How Social Influence Promotes the Adoption of Mobile Health among Young Adults in China: A Systematic Analysis of Trust, Health Consciousness, and User Experience
Abstract
1. Introduction
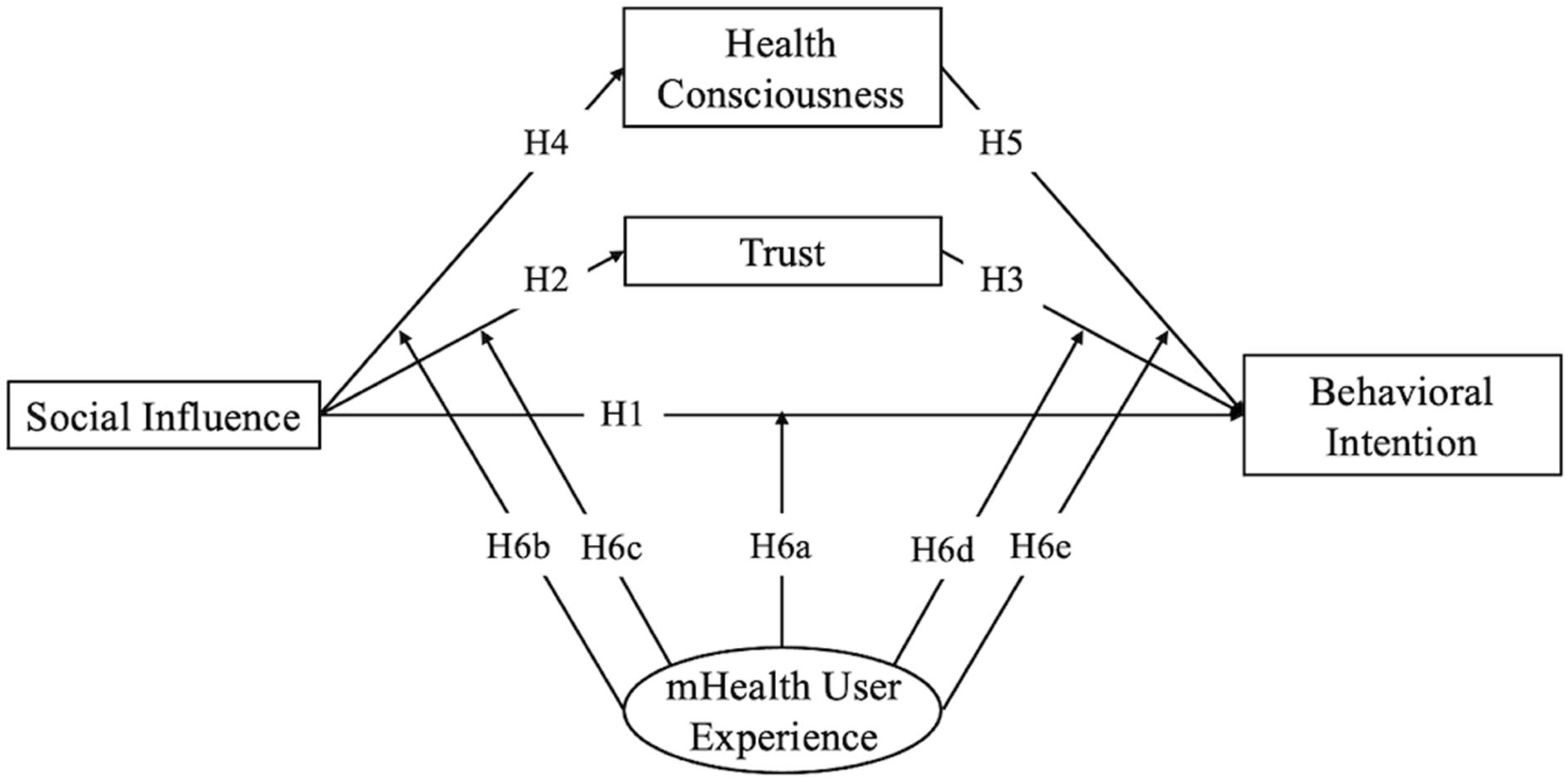
1.1. Theoretical Background and Hypotheses
Theoretical Framework Based on Social Influence
1.2. The Introduction of Trust as a Mediating Variable
1.3. The Introduction of Health Consciousness as a Mediating Variable
1.4. The Moderating Effect of mHealth User Experience
2. Methods
2.1. Questionnaire Design
2.2. Data Collection
2.3. Data Analysis
3. Results
3.1. Measurement Model
3.2. Results of the Structural Model and Hypothesis Testing
4. Discussion
4.1. Principal Findings
4.2. Theoretical Implications
4.3. Practical Implications
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Construct | Items | |
|---|---|---|
| Social Influence (SI) | SI1 | People who are important to me think that I should use mHealth service. |
| SI2 | People who influence my behavior think that I should use mHealth service. | |
| SI3 | People whose opinions I value prefer that I use mHealth service. | |
| Trust (TR) | TR1 | I have trust in academic researchers working on mHealth service projects. |
| TR2 | I have trust that mHealth service is providing great value to the society | |
| TR3 | I have trust that government will improves relevant regulations on mHealth service. | |
| TR4 | I have trust that mHealth providers will improve user privacy management. | |
| Health Consciousness (HC) | HC1 | I reflect about my health a lot. |
| HC2 | I am very self-conscious about my health. | |
| HC3 | I am generally attentive to my inner feelings about my health. | |
| HC4 | I am constantly examining my health conditions. | |
| HC5 | I think that I take health matters into account a lot in my life. | |
| HC6 | I think it is important to know well how to eat healthily. | |
| Behavioral Intention (BI) | BI1 | I intend to use mHealth service in the future. |
| BI2 | I will always try to use mHealth service in my daily life. | |
| BI3 | I plan to use mHealth service frequently. | |
References
- Cao, J.; Lim, Y.; Sengoku, S.; Guo, X.; Kodama, K. Exploring the Shift in International Trends in Mobile Health Research From 2000 to 2020: Bibliometric Analysis. JMIR mHealth uHealth 2021, 9, e31097. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. mHealth: New Horizons for Health through Mobile Technologies (Global Observatory for eHealth); WHO Press: Geneva, Switzerland, 2011; Available online: https://iris.who.int/bitstream/handle/10665/44607/9789241564250_eng.pdf;jsessionid=B5BF42C05D0775CCD552FD82AA82543A?sequence=1 (accessed on 25 March 2024).
