson, D.S.; Thiessen, M.S.; Lucas, P.; Swogger, M.T. Hallucinogen use and intimate partner violence: Prospective evidence consistent with protective effects among men with histories of problematic substance use. J. Psychopharmacol. 2016, 30, 601–607. [Google Scholar] [CrossRef]
- Baggott, M.J.; Coyle, J.R.; Erowid, E.; Erowid, F.; Robertson, L.C. Abnormal visual experiences in individuals with histories of hallucinogen use: A Web-based questionnaire. Drug Alcohol Depend. 2011, 114, 61–67. [Google Scholar] [CrossRef]
- Robles-Ramamurthy, B.; Zaki, S.; Sandoval, J.F.; Dube, A.R.; Hlozek, S.; Fortuna, L.R.; Williamson, A.A. Improving adolescent sleep in long-term Juvenile correctional settings: Case examples with clinical, research, and policy implications. SLEEP Adv. 2024, 5, zpae006. [Google Scholar] [CrossRef] [PubMed]
- Edwards, S.; Reeves, G.; Fishbein, D. Integrative Model of the Relationship Between Sleep Problems and Risk for Youth Substance Use. Curr. Addict. Rep. 2015, 2, 130–140. [Google Scholar] [CrossRef]
- Nguyen-Louie TT, Brumback T, Worley MJ, Colrain IM, Matt GE, Squeglia LM, Tapert SF: Effects of sleep on substance use in adolescents: A longitudinal perspective. Addict. Biol. 2018, 23, 750–760. [CrossRef]
- McBride, N.; McKay, M.; Sumnall, H. SHAHRP: School health and alcohol harm reduction project—Developments in Australia and the UK. Educ. Health 2013, 31, 79–83. [Google Scholar]
- Gorman, D.M.; Conde, E. The Making of Evidence-based Practice: The Case of Project ALERT. Child. Youth Serv. Rev. 2010, 32, 214–222. [Google Scholar] [CrossRef][Green Version]
- Longshore, D.; Ellickson, P.; McCaffrey, D.; Clair, P. School-Based Drug Prevention Among At-Risk Adolescents: Effects of ALERT Plus. Health Educ. Behav. 2007, 34, 651–668. [Google Scholar] [CrossRef]
- Kreeft, P.V.; Wiborg, G.; Galanti, M.R.; Siliquini, R.; Bohrn, K.; Scatigna, M.; Lindahl, A.M.; Melero, J.C.; Vassara, M.; Faggiano, F.; et al. “Unplugged”: A new European School programme against substance abuse. Drugs Educ. Prev. Policy 2009, 16, 167–181. [Google Scholar] [CrossRef]
- Alarcó-Rosales, R.; Sánchez-SanSegundo, M.; Ferrer-Cascales, R.; Albaladejo-Blazquez, N.; Lordan, O.; Zaragoza-Martí, A. Effects of a School-Based Intervention for Preventing Substance Use among Adolescents at Risk of Academic Failure: A Pilot Study of the Reasoning and Rehabilitation V2 Program. Healthcare 2021, 9, 1488. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).