- Hsu, J.; Liu, D.; Yu, Y.M.; Zhao, H.T.; Chen, Z.R.; Li, J.; Chen, W. The Top Chinese Mobile Health Apps: A Systematic Investigation. J. Med. Internet Res. 2016, 18, e222. [Google Scholar] [CrossRef] [PubMed]
- Seetharam, K.; Kagiyama, N.; Sengupta, P.P. Application of mobile health, telemedicine and artificial intelligence to echocardiography. Echo Res. Pract. 2019, 6, R41–R52. [Google Scholar] [CrossRef] [PubMed]
- Weinstein, R.S.; Krupinski, E.A.; Doarn, C.R. Clinical Examination Component of Telemedicine, Telehealth, mHealth, and Connected Health Medical Practices. Med. Clin. N. Am. 2018, 102, 533–544. [Google Scholar] [CrossRef] [PubMed]
- Lukas, H.; Xu, C.; Yu, Y.; Gao, W. Emerging Telemedicine Tools for Remote COVID-19 Diagnosis, Monitoring, and Management. ACS Nano 2020, 14, 16180–16193. [Google Scholar] [CrossRef]
- DeVore, A.D.; Wosik, J.; Hernandez, A.F. The Future of Wearables in Heart Failure Patients. JACC Heart Fail. 2019, 7, 922–932. [Google Scholar] [CrossRef] [PubMed]
- Anglada-Martinez, H.; Riu-Viladoms, G.; Martin-Conde, M.; Rovira-Illamola, M.; Sotoca-Momblona, J.M.; Codina-Jane, C. Does mHealth increase adherence to medication? Results of a systematic review. Int. J. Clin. Pract. 2015, 69, 9–32. [Google Scholar] [CrossRef]
- Kassianos, A.P.; Georgiou, G.; Papaconstantinou, E.P.; Detzortzi, A.; Horne, R. Smartphone Applications for Educating and Helping Non-motivating Patients Adhere to Medication That Treats Mental Health Conditions: Aims and Functioning. Front. Psychol. 2017, 8, 1769. [Google Scholar] [CrossRef]
- Su, Y.; Wu, K.-C.; Chien, S.-Y.; Naik, A.; Zaslavsky, O. A Mobile Intervention Designed Specifically for Older Adults With Frailty to Support Healthy Eating: Pilot Randomized Controlled Trial. JMIR Form. Res. 2023, 7, e50870. [Google Scholar] [CrossRef]
- Vandelanotte, C.; Müller, A.M.; Short, C.E.; Hingle, M.; Nathan, N.; Williams, S.L.; Lopez, M.L.; Parekh, S.; Maher, C.A. Past, Present, and Future of eHealth and mHealth Research to Improve Physical Activity and Dietary Behaviors. J. Nutr. Educ. Behav. 2016, 48, 219–228.e1. [Google Scholar] [CrossRef]
- Zapata, B.C.; Fernández-Alemán, J.L.; Idri, A.; Toval, A. Empirical Studies on Usability of mHealth Apps: A Systematic Literature Review. J. Med. Syst. 2015, 39, 1. [Google Scholar] [CrossRef] [PubMed]
- Bhavnani, S.P.; Narula, J.; Sengupta, P.P. Mobile technology and the digitization of healthcare. Eur. Heart J. 2017, 37, 1428–1438. [Google Scholar] [CrossRef] [PubMed]
- Steinhubl, S.R.; Muse, E.D.; Topol, E.J. The emerging field of mobile health. Sci. Transl. Med. 2015, 7, 283. [Google Scholar] [CrossRef] [PubMed]
- Sunyaev, A.; Dehling, T.; Taylor, P.L.; Mandl, K.D. Availability and quality of mobile health app privacy policies. J. Am. Med. Informa. Assoc. 2015, 22, e28–e33. [Google Scholar] [CrossRef] [PubMed]
- Guo, X.; Zhang, X.; Sun, Y. The privacy–personalization paradox in mHealth services acceptance of different age groups. Electron. Commer. Res. Appl. 2016, 16, 55–65. [Google Scholar] [CrossRef]
- Peng, C.; He, M.; Cutrona, S.L.; I Kiefe, C.; Liu, F.; Wang, Z. Theme Trends and Knowledge Structure on Mobile Health Apps: Bibliometric Analysis. JMIR mHealth uHealth 2020, 8, e18212. [Google Scholar] [CrossRef] [PubMed]
- Düking, P.; Tafler, M.; Wallmann-Sperlich, B.; Sperlich, B.; Kleih, S. Behavior Change Techniques in Wrist-Worn Wearables to Promote Physical Activity: Content Analysis. JMIR mHealth uHealth 2020, 8, e20820. [Google Scholar] [CrossRef]
- Huhn, S.; Axt, M.; Gunga, H.-C.; Maggioni, M.A.; Munga, S.; Obor, D.; Sié, A.; Boudo, V.; Bunker, A.; Sauerborn, R.; et al. The Impact of Wearable Technologies in Health Research: Scoping Review. JMIR mHealth uHealth 2022, 10, e34384. [Google Scholar] [CrossRef]
- Kim, B.Y.; Lee, J. Smart Devices for Older Adults Managing Chronic Disease: A Scoping Review. JMIR mHealth uHealth 2017, 5, e69. [Google Scholar] [CrossRef]
- Gordon, N.P.; Hornbrook, M.C. Older adults’ readiness to engage with eHealth patient education and self-care resources: A cross-sectional survey. BMC Health Serv. Res. 2018, 18, 220. [Google Scholar] [CrossRef]
- Meng, F.; Guo, X.; Peng, Z.; Lai, K.-H.; Zhao, X. Investigating the Adoption of Mobile Health Services by Elderly Users: Trust Transfer Model and Survey Study. JMIR mHealth uHealth 2019, 7, e12269. [Google Scholar] [CrossRef] [PubMed]
- Quaosar, G.M.A.A.; Hoque, M.R.; Bao, Y. Investigating Factors Affecting Elderly’s Intention to Use m-Health Services: An Empirical Study. Telemed. e-Health 2018, 24, 309–314. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.; Guo, Y.; Wang, X.; Zeng, Q. mHealth For Aging China: Opportunities and Challenges. Aging Dis. 2016, 7, 53–67. [Google Scholar] [CrossRef] [PubMed]
- Coorey, G.M.; Neubeck, L.; Mulley, J.; Redfern, J. Effectiveness, acceptability and usefulness of mobile applications for cardiovascular disease self-management: Systematic review with meta-synthesis of quantitative and qualitative data. Eur. J. Prev. Cardiol. 2018, 25, 505–521. [Google Scholar] [CrossRef] [PubMed]
- Wildenbos, G.; Peute, L.; Jaspers, M. Aging barriers influencing mobile health usability for older adults: A literature based framework (MOLD-US). Int. J. Med. Inform. 2018, 114, 66–75. [Google Scholar] [CrossRef] [PubMed]
- To, W.-M.; Lee, P.K.C.; Lu, J.; Wang, J.; Yang, Y.; Yu, Q. What Motivates Chinese Young Adults to Use mHealth? Healthcare 2019, 7, 156. [Google Scholar] [CrossRef] [PubMed]
- Cao, J.; Kurata, K.; Lim, Y.; Sengoku, S.; Kodama, K. Social Acceptance of Mobile Health among Young Adults in Japan: An Extension of the UTAUT Model. Int. J. Environ. Res. Public Health 2022, 19, 15156. [Google Scholar] [CrossRef] [PubMed]
- Slater, H.; Campbell, J.M.; Stinson, J.N.; Burley, M.M.; Briggs, A.M. End User and Implementer Experiences of mHealth Technologies for Noncommunicable Chronic Disease Management in Young Adults: Systematic Review. J. Med. Internet Res. 2017, 19, e406. [Google Scholar] [CrossRef] [PubMed]
- Lu, C.; Hu, Y.; Xie, J.; Fu, Q.; Leigh, I.; Governor, S.; Wang, G. The Use of Mobile Health Applications to Improve Patient Experience: Cross-Sectional Study in Chinese Public Hospitals. JMIR mHealth uHealth 2018, 6, e126. [Google Scholar] [CrossRef]
- China Internet Network Information Center (CNNIC). The 52nd Statistical Report on China’s Internet Development. 2023. Available online: https://www.cnnic.com.cn/IDR/ReportDownloads/202311/P020231121355042476714.pdf (accessed on 25 March 2024).
- Rai, A.; Chen, L.; Pye, J.; Baird, A. Understanding Determinants of Consumer Mobile Health Usage Intentions, Assimilation, and Channel Preferences. J. Med. Internet Res. 2013, 15, e149. [Google Scholar] [CrossRef]
- Chinese Government Website. Data Report: Young People Are Gradually Becoming the “Heads of Family Health”. 2017. Available online: https://www.gov.cn/xinwen/2017-12/17/content_5247942.htm (accessed on 25 March 2024).
- Venkatesh, V.; Morris, M.G.; Davis, G.B.; Davis, F.D. User Acceptance of Information Technology: Toward a Unified View. MIS Q. 2003, 27, 425–478. [Google Scholar] [CrossRef]
- Ndayizigamiye, P.; Kante, M.; Shingwenyana, S. An adoption model of mHealth applications that promote physical activity. Cogent Psychol. 2020, 7, 1764703. [Google Scholar] [CrossRef]
- Garavand, A.; Samadbeik, M.; Nadri, H.; Rahimi, B.; Asadi, H. Effective Factors in Adoption of Mobile Health Applications between Medical Sciences Students Using the UTAUT Model. Methods Inf. Med. 2019, 58, 131–139. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Tao, D.; Yu, N.; Qu, X. Understanding consumer acceptance of healthcare wearable devices: An integrated model of UTAUT and TTF. Int. J. Med. Inform. 2020, 139, 104156. [Google Scholar] [CrossRef] [PubMed]
- Venkatesh, V.; Thong, J.Y.L.; Xu, X. Consumer Acceptance and Use of Information Technology: Extending the Unified Theory of Acceptance and Use of Technology. MIS Q. 2012, 36, 157–178. [Google Scholar] [CrossRef]
- Li, Z.; Du, N.; Wang, B.; Oteng-Darko, C. Impact of social influence on users’ continuance intention toward sports and fitness applications. Front. Public Health 2022, 10, 1031520. [Google Scholar] [CrossRef] [PubMed]
- Hoque, R.; Sorwar, G. Understanding factors influencing the adoption of mHealth by the elderly: An extension of the UTAUT model. Int. J. Med. Inform. 2017, 101, 75–84. [Google Scholar] [CrossRef] [PubMed]
- Alam, M.Z.; Hu, W.; Kaium, A.; Hoque, R.; Alam, M.M.D. Understanding the determinants of mHealth apps adoption in Bangladesh: A SEM-Neural network approach. Technol. Soc. 2020, 61, 101255. [Google Scholar] [CrossRef]
- De Veer, A.J.E.; Peeters, J.M.; Brabers, A.E.M.; Schellevis, F.G.; Rademakers, J.J.D.J.M.; Francke, A.L. Determinants of the intention to use e-Health by community dwelling older people. BMC Health Serv. Res. 2015, 15, 103. [Google Scholar] [CrossRef]
- Castanha, J.; Pillai, S.K.B.; Indrawati. What Influences Consumer Behavior Toward Information and Communication Technology Applications: A Systematic Literature Review of UTAUT2 Model. In ICT Systems and Sustainability Singapore; Tuba, M., Akashe, S., Joshi, A., Eds.; Springer: Singapore, 2021; pp. 317–327. [Google Scholar] [CrossRef]
- Duarte, P.; Pinho, J.C. A mixed methods UTAUT2-based approach to assess mobile health adoption. J. Bus. Res. 2019, 102, 140–150. [Google Scholar] [CrossRef]
- Farid, M.; Cao, J.; Lim, Y.; Arato, T.; Kodama, K. Exploring Factors Affecting the Acceptance of Genetically Edited Food Among Youth in Japan. Int. J. Environ. Res. Public Health 2020, 17, 2935. [Google Scholar] [CrossRef] [PubMed]
- Gefen, D.; Karahanna, E.; Straub, D.W. Trust and TAM in Online Shopping: An Integrated Model. MIS Q. 2003, 27, 51–90. [Google Scholar] [CrossRef]
- Mayer, R.C.; Davis, J.H.; Schoorman, F.D. An Integrative Model of Organizational Trust. Acad. Manag. Rev. 1995, 20, 709. [Google Scholar] [CrossRef]
- Sheppard, M.K. mHEALTH Apps: Disruptive Innovation, Regulation, and Trust—A Need For Balance. Med. Law Rev. 2020, 28, 549–572. [Google Scholar] [CrossRef] [PubMed]
- Lewis, T.L.; Wyatt, J.C. mHealth and Mobile Medical Apps: A Framework to Assess Risk and Promote Safer Use. J. Med. Internet Res. 2014, 16, e210. [Google Scholar] [CrossRef] [PubMed]
- Hassanaly, P.; Dufour, J.C. Analysis of the Regulatory, Legal, and Medical Conditions for the Prescription of Mobile Health Applications in the United States, The European Union, and France. Med. Devices Évid. Res. 2021, 14, 389–409. [Google Scholar] [CrossRef] [PubMed]
- Charani, E.; Castro-Sánchez, E.; Moore, L.S.; Holmes, A. Do Smartphone Applications in Healthcare Require a Governance and Legal Framework? It Depends on the Application! BMC Med. 2014, 12, 29. [Google Scholar] [CrossRef] [PubMed]
- McKnight, D.H.; Choudhury, V.; Kacmar, C. The impact of initial consumer trust on intentions to transact with a web site: A trust building model. J. Strat. Inf. Syst. 2002, 11, 297–323. [Google Scholar] [CrossRef]
- Li, X.; Hess, T.J.; Valacich, J.S. Why do we trust new technology? A study of initial trust formation with organizational information systems. J. Strat. Inf. Syst. 2008, 17, 39–71. [Google Scholar] [CrossRef]
- Gao, L.; Waechter, K.A. Examining the role of initial trust in user adoption of mobile payment services: An empirical investigation. Inf. Syst. Front. 2017, 19, 525–548. [Google Scholar] [CrossRef]
- Gefen, D. E-commerce: The role of familiarity and trust. Omega 2000, 28, 725–737. [Google Scholar] [CrossRef]
- McKnight, D.H.; Chervany, N.L. Reflections on an Initial Trust-Building Model. In Handbook of Trust Research; Bachmann, R., Zaheer, A., Eds.; Edward Elgar Publishing; 2006. [CrossRef]
- Wei, Z.; Zhao, Z.; Zheng, Y. Following the Majority: Social Influence in Trusting Behavior. Front. Neurosci. 2019, 13, 89. [Google Scholar] [CrossRef]
- Jayanti, R.K.; Burns, A.C. The Antecedents of Preventive Health Care Behavior: An Empirical Study. J. Acad. Mark. Sci. 1998, 26, 6–15. [Google Scholar] [CrossRef]
- Hong, H. Scale development for measuring health consciousness: Re-conceptualization. In Proceedings of the Twelfth Annual International Public Relations Research Conference, Coral Gables, FL, USA, 11–14 March 2009; pp. 212–233. Available online: https://www.instituteforpr.org/wp-content/uploads/IPRRC_12_Proceedings.pdf#page=212 (accessed on 25 March 2024).
- Osborne, R.H.; Batterham, R.W.; Elsworth, G.R.; Hawkins, M.; Buchbinder, R. The grounded psychometric development and initial validation of the Health Literacy Questionnaire (HLQ). BMC Public Health 2013, 13, 658. [Google Scholar] [CrossRef] [PubMed]
- Hong, H. An Extension of the Extended Parallel Process Model (EPPM) in Television Health News: The Influence of Health Consciousness on Individual Message Processing and Acceptance. Health Commun. 2011, 26, 343–353. [Google Scholar] [CrossRef] [PubMed]
- Mai, R.; Hoffmann, S. Taste lovers versus nutrition fact seekers: How health consciousness and self-efficacy determine the way consumers choose food products. J. Consum. Behav. 2012, 11, 316–328. [Google Scholar] [CrossRef]
- Kraft, F.B.; Goodell, P.W. Identifying the health conscious consumer. J. Health care Mark. 1993, 13, 18–25. [Google Scholar] [PubMed]
- Meng, F.; Guo, X.; Peng, Z.; Zhang, X.; Vogel, D. The routine use of mobile health services in the presence of health consciousness. Electron. Commer. Res. Appl. 2019, 35, 100847. [Google Scholar] [CrossRef]
- Cho, J.; Park, D.; Lee, H.E. Cognitive Factors of Using Health Apps: Systematic Analysis of Relationships Among Health Consciousness, Health Information Orientation, eHealth Literacy, and Health App Use Efficacy. J. Med. Internet Res. 2014, 16, e125. [Google Scholar] [CrossRef]
- Guo, X.; Chen, S.; Zhang, X.; Ju, X.; Wang, X. Exploring Patients’ Intentions for Continuous Usage of mHealth Services: Elaboration-Likelihood Perspective Study. JMIR mHealth uHealth 2020, 8, e17258. [Google Scholar] [CrossRef]
- Bandura, A. Health promotion from the perspective of social cognitive theory. Psychol. Health 1998, 13, 623–649. [Google Scholar] [CrossRef]
- Anderson, E.S.; Winett, R.A.; Wojcik, J.R. Self-regulation, self-efficacy, outcome expectations, and social support: Social cognitive theory and nutrition behavior. Ann. Behav. Med. 2007, 34, 304–312. [Google Scholar] [CrossRef] [PubMed]
- Zheng, P.; Guo, F.; Chen, Y.; Fu, Y.; Ye, T.; Fu, H. A Randomized Controlled Trial of Group Intervention Based on Social Cognitive Theory for Smoking Cessation in China. J. Epidemiol. 2007, 17, 147–155. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Zhang, L.; Mao, R.; Zhao, Q.; Stanton, B. Effect of social cognitive theory-based HIV education prevention program among high school students in Nanjing, China. Health Educ. Res. 2011, 26, 419–431. [Google Scholar] [CrossRef] [PubMed]
- Metzger, M.J.; Flanagin, A.J. Credibility and trust of information in online environments: The use of cognitive heuristics. J. Pragmat. 2013, 59, 210–220. [Google Scholar] [CrossRef]
- Rubin, J.B.; Borden, W.B. Coronary Heart Disease in Young Adults. Curr. Atheroscler. Rep. 2012, 14, 140–149. [Google Scholar] [CrossRef] [PubMed]
- Li, J. Gastric Cancer in Young Adults: A Different Clinical Entity from Carcinogenesis to Prognosis. Gastroenterol. Res. Pract. 2020, 2020, 1–13. [Google Scholar] [CrossRef] [PubMed]
- WJX. Available online: https://www.wjx.cn (accessed on 16 February 2020).
- Hair, J.F.; Sarstedt, M.; Ringle, C.M.; Mena, J.A. An assessment of the use of partial least squares structural equation modeling in marketing research. J. Acad. Mark. Sci. 2012, 40, 414–433. [Google Scholar] [CrossRef]
- Hair, J.F., Jr.; Matthews, L.M.; Matthews, R.L.; Sarstedt, M. PLS-SEM or CB-SEM: Updated guidelines on which method to use. Int. J. Multivar. Data Anal. 2017, 1, 107. [Google Scholar] [CrossRef]
- Hair, J.F.; Ringle, C.M.; Sarstedt, M. PLS-SEM: Indeed a Silver Bullet. J. Mark. Theory Pract. 2011, 19, 139–152. [Google Scholar] [CrossRef]
- Carlson, K.D.; Herdman, A.O. Understanding the Impact of Convergent Validity on Research Results. Organ. Res. Methods 2012, 15, 17–32. [Google Scholar] [CrossRef]
- Salmerón, R.; García, C.B.; García, J. Variance Inflation Factor and Condition Number in multiple linear regression. J. Stat. Comput. Simul. 2018, 88, 2365–2384. [Google Scholar] [CrossRef]
- Taber, K.S. The Use of Cronbach’s Alpha When Developing and Reporting Research Instruments in Science Education. Res. Sci. Educ. 2018, 48, 1273–1296. [Google Scholar] [CrossRef]
- Fornell, C.; Larcker, D.F. Evaluating Structural Equation Models with Unobservable Variables and Measurement Error. J. Mark. Res. 1981, 18, 39–50. [Google Scholar] [CrossRef]
- Guetz, B.; Bidmon, S. The Impact of Social Influence on the Intention to Use Physician Rating Websites: Moderated Mediation Analysis Using a Mixed Methods Approach. J. Med. Internet Res. 2022, 24, e37505. [Google Scholar] [CrossRef]
- Wang, J.; Xue, Y.; Liu, T. Consumer motivation for organic food consumption: Health consciousness or herd mentality. Front. Public Health 2023, 10, 1042535. [Google Scholar] [CrossRef]
- Yang, L.; Wu, J.; Mo, X.; Chen, Y.; Huang, S.; Zhou, L.; Dai, J.; Xie, L.; Chen, S.; Shang, H.; et al. Changes in Mobile Health Apps Usage Before and After the COVID-19 Outbreak in China: Semilongitudinal Survey. JMIR Public Health Surveill. 2023, 9, e40552. [Google Scholar] [CrossRef]

| Measure | Category | Value (N = 300), n (%) |
|---|---|---|
| Age | ||
| ≤20 | 203 (67.7) | |
| 21–30 | 93 (31) | |
| 31–40 | 4 (1.3) | |
| Gender | ||
| Men | 109 (36.3) | |
| Women | 191 (63.7) | |
| Job | ||
| Student | 300 (100) | |
| Smartphone Use (Year) | ||
| 1–3 | 23 (7.7) | |
| 4–6 | 137 (45.7) | |
| 8–10 | 89 (29.7) | |
| ≥10 | 51 (17) | |
| mHealth User Experience | ||
| Yes | 67 (22.3) | |
| No | 233 (77.7) |
| Items | Item Loadings | p-Value | |||
|---|---|---|---|---|---|
| BI a | HC b | SI c | TR d | ||
| BI1 | 0.946 | 0.000 | |||
| BI2 | 0.957 | 0.000 | |||
| BI3 | 0.957 | 0.000 | |||
| HC1 | 0.899 | 0.000 | |||
| HC3 | 0.898 | 0.000 | |||
| HC4 | 0.892 | 0.000 | |||
| HC5 | 0.904 | 0.000 | |||
| SI1 | 0.958 | 0.000 | |||
| SI2 | 0.975 | 0.000 | |||
| SI3 | 0.960 | 0.000 | |||
| TR1 | 0.889 | 0.000 | |||
| TR2 | 0.941 | 0.000 | |||
| TR3 | 0.949 | 0.000 | |||
| TR4 | 0.938 | 0.000 | |||
| TR5 | 0.904 | 0.000 | |||
| Construct | Cronbach’s Alpha | rho_a | CR e | AVE f |
|---|---|---|---|---|
| BI a | 0.950 | 0.950 | 0.968 | 0.909 |
| HC b | 0.920 | 0.924 | 0.943 | 0.807 |
| SI c | 0.962 | 0.962 | 0.975 | 0.930 |
| TR d | 0.957 | 0.958 | 0.967 | 0.854 |
| Construct | Correlation | |||
|---|---|---|---|---|
| BI | HC | SI | TR | |
| BI a | 0.953 | |||
| HC b | 0.793 | 0.898 | ||
| SI c | 0.858 | 0.748 | 0.964 | |
| TR d | 0.853 | 0.776 | 0.830 | 0.924 |
| Path (Hypothesis) | Model 1 | Model 2 | Hypothesis Test | ||
|---|---|---|---|---|---|
| Path Coefficient | p-Value | Path Coefficient | p-Value | ||
| SI a → BI b (H1) | 0.407 | 0.000 | 0.489 | 0.000 | Supported |
| SI → TR c (H2) | 0.830 | 0.000 | 0.903 | 0.000 | Supported |
| TR → BI (H3) | 0.342 | 0.000 | 0.334 | 0.001 | Supported |
| SI → HC d (H4) | 0.748 | 0.000 | 0.853 | 0.000 | Supported |
| HC → BI (H5) | 0.226 | 0.000 | 0.153 | 0.030 | Supported |
| mHealth User Experience × SI → BI (H6a) | N/A e | N/A | −0.173 | 0.258 | Unsupported |
| mHealth User Experience × SI → HC (H6b) | N/A | N/A | −0.537 | 0.000 | Supported |
| mHealth User Experience × SI → TR (H6c) | N/A | N/A | −0.373 | 0.000 | Supported |
| mHealth User Experience × TR → BI (H6d) | N/A | N/A | −0.004 | 0.979 | Unsupported |
| mHealth User Experience × HC → BI (H6e) | N/A | N/A | 0.245 | 0.040 | Supported |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cao, J.; Feng, H.; Lim, Y.; Kodama, K.; Zhang, S. How Social Influence Promotes the Adoption of Mobile Health among Young Adults in China: A Systematic Analysis of Trust, Health Consciousness, and User Experience. Behav. Sci. 2024, 14, 498. https://doi.org/10.3390/bs14060498
Cao J, Feng H, Lim Y, Kodama K, Zhang S. How Social Influence Promotes the Adoption of Mobile Health among Young Adults in China: A Systematic Analysis of Trust, Health Consciousness, and User Experience. Behavioral Sciences. 2024; 14(6):498. https://doi.org/10.3390/bs14060498
Chicago/Turabian StyleCao, Jianfei, Hanlin Feng, Yeongjoo Lim, Kota Kodama, and Shuo Zhang. 2024. "How Social Influence Promotes the Adoption of Mobile Health among Young Adults in China: A Systematic Analysis of Trust, Health Consciousness, and User Experience" Behavioral Sciences 14, no. 6: 498. https://doi.org/10.3390/bs14060498
APA StyleCao, J., Feng, H., Lim, Y., Kodama, K., & Zhang, S. (2024). How Social Influence Promotes the Adoption of Mobile Health among Young Adults in China: A Systematic Analysis of Trust, Health Consciousness, and User Experience. Behavioral Sciences, 14(6), 498. https://doi.org/10.3390/bs14060498






